Diverticular disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diverticular disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diverticular disease US Medical PG Question 1: A 62-year-old man presents to the emergency department with acute pain in the left lower abdomen and profuse rectal bleeding. These symptoms started 3 hours ago. The patient has chronic constipation and bloating, for which he takes lactulose. His family history is negative for gastrointestinal disorders. His temperature is 38.2°C (100.8°F), blood pressure is 90/60 mm Hg, and pulse is 110/min. On physical examination, the patient appears drowsy, and there is tenderness with guarding in the left lower abdominal quadrant. Flexible sigmoidoscopy shows multiple, scattered diverticula with acute mucosal inflammation in the sigmoid colon. Which of the following is the best initial treatment for this patient?
- A. Elective colectomy
- B. Dietary modification and antibiotics
- C. Volume replacement, analgesia, intravenous antibiotics, and endoscopic hemostasis
- D. Volume replacement, analgesia, intravenous antibiotics, and surgical hemostasis (Correct Answer)
- E. Reassurance and no treatment is required
Diverticular disease Explanation: ***Volume replacement, analgesia, intravenous antibiotics, and surgical hemostasis***
- This patient presents with **acute complicated diverticulitis** with signs of **peritonitis** (left lower abdominal pain with guarding) and **septic shock** (fever 38.2°C, hypotension 90/60 mm Hg, tachycardia 110/min, drowsiness).
- Initial management requires **volume replacement** to address hypovolemia and shock, **analgesia** for pain control, and **broad-spectrum intravenous antibiotics** covering gram-negative and anaerobic organisms.
- The presence of **peritonitis with hemodynamic instability** indicates complicated diverticulitis requiring **surgical intervention** (typically sigmoid resection with colostomy - Hartmann procedure) after initial resuscitation.
- While the patient has rectal bleeding, the dominant clinical picture is **perforation/transmural inflammation** requiring surgery, not just bleeding control.
*Volume replacement, analgesia, intravenous antibiotics, and endoscopic hemostasis*
- **Endoscopic hemostasis** is appropriate for uncomplicated diverticular bleeding without signs of perforation or peritonitis.
- In this case, the patient has **guarding** (indicating peritonitis) and **septic shock**, suggesting transmural inflammation or perforation that cannot be managed endoscopically.
- Endoscopy is relatively contraindicated in acute diverticulitis with peritonitis due to risk of worsening perforation.
*Elective colectomy*
- While colectomy is the correct surgical approach, the term **"elective"** is inappropriate for this acute, life-threatening emergency.
- This patient requires **urgent/emergency surgery** after initial resuscitation, not scheduled elective surgery.
*Dietary modification and antibiotics*
- **Dietary modification** (high-fiber diet) is a preventive strategy for uncomplicated diverticular disease, not treatment for acute complicated diverticulitis.
- While antibiotics are necessary, this option fails to address the **septic shock, hypovolemia, and need for surgical intervention** in complicated diverticulitis with peritonitis.
*Reassurance and no treatment is required*
- The patient exhibits **life-threatening complications**: septic shock, peritonitis, and hemodynamic instability.
- **No treatment** would result in rapid deterioration, multi-organ failure, and death.
Diverticular disease US Medical PG Question 2: A 46-year-old woman comes to the emergency department because of intermittent abdominal pain and vomiting for 2 days. The abdominal pain is colicky and diffuse. The patient's last bowel movement was 3 days ago. She has had multiple episodes of upper abdominal pain that radiates to her scapulae and vomiting over the past 3 months; her symptoms subsided after taking ibuprofen. She has coronary artery disease, type 2 diabetes mellitus, gastroesophageal reflux disease, and osteoarthritis of both knees. Current medications include aspirin, atorvastatin, rabeprazole, insulin, and ibuprofen. She appears uncomfortable. Her temperature is 39°C (102.2°F), pulse is 111/min, and blood pressure is 108/68 mm Hg. Examination shows dry mucous membranes. The abdomen is distended and tympanitic with diffuse tenderness; bowel sounds are high-pitched. Rectal examination shows a collapsed rectum. Her hemoglobin concentration is 13.8 g/dL, leukocyte count is 14,400/mm3, and platelet count is 312,000/mm3. An x-ray of the abdomen is shown. Which of the following is the most likely cause of this patient's findings?
- A. Cecal torsion
- B. Viscus perforation
- C. Colonic diverticular inflammation
- D. Cholecystoenteric fistula (Correct Answer)
- E. Bowel infarction
Diverticular disease Explanation: ***Cholecystoenteric fistula***
- The patient's history of recurrent upper abdominal pain radiating to the scapula, responsive to NSAIDs, is highly suggestive of **biliary colic** due to **cholelithiasis**.
- The diffuse colicky pain, vomiting, distended abdomen with high-pitched bowel sounds, and particularly the **pneumobilia** (air in the biliary tree, visible as branching lucency in the hepatic area on X-ray, indicated by red arrows) along with signs of **small bowel obstruction** (dilated small bowel loops and air-fluid levels, indicated by green arrows), are classic features of **gallstone ileus** resulting from a cholecystoenteric fistula.
*Cecal torsion*
- While cecal torsion can cause a large bowel obstruction with colicky pain and distension, it typically presents with a **dilated cecum** and a characteristic "coffee-bean" appearance on X-ray, often without pneumobilia.
- The history of recurrent biliary pain and the presence of pneumobilia are not typical for cecal torsion.
*Viscus perforation*
- A viscus perforation would likely cause **sudden, severe onset abdominal pain**, signs of peritonitis, and usually **free air under the diaphragm** on an upright chest X-ray.
- While the patient has diffuse tenderness, the X-ray findings do not show free intraperitoneal air; instead, they show pneumobilia and small bowel obstruction.
*Colonic diverticuli inflammation*
- **Diverticulitis** typically presents with **left lower quadrant pain**, fever, and changes in bowel habits, though diffuse pain can occur with complications.
- It does not explain the history of recurrent upper abdominal pain radiating to the scapula or the radiologic findings of pneumobilia and small bowel obstruction.
*Bowel infarction*
- Bowel infarction often presents with **severe, disproportionate abdominal pain** (pain out of proportion to exam findings), bloody diarrhea, and signs of sepsis.
- While the patient has some signs of systemic inflammation (fever, leukocytosis), the X-ray findings of pneumobilia and typical small bowel obstruction, without signs of portal venous gas or extensive bowel wall thickening, make infarction less likely as the primary cause.
Diverticular disease US Medical PG Question 3: A 75-year-old man presents to the emergency department for abdominal pain. The patient states the pain started this morning and has been worsening steadily. He decided to come to the emergency department when he began vomiting. The patient has a past medical history of obesity, diabetes, alcohol abuse, and hypertension. His current medications include captopril, insulin, metformin, sodium docusate, and ibuprofen. His temperature is 104.0°F (40°C), blood pressure is 160/97 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Abdominal exam reveals left lower quadrant tenderness. Cardiac exam reveals a crescendo systolic murmur heard best by the right upper sternal border. Lab values are ordered and return as below.
Hemoglobin: 15 g/dL
Hematocrit: 42%
Leukocyte count: 19,500 cells/mm^3 with normal differential
Platelet count: 226,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 144 mg/dL
Creatinine: 1.2 mg/dL
Ca2+: 9.8 mg/dL
Which of the following is the most accurate test for this patient's condition?
- A. Colonoscopy
- B. Sigmoidoscopy
- C. Amylase and lipase levels
- D. Barium enema
- E. CT scan (Correct Answer)
Diverticular disease Explanation: ***CT scan***
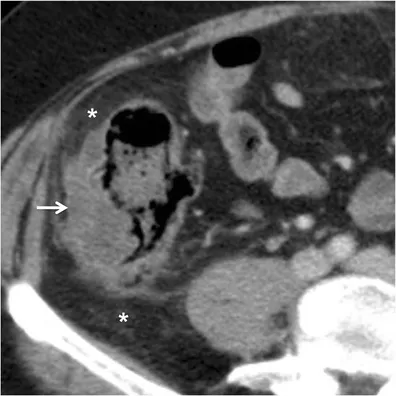
- The patient presents with classic symptoms of **diverticulitis**, including **left lower quadrant pain**, **fever**, and **leukocytosis**. A **CT scan with oral and IV contrast** is the most accurate diagnostic test to identify diverticular inflammation, abscess formation, or perforation.
- A CT scan can also help rule out other causes of abdominal pain and guide further management, such as the need for percutaneous drainage of an abscess.
*Colonoscopy*
- **Colonoscopy is contraindicated during an acute episode of diverticulitis** due to the risk of **perforation** of an inflamed colon.
- It may be considered **6-8 weeks after resolution of acute diverticulitis** to investigate for other pathologies such as malignancy.
*Sigmoidoscopy*
- Similar to colonoscopy, **sigmoidoscopy is generally avoided in acute diverticulitis** because of the risk of **perforation** of the inflamed bowel from instrumentation.
- Its diagnostic yield in acute settings is also limited compared to CT imaging.
*Amylase and lipase levels*
- These tests are primarily used to diagnose **pancreatitis**, which typically presents with **epigastric pain radiating to the back**, often associated with elevated enzyme levels.
- While vomiting is present, the **left lower quadrant tenderness and fever** point away from pancreatitis as the primary diagnosis.
*Barium enema*
- **Barium enema is generally contraindicated in acute diverticulitis** due to the risk of **perforation** and the introduction of barium into the peritoneum, which can cause severe peritonitis.
- It has largely been replaced by **CT scanning** for its superior safety profile and diagnostic accuracy in acute abdominal conditions.
Diverticular disease US Medical PG Question 4: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Diverticular disease Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
Diverticular disease US Medical PG Question 5: A 24-year-old man presents to the emergency department for severe abdominal pain for the past day. The patient states he has had profuse, watery diarrhea and abdominal pain that is keeping him up at night. The patient also claims that he sees blood on the toilet paper when he wipes and endorses having lost 5 pounds recently. The patient's past medical history is notable for IV drug abuse and a recent hospitalization for sepsis. His temperature is 99.5°F (37.5°C), blood pressure is 120/68 mmHg, pulse is 100/min, respirations are 14/min, and oxygen saturation is 98% on room air. On physical exam, you note a young man clutching his abdomen in pain. Abdominal exam demonstrates hyperactive bowel sounds and diffuse abdominal tenderness. Cardiopulmonary exam is within normal limits. Which of the following is the next best step in management?
- A. Vancomycin (Correct Answer)
- B. Mesalamine enema
- C. Metronidazole
- D. Clindamycin
- E. Supportive therapy and ciprofloxacin if symptoms persist
Diverticular disease Explanation: ***Vancomycin***
- The patient's history of **IV drug abuse**, recent **hospitalization for sepsis**, and severe abdominal symptoms with **bloody diarrhea** and **weight loss** are highly suggestive of **Clostridioides difficile infection (CDI)**.
- **Oral vancomycin** is the recommended first-line treatment for **severe C. difficile infection**, especially with signs like systemic illness (tachycardia) and marked abdominal tenderness.
*Mesalamine enema*
- **Mesalamine** is an **anti-inflammatory drug** primarily used for **mild to moderate ulcerative colitis**, particularly when the disease is limited to the rectum or rectosigmoid colon.
- While inflammatory bowel disease can cause bloody diarrhea, the acute presentation with recent hospitalization and IV drug use makes **infectious etiologies**, particularly CDI, much more likely.
*Metronidazole*
- **Metronidazole** is an antibiotic that was previously used for uncomplicated **C. difficile infection**.
- However, **oral vancomycin** is now preferred for **initial CDI episodes** due to superior efficacy, especially in severe cases, and metronidazole is generally reserved for non-severe cases if vancomycin is unavailable or not tolerated.
*Clindamycin*
- **Clindamycin** is an antibiotic notorious for being a common cause of **antibiotic-associated C. difficile infection**.
- Giving clindamycin in this scenario would likely **worsen the patient's condition** if C. difficile is indeed the cause, as it promotes C. difficile overgrowth.
*Supportive therapy and ciprofloxacin if symptoms persist*
- While **supportive care** (hydration, electrolyte management) is essential, it is **insufficient as the sole treatment** for severe C. difficile infection.
- **Ciprofloxacin** is an antibiotic that is **ineffective against C. difficile** and could potentially exacerbate the infection by disrupting the normal gut microbiota.
Diverticular disease US Medical PG Question 6: A 65-year-old man comes to the physician because of abdominal pain and bloody, mucoid diarrhea for 3 days. He has been taking over-the-counter supplements for constipation over the past 6 months. He was diagnosed with type 2 diabetes mellitus 15 years ago. He has smoked one pack of cigarettes daily for 35 years. His current medications include metformin. His temperature is 38.4°C (101.1°F), pulse is 92/min, and blood pressure is 134/82 mm Hg. Examination of the abdomen shows no masses. Palpation of the left lower abdomen elicits tenderness. A CT scan of the abdomen is shown. Which of the following is the most likely underlying cause of the patient's condition?
- A. Focal weakness of the colonic muscularis layer (Correct Answer)
- B. Twisting of the sigmoid colon around its mesentery
- C. Transmural inflammation of the terminal ileum
- D. Infiltrative growth in the descending colon
- E. Decreased perfusion to mesenteric blood vessel
Diverticular disease Explanation: **Focal weakness of the colonic muscularis layer**
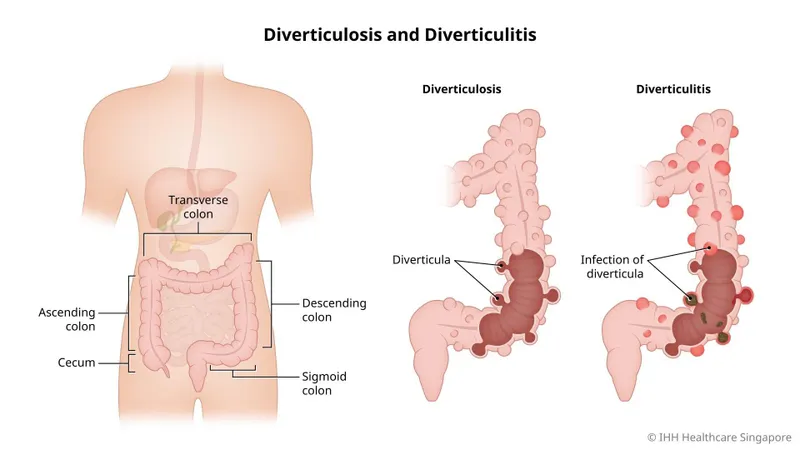
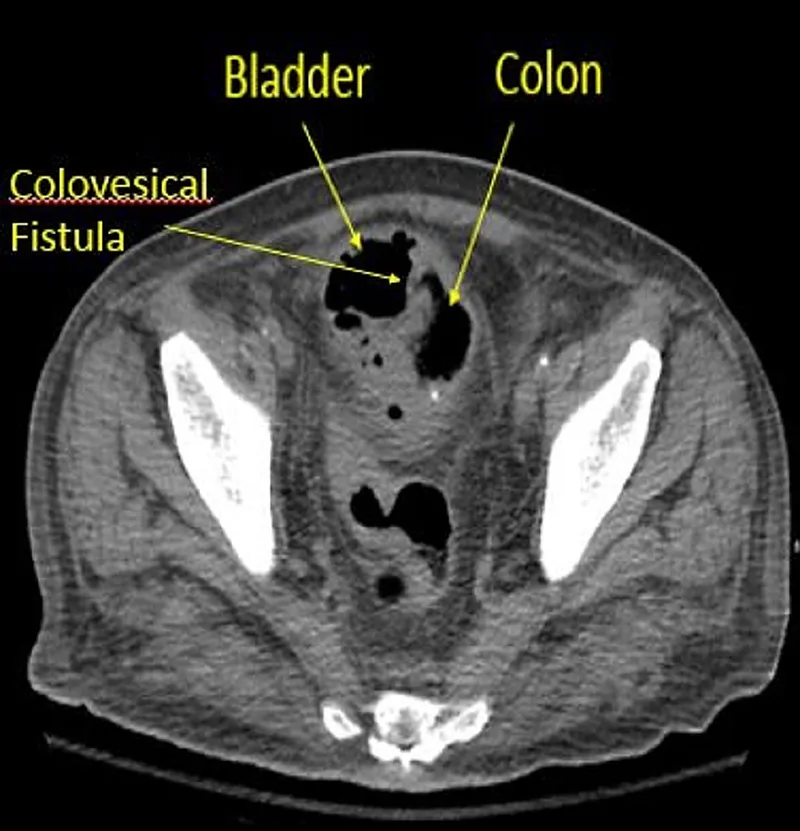
- The patient's symptoms of **abdominal pain**, **bloody, mucoid diarrhea**, and **left lower abdominal tenderness** are classic for **diverticulitis**, which occurs when small pouches (diverticula) in the colon become inflamed or infected. Diverticula form due to **focal weakness in the colonic muscularis layer**, often at points where blood vessels penetrate the muscle wall.
- **Constipation** and a history of **smoking** are risk factors for diverticular disease, contributing to increased intraluminal pressure and the formation of diverticula.
*Twisting of the sigmoid colon around its mesentery*
- This describes a **sigmoid volvulus**, which presents with acute onset of **severe abdominal pain**, distension, and obstipation (complete absence of stool and gas).
- While a volvulus can cause bloody stools due to ischemia, the clinical presentation and likely CT findings (not provided, but inferred to show diverticula) are inconsistent with this condition, and the described symptoms point more towards inflammation.
*Transmural inflammation of the terminal ileum*
- This suggests **Crohn's disease**, which can cause abdominal pain and diarrhea. However, Crohn's disease typically affects the **terminal ileum** and has a more chronic course, often with weight loss, perianal disease, and extraintestinal manifestations.
- Bloody, mucoid diarrhea is less typical for Crohn's unless there is severe colonic involvement, and the acute onset and tenderness in the left lower quadrant point away from isolated terminal ileitis.
*Infiltrative growth in the descending colon*
- An **infiltrative growth** (e.g., colorectal cancer) can cause changes in bowel habits, abdominal pain, and bloody stools. However, it usually presents with more **chronic symptoms** and weight loss.
- The acute inflammatory picture presented (fever, tenderness, mucoid diarrhea) is less characteristic of an uncomplicated infiltrative growth without obstruction or perforation.
*Decreased perfusion to mesenteric blood vessel*
- This describes **ischemic colitis**, which causes acute abdominal pain, bloody diarrhea, and tenderness. While it's a possibility, especially in older patients with vascular risk factors (diabetes, smoking), the description of **mucoid diarrhea** and the strong association with a history of constipation and symptoms pointing to localized inflammation (tenderness in left lower abdomen suggesting sigmoid/descending colon involvement) make **diverticulitis** a more likely primary cause in this context unless imaging strongly suggests ischemia.
- Ischemic colitis often presents with more severe, diffuse abdominal pain often out of proportion to physical exam findings initially.
Diverticular disease US Medical PG Question 7: Please refer to the summary above to answer this question
Which of the following is the most likely diagnosis?
Patient information
Age: 61 years
Gender: F, self-identified
Ethnicity: unspecified
Site of care: emergency department
History
Reason for Visit/Chief Concern: "My belly really hurts."
History of Present Illness:
developed abdominal pain 12 hours ago
pain constant; rated at 7/10
has nausea and has vomited twice
has had two episodes of nonbloody diarrhea in the last 4 hours
12-month history of intermittent constipation
reports no sick contacts or history of recent travel
Past medical history:
hypertension
type 2 diabetes mellitus
mild intermittent asthma
allergic rhinitis
Social history:
diet consists mostly of high-fat foods
does not smoke
drinks 1–2 glasses of wine per week
does not use illicit drugs
Medications:
lisinopril, metformin, albuterol inhaler, fexofenadine, psyllium husk fiber
Allergies:
no known drug allergies
Physical Examination
Temp Pulse Resp. BP O2 Sat Ht Wt BMI
38.4°C
(101.1°F)
85/min 16/min 134/85 mm Hg –
163 cm
(5 ft 4 in)
94 kg
(207 lb)
35 kg/m2
Appearance: lying back in a hospital bed; appears uncomfortable
Neck: no jugular venous distention
Pulmonary: clear to auscultation; no wheezes, rales, or rhonchi
Cardiac: regular rate and rhythm; normal S1 and S2; no murmurs, rubs, or gallops
Abdominal: obese; soft; tender to palpation in the left lower quadrant; no guarding or rebound tenderness; normal bowel sounds
Extremities: no edema; warm and well-perfused
Skin: no rashes; dry
Neurologic: alert and oriented; cranial nerves grossly intact; no focal neurologic deficits
- A. Cholecystitis
- B. Crohn disease
- C. Diverticulitis (Correct Answer)
- D. Appendicitis
- E. Irritable bowel syndrome
Diverticular disease Explanation: ***Diverticulitis***
- The patient's presentation of acute **left lower quadrant abdominal pain**, fever (38.4°C), nausea, vomiting, and a history of intermittent constipation is highly suggestive of diverticulitis.
- Her obesity (BMI 35 kg/m2) and diet consisting mostly of high-fat foods are also **risk factors** for diverticular disease.
*Cholecystitis*
- This condition typically causes acute pain in the **right upper quadrant** of the abdomen, sometimes radiating to the right shoulder, which is inconsistent with the patient's left lower quadrant pain.
- While nausea and vomiting can occur, the localization of pain is a key differentiator.
*Crohn disease*
- Crohn disease usually presents with **chronic abdominal pain**, weight loss, fatigue, and persistent diarrhea, often with blood.
- The acute, localized pain with fever and recent constipation followed by non-bloody diarrhea does not fit the typical presentation of an acute flare of Crohn disease, though it can occur anywhere in the GI tract.
*Appendicitis*
- Acute appendicitis almost universally presents with pain that localizes to the **right lower quadrant** (McBurney's point), initially periumbilical.
- The patient's pain is clearly localized to the left lower quadrant, ruling out appendicitis.
*Irritable bowel syndrome*
- While IBS can cause recurrent abdominal pain, constipation, and diarrhea, it is a **functional disorder** and does not typically involve fever or a localized, acute inflammatory process as seen in this patient.
- The acute presentation with fever and severe, localized pain points away from IBS.
Diverticular disease US Medical PG Question 8: A 68-year-old female presents to your office for her annual check-up. Her vitals are HR 85, T 98.8 F, RR 16, BP 125/70. She has a history of smoking 1 pack a day for 35 years, but states she quit five years ago. She had her last pap smear at age 64 and states all of her pap smears have been normal. She had her last colonoscopy at age 62, which was also normal. Which of the following is the next best test for this patient?
- A. Pap smear
- B. Chest radiograph
- C. Abdominal ultrasound
- D. Colonoscopy
- E. Chest CT scan (Correct Answer)
Diverticular disease Explanation: ***Chest CT scan***
- This patient is a 68-year-old female with a **35-pack-year smoking history** who quit 5 years ago, placing her in a high-risk group for lung cancer.
- **Low-dose computed tomography (LDCT)** for lung cancer screening is recommended annually for individuals aged 50-80 with a 20-pack-year smoking history who currently smoke or have quit within the past 15 years.
*Pap smear*
- A Pap smear is not indicated as she had her last one at age 64 and all previous results were normal.
- Guidelines recommend discontinuing Pap smears at age 65 if there is no history of moderate or severe dysplasia and three consecutive negative results within the last 10 years.
*Chest radiograph*
- A chest radiograph is a less sensitive and specific tool for detecting early lung cancer compared to LDCT.
- It misses a significant proportion of early-stage lung cancers and is not recommended for lung cancer screening.
*Abdominal ultrasound*
- An abdominal ultrasound is generally used to screen for conditions like abdominal aortic aneurysm in specific high-risk populations (males 65-75 who have ever smoked).
- There is no indication from the provided history for an abdominal ultrasound in this patient.
*Colonoscopy*
- This patient had a normal colonoscopy at age 62.
- Current guidelines recommend repeating colonoscopy every 10 years if the previous one was normal, so she is not due for another one yet.
Diverticular disease US Medical PG Question 9: A 65-year-old man presents to his primary care physician for a yearly checkup. He states he feels he has been in good health other than minor fatigue, which he attributes to aging. The patient has a past medical history of hypertension and is currently taking chlorthalidone. He drinks 1 glass of red wine every night. He has lost 5 pounds since his last appointment 4 months ago. His temperature is 99.2°F (37.3°C), blood pressure is 147/98 mmHg, pulse is 80/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam reveals an obese man in no acute distress. Laboratory values are ordered as seen below.
Hemoglobin: 9 g/dL
Hematocrit: 27%
Mean corpuscular volume: 72 µm^3
Leukocyte count: 6,500/mm^3 with normal differential
Platelet count: 193,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 9.0 mg/dL
AST: 32 U/L
ALT: 20 U/L
25-OH vitamin D: 15 ng/mL
Which of the following is the best next step in management?
- A. Counseling for alcohol cessation
- B. Vitamin D supplementation
- C. Colonoscopy (Correct Answer)
- D. Exercise regimen and weight loss
- E. Iron supplementation
Diverticular disease Explanation: ***Colonoscopy***
- The patient presents with **microcytic anemia** (hemoglobin 9 g/dL, MCV 72 µm^3) and **unexplained weight loss** in an elderly male, which is highly suggestive of **gastrointestinal bleeding**, often due to **colorectal cancer**.
- A **colonoscopy** is the definitive diagnostic and therapeutic procedure for evaluating the lower gastrointestinal tract for sources of bleeding and identifying/removing suspicious lesions.
*Counseling for alcohol cessation*
- While chronic alcohol use can contribute to various health issues, including some anemias (e.g., folate deficiency), the patient's presented **microcytic anemia** is not typical for alcohol-related causes.
- The patient's reported alcohol intake of one glass of red wine nightly is generally considered moderate and less likely to be the primary cause of his symptoms and lab findings.
*Vitamin D supplementation*
- The patient has a **low 25-OH vitamin D level (15 ng/mL)**. However, this finding, while important for bone health and overall well-being, does not explain his microcytic anemia or unexplained weight loss.
- Addressing the **anemia and weight loss** takes precedence as these symptoms point to a more urgent, potentially life-threatening condition.
*Exercise regimen and weight loss*
- The patient is obese and has hypertension, for which an **exercise regimen and weight loss** would be beneficial for overall health and blood pressure management.
- However, these interventions **do not address the microcytic anemia and unexplained weight loss**, which are more pressing concerns requiring immediate investigation.
*Iron supplementation*
- The **microcytic anemia** strongly suggests **iron deficiency**, and iron supplementation would eventually be part of treatment.
- However, **iron supplementation** without identifying and treating the underlying cause of iron loss (e.g., gastrointestinal bleeding) would be insufficient and could delay a crucial diagnosis.
Diverticular disease US Medical PG Question 10: A 26-year-old white man comes to the physician because of increasing generalized fatigue for 6 months. He has been unable to work out at the gym during this period. He has also had cramping lower abdominal pain and diarrhea for the past 5 weeks that is occasionally bloody. His father was diagnosed with colon cancer at the age of 65. He has smoked half a pack of cigarettes daily for the past 10 years. He drinks 1–2 beers on social occasions. His temperature is 37.3°C (99.1°F), pulse is 88/min, and blood pressure is 116/74 mm Hg. Physical examination shows dry mucous membranes. The abdomen is soft and nondistended with slight tenderness to palpation over the lower quadrants bilaterally. Rectal examination shows stool mixed with blood. His hemoglobin concentration is 13.5 g/dL, leukocyte count is 7,500/mm3, and platelet count is 480,000/mm3. Urinalysis is within normal limits. Which of the following is the most appropriate next step in management?
- A. D-xylose absorption test
- B. CT scan of the abdomen and pelvis with contrast
- C. Capsule endoscopy
- D. Colonoscopy (Correct Answer)
- E. Flexible sigmoidoscopy
Diverticular disease Explanation: ***Colonoscopy***
- The patient presents with **bloody diarrhea** and **lower abdominal pain**, which are classic symptoms of inflammatory bowel disease (IBD), particularly **Crohn's disease** or **ulcerative colitis**. A colonoscopy allows for direct visualization of the colonic and terminal ileal mucosa, **biopsy collection** for histological confirmation, and assessment of disease extent and severity.
- While the patient's hemoglobin is currently normal, the presence of bloody stools indicates potential ongoing blood loss, and the history of fatigue suggests chronic inflammation. **Colonoscopy is the gold standard** for diagnosing and differentiating types of IBD.
*D-xylose absorption test*
- This test is used to assess **small bowel mucosal function** and carbohydrate absorption, typically in cases of suspected malabsorption like **celiac disease**.
- While malabsorption can cause fatigue, the patient's primary symptoms of bloody diarrhea and abdominal pain are not typical for isolated malabsorption, and a d-xylose test would not identify the source of bleeding.
*CT scan of the abdomen and pelvis with contrast*
- A CT scan can identify **extraintestinal manifestations** of IBD, abscesses, or bowel wall thickening, but it is **less sensitive** than colonoscopy for direct mucosal evaluation and cannot obtain biopsies for definitive diagnosis.
- It might be considered after colonoscopy for assessing transmural involvement or complications but is not the initial diagnostic step for primary luminal symptoms.
*Capsule endoscopy*
- Capsule endoscopy is primarily used to evaluate the **small bowel** for lesions beyond the reach of standard upper endoscopy and colonoscopy, such as obscure GI bleeding or suspected Crohn's disease confined to the small bowel.
- Given the patient's symptoms of **lower abdominal pain** and bloody diarrhea, the pathology is likely in the colon or terminal ileum, making colonoscopy more appropriate for initial evaluation. A capsule endoscopy does not visualize the colon.
*Flexible sigmoidoscopy*
- A flexible sigmoidoscopy visualizes the **rectum and a portion of the sigmoid colon**, which might be affected in ulcerative colitis.
- However, it would miss lesions in the more proximal colon or terminal ileum, which are common sites for Crohn's disease and some forms of ulcerative colitis, thus potentially leading to an incomplete diagnosis.
More Diverticular disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.