Type 2 diabetes mellitus US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Type 2 diabetes mellitus. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Type 2 diabetes mellitus US Medical PG Question 1: A 19-year-old man with a history of type 1 diabetes presents to the emergency department for the evaluation of a blood glucose level of 492 mg/dL. Laboratory examination revealed a serum bicarbonate level of 13 mEq/L, serum sodium level of 122 mEq/L, and ketonuria. Arterial blood gas demonstrated a pH of 6.9. He is admitted to the hospital and given bicarbonate and then started on an insulin drip and intravenous fluid. Seven hours later when his nurse is making rounds, he is confused and complaining of a severe headache. Repeat sodium levels are unchanged, although his glucose level has improved. His vital signs include a temperature of 36.6°C (98.0°F), pulse 50/min, respiratory rate 13/min and irregular, and blood pressure 177/95 mm Hg. What other examination findings would be expected in this patient?
- A. Hypoglycemia
- B. Pupillary constriction
- C. Papilledema (Correct Answer)
- D. Pancreatitis
- E. Peripheral edema
Type 2 diabetes mellitus Explanation: ***Papilledema***
- This patient's symptoms (confusion, severe headache, bradycardia, irregular respiration, hypertension) following treatment for **diabetic ketoacidosis (DKA)** are highly suggestive of **cerebral edema**.
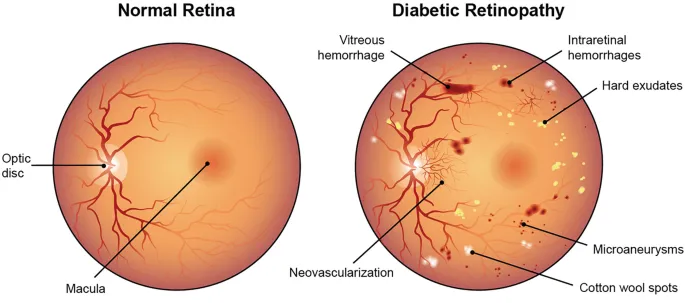
- **Papilledema** is a retinal finding resulting from increased intracranial pressure (ICP), which is a characteristic sign of cerebral edema.
*Hypoglycemia*
- While the patient's glucose level has improved, it is not described as being low enough to cause hypoglycemia, and the symptoms are more consistent with **increased ICP**.
- Symptoms of hypoglycemia (e.g., tremors, sweating, hunger, anxiety) are different from the patient's current presentation of confusion and severe headache.
*Pupillary constriction*
- **Pupillary constriction** (miosis) is typically not associated with cerebral edema; instead, **pupillary dilation** (mydriasis) can occur with severe increase in ICP due to uncal herniation.
- The combination of bradycardia, irregular respiration, and hypertension (Cushing's triad) is indicative of increased ICP, which would likely cause pupillary changes related to brainstem compression.
*Pancreatitis*
- Pancreatitis is a known complication of DKA, but it typically presents with **severe abdominal pain**, nausea, and vomiting, rather than cerebral symptoms.
- Although the patient had DKA, the current neurological symptoms point directly to an intracranial process rather than an abdominal issue.
*Peripheral edema*
- **Peripheral edema** results from fluid accumulation in peripheral tissues and is not a direct consequence or expected finding in cerebral edema.
- While fluid administration can cause some peripheral fluid retention, it typically does not lead to the acute neurological deterioration seen in this patient.
Type 2 diabetes mellitus US Medical PG Question 2: A 54-year-old woman presents for follow-up care for her type 2 diabetes mellitus. She was diagnosed approximately 2 years ago and was treated with dietary modifications, an exercise regimen, metformin, and glipizide. She reports that her increased thirst and urinary frequency has not improved with her current treatment regimen. Her hemoglobin A1c is 8.5% at this visit. She is started on a medication that will result in weight loss but places her at increased risk of developing urinary tract infections and vulvovaginal candidiasis. Which of the following is the mechanism of action of the prescribed medication?
- A. Peroxisome proliferator-activated receptor activator
- B. Glucagon-like protein-1 receptor agonist
- C. Sodium-glucose co-transporter-2 inhibitor (Correct Answer)
- D. Alpha-glucosidase inhibitor
- E. Dipeptidyl peptidase-4 inhibitor
Type 2 diabetes mellitus Explanation: ***Sodium-glucose co-transporter-2 inhibitor***
- The patient's **HbA1c of 8.5%** indicates uncontrolled diabetes, and the mention of weight loss and increased risk of **urinary tract infections (UTIs)** and **vulvovaginal candidiasis** strongly points to an SGLT2 inhibitor.
- SGLT2 inhibitors work by **blocking glucose reabsorption in the renal tubules**, leading to increased glucose excretion in urine, which can cause candidiasis and UTIs, and also contributes to weight loss.
*Peroxisome proliferator-activated receptor activator*
- This refers to **thiazolidinediones (TZDs)**, which reduce insulin resistance by increasing glucose uptake in peripheral tissues, but are not associated with increased UTIs or vulvovaginal candidiasis.
- TZDs can cause **weight gain** and fluid retention, which is contrary to the weight loss mentioned in the stem.
*Glucagon-like protein-1 receptor agonist*
- GLP-1 receptor agonists like liraglutide and semaglutide encourage **weight loss** and improve glycemic control by increasing insulin secretion and decreasing glucagon secretion, but they are not primarily associated with increased risk of UTIs or candidiasis.
- Their common side effects include **gastrointestinal issues** such as nausea and vomiting.
*Alpha-glucosidase inhibitor*
- These medications (e.g., acarbose) work by **delaying carbohydrate absorption** in the gut, which primarily helps reduce postprandial glucose levels.
- They commonly cause **gastrointestinal side effects** such as flatulence and diarrhea, and are not associated with UTIs, candidiasis, or significant weight loss.
*Dipeptidyl peptidase-4 inhibitor*
- DPP-4 inhibitors (e.g., sitagliptin, saxagliptin) enhance the effects of incretin hormones by **preventing their breakdown**, leading to increased insulin secretion and decreased glucagon.
- They are generally **weight-neutral** and do not cause the specific adverse effects (UTIs, candidiasis) mentioned in the clinical scenario.
Type 2 diabetes mellitus US Medical PG Question 3: A 58-year-old male presents to the clinic for a follow-up visit. He takes metformin every day and says that he is compliant with his medication but can not control his diet. Three months prior, his HbA1c was 8.2% when he was started on metformin. He does not have any complaints on this visit. His temperature is 37°C (98.6°F), respirations are 15/min, pulse is 67/min and blood pressure is 122/88 mm Hg. His BMI is 33. Physical examination is within normal limits. Blood is drawn for laboratory tests and the results are given below:
Fasting blood glucose 150 mg/dL
Glycated hemoglobin (HbA1c) 7.2 %
Serum Creatinine 1.1 mg/dL
BUN 12 mg/dL
The physician wants to initiate another medication for his blood glucose control, specifically one that does not carry a risk of weight gain. Addition of which of the following drugs would be most suitable for this patient?
- A. Sitagliptin (Correct Answer)
- B. Glimepiride
- C. Rosiglitazone
- D. Glyburide
- E. Pioglitazone
Type 2 diabetes mellitus Explanation: ***Sitagliptin***
- This is a **dipeptidyl peptidase-4 (DPP-4) inhibitor** that enhances incretin effects, leading to glucose-dependent insulin secretion and suppressed glucagon.
- DPP-4 inhibitors like sitagliptin are **weight-neutral** and pose a low risk of hypoglycemia, making them suitable additions for patients who need further glycemic control without weight gain, especially with their current BMI.
*Glimepiride*
- This is a **sulfonylurea** that stimulates insulin release from pancreatic beta cells independently of glucose levels.
- Sulfonylureas are associated with a **risk of weight gain** and hypoglycemia, which is an undesirable effect for this patient.
*Rosiglitazone*
- This is a **thiazolidinedione (TZD)** that improves insulin sensitivity in peripheral tissues and the liver.
- TZDs, including rosiglitazone, are associated with **weight gain** due to fluid retention and increased adipogenesis, and can also cause congestive heart failure.
*Glyburide*
- This is also a **sulfonylurea**, similar to glimepiride, that stimulates insulin secretion.
- Like other sulfonylureas, glyburide carries a significant risk of **weight gain** and hypoglycemia, making it less ideal for this patient.
*Pioglitazone*
- This is another **thiazolidinedione (TZD)** that improves insulin sensitivity.
- Pioglitazone is known to cause **weight gain** and fluid retention, and it has a black box warning for exacerbating heart failure.
Type 2 diabetes mellitus US Medical PG Question 4: A 65-year-old woman comes to the emergency department because of blurry vision for 10 hours. She has also had urinary urgency and discomfort while urinating for the past 4 days. She has been feeling increasingly weak and nauseous since yesterday. She has a history of type 2 diabetes mellitus and arterial hypertension. One year ago she was treated for an infection of her eyes. She drinks 2–3 glasses of wine weekly. Current medications include captopril, metoprolol, metformin, and insulin. Her temperature is 37.5°C (99.5°F), pulse is 107/min, and blood pressure is 95/70 mm Hg. Visual acuity is decreased in both eyes. The pupils are equal and reactive to light. The corneal reflexes are brisk. The mucous membranes of the mouth are dry. The abdomen is soft and not distended. Cardiopulmonary examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Alcoholic ketoacidosis
- B. Hypoglycemia
- C. Ischemic optic neuropathy
- D. Hyperosmolar hyperglycemic state (Correct Answer)
- E. Posterior uveitis
Type 2 diabetes mellitus Explanation: ***Hyperosmolar hyperglycemic state***
- The patient's history of **type 2 diabetes mellitus**, recent **infection** (urinary urgency and discomfort), blurry vision, weakness, nausea, and signs of **dehydration** (dry mucous membranes, hypotension, tachycardia) are all consistent with Hyperosmolar Hyperglycemic State (HHS).
- HHS is characterized by severe hyperglycemia, hyperosmolarity, and dehydration without significant ketoacidosis, often triggered by stress such as infection in patients with T2DM.
*Alcoholic ketoacidosis*
- Although the patient drinks wine, the amount (2-3 glasses weekly) is not typically sufficient to induce **alcoholic ketoacidosis**.
- Alcoholic ketoacidosis usually occurs in chronic alcoholics after an acute reduction in alcohol intake and inadequate nutritional intake, leading to elevated anion gap metabolic acidosis.
*Hypoglycemia*
- While patients on insulin and metformin are at risk for hypoglycemia, the presented symptoms of **dehydration**, sustained **blurry vision**, and **weakness** over an extended period (10 hours) are not typical for hypoglycemia, which usually presents with rapid onset neuroglycopenic symptoms and resolves quickly with glucose.
- The patient's symptoms are more indicative of a state of high blood glucose rather than low.
*Ischemic optic neuropathy*
- This condition causes **sudden, painless vision loss** due to infarction of the optic nerve, often associated with diabetes and hypertension.
- While the patient has blurry vision and risk factors, the presence of systemic symptoms like **urinary infection**, **nausea**, and **dehydration** points to a broader metabolic derangement rather than an isolated ocular event.
*Posterior uveitis*
- Posterior uveitis involves **inflammation of the choroid and retina**, which can cause blurry vision, floaters, and photophobia.
- However, there are no signs of inflammation (e.g., pain, redness), and the systemic symptoms of **dehydration and infection** are not directly explained by uveitis, making a metabolic cause more likely given the patient's diabetes.
Type 2 diabetes mellitus US Medical PG Question 5: A 53-year-old woman with type 2 diabetes mellitus is admitted for evaluation of recurrent episodes of nausea, tremors, and excessive sweating. She works as a nurse and reports self-measured blood glucose levels below 50 mg/dL on several occasions. Her family history is positive for borderline personality disorder. The only medication listed in her history is metformin. Which of the following is the most appropriate next step in management?
- A. Measure serum C-peptide concentration
- B. Ask the patient if she is taking any medications other than metformin (Correct Answer)
- C. Search the patient's belongings for insulin
- D. Measure glycated hemoglobin concentration
- E. Report the patient to her employer
Type 2 diabetes mellitus Explanation: ***Ask the patient if she is taking any medications other than metformin***
- The patient's presentation with recurrent **hypoglycemic symptoms** (nausea, tremors, sweating) and documented low blood glucose, while only being prescribed metformin (which does not cause hypoglycemia), strongly suggests **exogenous insulin or sulfonylurea use**.
- A direct question about other medications is a crucial initial step to ascertain the cause of her hypoglycemia and to rule out **factitious hypoglycemia**, especially given her profession as a nurse and a family history that might suggest psychological vulnerabilities, although not a direct diagnosis for the patient.
*Measure serum C-peptide concentration*
- While **low C-peptide** in the presence of hypoglycemia would suggest exogenous insulin administration, and high C-peptide might point to an insulinoma, this test should be done *after* ruling out common causes like the undisclosed use of other medications.
- This is a more invasive and less direct initial step compared to simply asking the patient about medication use, especially when a readily reversible cause (undisclosed medication) is possible.
*Search the patient's belongings for insulin*
- Searching a patient's belongings without their consent is a serious ethical breach and a violation of privacy.
- This action should only be considered as a last resort in extreme circumstances and with appropriate legal and ethical oversight, not as an initial diagnostic step.
*Measure glycated hemoglobin concentration*
- **Glycated hemoglobin (HbA1c)** reflects average blood glucose levels over the past 2-3 months and is used to monitor long-term glycemic control in diabetic patients.
- While useful for diabetes management, it will not directly identify the acute cause of recurrent hypoglycemic episodes or distinguish between endogenous and exogenous insulin sources.
*Report the patient to her employer*
- Reporting the patient to her employer prematurely, without a definitive diagnosis or understanding the full context of her condition, is unethical and unprofessional.
- The immediate priority is to diagnose and manage the patient's medical condition, ensuring her safety and well-being, before considering professional implications.
Type 2 diabetes mellitus US Medical PG Question 6: A 50-year-old Caucasian man presents for a routine checkup. He does not have any current complaint. He is healthy and takes no medications. He has smoked 10–15 cigarettes per day for the past 10 years. His family history is negative for gastrointestinal disorders. Which of the following screening tests is recommended for this patient according to the United States Preventive Services Task Force (USPSTF)?
- A. Abdominal ultrasonography for abdominal aortic aneurysm
- B. Carcinoembryonic antigen for colorectal cancer
- C. Low-dose computerized tomography for lung cancer
- D. Colonoscopy for colorectal cancer (Correct Answer)
- E. Prostate-specific antigen for prostate cancer
Type 2 diabetes mellitus Explanation: **Colonoscopy for colorectal cancer**
- The **USPSTF recommends screening for colorectal cancer in adults aged 45 to 75 years**. This patient is 50 years old, placing him squarely within this recommended age range for colonoscopy, irrespective of smoking status or other risk factors.
- **Colonoscopy** is a highly effective screening tool for colorectal cancer, allowing for the detection and removal of precancerous polyps.
*Abdominal ultrasonography for abdominal aortic aneurysm*
- The **USPSTF recommends one-time screening for abdominal aortic aneurysm (AAA) with ultrasonography in men aged 65 to 75 years who have ever smoked**. This patient is 50 years old, falling outside the recommended age range for this screening, despite his smoking history.
- The benefit of screening for AAA is primarily for older men with a history of smoking, as the prevalence of AAA significantly increases with age.
*Low-dose computerized tomography for lung cancer*
- The **USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years**. This patient has a 10-pack-year smoking history (10-15 cigarettes/day for 10 years ≈ 0.5-0.75 packs/day * 10 years = 5-7.5 pack-years), which does not meet the 20 pack-year threshold.
- While the patient is within the age range, his smoking history is insufficient to meet the criteria for routine lung cancer screening with LDCT.
*Carcinoembryonic antigen for colorectal cancer*
- **Carcinoembryonic antigen (CEA) is a tumor marker primarily used for monitoring the recurrence of colorectal cancer after treatment**, not for initial screening in asymptomatic individuals.
- The USPSTF and other guidelines do not recommend CEA as a screening test for colorectal cancer due to its low sensitivity and specificity in asymptomatic populations.
*Prostate-specific antigen for prostate cancer*
- The **USPSTF recommends that men aged 55 to 69 years should make an individual decision about being screened for prostate cancer with a prostate-specific antigen (PSA) test**, after discussing the potential benefits and harms with their clinician.
- This patient is 50 years old, which is younger than the age range where the USPSTF recommends shared decision-making for PSA screening.
Type 2 diabetes mellitus US Medical PG Question 7: A 51-year-old man presents to his physician with increased thirst, frequent urination, and fatigue. These symptoms have increased gradually over the past 3 years. He has no past medical history or current medications. Also, he has no family history of endocrinological or cardiovascular diseases. The blood pressure is 140/90 mm Hg, and the heart rate is 71/min. The patient is afebrile. The BMI is 35.4 kg/m2. On physical examination, there is an increased adipose tissue over the back of the neck, and hyperpigmentation of the axilla and inguinal folds. Which of the following laboratory results is diagnostic of this patient’s most likely condition?
- A. Random plasma glucose 167 mg/dL
- B. Serum insulin level of 10 μU/mL
- C. Plasma glucose of 209 mg/dL 2 hours after the oral glucose load (Correct Answer)
- D. HbA1c 5.9%
- E. Fasting plasma glucose 123 mg/dL
Type 2 diabetes mellitus Explanation: ***Plasma glucose of 209 mg/dL 2 hours after the oral glucose load***
- This value indicates **diabetes mellitus** if the 2-hour plasma glucose is ≥200 mg/dL after a 75-g oral glucose tolerance test (OGTT). The patient's symptoms (thirst, frequent urination, fatigue) and risk factors (obesity, hypertension, acanthosis nigricans) are highly suggestive of type 2 diabetes.
- The elevated BMI, increased adipose tissue in the neck, and **hyperpigmentation** of the axilla and inguinal folds (**acanthosis nigricans**) are strong indicators of **insulin resistance**, a hallmark of type 2 diabetes.
*Random plasma glucose 167 mg/dL*
- A random plasma glucose ≥200 mg/dL with classic symptoms of hyperglycemia (polyuria, polydipsia, unexplained weight loss) is diagnostic of diabetes. A value of 167 mg/dL is **elevated** but, in isolation, without meeting the ≥200 mg/dL threshold for a random test, is **not definitively diagnostic** of diabetes.
- This result would typically warrant further confirmatory testing, such as a fasting plasma glucose or an oral glucose tolerance test.
*Serum insulin level of 10 μU/mL*
- A serum insulin level of 10 μU/mL is within the normal range (typically 2-25 μU/mL). In the setting of **insulin resistance**, patients with type 2 diabetes often have **elevated insulin levels** initially as the pancreas tries to compensate, or normal levels if beta-cell function has declined.
- An isolated insulin level is **not a diagnostic criterion** for diabetes.
*HbA1c 5.9%*
- An HbA1c value between 5.7% and 6.4% indicates **prediabetes**. An HbA1c of ≥6.5% is diagnostic of diabetes.
- While this value suggests impaired glucose regulation, it is **below the diagnostic threshold** for diabetes.
*Fasting plasma glucose 123 mg/dL*
- A fasting plasma glucose between 100 mg/dL and 125 mg/dL indicates **prediabetes** (impaired fasting glucose). A fasting plasma glucose of ≥126 mg/dL is diagnostic of diabetes.
- This value is **below the diagnostic threshold** for diabetes, similar to the HbA1c result, and would indicate prediabetes rather than confirmed diabetes.
Type 2 diabetes mellitus US Medical PG Question 8: A 26-year-old primigravida woman comes to her primary care physician for the second prenatal visit. She is 10 weeks pregnant. She has no current complaint except for occasional nausea. She does not have any chronic health problems. She denies smoking or alcohol intake. Her family history is positive for paternal colon cancer at the age of 55. Vital signs include a temperature of 37.1°C (98.8°F), blood pressure of 120/60 mm Hg, and pulse of 90/min. Physical examination discloses no abnormalities. According to the United States Preventive Services Task Force (USPSTF), which of the following screening tests is recommended for this patient?
- A. Colonoscopy for colorectal cancer at the age of 40
- B. HbA1C for type 2 diabetes mellitus
- C. Colonoscopy for colorectal cancer at the age of 50
- D. Glucose tolerance test for gestational diabetes mellitus
- E. Urine culture for asymptomatic bacteriuria (Correct Answer)
Type 2 diabetes mellitus Explanation: ***Urine culture for asymptomatic bacteriuria***
- The **USPSTF** recommends **screening pregnant individuals for asymptomatic bacteriuria** with a urine culture at the first prenatal visit or at 12-16 weeks' gestation to prevent pyelonephritis and other adverse pregnancy outcomes.
- This patient is in her second prenatal visit at 10 weeks, making this a timely and recommended screening.
*Colonoscopy for colorectal cancer at the age of 40*
- Although the patient has a **family history of paternal colon cancer at age 55**, the general recommendation for earlier screening due to family history typically starts 10 years before the youngest affected relative's diagnosis, but not earlier than age 40, and is not a routine screening for a 26-year-old.
- This screening is not universally recommended at age 40 for everyone, and current guidelines often suggest individualized approaches based on specific family history details that are not fully met by this patient at this age.
*HbA1C for type 2 diabetes mellitus*
- The patient has **no risk factors for type 2 diabetes**, such as obesity, history of gestational diabetes, or strong family history of diabetes, that would warrant early screening with HbA1c.
- Routine screening for type 2 diabetes for an individual of her age and health status is not typically recommended by the USPSTF.
*Colonoscopy for colorectal cancer at the age of 50*
- The **USPSTF recommends screening for colorectal cancer in average-risk individuals beginning at age 45-50**.
- This patient is only 26 years old and is not in the appropriate age group for this general screening recommendation.
*Glucose tolerance test for gestational diabetes mellitus*
- Screening for **gestational diabetes mellitus (GDM)** typically occurs much later in pregnancy, usually between **24 and 28 weeks of gestation**.
- Performing a glucose tolerance test at 10 weeks pregnant is too early for GDM screening based on standard guidelines.
Type 2 diabetes mellitus US Medical PG Question 9: A 40-year-old man presents to the physician for a scheduled checkup. He was diagnosed with type 2 diabetes mellitus 5 years ago and has been taking his prescribed metformin daily, as prescribed. He also started exercising and has improved his diet. He has no particular complaints at the time. The patient has no other medical concerns and takes no medications. There is no family history of cardiovascular disease or diabetes. He does not smoke tobacco, drink alcohol, or use illicit drugs. Vitals are normal. There are no physical findings. His laboratory tests show:
Serum glucose (fasting) 149 mg/dL
Hemoglobin A1c 7.7 %
Serum electrolytes
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 0.8 mg/dL
Blood urea nitrogen 9 mg/dL
Urinalysis
Glucose Negative
Ketones Negative
Leucocytes Negative
Nitrite Negative
Red blood cells (RBC) Negative
Casts Negative
Which of the following lipid profile abnormalities is most likely to be seen?
- A. Normal lipid profile
- B. Normal triglycerides, elevated LDL
- C. Low HDL, elevated LDL
- D. Elevated triglycerides, low HDL (Correct Answer)
- E. Elevated HDL, low LDL
Type 2 diabetes mellitus Explanation: ***Elevated triglycerides, low HDL***
- Patients with **type 2 diabetes mellitus** often exhibit **dyslipidemia** characterized by **elevated triglycerides** and **low high-density lipoprotein (HDL)** cholesterol, even with controlled glucose levels.
- This pattern is part of the **atherogenic dyslipidemia** frequently observed in insulin resistance, increasing cardiovascular risk.
*Normal lipid profile*
- Given the patient's diagnosis of **type 2 diabetes** and suboptimal **HbA1c of 7.7%** (target typically <7%), it is **unlikely** he would have a completely normal lipid profile due to the metabolic disturbances associated with insulin resistance.
- **Diabetes** itself is a risk factor for **dyslipidemia**, which mandates regular lipid screening even without overt symptoms.
*Normal triglycerides, elevated LDL*
- While **elevated LDL** cholesterol can occur in diabetes, a **normal triglyceride** level is **less typical** for diabetic dyslipidemia, which classically features hypertriglyceridemia.
- The most characteristic lipid abnormality in **type 2 diabetes** is often a combination of **high triglycerides** and **low HDL**, rather than isolated elevated LDL with normal triglycerides.
*Low HDL, elevated LDL*
- This option partially captures the typical dyslipidemia, as **low HDL** is characteristic. However, the most consistent abnormality alongside low HDL in diabetes is **elevated triglycerides**, often more prominent than just elevated LDL.
- While **elevated LDL** can occur, the combined pattern of **low HDL** and **elevated triglycerides** is more specific for **diabetic dyslipidemia**.
*Elevated HDL, low LDL*
- This lipid profile is generally considered **protective against cardiovascular disease** and is the **opposite** of what is typically seen in patients with **type 2 diabetes**.
- **Elevated HDL** and **low LDL** would be a favorable lipid profile, which is inconsistent with the metabolic derangements associated with diabetes.
Type 2 diabetes mellitus US Medical PG Question 10: A 75-year-old man presents to his primary care physician for foot pain. The patient states that he has had chronic foot pain, which has finally caused him to come and see the doctor. The patient's past medical history is unknown and he has not seen a doctor in over 50 years. The patient states he has led a healthy lifestyle, consumes a plant-based diet, exercised regularly, and avoided smoking, thus his lack of checkups with a physician. The patient lives alone as his wife died recently. His temperature is 98.1°F (36.7°C), blood pressure is 128/64 mmHg, pulse is 80/min, respirations are 13/min, and oxygen saturation is 98% on room air. The patient's BMI is 19 kg/m^2 and he appears healthy. Physical exam demonstrates a right foot that is diffusely swollen, mildly tender, and deformed. The patient's gait is abnormal. Which of the following is associated with the underlying cause of this patient's presentation?
- A. Methicillin-resistant bacterial agent
- B. Unprotected sexual intercourse
- C. Megaloblastic anemia
- D. High-impact trauma to the foot
- E. Hyperfiltration damage of the kidney (Correct Answer)
Type 2 diabetes mellitus Explanation: ***Hyperfiltration damage of the kidney***
- The patient's presentation of a **deformed and diffusely swollen, mildly tender foot** in a 75-year-old, alongside his self-reported healthy lifestyle (plant-based diet, exercise), points toward **Charcot arthropathy (diabetic foot)**, which is typically a complication of **diabetes mellitus**.
- **Hyperfiltration damage of the kidney** is a key early sign of **diabetic nephropathy**, occurring during stages 1 and 2, where the kidneys compensate for damage by increasing the glomerular filtration rate, eventually leading to proteinuria and chronic kidney disease. This is a common association with long-standing, undiagnosed diabetes.
*Methicillin-resistant bacterial agent*
- This typically causes **acute infections**, often with signs of severe inflammation, warmth, erythema, and possibly purulence. The patient's presentation is of **chronic foot pain** and **deformity**, less suggestive of an acute bacterial infection.
- While foot ulcers related to diabetes can become infected with MRSA, the primary underlying cause of the foot deformity and pain is not MRSA itself, but rather the neuropathic and vascular complications of diabetes.
*Unprotected sexual intercourse*
- **Unprotected sexual intercourse** is a risk factor for sexually transmitted infections (STIs) and their sequelae, such as **reactive arthritis**.
- Reactive arthritis typically presents with acute, asymmetric oligoarthritis, often affecting the lower extremities, and usually has associated urethritis or conjunctivitis, which are not mentioned in this chronic, deforming condition.
*Megaloblastic anemia*
- **Megaloblastic anemia** is primarily caused by **vitamin B12 or folate deficiency** and can lead to neurological symptoms like **peripheral neuropathy** (e.g., paresthesias, gait disturbance).
- While peripheral neuropathy can contribute to foot problems, megaloblastic anemia itself does not directly cause the severe **bone and joint destruction** seen in Charcot arthropathy; it's a consequence of diabetic neuropathy.
*High-impact trauma to the foot*
- **High-impact trauma** can cause fractures, dislocations, or acute soft tissue injuries to the foot, leading to pain and swelling.
- However, the patient's presentation is of **chronic pain and progressive deformity**, indicating a degenerative process rather than an acute traumatic injury. While trauma can exacerbate Charcot foot, it's not the underlying cause.
More Type 2 diabetes mellitus US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.