Functional GI disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Functional GI disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Functional GI disorders US Medical PG Question 1: A 54-year-old man presents to the clinic for epigastric discomfort during the previous month. He states he has not vomited, but reports of having epigastric pain that worsens after most meals. The patient states that his stool “looks black sometimes.” The patient does not report of any weight loss. He has a past medical history of gastroesophageal reflux disease, diabetes mellitus, peptic ulcer disease, and Crohn’s disease. The patient takes over-the-counter ranitidine, and holds prescriptions for metformin and infliximab. The blood pressure is 132/84 mm Hg, the heart rate is 64/min, the respiratory rate is 14/min, and the temperature is 37.3°C (99.1°F). On physical examination, the abdomen is tender to palpation in the epigastric region. Which of the following is the most appropriate next step to accurately determine the diagnosis of this patient?
- A. Treat with PPI, clarithromycin, and amoxicillin before doing lab and imaging tests
- B. Urea breath testing
- C. Serology for Helicobacter pylori
- D. CT abdomen
- E. Endoscopy with biopsy (Correct Answer)
Functional GI disorders Explanation: ***Endoscopy with biopsy***
- Given the patient's age (>50 years), new-onset epigastric pain, history of **peptic ulcer disease**, and "black sometimes" stools suggesting **melena** or **upper gastrointestinal bleeding**, an endoscopy with biopsy is crucial [1].
- This procedure allows direct visualization of the esophageal, gastric, and duodenal mucosa, enabling identification of ulcers, erosions, or masses, and tissue collection for **histopathological examination** (e.g., for *H. pylori* infection, malignancy, or Crohn's disease involvement) [1].
*Treat with PPI, clarithromycin, and amoxicillin before doing lab and imaging tests*
- This approach, known as **"triple therapy,"** is a treatment for **H. pylori infection**, but it should not be initiated without a confirmed diagnosis in this patient presenting with alarm symptoms [2].
- Doing so without a prior diagnosis could mask underlying pathology, such as **malignancy**, and delay appropriate treatment.
*Urea breath testing*
- **Urea breath testing** is a non-invasive method to detect active *H. pylori* infection [2].
- While useful, it does not allow for direct visualization of the mucosa or biopsy collection, which is essential given the patient's **alarm features** like age and potential bleeding [2].
*Serology for Helicobacter pylori*
- **H. pylori serology** detects antibodies to *H. pylori*, indicating past or present infection [2].
- It cannot differentiate between active and past infection and, importantly, does not provide information about the **mucosal integrity** or allow for biopsy of suspicious lesions [2].
*CT abdomen*
- A **CT scan of the abdomen** can visualize abdominal organs and detect masses or significant inflammation.
- However, it is not the primary diagnostic tool for evaluating the **upper gastrointestinal mucosa** and cannot directly identify ulcers, erosions, or provide tissue for biopsy in the same way an endoscopy can.
Functional GI disorders US Medical PG Question 2: A 25-year-old male presents to his primary care physician for fatigue, abdominal pain, diarrhea, and weight loss. He states that this issue has occurred throughout his life but seems to “flare up” on occasion. He states that his GI pain is relieved with defecation, and his stools are frequent, large, and particularly foul-smelling. The patient has a past medical history of an ACL tear, as well as a car accident that resulted in the patient needing a transfusion and epinephrine to treat transfusion anaphylaxis. His current medications include vitamin D and ibuprofen. He recently returned from a camping trip in the eastern United States. He states that on the trip they cooked packed meats over an open fire and obtained water from local streams. His temperature is 99.5°F (37.5°C), blood pressure is 120/77 mmHg, pulse is 70/min, respirations are 11/min, and oxygen saturation is 98% on room air. Physical exam reveals poor motor control and an ataxic gait on neurologic exam. Cardiac and pulmonary exams are within normal limits. Laboratory studies are ordered and return as below:
Hemoglobin: 9.0 g/dL
Hematocrit: 25%
Haptoglobin: 12 mg/dL
Leukocyte count: 7,500 cells/mm^3 with normal differential
Platelet count: 255,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 102 mEq/L
K+: 5.0 mEq/L
HCO3-: 24 mEq/L
BUN: 24 mg/dL
Glucose: 82 mg/dL
Creatinine: 1.0 mg/dL
Ca2+: 9.0 mg/dL
LDH: 457 U/L
AST: 11 U/L
ALT: 11 U/L
Radiography is ordered which reveals a stress fracture in the patient’s left tibia. Which of the following is the best confirmatory test for this patient’s condition?
- A. Stool ELISA
- B. Vitamin B12 and folate level
- C. Vitamin E level (Correct Answer)
- D. Bowel wall biopsy
- E. Iron studies
Functional GI disorders Explanation: ***Vitamin E level***
- The patient's presentation suggests **celiac disease** causing **malabsorption** with secondary **vitamin E deficiency**, which is causing the specific complications seen here.
- The **neurological findings** of **ataxic gait** and **poor motor control** combined with **hemolytic anemia** (low haptoglobin 12 mg/dL, elevated LDH 457 U/L, anemia) are **pathognomonic for vitamin E deficiency**.
- Vitamin E deficiency causes **spinocerebellar degeneration**, **peripheral neuropathy**, and **hemolytic anemia** due to oxidative damage to RBC membranes and neuronal lipids.
- The **stress fracture** suggests bone disease from calcium/vitamin D malabsorption, but the neuro-hematologic picture is most specific for vitamin E.
- **Serum vitamin E level** is the **confirmatory test** for this specific deficiency syndrome causing the patient's neurological and hematological complications.
- While the underlying condition is likely celiac disease, confirming vitamin E deficiency directly explains the constellation of findings and guides immediate treatment.
*Bowel wall biopsy*
- A **small intestine biopsy** would confirm the underlying diagnosis of **celiac disease** (villous atrophy, crypt hyperplasia) causing the malabsorption.
- However, the question asks for confirmation of "this patient's condition" - referring to the specific syndrome presenting with the characteristic triad of **ataxia + hemolysis + malabsorption**.
- This triad is pathognomonic for **vitamin E deficiency**, making direct measurement more confirmatory for the presenting complication than tissue diagnosis of the underlying cause.
*Vitamin B12 and folate level*
- **Vitamin B12 deficiency** can cause **subacute combined degeneration** with ataxia and neurological symptoms, but typically presents with **posterior column signs** (loss of proprioception, vibration) and **peripheral neuropathy**, not primarily cerebellar ataxia.
- **Folate deficiency** causes **megaloblastic anemia** but does **not** cause neurological deficits or the hemolytic pattern seen here (low haptoglobin, elevated LDH with normal liver enzymes).
- The **hemolytic anemia** is specific to vitamin E deficiency, not B12/folate deficiency.
*Stool ELISA*
- Could detect **Giardia lamblia** given the history of drinking stream water during camping, which can cause acute diarrhea and malabsorption.
- However, this does not explain the **lifelong, recurring symptoms**, **neurological deficits**, **hemolytic anemia**, or **stress fracture**.
- The chronic nature points to a primary malabsorption disorder, not acute infection.
*Iron studies*
- **Iron deficiency** commonly occurs with celiac disease due to duodenal malabsorption and could contribute to the **anemia**.
- However, iron deficiency causes **microcytic anemia**, not hemolytic anemia, and does **not** explain the **low haptoglobin**, **elevated LDH**, **ataxic gait**, or **motor control issues**.
- These findings are specific to vitamin E deficiency.
Functional GI disorders US Medical PG Question 3: A 28-year-old graduate student visits the university health clinic for 3-weeks of epigastric pain that worsens with meals, associated with retrosternal pain, early satiety, and bloating. She denies vomiting blood or blood in her stool. She has been consuming large volumes of caffeinated-drinks and fast-food for a month, as she has been studying for her tests. Her family and personal history are unremarkable with no history of gastrointestinal cancer. Her vital signs are within normal limits. Physical examination is only positive for a mild epigastric tenderness. Which of the following is the most appropriate approach in this case?
- A. Treatment with metoclopramide
- B. Upper endoscopy
- C. Fecal antigen testing for Helicobacter pylori (Correct Answer)
- D. Treatment with omeprazole
- E. Barium swallow radiograph
Functional GI disorders Explanation: ***Fecal antigen testing for Helicobacter pylori***
- The patient presents with **dyspeptic symptoms** (epigastric pain, early satiety, bloating) and no **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia).
- Given her age (< 60 years) and lack of alarm symptoms, a "test-and-treat" strategy for **Helicobacter pylori** is recommended, with fecal antigen testing being a non-invasive and accurate option.
*Treatment with metoclopramide*
- Metoclopramide is a **prokinetic agent** used for conditions like gastroparesis, not primarily for initial management of undiagnosed dyspepsia.
- While she has early satiety, the primary approach should be to rule out common causes of dyspepsia like **H. pylori** before considering symptomatic treatments for motility issues.
*Upper endoscopy*
- An **upper endoscopy** is indicated if the patient is older (typically > 60 years) or has **alarm symptoms** (e.g., GI bleeding, unexplained weight loss, dysphagia, persistent vomiting).
- This 28-year-old patient lacks any alarm symptoms and is below the age threshold for an immediate endoscopic evaluation for dyspepsia.
*Treatment with omeprazole*
- While a **proton pump inhibitor (PPI)** like omeprazole can treat dyspeptic symptoms, it is not the most appropriate *initial* approach without first testing for **H. pylori**.
- Empiric PPI therapy can **mask H. pylori infection**, potentially delaying appropriate eradication therapy if the test-and-treat strategy is not followed.
*Barium swallow radiograph*
- A **barium swallow** is primarily used to evaluate structural abnormalities of the **esophagus**, such as strictures, diverticula, or achalasia, and is less effective for diagnosing mucosal diseases of the stomach or duodenum.
- It is not the preferred diagnostic test for evaluating dyspepsia or identifying **H. pylori** infection.
Functional GI disorders US Medical PG Question 4: A 58-year-old man presents to the emergency department with a 1-day history of difficulty swallowing. He also mentions that he has been frequently experiencing moderate to severe burning pain localized to the epigastric region for the last 3 weeks. The patient denies any history of vomiting, hematemesis, or black-colored stools. His past medical history is significant for gastroesophageal reflux disease diagnosed 10 years ago, for which he has not been compliant with medications. He has seen multiple physicians for similar complaints of retrosternal burning with regurgitation over the last 10 years but has not taken the medications suggested by the physicians regularly. He has never had a colonoscopy or endoscopy. He does not have any other known medical conditions, but he frequently takes over-the-counter analgesics for the relief of muscular pain. On physical examination, his vital signs are stable. Physical examination is normal except for the presence of mild pallor. Examination of the chest and abdomen does not reveal any abnormality. Which of the following investigations is indicated as the next step in the diagnostic evaluation of this patient?
- A. Ambulatory 24-hour pH monitoring
- B. Esophageal manometry
- C. Upper gastrointestinal endoscopy (Correct Answer)
- D. Intraluminal impedance monitoring
- E. Barium radiography of esophagus, stomach, and duodenum
Functional GI disorders Explanation: ***Upper gastrointestinal endoscopy***
- This patient presents with **dysphagia** and a long history of **untreated GERD**, raising concern for complications like **esophageal stricture** or **Barrett's esophagus**, which necessitate direct visualization.
- Endoscopy allows for **biopsy** of suspicious lesions (e.g., dysplasia, adenocarcinoma) and therapeutic interventions like **dilation of strictures**.
*Ambulatory 24-hour pH monitoring*
- This test is primarily used to **confirm GERD** in patients with atypical symptoms or to evaluate response to treatment, but it does not assess for structural complications.
- It would not identify conditions like **esophageal stricture** or **Barrett's esophagus**, which are a concern given the patient's dysphagia and long history of untreated GERD.
*Esophageal manometry*
- Esophageal manometry assesses **esophageal motility** and is useful in diagnosing motility disorders like **achalasia** but does not visualize the mucosa or detect structural abnormalities.
- While dysphagia can be a symptom of motility disorders, the patient's long history of GERD makes structural complications a more urgent concern.
*Intraluminal impedance monitoring*
- This test is often combined with pH monitoring to detect **non-acid reflux** or to evaluate patients with persistent symptoms despite acid-suppressive therapy.
- It does not provide information about the **mucosal integrity** or detect **structural abnormalities** that are highly suspected in this patient.
*Barium radiography of esophagus, stomach, and duodenum*
- While barium studies can identify **structural abnormalities** such as strictures or large ulcers, they are less sensitive than endoscopy for detecting subtle mucosal changes like **Barrett's esophagus** or early cancer.
- Barium studies also do not allow for **biopsy** of suspicious lesions, which is crucial for definitive diagnosis in this high-risk patient.
Functional GI disorders US Medical PG Question 5: A 31-year-old woman visits the clinic with chronic diarrhea on most days for the past four months. She also complains of lower abdominal discomfort and cramping, which is relieved by episodes of diarrhea. She denies any recent change in her weight. Bowel movements are preceded by a sensation of urgency, associated with mucus discharge, and followed by a feeling of incomplete evacuation. The patient went camping several months earlier, and another member of her camping party fell ill recently. Her temperature is 37° C (98.6° F), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Her physical examination is unremarkable. A routine stool examination is within normal limits and blood test results show:
Hb% 13 gm/dL
Total count (WBC): 11,000/mm3
Differential count:
Neutrophils: 70%
Lymphocytes: 25%
Monocytes: 5%
ESR: 10 mm/hr
What is the most likely diagnosis?
- A. Giardiasis
- B. Ulcerative colitis
- C. Crohn’s disease
- D. Irritable bowel syndrome (Correct Answer)
- E. Laxative abuse
Functional GI disorders Explanation: ***Irritable bowel syndrome (IBS)***
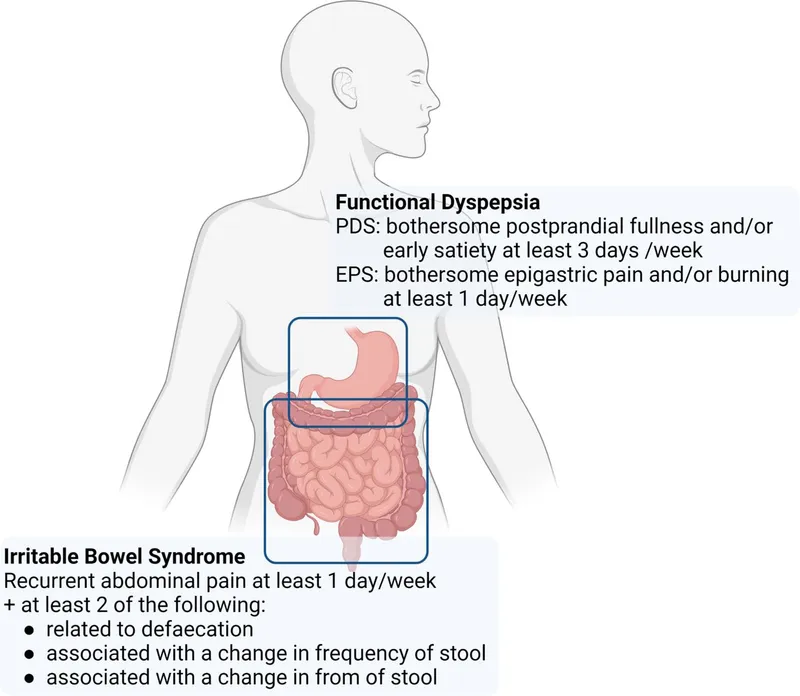
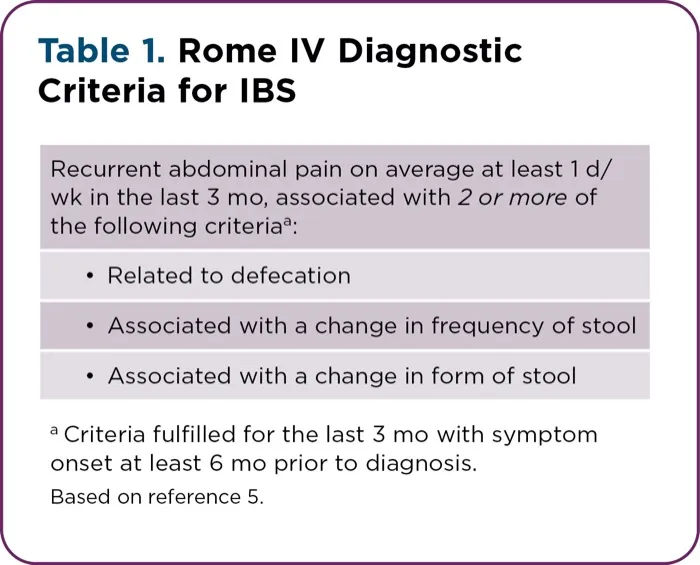
- The patient's symptoms of chronic diarrhea, abdominal discomfort relieved by defecation, urgency, and incomplete evacuation, without significant weight loss or alarming signs, are highly characteristic of **Irritable Bowel Syndrome** meeting **Rome IV criteria**.
- The camping history suggests possible infectious gastroenteritis, but the **chronic duration (4 months)**, **normal stool examination**, and **absence of systemic illness** make infectious causes unlikely.
- The mild WBC elevation and normal ESR are non-specific findings; IBS is a **functional disorder** without inflammatory markers.
*Giardiasis*
- While giardiasis can cause chronic diarrhea, it often presents with **malabsorption symptoms** such as fatty stools, weight loss, and nutrient deficiencies.
- The routine stool examination being within normal limits makes giardiasis less likely, as **Giardia cysts or trophozoites** would typically be detected on microscopy.
*Ulcerative colitis*
- Ulcerative colitis is an **inflammatory bowel disease** typically characterized by bloody diarrhea, abdominal pain, and systemic symptoms like fever and weight loss.
- The patient's symptoms include the absence of blood in stools and no weight loss, with **normal ESR**, which makes ulcerative colitis unlikely.
*Crohn's disease*
- Crohn's disease is another **inflammatory bowel disease** that can affect any part of the GI tract and presents with chronic diarrhea, abdominal pain, and often systemic symptoms like weight loss, fever, or perianal disease.
- The lack of weight loss, systemic inflammation markers (normal ESR), and absence of blood or inflammatory markers in the stool make Crohn's disease less probable.
*Laxative abuse*
- Laxative abuse can cause chronic diarrhea, but it's typically associated with a history of **eating disorders** (anorexia nervosa, bulimia nervosa) or other psychological conditions, which are not mentioned in this case.
- The patient's description of abdominal discomfort relieved by defecation, urgency, and incomplete evacuation is more consistent with **IBS** (a functional bowel disorder) rather than solely laxative-induced diarrhea.
Functional GI disorders US Medical PG Question 6: A 7-year-old boy is brought to the physician by his mother for the evaluation of abdominal pain and trouble sleeping for the past 6 months. His mother says he complains of crampy abdominal pain every morning on school days. He started attending a new school 7 months ago and she is concerned because he has missed school frequently due to the abdominal pain. He also has trouble falling asleep at night and asks to sleep in the same room with his parents every night. He has not had fever, vomiting, diarrhea, or weight loss. He sits very close to his mother and starts to cry when she steps out of the room to take a phone call. Abdominal examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Acute stress disorder
- B. Separation anxiety disorder (Correct Answer)
- C. Normal behavior
- D. Irritable bowel syndrome
- E. Conduct disorder
Functional GI disorders Explanation: ***Separation anxiety disorder***
- This child exhibits classic symptoms of **separation anxiety disorder**, including **school refusal** due to physical complaints (abdominal pain), **difficulty sleeping alone**, and **excessive distress** when separated from a primary attachment figure (mother).
- The symptoms started shortly after attending a new school, a common trigger for separation anxiety, and have persisted for 6 months, meeting the **diagnostic criteria for duration** in children (≥4 weeks).
*Acute stress disorder*
- **Acute stress disorder** typically occurs within one month of exposure to a **traumatic event** and involves symptoms like intrusive thoughts, negative mood, dissociation, and hypervigilance.
- The boy's symptoms are **chronic (6 months)** and are related to separation, not a specific traumatic event, making this diagnosis less likely.
*Normal behavior*
- While some mild separation anxiety is normal in young children, the **severity**, **duration (6 months)**, and **functional impairment** (missing school, difficulty sleeping alone) in this 7-year-old go beyond what is considered typical developmental behavior.
- Normal separation anxiety usually resolves by preschool age or is short-lived without significant impact on daily life.
*Irritable bowel syndrome*
- **Irritable bowel syndrome (IBS)** is a common cause of recurrent abdominal pain, but it is typically associated with **changes in bowel habits** (constipation or diarrhea), which are absent in this case.
- Furthermore, the child's other symptoms, such as **school refusal**, **sleep disturbances**, and **distress upon separation**, are not characteristic of IBS and point towards a psychological rather than purely gastrointestinal etiology.
*Conduct disorder*
- **Conduct disorder** involves a persistent pattern of **aggressive behavior**, **destruction of property**, **deceitfulness or theft**, and **serious rule violations**, none of which are described in this case.
- The child's symptoms are characterized by anxiety and emotional distress related to separation, not defiant or antisocial behavior.
Functional GI disorders US Medical PG Question 7: A 25-year-old woman presents with abdominal pain and discomfort for the past 3 days. She was diagnosed with irritable bowel syndrome (IBS) a couple of years ago, managed until recently with imipramine, psyllium, and loperamide. 5 days ago, because she had developed alternating diarrhea and constipation, bloating, and abdominal pain on her medication, she was started on alosetron. Her current temperature is 39.0°C (102.2°F), the heart rate is 115/min, the blood pressure is 90/60 mm Hg and the respiratory rate is 22/min. Abdominal examination shows diffuse tenderness to palpation with guarding but no rebound. Bowel sounds are hypoactive on auscultation. A fecal occult blood test is positive and laboratory tests show her white cell count to be 15,800/µL. Arterial blood gas (ABG) analysis reveals a metabolic acidosis. Which of the following is the most likely diagnosis in this patient?
- A. Perforated duodenal ulcer
- B. Pseudomembranous colitis
- C. Appendicitis
- D. Crohn’s disease
- E. Ischemic colitis (Correct Answer)
Functional GI disorders Explanation: ***Ischemic colitis***
- The patient's presentation with **abdominal pain**, **fever**, **tachycardia**, **hypotension**, **diffuse tenderness with guarding**, **positive fecal occult blood**, **leukocytosis**, and **metabolic acidosis** after starting **alosetron** is highly suggestive of ischemic colitis. Alosetron, a 5-HT3 antagonist, can cause severe constipation and, rarely, **ischemic colitis**.
- The **hypoactive bowel sounds** and signs of **systemic inflammatory response** (fever, tachycardia, leukocytosis) further support a diagnosis of ischemic bowel compromise leading to colitis.
*Perforated duodenal ulcer*
- A perforated duodenal ulcer typically presents with sudden onset, **severe, sharp epigastric pain** that rapidly generalizes, often with a rigid, board-like abdomen and **rebound tenderness**, which is not seen here.
- While it can cause peritonitis and systemic signs, the history of recent medication change and more diffuse abdominal tenderness points away from an isolated perforation.
*Pseudomembranous colitis*
- Pseudomembranous colitis is primarily associated with **Clostridium difficile infection**, often following antibiotic use, and typically presents with severe watery diarrhea, not necessarily with a metabolic acidosis or overt signs of ischemia as seen in this case.
- While it can cause abdominal pain and systemic symptoms, the acute onset with severe tenderness and shock-like picture makes ischemic colitis more likely given the drug history.
*Appendicitis*
- Appendicitis typically presents with **periumbilical pain** that migrates to the **right lower quadrant**, often with localized tenderness at McBurney's point and rebound tenderness.
- The patient's **diffuse abdominal tenderness**, associated with such severe systemic symptoms and a history of specific medication use, is inconsistent with typical appendicitis.
*Crohn’s disease*
- Crohn's disease is a **chronic inflammatory bowel condition** characterized by transmural inflammation, often with intermittent abdominal pain, diarrhea, and weight loss, but it is less likely to present acutely with such severe, systemic signs and shock-like features without a clear exacerbating factor like acute ischemia.
- While Crohn's can cause complications like strictures or fistulas, an acute presentation resembling ischemic colitis with a clear provoking drug history is less common for an initial severe flare.
Functional GI disorders US Medical PG Question 8: A 58-year-old man presents to the Emergency Department after 3 hours of intense suprapubic pain associated with inability to urinate for the past day or two. His medical history is relevant for benign prostatic hyperplasia (BPH) that has been under treatment with prazosin and tadalafil. Upon admission, he is found to have a blood pressure of 180/100 mm Hg, a pulse of 80/min, a respiratory rate of 23/min, and a temperature of 36.5°C (97.7°F). He weighs 84 kg (185.1 lb) and is 175 cm (5 ft 7 in) tall. Physical exam, he has suprapubic tenderness. A bladder scan reveals 700 ml of urine. A Foley catheter is inserted and the urine is drained. Initial laboratory tests and their follow up 8 hours after admission are shown below.
Admission 8 hours after admission
Serum potassium 4.2 mmol/L Serum potassium 4.0 mmol/L
Serum sodium 140 mmol/L Serum sodium 142 mmol/L
Serum chloride 102 mmol/L Serum chloride 110 mmol/L
Serum creatinine 1.4 mg/dL Serum creatinine 1.6 mg/dL
Serum blood urea nitrogen 64 mg/dL Serum blood urea nitrogen 62 mg/dL
Urine output 250 mL Urine output 260 mL
A senior attending suggests a consultation with Nephrology. Which of the following best justifies this suggestion?
- A. Estimated glomerular filtration rate (eGFR)
- B. Urine output (Correct Answer)
- C. Serum creatinine (SCr)
- D. Serum blood urea nitrogen (BUN)
- E. Serum potassium
Functional GI disorders Explanation: ***Urine output***
- The patient's **urine output is severely reduced** at 260 mL over 8 hours (approximately **32.5 mL/hour**), which constitutes **oliguria** (defined as <0.5 mL/kg/hr; this patient at 84 kg should produce ≥42 mL/hr).
- Despite **relief of the post-renal obstruction** via Foley catheterization, the persistent oliguria indicates **intrinsic kidney injury** rather than simple mechanical obstruction.
- The combination of **oliguria persisting after decompression** + **rising serum creatinine** (1.4→1.6 mg/dL) meets **KDIGO criteria for Stage 2 AKI** (urine output <0.5 mL/kg/hr for ≥12 hours).
- This requires **urgent nephrology consultation** to assess for acute tubular necrosis (ATN), guide fluid management during potential post-obstructive diuresis, and consider renal replacement therapy if oliguria worsens.
*Serum creatinine (SCr)*
- The serum creatinine **rose from 1.4 to 1.6 mg/dL** despite bladder decompression, which is concerning and suggests intrinsic renal injury.
- However, creatinine is a **lagging indicator** of kidney function - it takes 24-48 hours to reflect acute changes in GFR, whereas **urine output is a real-time indicator** of kidney function.
- While the rising creatinine supports the need for nephrology involvement, **urine output is the more immediate and actionable parameter** that prompted the attending's suggestion at this early time point.
*Estimated glomerular filtration rate (eGFR)*
- eGFR is **calculated from serum creatinine** using equations that assume steady-state conditions, which **do not apply in acute kidney injury**.
- In the **acute setting with rapidly changing kidney function**, eGFR calculations are unreliable and can significantly overestimate or underestimate true GFR.
- Clinicians rely more on **urine output and serial creatinine measurements** rather than eGFR when managing AKI.
*Serum blood urea nitrogen (BUN)*
- The BUN decreased slightly from 64 to 62 mg/dL, remaining elevated but showing minimal change after catheterization.
- Elevated BUN can reflect **pre-renal azotemia, dehydration, or upper GI bleeding** and is less specific for intrinsic kidney injury than oliguria.
- The **BUN:Cr ratio** is approximately 40:1 (64/1.6), suggesting a **pre-renal component**, but this alone doesn't justify urgent nephrology consultation as strongly as the persistent oliguria does.
*Serum potassium*
- Serum potassium levels remain **normal** (4.2→4.0 mmol/L) and do not indicate a metabolic emergency.
- While **hyperkalemia** is a common complication of AKI that would warrant nephrology involvement, this patient's potassium is well-controlled and not the driving concern at this time.
Functional GI disorders US Medical PG Question 9: A 42-year-old woman presents for a follow-up visit. She was diagnosed with iron deficiency anemia 3 months ago, for which she was prescribed ferrous sulfate twice daily. She says the medication has not helped, and she still is suffering from fatigue and shortness of breath when she exerts herself. Past medical history is remarkable for chronic dyspepsia. The patient denies smoking, drinking alcohol, or use of illicit drugs. She immigrated from Egypt 4 years ago. No significant family history. Physical examination is unremarkable. Laboratory findings are significant for the following:
3 month ago Current
Hemoglobin 10.1 g/dL 10.3 g/dL
Erythrocyte count 3.2 million/mm3 3.3 million/mm3
Mean corpuscular volume (MCV) 72 μm3 74 μm3
Mean corpuscular hemoglobin (MCH) 20.1 pg/cell 20.3 pg/cell
Red cell distribution width (RDW) 17.2% 17.1%
Serum ferritin 10.1 ng/mL 10.3 ng/mL
Total iron binding capacity (TIBC) 475 µg/dL 470 µg/dL
Transferrin saturation 11% 12%
Which of the following is the next best step in the management of this patient’s most likely condition?
- A. Helicobacter pylori fecal antigen
- B. Bone marrow biopsy
- C. Hemoglobin electrophoresis
- D. Gastrointestinal endoscopy (Correct Answer)
- E. Fecal occult blood tests
Functional GI disorders Explanation: ***Gastrointestinal endoscopy***
- In adults with **iron deficiency anemia refractory to oral supplementation**, the next best step is **upper GI endoscopy (EGD)** to investigate for sources of chronic blood loss and rule out malignancy.
- This patient has persistent microcytic anemia despite 3 months of iron therapy, with classic laboratory findings of iron deficiency (low ferritin, high TIBC, low transferrin saturation).
- **Key indications for endoscopy**: chronic dyspepsia + refractory iron deficiency anemia in an adult patient.
- Endoscopy allows **direct visualization** of the upper GI tract, identification of bleeding sources (ulcers, gastritis, malignancy), and **biopsy for H. pylori** testing and histopathology.
- While H. pylori infection is a reasonable consideration given her chronic dyspepsia and origin from an endemic region, endoscopy provides more comprehensive evaluation and addresses the critical need to **exclude gastric or esophageal malignancy**.
*Helicobacter pylori fecal antigen*
- Non-invasive H. pylori testing is reasonable for patients with dyspepsia under age 60 in low-risk populations (test-and-treat strategy).
- However, in the setting of **refractory iron deficiency anemia**, this approach is insufficient as it would miss other important causes of GI blood loss including **malignancy, erosive gastritis, celiac disease**, and vascular lesions.
- H. pylori testing can be performed during endoscopy via biopsy or rapid urease test, making separate fecal antigen testing unnecessary.
*Bone marrow biopsy*
- This is an **invasive procedure** reserved for investigating unexplained cytopenias, suspected bone marrow failure, or hematologic malignancies.
- The laboratory findings clearly indicate **iron deficiency** (low ferritin, high TIBC), not a primary bone marrow disorder, making biopsy unnecessary at this stage.
*Fecal occult blood tests*
- While screening for GI bleeding is important in iron deficiency anemia, **fecal occult blood testing has poor sensitivity** for upper GI lesions and intermittent bleeding.
- Given the lack of response to iron therapy, a more definitive diagnostic approach with **direct visualization** is warranted rather than indirect testing.
- Negative fecal occult blood does not exclude significant GI pathology.
*Hemoglobin electrophoresis*
- This test identifies **hemoglobinopathies** such as thalassemia trait, which can cause microcytic anemia.
- However, the patient's **low serum ferritin (10.3 ng/mL)** and **high TIBC (470 µg/dL)** are pathognomonic for iron deficiency, not thalassemia.
- In thalassemia trait, ferritin and TIBC would typically be normal, and the MCV would be disproportionately low relative to the degree of anemia.
- While hemoglobin electrophoresis could be considered if iron studies were normal, it is not indicated here.
Functional GI disorders US Medical PG Question 10: A 55-year-old man presents to urgent care for weakness and weight loss. He states for the past several months he has felt progressively weaker and has lost 25 pounds. The patient also endorses intermittent abdominal pain. The patient has not seen a physician in 30 years and recalls being current on most of his vaccinations. He says that a few years ago, he went to the emergency department due to abdominal pain and was found to have increased liver enzymes due to excessive alcohol use and incidental gallstones. The patient has a 50 pack-year smoking history. His temperature is 99.5°F (37.5°C), blood pressure is 161/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 95% on room air. Physical exam reveals an emaciated man. The patient has a negative Murphy's sign and his abdomen is non-tender. Cardiopulmonary exam is within normal limits. Which of the following is the next best step in management?
- A. CT scan of the abdomen (Correct Answer)
- B. CT scan of the liver
- C. Right upper quadrant ultrasound
- D. HIDA scan
- E. Smoking cessation advice and primary care follow up
Functional GI disorders Explanation: ***CT scan of the abdomen***
- The patient presents with **constitutional symptoms** (weakness, significant weight loss), **intermittent abdominal pain**, and a **50 pack-year smoking history**, which are red flags for potential **malignancy**.
- A CT scan of the abdomen is the most appropriate initial imaging study to **evaluate for masses, metastases, or other pathologies** that would explain these symptoms comprehensively.
*CT scan of the liver*
- While the patient has a history of elevated liver enzymes and gallstones, focusing solely on the liver might **miss other abdominal pathologies** that could explain his symptoms.
- A CT of the liver is a more targeted scan, usually performed after a broader abdominal assessment suggests a primary liver issue.
*Right upper quadrant ultrasound*
- An ultrasound of the right upper quadrant is excellent for evaluating the **gallbladder, bile ducts, and liver parenchyma** for stones, cholecystitis, or focal lesions.
- However, it has **limited ability to visualize the retroperitoneum, pancreas, or other bowel structures** which could be the source of the patient's symptoms.
*HIDA scan*
- A HIDA scan is used to assess **gallbladder function** and is primarily indicated for suspected **acute cholecystitis** when ultrasound findings are equivocal, or for chronic gallbladder dysfunction.
- The patient's presentation of generalized weakness, significant weight loss, and non-tender abdomen does not acutely point towards biliary obstruction or acute cholecystitis.
*Smoking cessation advice and primary care follow up*
- While **smoking cessation** is crucial for long-term health, and **primary care follow-up** is necessary, these steps are not the *next best step in management* for a patient presenting with alarming symptoms of weakness, significant weight loss, and abdominal pain.
- These are important secondary measures, but the immediate concern is to **investigate the cause of his current severe symptoms**.
More Functional GI disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.