Celiac disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Celiac disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Celiac disease US Medical PG Question 1: A 35-year-old Caucasian female presents with anemia, malaise, bloating, and diarrhea. Past genetic testing revealed that this patient carries the HLA-DQ2 allele. The physician suspects that the patient's presentation is dietary in cause. Which of the following findings would definitively confirm this diagnosis?
- A. CT scan showing inflammation of the small bowel wall
- B. Biopsy of the duodenum showing atrophy and blunting of villi (Correct Answer)
- C. Biopsy of the colon showing epithelial cell apoptosis
- D. Esophageal endoscopy showing lower esophageal metaplasia
- E. Liver biopsy showing apoptosis of hepatocytes
Celiac disease Explanation: ***Biopsy of the duodenum showing atrophy and blunting of villi***
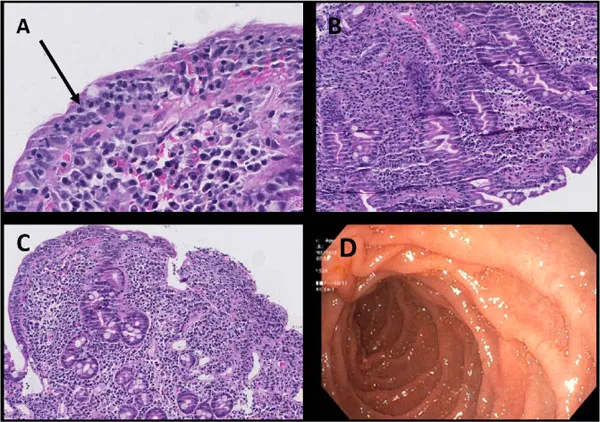
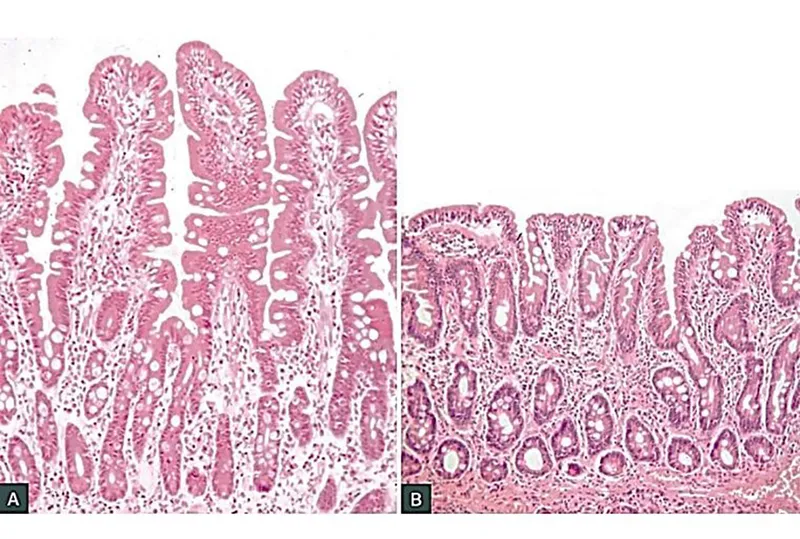
- This finding is the **gold standard** for diagnosing **celiac disease**, which aligns with the patient's symptoms (anemia, malaise, bloating, diarrhea), genetic predisposition (HLA-DQ2 allele), and suspected dietary cause.
- The characteristic **villous atrophy** and **crypt hyperplasia** seen in duodenal biopsies are hallmark pathological changes in celiac disease due to gluten exposure.
*CT scan showing inflammation of the small bowel wall*
- While a CT scan can show **inflammation**, it is not specific enough to definitively diagnose celiac disease, as many other conditions can cause small bowel inflammation.
- It does not provide the **histopathological detail** necessary to confirm villous atrophy, which is key for celiac diagnosis.
*Biopsy of the colon showing epithelial cell apoptosis*
- **Epithelial cell apoptosis** in the colon is not a primary diagnostic feature of celiac disease, which primarily affects the **small intestine**.
- This finding might be associated with other inflammatory bowel conditions or infections, not gluten-induced enteropathy.
*Esophageal endoscopy showing lower esophageal metaplasia*
- **Lower esophageal metaplasia**, or **Barrett's esophagus**, is a pre-cancerous condition of the esophagus, often caused by chronic acid reflux.
- This finding is unrelated to celiac disease and does not explain the patient's gastrointestinal symptoms or genetic predisposition.
*Liver biopsy showing apoptosis of hepatocytes*
- **Apoptosis of hepatocytes** (liver cell death) would indicate liver damage or disease, such as hepatitis or drug-induced injury.
- While celiac disease can sometimes have **hepatic manifestations**, liver apoptosis is not a primary or definitive diagnostic criterion for celiac disease itself.
Celiac disease US Medical PG Question 2: A 23-year-old man presents to the office complaining of weight loss and fatigue for the past 2 months. He states that he has been experiencing foul-smelling, light-colored stools but thinks it is because he hasn’t been eating well, recently. He has a past medical history significant for cystic fibrosis, which is well-controlled medically. He denies any shortness of breath, chest or abdominal pain, nausea, vomiting, or melena. On physical examination, his skin is pale and dry. Which of the following would be the most likely etiology of a malabsorption syndrome giving rise to this patient’s current condition?
- A. Decreased recycling of bile acids
- B. Pancreatic insufficiency (Correct Answer)
- C. Autoimmune damage to parietal cells
- D. Chronic damage to intestinal mucosa
- E. Damage to intestinal brush border
Celiac disease Explanation: ***Pancreatic insufficiency***
- Cystic fibrosis typically causes **exocrine pancreatic insufficiency** due to thick secretions blocking the pancreatic ducts, leading to malabsorption of fats and fat-soluble vitamins.
- **Foul-smelling, light-colored stools** (steatorrhea) are a classic symptom of fat malabsorption resulting from inadequate lipase production.
*Decreased recycling of bile acids*
- This typically results in **fat malabsorption**, but it is commonly associated with diseases affecting the **terminal ileum** (e.g., Crohn's disease, resection).
- While it can cause steatorrhea, it is not the primary or most common cause of malabsorption in cystic fibrosis.
*Autoimmune damage to parietal cells*
- This condition leads to **pernicious anemia** due to a lack of intrinsic factor and subsequent **vitamin B12 malabsorption**.
- It does not typically cause **steatorrhea** or generalized fat malabsorption, and it is not directly associated with cystic fibrosis.
*Chronic damage to intestinal mucosa*
- This points towards conditions like **celiac disease** or severe inflammatory bowel disease, which impair nutrient absorption through mucosal injury.
- While cystic fibrosis can have gastrointestinal manifestations, primary mucosal damage is not the leading cause of malabsorption, and the patient's symptoms are more consistent with fat malabsorption.
*Damage to intestinal brush border*
- This is characteristic of conditions like **lactase deficiency** or **celiac disease**, which affect the absorption of specific nutrients (e.g., carbohydrates).
- While it causes malabsorption, the patient's presentation with **steatorrhea** points more specifically to fat malabsorption, which is primarily due to pancreatic enzyme deficiency in cystic fibrosis.
Celiac disease US Medical PG Question 3: A previously healthy 20-year-old woman comes to the physician because of recurrent abdominal cramps, bloating, and diarrhea for 4 months. She describes her stools as greasy, foul-smelling, and difficult to flush. During this time she has had a 6-kg (13.2-lb) weight loss. She has no personal or family history of serious illness. Physical examination shows pallor and cheilitis. Laboratory studies show a hemoglobin concentration of 11 g/dL. Serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Test of the stool for occult blood is negative and stool microscopy reveals no pathogens and no leukocytes. Analysis of a 24-hour stool sample shows 12 g of fat. The patient is asked to consume 25 g of d-xylose. Five hours later, its concentration is measured in urine at 2 g (N = > 4 g/5 h). The test is repeated after a two-week course of rifaximin, but the urinary concentration of d-xylose remains the same. Which of the following is the most likely diagnosis?
- A. Exocrine pancreatic insufficiency
- B. Bacterial overgrowth in the small intestine
- C. Tropheryma whipplei infection
- D. Hypersensitivity to gliadin (Correct Answer)
- E. Lactose intolerance
Celiac disease Explanation: ***Hypersensitivity to gliadin***
* The patient's symptoms (greasy, foul-smelling stools, weight loss, abdominal cramps, bloating, diarrhea, pallor, cheilitis, iron-deficiency anemia) are highly suggestive of **malabsorption**.
* The **impaired d-xylose absorption** that does not improve after antibiotics points to an intrinsic small bowel mucosal defect rather than bacterial overgrowth, making celiac disease (hypersensitivity to gliadin) the most likely diagnosis.
*Exocrine pancreatic insufficiency*
* While it causes **steatorrhea** and malabsorption, it typically presents with normal d-xylose absorption because **d-xylose is a monosaccharide that is absorbed directly by the intestinal mucosa without requiring pancreatic enzymes**.
* The normal function of the small intestinal mucosa would allow for adequate d-xylose absorption.
*Bacterial overgrowth in the small intestine*
* Symptoms can mimic malabsorption, and d-xylose absorption may be impaired due to bacterial consumption.
* However, the patient's d-xylose test did not improve after a course of **rifaximin**, which is an antibiotic effective against bacterial overgrowth.
*Tropheryma whipplei infection*
* Whipple's disease can cause malabsorption, **steatorrhea**, and abdominal symptoms similar to those described.
* However, it also commonly presents with **arthralgia, lymphadenopathy, and neurological symptoms**, which are absent in this patient.
*Lactose intolerance*
* This condition primarily causes bloating, cramps, and diarrhea, but typically does not lead to **significant weight loss** or **steatorrhea (greasy stools)**.
* D-xylose absorption would also be expected to be normal because it is a **monosaccharide** that is absorbed directly, unlike lactose which requires lactase.
Celiac disease US Medical PG Question 4: An 82-year-old woman presents with 2 months of foul-smelling, greasy diarrhea. She says that she also has felt very tired recently and has had some associated bloating and flatus. She denies any recent abdominal pain, nausea, melena, hematochezia, or vomiting. She also denies any history of recent travel and states that her home has city water. Which of the following tests would be most appropriate to initially work up the most likely diagnosis in this patient?
- A. Fecal fat test (Correct Answer)
- B. Tissue transglutaminase antibody test
- C. Stool O&P
- D. Stool guaiac test
- E. CT of the abdomen with oral contrast
Celiac disease Explanation: ***Fecal fat test***
- The patient's symptoms of **foul-smelling, greasy diarrhea**, along with **fatigue, bloating, and flatus**, strongly suggest **malabsorption**, specifically **steatorrhea** (excess fat in stool).
- A **fecal fat test** (e.g., Sudan stain or 72-hour quantitative stool fat collection) directly assesses fat malabsorption and would be the most appropriate initial diagnostic test.
*Tissue transglutaminase antibody test*
- This test is used to screen for **celiac disease**, which can cause malabsorption symptoms.
- While celiac disease is a possibility, a fecal fat test is a more general and appropriate initial step to confirm fat malabsorption before looking for specific causes.
*Stool O&P*
- Stands for **Stool Ova and Parasites**, used to detect parasitic infections like **Giardia** or **Cryptosporidium**, which can cause diarrhea.
- However, the absence of recent travel, city water, and the prominent greasy nature of the stool make this less likely as the primary initial investigation compared to confirming malabsorption.
*Stool guaiac test*
- This test detects **occult blood in stool**.
- The patient denies **melena or hematochezia**, and there are no signs pointing to gastrointestinal bleeding, making this test irrelevant for her presenting symptoms.
*CT of the abdomen with oral contrast*
- A CT scan with contrast might be used to investigate structural abnormalities or inflammation if other tests confirm malabsorption or point to a specific organ pathology (e.g., pancreatitis, Crohn's disease).
- It's an imaging study and generally not the most appropriate *initial* test for evaluating the described symptoms of malabsorption.
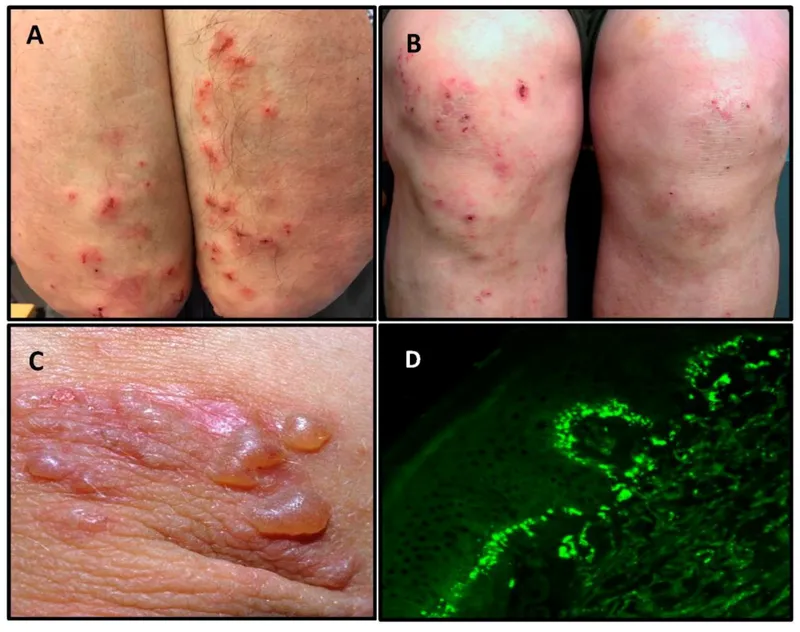
Celiac disease US Medical PG Question 5: A 24-year-old man comes to the physician for the evaluation of a severely pruritic skin rash. Physical examination shows a symmetrical rash over the knees and elbows with tense, grouped vesicles, and several excoriation marks. Microabscesses in the papillary dermis are seen on light microscopy. Immunofluorescence shows deposits of immunoglobulin A at the tips of dermal papillae. This patient's skin findings are most likely associated with which of the following?
- A. Mite eggs and fecal pellets
- B. Positive Nikolsky sign
- C. Gliadin-dependent hypersensitivity (Correct Answer)
- D. Multinucleated giant cells
- E. Nail pitting
Celiac disease Explanation: ***Gliadin-dependent hypersensitivity***
- The description of a severely **pruritic rash** with **grouped vesicles** on extensor surfaces (knees and elbows), along with **IgA deposits** at the tips of dermal papillae and **microabscesses**, is classic for **dermatitis herpetiformis**.
- Dermatitis herpetiformis is strongly associated with **celiac disease**, which is caused by a **hypersensitivity reaction to gliadin**, a protein found in gluten.
*Mite eggs and fecal pellets*
- This finding is characteristic of **scabies**, which presents with burrows, intense pruritus, and a rash that primarily affects the web spaces of fingers, wrists, and other areas where mites burrow.
- The clinical presentation and microscopic findings (IgA deposits, microabscesses) do not align with scabies.
*Positive Nikolsky sign*
- A positive Nikolsky sign (skin sloughing with gentle lateral pressure) is typically seen in **pemphigus vulgaris** or **toxic epidermal necrolysis (TEN)**.
- These conditions involve blistering but have distinct histological features and different immune pathologies (e.g., IgG antibodies against desmoglein in pemphigus vulgaris).
*Multinucleated giant cells*
- The presence of **multinucleated giant cells** is a histological hallmark of **viral infections**, such as **herpes simplex virus (HSV)** or **varicella-zoster virus (VZV)**.
- While these can cause vesicular rashes, the characteristic IgA deposition and microabscesses are not typical of viral infections.
*Nail pitting*
- **Nail pitting** is a common finding in **psoriasis** and **psoriatic arthritis**.
- Psoriasis typically presents with erythematous plaques with silvery scales, which is different from the vesicular rash seen in this patient.
Celiac disease US Medical PG Question 6: A 24-year-old woman with 45,X syndrome comes to the physician because of diarrhea for 4 months. She also reports bloating, nausea, and abdominal discomfort that persists after defecation. For the past 6 months, she has felt tired and has been unable to do her normal chores. She went on a backpacking trip across Southeast Asia around 7 months ago. She is 144 cm (4 ft 9 in) tall and weighs 40 kg (88 lb); BMI is 19 kg/m2. Her blood pressure is 110/60 mm Hg in the upper extremities and 80/40 mm Hg in the lower extremities. Examination shows pale conjunctivae and angular stomatitis. Abdominal examination is normal. Laboratory studies show:
Hemoglobin 9.1 mg/dL
Leukocyte count 5100/mm3
Platelet count 200,000/mm3
Mean corpuscular volume 67 μmm3
Serum
Na+ 136 mEq/L
K+ 3.7 mEq/L
Cl- 105 mEq/L
Glucose 89 mg/dL
Creatinine 1.4 mg/dL
Ferritin 10 ng/mL
IgA tissue transglutaminase antibody positive
Based on the laboratory studies, a biopsy for confirmation of the diagnosis is suggested, but the patient is unwilling to undergo the procedure. Which of the following is the most appropriate next step in management of this patient's gastrointestinal symptoms?
- A. Avoid milk products
- B. Gluten-free diet (Correct Answer)
- C. Metronidazole therapy
- D. Intravenous immunoglobulin therapy
- E. Trimethoprim-sulfamethoxazole therapy
Celiac disease Explanation: ***Gluten-free diet***
- The patient's symptoms (diarrhea, bloating, abdominal discomfort, fatigue) and lab findings (**microcytic anemia** with **low ferritin**, and **positive IgA tissue transglutaminase antibody**) are highly suggestive of **celiac disease**.
- Given the strong serological evidence and patient's unwillingness for biopsy, initiating a **gluten-free diet** is the most appropriate next step, as it is the primary treatment for celiac disease and should alleviate symptoms.
*Avoid milk products*
- While **lactose intolerance** can cause similar GI symptoms like diarrhea and bloating, and is sometimes comorbid with celiac disease due to damage to intestinal villi, the primary driver here appears to be celiac disease based on the specific antibody test.
- Avoiding milk products without addressing the underlying celiac disease would likely not resolve all symptoms, and a gluten-free diet is the more targeted initial therapy for the confirmed serology.
*Metronidazole therapy*
- **Metronidazole** is an antibiotic used to treat bacterial and parasitic infections, such as *Giardia* or *Clostridium difficile*.
- Although the patient traveled to Southeast Asia, suggesting a possible exposure to parasitic infections, the presence of **positive IgA tissue transglutaminase antibody** strongly points towards celiac disease, not solely an infection requiring antibiotics (though infections can sometimes trigger celiac disease onset).
*Intravenous immunoglobulin therapy*
- **Intravenous immunoglobulin (IVIG) therapy** is used for various immune deficiencies or autoimmune conditions, but it is not indicated for the initial management of celiac disease.
- Celiac disease is managed by dietary changes (gluten-free diet) to prevent autoimmune damage to the small intestine.
*Trimethoprim-sulfamethoxazole therapy*
- **Trimethoprim-sulfamethoxazole** is an antibiotic primarily used for bacterial infections, including some diarrheal diseases.
- Similar to metronidazole, while an infection is plausible given the travel history, the strong serological evidence for celiac disease makes antibiotic therapy a less appropriate first step compared to a gluten-free diet.
Celiac disease US Medical PG Question 7: A 54-year-old man comes to the physician because of diarrhea that has become progressively worse over the past 4 months. He currently has 4–6 episodes of foul-smelling stools per day. Over the past 3 months, he has had fatigue and a 5-kg (11-lb) weight loss. He returned from Bangladesh 6 months ago after a year-long business assignment. He has osteoarthritis and hypertension. Current medications include amlodipine and naproxen. He appears pale and malnourished. His temperature is 37.3°C (99.1°F), pulse is 76/min, and blood pressure is 140/86 mm Hg. Examination shows pale conjunctivae and dry mucous membranes. Angular stomatitis and glossitis are present. The abdomen is distended but soft and nontender. Rectal examination shows no abnormalities. Laboratory studies show:
Hemoglobin 8.9 g/dL
Leukocyte count 4100/mm3
Platelet count 160,000/mm3
Mean corpuscular volume 110 μm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/l
K+ 3.3 mEq/L
Creatinine 1.1 mg/dL
IgA 250 mg/dL
Anti-tissue transglutaminase, IgA negative
Stool culture and studies for ova and parasites are negative. Test of the stool for occult blood is negative. Fecal fat content is 22 g/day (N < 7). Fecal lactoferrin is negative and elastase is within normal limits. Which of the following is the most appropriate next step in diagnosis?
- A. CT scan of the abdomen
- B. IgG against deamidated gliadin peptide
- C. Schilling test
- D. Enteroscopy
- E. PAS-stained biopsy of small bowel (Correct Answer)
Celiac disease Explanation: ***PAS-stained biopsy of small bowel***
- The patient's history of travel to Bangladesh, chronic diarrhea, malabsorption (weight loss, fatigue, elevated fecal fat, macrocytic anemia), and negative celiac serology (anti-tissue transglutaminase IgA) are highly suggestive of **Whipple's disease**.
- **Periodic Acid-Schiff (PAS) staining** of a small bowel biopsy is the gold standard for diagnosing Whipple's disease, revealing **PAS-positive macrophages** containing *Tropheryma whipplei*.
*CT scan of the abdomen*
- While a CT scan can identify structural abnormalities or masses, it is not the most direct diagnostic test for **malabsorptive conditions** like Whipple's disease.
- It would likely show non-specific findings such as **bowel wall thickening** or **lymphadenopathy**, but not the definitive histological changes.
*IgG against deamidated gliadin peptide*
- This test is used to diagnose **celiac disease**, but the patient's IgA anti-tissue transglutaminase was already negative, and this IgG test is typically performed when IgA deficiency is suspected or in young children.
- Given the strong suspicion of an infectious etiology due to travel history and systemic symptoms, focusing solely on celiac serology is less appropriate as the first next step.
*Schilling test*
- The Schilling test is an **obsolete test** that was historically used to assess **vitamin B12 absorption** and differentiate causes of B12 deficiency (pernicious anemia, bacterial overgrowth, or pancreatic insufficiency).
- This test is **no longer performed in clinical practice** due to unavailability of radioactive B12; modern evaluation uses serum B12, methylmalonic acid, and homocysteine levels.
- While the patient has macrocytic anemia, the test would not directly address the underlying cause of fat malabsorption and systemic symptoms present.
*Enteroscopy*
- Enteroscopy allows for visualization and biopsy of the small bowel beyond the reach of a standard upper endoscopy.
- While useful for obtaining biopsies, simply performing an enteroscopy without knowing what to look for or what specific stain to request (referring to PAS) on the biopsy would be less targeted than ordering a **PAS-stained biopsy** specifically.
Celiac disease US Medical PG Question 8: A 42-year-old woman presents with exertional dyspnea and fatigue for the past 3 months. Her past medical history is significant for multiple episodes of mild diarrhea for many years, which was earlier diagnosed as irritable bowel syndrome (IBS). She denies any current significant gastrointestinal symptoms. The patient is afebrile and vital signs are within normal limits. Physical examination reveals oral aphthous ulcers and mild conjunctival pallor. Abdominal examination is unremarkable. There is a rash present on the peripheral extremities bilaterally (see image). Laboratory findings are significant for evidence of microcytic hypochromic anemia. FOBT is negative. Which of the following is the most likely diagnosis in this patient?
- A. Small intestinal bacterial overgrowth
- B. Whipple's disease
- C. Non-tropical sprue (Correct Answer)
- D. Inflammatory bowel disease
- E. Tropical sprue
Celiac disease Explanation: ***Non-tropical sprue***
- The patient's presentation with **exertional dyspnea, fatigue, oral aphthous ulcers, microcytic hypochromic anemia** (indicating **iron deficiency from malabsorption**), and a rash consistent with **dermatitis herpetiformis** (as indicated by the peripheral rash on extremities) despite no current significant GI symptoms, strongly points to **celiac disease (non-tropical sprue)**.
- Celiac disease can manifest with **extra-intestinal symptoms** like iron deficiency anemia, skin rashes, and oral ulcers due to malabsorption, even in the absence of severe gastrointestinal complaints, and its diagnosis can be often delayed due to misdiagnosis of IBS.
- **Iron deficiency anemia** is the most common hematologic manifestation of celiac disease due to impaired absorption in the proximal small intestine.
*Small intestinal bacterial overgrowth*
- While SIBO can cause malabsorption and diarrhea, it **does not typically present with oral aphthous ulcers or a rash consistent with dermatitis herpetiformis**.
- **Anemia** can occur due to long-standing SIBO, but the overall constellation of findings is more suggestive of another diagnosis.
*Whipple's disease*
- Whipple's disease is a rare systemic infection that can cause **malabsorption, arthralgias, ocular symptoms**, and **neurological abnormalities**.
- However, **oral aphthous ulcers and dermatitis herpetiformis are not characteristic features** of Whipple's disease, and the skin lesions in Whipple's are usually hyperpigmentation.
*Inflammatory bowel disease*
- While Crohn's disease (a type of IBD) can be associated with **oral aphthous ulcers** and **anemia**, the rash on the extremities is not typical for IBD except for **erythema nodosum or pyoderma gangrenosum** which do not match the expected dermatitis herpetiformis pattern.
- The patient's long history of episodic diarrhea diagnosed as IBS, but with evolving extra-intestinal symptoms, makes celiac disease a more fitting diagnosis.
*Tropical sprue*
- **Tropical sprue** is a malabsorption syndrome occurring in residents or visitors to tropical regions, typically presenting with **chronic diarrhea, steatorrhea, and weight loss**.
- It is **not commonly associated with oral aphthous ulcers or specific dermatological manifestations like dermatitis herpetiformis**, and the patient's history does not indicate recent travel to tropical areas.
Celiac disease US Medical PG Question 9: A 74-year-old woman presents to the clinic for evaluation of an erythematous and edematous skin rash on her right leg that has progressively worsened over the last 2 weeks. The medical history is significant for hypertension and diabetes mellitus type 2. She takes prescribed lisinopril and metformin. The vital signs include: blood pressure 152/92 mm Hg, heart rate 76/min, respiratory rate 12/min, and temperature 37.8°C (100.1°F). On physical exam, the patient appears alert and oriented. Observation of the lesion reveals a poorly demarcated region of erythema and edema along the anterior aspect of the right tibia. Within the region of erythema is a 2–3 millimeter linear break in the skin that does not reveal any serous or purulent discharge. Tenderness to palpation and warmth is associated with the lesion. There are no vesicles, pustules, papules, or nodules present. Ultrasound of the lower extremity is negative for deep vein thrombosis or skin abscess. The blood cultures are pending. Which of the following is the most likely diagnosis based on history and physical examination?
- A. Irritant contact dermatitis
- B. Gas gangrene
- C. Folliculitis
- D. Erysipelas
- E. Cellulitis (Correct Answer)
Celiac disease Explanation: **Cellulitis**
- The patient's presentation with a **poorly demarcated**, erythematous, and edematous rash on the lower leg, accompanied by warmth, tenderness, and a low-grade fever, is highly consistent with **cellulitis**. The linear skin break provides a potential port of entry for bacteria.
- Her history of **diabetes mellitus** is a significant risk factor for cellulitis due to impaired immune function and compromised peripheral circulation. The absence of vesicles or pustules further supports this diagnosis.
*Irritant contact dermatitis*
- This condition is typically characterized by **pruritus (itching)** and a rash that develops after exposure to an irritant, which is not described.
- While it can cause redness and edema, contact dermatitis usually does not present with significant **warmth**, tenderness, or fever.
*Gas gangrene*
- This is a severe, rapidly progressing infection characterized by **crepitus** (gas in the tissues), severe pain, and often a foul-smelling discharge, none of which are noted in the patient's presentation.
- The patient's symptoms are localized and do not suggest the systemic toxicity and rapid tissue necrosis associated with gas gangrene.
*Folliculitis*
- Folliculitis involves inflammation of hair follicles, presenting as small, **pustular lesions centered on hair follicles**, which are explicitly stated to be absent in this case.
- The extensive, diffuse erythema and edema described are not typical features of folliculitis.
*Erysipelas*
- Erysipelas is a superficial skin infection that typically presents with a **sharply demarcated**, raised border, unlike the "poorly demarcated" lesion described.
- While it shares some features with cellulitis (erythema, edema), the distinct border is a key differentiator, and erysipelas is also more likely to affect the face.
Celiac disease US Medical PG Question 10: A 21-year-old woman presents with malaise, joint pains, and a rash that worsens with sun exposure. Examination reveals an erythematous facial rash with edema. Her complete blood count shows lymphocytopenia. In addition to the most likely diagnosis, which of the following disorders can also cause lymphocytopenia? I. HIV II. Autoimmune disorders III. Tuberculosis IV. Lymphoma V. Hypersplenism
- A. I, II, IV, V (Correct Answer)
- B. III, V
- C. I, II, III
- D. III, IV
- E. I, III, V
Celiac disease Explanation: ***I, II, IV, V***
- The patient's symptoms (malar rash, photosensitivity, joint pains, malaise, lymphocytopenia) are highly suggestive of **Systemic Lupus Erythematosus (SLE)**, an **autoimmune disorder** (II).
- **HIV (I)** directly destroys CD4+ T lymphocytes, causing profound lymphocytopenia.
- **Autoimmune disorders (II)** like SLE, rheumatoid arthritis, and Sjögren's syndrome cause lymphocytopenia via antibody-mediated destruction.
- **Lymphoma (IV)** causes lymphocytopenia through bone marrow infiltration, increased consumption, or sequestration.
- **Hypersplenism (V)** causes sequestration and destruction of lymphocytes along with other blood cells.
- While disseminated tuberculosis can occasionally cause lymphocytopenia, **chronic tuberculosis typically causes lymphocytosis**, making it a less reliable answer.
*III, V*
- This option is incomplete as it correctly identifies hypersplenism but omits HIV, autoimmune disorders, and lymphoma, which are more consistent causes of lymphocytopenia.
- **Tuberculosis (III)** in its chronic form typically causes **lymphocytosis**, not lymphocytopenia, though severe disseminated disease may cause lymphocytopenia.
*I, II, III*
- While HIV and autoimmune disorders are correct, including **tuberculosis (III)** is problematic as chronic TB typically causes **lymphocytosis**, not lymphocytopenia.
- This option omits lymphoma and hypersplenism, both important causes.
*III, IV*
- **Tuberculosis (III)** in chronic form typically causes **lymphocytosis** rather than lymphocytopenia, making it an unreliable choice.
- Although **lymphoma (IV)** is correct, this option excludes HIV, autoimmune disorders, and hypersplenism.
*I, III, V*
- **HIV (I)** and **hypersplenism (V)** are valid causes, but **tuberculosis (III)** is inconsistent as chronic TB typically causes lymphocytosis.
- This option incorrectly includes tuberculosis while omitting autoimmune disorders and lymphoma.
More Celiac disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.