Type 1 diabetes mellitus US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Type 1 diabetes mellitus. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Type 1 diabetes mellitus US Medical PG Question 1: A 52-year-old man presents to his primary care physician to discuss laboratory results that were obtained during his annual checkup. He has no symptoms or concerns and denies changes in eating or urination patterns. Specifically, the physician ordered a panel of metabolic laboratory tests to look for signs of diabetes, hyperlipidemia, or other chronic disorders. A spot glucose check from a random blood sample showed a glucose level of 211 mg/dL. A hemoglobin A1c level was obtained at the same time that showed a level of 6.3%. A fasting blood glucose was obtained that showed a blood glucose level of 125 mg/dL. Finally, a 2-hour glucose level was obtained after an oral glucose tolerance test that showed a glucose level of 201 mg/dL. Which of the following statements is most accurate for this patient?
- A. This patient does not have type 2 diabetes
- B. This patient has type 2 diabetes as diagnosed by his fasting blood glucose
- C. This patient has type 2 diabetes as diagnosed by his oral tolerance blood glucose (Correct Answer)
- D. This patient has type 2 diabetes as diagnosed by his random blood glucose
- E. This patient has type 2 diabetes as diagnosed by his hemoglobin A1c
Type 1 diabetes mellitus Explanation: **This patient has type 2 diabetes as diagnosed by his oral tolerance blood glucose**
- A 2-hour plasma glucose of **200 mg/dL or higher** during an Oral Glucose Tolerance Test (OGTT) is a diagnostic criterion for diabetes. This patient's 2-hour glucose level of **201 mg/dL** meets this criterion.
- The combination of this elevated OGTT result with a random glucose over 200 mg/dL further supports the diagnosis, even in an asymptomatic individual.
*This patient does not have type 2 diabetes*
- The patient has multiple laboratory values that meet or exceed diagnostic thresholds for diabetes, including a random glucose of **211 mg/dL**, an HbA1c of **6.3%**, and a 2-hour OGTT glucose of **201 mg/dL**.
- While one individual threshold might not be conclusive, the overall pattern of results clearly indicates diabetes.
*This patient has type 2 diabetes as diagnosed by his fasting blood glucose*
- A fasting plasma glucose (FPG) of **126 mg/dL or higher** is diagnostic for diabetes. This patient's FPG of **125 mg/dL** is just below this threshold.
- While concerning, an FPG of 125 mg/dL alone is considered **impaired fasting glucose** (pre-diabetes), not diabetes.
*This patient has type 2 diabetes as diagnosed by his random blood glucose*
- A random plasma glucose of **200 mg/dL or higher** in a symptomatic patient is diagnostic for diabetes. However, this patient is **asymptomatic**.
- In an asymptomatic patient, an elevated random glucose requires confirmation by another diagnostic test (e.g., FPG, OGTT, or HbA1c) on a subsequent day, or concurrent with another positive test (like the OGTT in this case).
*This patient has type 2 diabetes as diagnosed by his hemoglobin A1c*
- An HbA1c level of **6.5% or higher** is diagnostic for diabetes. This patient's HbA1c of **6.3%** is below this cutoff.
- An HbA1c between 5.7% and 6.4% indicates **pre-diabetes**, specifically increased risk for diabetes.
Type 1 diabetes mellitus US Medical PG Question 2: A 14-year-old boy presents to his pediatrician with weakness and frequent episodes of dizziness. He had chronic mucocutaneous candidiasis when he was 4 years old and was diagnosed with autoimmune hypoparathyroidism at age 8. On physical examination, his blood pressure is 118/70 mm Hg in the supine position and 96/64 mm Hg in the upright position. Hyperpigmentation is present over many areas of his body, most prominently over the extensor surfaces, elbows, and knuckles. His laboratory evaluation suggests the presence of antibodies to 21-hydroxylase and a mutation in the AIRE (autoimmune regulator) gene. The pediatrician explains to his parents that his condition is due to the failure of immunological tolerance. Which of the following mechanisms is most likely to have failed in the child?
- A. Inhibition of the inactivation of harmful lymphocytes by regulatory T cells
- B. Positive selection
- C. Negative selection (Correct Answer)
- D. Deletion of mature lymphocytes
- E. Anergy
Type 1 diabetes mellitus Explanation: ***Negative selection***
- This patient's symptoms (chronic mucocutaneous candidiasis, autoimmune hypoparathyroidism, orthostatic hypotension, hyperpigmentation, and antibodies to 21-hydroxylase) are characteristic of **Autoimmune Polyendocrine Syndrome Type 1 (APS-1)**, which is caused by a **mutation in the AIRE gene**.
- The AIRE gene is crucial for the expression of **tissue-specific self-antigens in the thymus**, which is necessary for the **negative selection** of autoreactive T cells during T-cell development. Failure of negative selection allows auto-reactive T cells to escape the thymus, leading to autoimmunity.
*Inhibition of the inactivation of harmful lymphocytes by regulatory T cells*
- This describes a mechanism of **peripheral tolerance**, where **regulatory T cells (Treg)** suppress self-reactive lymphocytes in the periphery.
- While critical for preventing autoimmunity, the primary defect in APS-1 is central tolerance due to AIRE mutation, not a failure of Treg function.
*Positive selection*
- **Positive selection** occurs in the thymus and ensures that T cells can recognize **MHC molecules** (self-MHC restriction).
- Failure of positive selection would lead to a lack of functional T cells, resulting in immunodeficiency, not autoimmunity.
*Deletion of mature lymphocytes*
- The deletion of mature lymphocytes refers to other mechanisms of **peripheral tolerance**, such as activation-induced cell death, which removes self-reactive T cells that have escaped central tolerance and become activated in the periphery.
- This mechanism is distinct from the **central tolerance defect (negative selection)** caused by the AIRE gene mutation.
*Anergy*
- **Anergy** is a state of functional inactivation in lymphocytes that occurs when they recognize self-antigens without adequate co-stimulation. It is a mechanism of **peripheral tolerance**.
- While a form of peripheral tolerance, the primary defect in APS-1 stems from a failure of **central tolerance (negative selection)**, allowing highly autoreactive T cells to mature.
Type 1 diabetes mellitus US Medical PG Question 3: A 19-year-old man with a history of type 1 diabetes presents to the emergency department for the evaluation of a blood glucose level of 492 mg/dL. Laboratory examination revealed a serum bicarbonate level of 13 mEq/L, serum sodium level of 122 mEq/L, and ketonuria. Arterial blood gas demonstrated a pH of 6.9. He is admitted to the hospital and given bicarbonate and then started on an insulin drip and intravenous fluid. Seven hours later when his nurse is making rounds, he is confused and complaining of a severe headache. Repeat sodium levels are unchanged, although his glucose level has improved. His vital signs include a temperature of 36.6°C (98.0°F), pulse 50/min, respiratory rate 13/min and irregular, and blood pressure 177/95 mm Hg. What other examination findings would be expected in this patient?
- A. Hypoglycemia
- B. Pupillary constriction
- C. Papilledema (Correct Answer)
- D. Pancreatitis
- E. Peripheral edema
Type 1 diabetes mellitus Explanation: ***Papilledema***
- This patient's symptoms (confusion, severe headache, bradycardia, irregular respiration, hypertension) following treatment for **diabetic ketoacidosis (DKA)** are highly suggestive of **cerebral edema**.
- **Papilledema** is a retinal finding resulting from increased intracranial pressure (ICP), which is a characteristic sign of cerebral edema.
*Hypoglycemia*
- While the patient's glucose level has improved, it is not described as being low enough to cause hypoglycemia, and the symptoms are more consistent with **increased ICP**.
- Symptoms of hypoglycemia (e.g., tremors, sweating, hunger, anxiety) are different from the patient's current presentation of confusion and severe headache.
*Pupillary constriction*
- **Pupillary constriction** (miosis) is typically not associated with cerebral edema; instead, **pupillary dilation** (mydriasis) can occur with severe increase in ICP due to uncal herniation.
- The combination of bradycardia, irregular respiration, and hypertension (Cushing's triad) is indicative of increased ICP, which would likely cause pupillary changes related to brainstem compression.
*Pancreatitis*
- Pancreatitis is a known complication of DKA, but it typically presents with **severe abdominal pain**, nausea, and vomiting, rather than cerebral symptoms.
- Although the patient had DKA, the current neurological symptoms point directly to an intracranial process rather than an abdominal issue.
*Peripheral edema*
- **Peripheral edema** results from fluid accumulation in peripheral tissues and is not a direct consequence or expected finding in cerebral edema.
- While fluid administration can cause some peripheral fluid retention, it typically does not lead to the acute neurological deterioration seen in this patient.
Type 1 diabetes mellitus US Medical PG Question 4: A 10-year-old boy is brought to the emergency department by his mother due to frequent vomiting, abdominal pain, and weakness. Over the last 5 days, has been noted to have polydipsia and polyuria. Family history is irrelevant. His temperature is 37.1°C (98.7°F), blood pressure is 100/70 mm Hg, and pulse is 110/min. Physical examination reveals no response to verbal commands, sunken eyes, poor skin turgor, and rapid deep respirations. Laboratory results are shown:
Random plasma glucose 420 mg/dL
Serum beta-hydroxybutyrate elevated
Fasting C-peptide undetectable
Antiglutamic acid decarboxylase (GAD) antibodies positive
This patient's condition occurs as a result of which of the following?
- A. Insulin resistance
- B. Starvation
- C. Immune-mediated destruction of pancreatic beta cells (Correct Answer)
- D. Defective synthesis or release of arginine vasopressin
- E. Salicylate poisoning
Type 1 diabetes mellitus Explanation: ***Immune-mediated destruction of pancreatic beta cells***
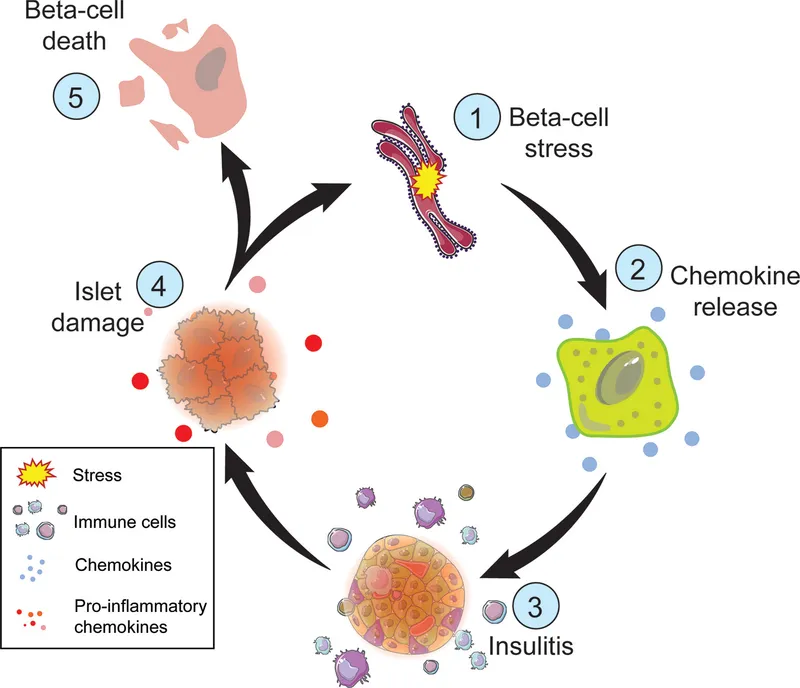
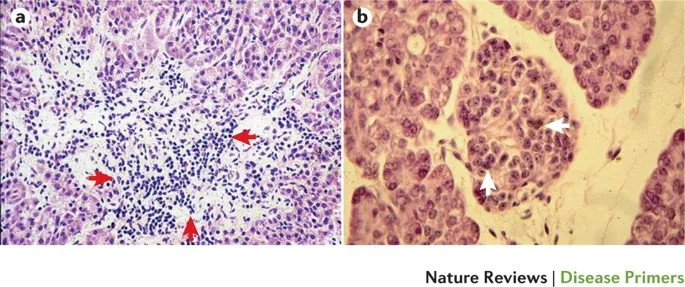
- The diagnosis of **Type 1 Diabetes Mellitus (T1DM)** is strongly supported by the patient's age (10 years old), rapid onset of symptoms (frequent vomiting, abdominal pain, weakness, polydipsia, polyuria), **random plasma glucose of 420 mg/dL**, elevated **serum beta-hydroxybutyrate** (indicating **diabetic ketoacidosis**), and specifically, the **positive antiglutamic acid decarboxylase (GAD) antibodies** and **undetectable fasting C-peptide**.
- **Antiglutamic acid decarboxylase (GAD) antibodies** are a common marker for autoimmune destruction of **pancreatic beta cells**, which leads to **absolute insulin deficiency**. **C-peptide** is a byproduct of insulin synthesis; its absence indicates the pancreas is not producing insulin.
*Insulin resistance*
- **Insulin resistance** is characteristic of **Type 2 Diabetes Mellitus (T2DM)**, which typically presents in older individuals, often with **obesity**, and is not associated with **positive GAD antibodies** or **undetectable C-peptide**.
- In **insulin resistance**, the body produces insulin, often in high amounts initially, but the cells do not respond effectively, leading to hyperglycemia.
*Starvation*
- While **starvation** can lead to **ketogenesis** and signs like weakness, it would typically result in **hypoglycemia** or normal glucose levels, not profound hyperglycemia (420 mg/dL).
- The presence of **polydipsia**, **polyuria**, and positive **GAD antibodies** rules out starvation as the primary cause.
*Defective synthesis or release of arginine vasopressin*
- This describes **diabetes insipidus**, a condition characterized by **polyuria** and **polydipsia** due to impaired water reabsorption by the kidneys.
- However, **diabetes insipidus** is not associated with **hyperglycemia**, **ketosis**, or **positive GAD antibodies** and therefore does not fit the overall clinical picture.
*Salicylate poisoning*
- **Salicylate poisoning** can cause metabolic acidosis (often with a respiratory alkalosis component), vomiting, and altered mental status.
- However, it does not explain the profound **hyperglycemia** and is not associated with **positive GAD antibodies** or undetectable **C-peptide**.
Type 1 diabetes mellitus US Medical PG Question 5: A 13-year-old girl presents after losing consciousness during class 30 minutes ago. According to her friends, she was doing okay since morning, and nobody noticed anything abnormal. The patient’s mother says that her daughter does not have any medical conditions. She also says that the patient has always been healthy but has recently lost weight even though she was eating as usual. Her vital signs are a blood pressure of 100/78 mm Hg, a pulse of 89/min, and a temperature of 37.2°C (99.0°F). Her breathing is rapid but shallow. Fingerstick glucose is 300 mg/dL. Blood is drawn for additional lab tests, and she is started on intravenous insulin and normal saline. Which of the following HLA subtypes is associated with this patient’s most likely diagnosis?
- A. DR3 (Correct Answer)
- B. A3
- C. B8
- D. DR5
- E. B27
Type 1 diabetes mellitus Explanation: ***DR3***
- The patient's presentation with **recent weight loss despite normal eating**, rapid but shallow breathing (**Kussmaul respiration** hinting at **metabolic acidosis**), elevated blood glucose (300 mg/dL), and loss of consciousness strongly suggests **Type 1 Diabetes Mellitus (T1DM)** presenting as **diabetic ketoacidosis (DKA)**.
- **HLA-DR3** and **HLA-DR4** are the primary genetic markers most strongly associated with an increased susceptibility to Type 1 Diabetes Mellitus, an **autoimmune disease** affecting pancreatic beta cells.
- **HLA-DR3** is the most direct answer as it is one of the two strongest HLA-DR associations with T1DM.
*A3*
- **HLA-A3** is primarily associated with **hemochromatosis**, a disorder of iron metabolism, and is not a common genetic marker for Type 1 Diabetes Mellitus.
- The symptoms described in the patient (weight loss, hyperglycemia, DKA) are not characteristic of hemochromatosis.
*B8*
- **HLA-B8** is actually associated with Type 1 Diabetes Mellitus as part of the **extended haplotype A1-B8-DR3**, which shows strong linkage disequilibrium.
- However, **HLA-B8 is not as directly or specifically associated with T1DM** as the HLA-DR subtypes (DR3 and DR4), which are considered the primary genetic markers.
- When asking about HLA subtypes associated with T1DM, **DR3 or DR4** are the best answers as they show the strongest and most direct association.
- HLA-B8 is also associated with other autoimmune conditions like **myasthenia gravis** and **Graves' disease**.
*DR5*
- While part of the **HLA-DR family**, **HLA-DR5** is less commonly associated with **Type 1 Diabetes Mellitus** compared to DR3 and DR4.
- This subtype is more frequently linked with conditions like **pernicious anemia** or increased risk of certain infections.
*B27*
- **HLA-B27** is strongly associated with **seronegative spondyloarthropathies**, such as **ankylosing spondylitis** and **reactive arthritis**.
- It has no known direct association with **Type 1 Diabetes Mellitus**.
Type 1 diabetes mellitus US Medical PG Question 6: A 56-year-old man presents for a follow-up regarding his management for type 2 diabetes mellitus (DM). He was diagnosed with type 2 DM about 7 years ago and was recently started on insulin therapy because oral agents were insufficient to control his glucose levels. He is currently following a regimen combining insulin lispro and neutral protamine Hagedorn (NPH) insulin. He is taking insulin lispro 3 times a day before meals and NPH insulin once in the morning. He has been on this regimen for about 2 months. He says that his glucose reading at night averages around 200 mg/dL and remains close to 180 mg/dL before his shot of NPH in the morning. The readings during the rest of the day range between 100–120 mg/dL. The patient denies any changes in vision or tingling or numbness in his hands or feet. His latest HbA1C level was 6.2%. Which of the following adjustments to his insulin regimen would be most effective in helping this patient achieve better glycemic control?
- A. Add another dose of insulin lispro in the evening.
- B. Reduce a dose of insulin lispro.
- C. Replace lispro with insulin aspart.
- D. Add insulin glargine to the current regimen.
- E. Add another dose of NPH in the evening. (Correct Answer)
Type 1 diabetes mellitus Explanation: ***Add another dose of NPH in the evening.***
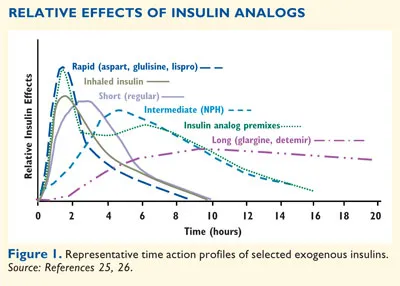
- The patient has persistently elevated **nighttime** and **pre-morning glucose levels** (200 mg/dL and 180 mg/dL, respectively), while daytime levels are well-controlled. This indicates insufficient **basal insulin coverage** overnight.
- Adding a dose of **intermediate-acting NPH insulin** in the evening would provide longer-acting basal insulin to cover the overnight period and address the high morning fasting glucose.
*Add another dose of insulin lispro in the evening.*
- Insulin lispro is a **rapid-acting insulin** primarily used to cover post-prandial glucose spikes. Adding another dose would primarily affect post-dinner glucose, not the sustained overnight hyperglycemia.
- While it might slightly lower evening glucose, its short duration of action would not adequately address the **pre-morning hyperglycemia**.
*Reduce a dose of insulin lispro.*
- The patient's **daytime glucose levels (100–120 mg/dL)** are well-controlled, suggesting that the current lispro doses are appropriate for meal coverage.
- Reducing lispro could lead to **post-prandial hyperglycemia** during the day, worsening overall control.
*Replace lispro with insulin aspart.*
- Both insulin lispro and insulin aspart are **rapid-acting insulins** with very similar pharmacokinetics and duration of action.
- Replacing one with the other would likely not significantly alter the glycemic profile, as the problem lies with **basal insulin coverage**, not rapid-acting insulin.
*Add insulin glargine to the current regimen.*
- While **insulin glargine** is a **long-acting basal insulin** and could address the overnight hyperglycemia, the patient is already on NPH as his basal insulin.
- The simpler and more direct adjustment would be to optimize the **existing NPH regimen** by adding an evening dose, rather than introducing a new type of basal insulin, which might complicate the regimen further or be less cost-effective.
Type 1 diabetes mellitus US Medical PG Question 7: A previously healthy 10-year-old boy is brought to the emergency room by his mother 5 hours after the onset of abdominal pain and nausea. Over the past 2 weeks, he has also had progressive abdominal pain and a 4-kg (8.8-lb) weight loss. The mother reports that her son has been drinking more water than usual during this period. Last week he wet his bed three times despite being completely toilet-trained since 3 years of age. His temperature is 37.8°C (100°F), pulse is 128/min, respirations are 35/min, and blood pressure is 95/55 mm Hg. He appears lethargic. Physical examination shows deep and labored breathing and dry mucous membranes. The abdomen is soft, and there is diffuse tenderness to palpation with no guarding or rebound. Serum laboratory studies show:
Na+ 133 mEq/L
K+ 5.9 mEq/L
Cl- 95 mEq/L
HCO3- 13 mEq/L
Urea nitrogen 25 mg/dL
Creatinine 1.0 mg/dL
Urine dipstick is positive for ketones and glucose. Further evaluation is most likely to reveal which of the following?
- A. Serum glucose concentration > 600 mg/dL
- B. Increased total body sodium
- C. Increased arterial pCO2
- D. Hypervolemia
- E. Decreased total body potassium (Correct Answer)
Type 1 diabetes mellitus Explanation: **Decreased total body potassium**
- Despite **hyperkalemia** on serum labs, patients with **diabetic ketoacidosis (DKA)** often have a **total body potassium deficit** due to increased renal losses and intracellular-to-extracellular shifts.
- The combination of polyuria, vomiting, and acidemia all contribute to significant potassium disturbances.
*Serum glucose concentration > 600 mg/dL*
- A glucose level of **over 600 mg/dL** is more characteristic of **hyperglycemic hyperosmolar state (HHS)**, not typically seen in pediatric DKA.
- While DKA involves hyperglycemia, severe dehydration and altered mentation typically occur at lower glucose thresholds in DKA.
*Increased total body sodium*
- Patients with DKA are typically **hypovolemic and hyponatremic** (even if serum sodium appears normal due to pseudohyponatremia) due to osmotic diuresis caused by hyperglycemia.
- There is no mechanism in DKA that would lead to an increase in total body sodium.
*Increased arterial pCO2*
- The patient's **deep and labored breathing (Kussmaul respirations)** is a compensatory mechanism to **blow off CO2** and correct the metabolic acidosis.
- Therefore, arterial pCO2 would be **decreased**, not increased.
*Hypervolemia*
- **Polyuria** (increased urination) due to osmotic diuresis and poor oral intake typically leads to **hypovolemia and dehydration** in DKA patients.
- The patient exhibits signs of dehydration such as dry mucous membranes, increased pulse, and low blood pressure.
Type 1 diabetes mellitus US Medical PG Question 8: A previously healthy 14-year-old girl is brought to the emergency department by her mother because of abdominal pain, nausea, and vomiting for 6 hours. Over the past 6 weeks, she has also had increased frequency of urination, and she has been drinking more water than usual. She has lost 6 kg (13 lb) over the same time period despite having a good appetite. Her temperature is 37.1°C (98.8°F), pulse is 125/min, respirations are 32/min, and blood pressure is 94/58 mm Hg. She appears lethargic. Physical examination shows deep and labored breathing and dry mucous membranes. The abdomen is soft, and there is diffuse tenderness to palpation with no guarding or rebound. Urine dipstick is positive for ketones and glucose. Further evaluation is most likely to show which of the following findings?
- A. Excess water retention
- B. Serum glucose concentration > 800 mg/dL
- C. Increased arterial pCO2
- D. Increased arterial blood pH
- E. Decreased total body potassium (Correct Answer)
Type 1 diabetes mellitus Explanation: ***Decreased total body potassium***
- This is the correct answer. In **diabetic ketoacidosis (DKA)**, patients have **significant total body potassium depletion** due to osmotic diuresis and urinary losses.
- **Serum potassium may initially appear normal or even elevated** due to acidosis-induced extracellular shift of potassium from cells.
- However, **total body potassium stores are markedly depleted**, and during treatment with insulin and fluids, severe hypokalemia can develop as potassium shifts back intracellularly.
*Excess water retention*
- The patient's symptoms, including **polydipsia**, **polyuria**, and **dry mucous membranes**, indicate **dehydration**, not excessive water retention.
- Her blood pressure of 94/58 mm Hg also suggests **volume depletion**.
*Serum glucose concentration > 800 mg/dL*
- While the patient has significant hyperglycemia (indicated by glucose in urine), **DKA** typically presents with glucose levels between **250-600 mg/dL**.
- Glucose levels >800 mg/dL are more characteristic of **hyperosmolar hyperglycemic state (HHS)**, which is less common in children and usually lacks significant ketosis.
*Increased arterial pCO2*
- The patient exhibits **Kussmaul respirations** (deep and labored breathing) and an increased respiratory rate (32/min), which are compensatory mechanisms for **metabolic acidosis**.
- This compensation leads to **decreased arterial pCO2** as the body tries to blow off CO2 to raise pH.
*Increased arterial blood pH*
- The symptoms, particularly **Kussmaul respirations** and the presence of **ketones** in the urine, strongly suggest **diabetic ketoacidosis (DKA)**.
- DKA is characterized by **severe metabolic acidosis**, meaning the arterial blood pH would be **decreased**, not increased.
Type 1 diabetes mellitus US Medical PG Question 9: A 51-year-old man presents to his physician with increased thirst, frequent urination, and fatigue. These symptoms have increased gradually over the past 3 years. He has no past medical history or current medications. Also, he has no family history of endocrinological or cardiovascular diseases. The blood pressure is 140/90 mm Hg, and the heart rate is 71/min. The patient is afebrile. The BMI is 35.4 kg/m2. On physical examination, there is an increased adipose tissue over the back of the neck, and hyperpigmentation of the axilla and inguinal folds. Which of the following laboratory results is diagnostic of this patient’s most likely condition?
- A. Random plasma glucose 167 mg/dL
- B. Serum insulin level of 10 μU/mL
- C. Plasma glucose of 209 mg/dL 2 hours after the oral glucose load (Correct Answer)
- D. HbA1c 5.9%
- E. Fasting plasma glucose 123 mg/dL
Type 1 diabetes mellitus Explanation: ***Plasma glucose of 209 mg/dL 2 hours after the oral glucose load***
- This value indicates **diabetes mellitus** if the 2-hour plasma glucose is ≥200 mg/dL after a 75-g oral glucose tolerance test (OGTT). The patient's symptoms (thirst, frequent urination, fatigue) and risk factors (obesity, hypertension, acanthosis nigricans) are highly suggestive of type 2 diabetes.
- The elevated BMI, increased adipose tissue in the neck, and **hyperpigmentation** of the axilla and inguinal folds (**acanthosis nigricans**) are strong indicators of **insulin resistance**, a hallmark of type 2 diabetes.
*Random plasma glucose 167 mg/dL*
- A random plasma glucose ≥200 mg/dL with classic symptoms of hyperglycemia (polyuria, polydipsia, unexplained weight loss) is diagnostic of diabetes. A value of 167 mg/dL is **elevated** but, in isolation, without meeting the ≥200 mg/dL threshold for a random test, is **not definitively diagnostic** of diabetes.
- This result would typically warrant further confirmatory testing, such as a fasting plasma glucose or an oral glucose tolerance test.
*Serum insulin level of 10 μU/mL*
- A serum insulin level of 10 μU/mL is within the normal range (typically 2-25 μU/mL). In the setting of **insulin resistance**, patients with type 2 diabetes often have **elevated insulin levels** initially as the pancreas tries to compensate, or normal levels if beta-cell function has declined.
- An isolated insulin level is **not a diagnostic criterion** for diabetes.
*HbA1c 5.9%*
- An HbA1c value between 5.7% and 6.4% indicates **prediabetes**. An HbA1c of ≥6.5% is diagnostic of diabetes.
- While this value suggests impaired glucose regulation, it is **below the diagnostic threshold** for diabetes.
*Fasting plasma glucose 123 mg/dL*
- A fasting plasma glucose between 100 mg/dL and 125 mg/dL indicates **prediabetes** (impaired fasting glucose). A fasting plasma glucose of ≥126 mg/dL is diagnostic of diabetes.
- This value is **below the diagnostic threshold** for diabetes, similar to the HbA1c result, and would indicate prediabetes rather than confirmed diabetes.
Type 1 diabetes mellitus US Medical PG Question 10: A 75-year-old man presents to his primary care physician for foot pain. The patient states that he has had chronic foot pain, which has finally caused him to come and see the doctor. The patient's past medical history is unknown and he has not seen a doctor in over 50 years. The patient states he has led a healthy lifestyle, consumes a plant-based diet, exercised regularly, and avoided smoking, thus his lack of checkups with a physician. The patient lives alone as his wife died recently. His temperature is 98.1°F (36.7°C), blood pressure is 128/64 mmHg, pulse is 80/min, respirations are 13/min, and oxygen saturation is 98% on room air. The patient's BMI is 19 kg/m^2 and he appears healthy. Physical exam demonstrates a right foot that is diffusely swollen, mildly tender, and deformed. The patient's gait is abnormal. Which of the following is associated with the underlying cause of this patient's presentation?
- A. Methicillin-resistant bacterial agent
- B. Unprotected sexual intercourse
- C. Megaloblastic anemia
- D. High-impact trauma to the foot
- E. Hyperfiltration damage of the kidney (Correct Answer)
Type 1 diabetes mellitus Explanation: ***Hyperfiltration damage of the kidney***
- The patient's presentation of a **deformed and diffusely swollen, mildly tender foot** in a 75-year-old, alongside his self-reported healthy lifestyle (plant-based diet, exercise), points toward **Charcot arthropathy (diabetic foot)**, which is typically a complication of **diabetes mellitus**.
- **Hyperfiltration damage of the kidney** is a key early sign of **diabetic nephropathy**, occurring during stages 1 and 2, where the kidneys compensate for damage by increasing the glomerular filtration rate, eventually leading to proteinuria and chronic kidney disease. This is a common association with long-standing, undiagnosed diabetes.
*Methicillin-resistant bacterial agent*
- This typically causes **acute infections**, often with signs of severe inflammation, warmth, erythema, and possibly purulence. The patient's presentation is of **chronic foot pain** and **deformity**, less suggestive of an acute bacterial infection.
- While foot ulcers related to diabetes can become infected with MRSA, the primary underlying cause of the foot deformity and pain is not MRSA itself, but rather the neuropathic and vascular complications of diabetes.
*Unprotected sexual intercourse*
- **Unprotected sexual intercourse** is a risk factor for sexually transmitted infections (STIs) and their sequelae, such as **reactive arthritis**.
- Reactive arthritis typically presents with acute, asymmetric oligoarthritis, often affecting the lower extremities, and usually has associated urethritis or conjunctivitis, which are not mentioned in this chronic, deforming condition.
*Megaloblastic anemia*
- **Megaloblastic anemia** is primarily caused by **vitamin B12 or folate deficiency** and can lead to neurological symptoms like **peripheral neuropathy** (e.g., paresthesias, gait disturbance).
- While peripheral neuropathy can contribute to foot problems, megaloblastic anemia itself does not directly cause the severe **bone and joint destruction** seen in Charcot arthropathy; it's a consequence of diabetic neuropathy.
*High-impact trauma to the foot*
- **High-impact trauma** can cause fractures, dislocations, or acute soft tissue injuries to the foot, leading to pain and swelling.
- However, the patient's presentation is of **chronic pain and progressive deformity**, indicating a degenerative process rather than an acute traumatic injury. While trauma can exacerbate Charcot foot, it's not the underlying cause.
More Type 1 diabetes mellitus US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.