Thyroid function testing US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroid function testing. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroid function testing US Medical PG Question 1: An 18-year-old girl comes to the clinic because she is concerned about her weight. She states that she is on her school’s cheerleading team and is upset because she feels she is the “fattest” girl on the team despite her healthy diet. She says that in the last 2 weeks since practice began, she has lost 2 lbs. The patient has bipolar disorder I. Her medications include lithium and a combined oral contraceptive that was recently started by her gynecologist, because “everyone is on it." Her mother has hypothyroidism and is treated with levothyroxine. The patient’s BMI is 23.2 kg/m2. Thyroid function labs are drawn and shown below:
Thyroid-stimulating hormone (TSH): 4.0 mIU/L
Serum thyroxine (T4): 18 ug/dL
Free thyroxine (Free T4): 1.4 ng/dl (normal range: 0.7-1.9 ng/dL)
Serum triiodothyronine (T3): 210 ng/dL
Free triiodothyronine (T3): 6.0 pg/mL (normal range: 3.0-7.0 pg/mL)
Which of the following is the most likely cause of the patient’s abnormal lab values?
- A. Familial hyperthyroidism
- B. Hypocholesterolemia
- C. Lithium
- D. Oral contraception-induced (Correct Answer)
- E. Surreptitious use of levothyroxine
Thyroid function testing Explanation: ***Oral contraception-induced***
- The patient's **total T4 and T3 are elevated**, while **free T4 and T3** are within normal limits, indicating an increase in thyroid-binding globulin (TBG).
- Oral contraceptives, specifically **estrogen**, increase the synthesis of TBG in the liver, leading to higher total thyroid hormone levels as more hormone is bound.
*Familial hyperthyroidism*
- Familial hyperthyroidism would present with genuinely **elevated free T4 and T3** levels, alongside suppressed TSH, indicating true hyperthyroidism.
- The patient's **normal free T4 and T3** and slightly elevated TSH rule out true hyperthyroidism.
*Hypocholesterolemia*
- While thyroid hormones can affect lipid metabolism, **hypocholesterolemia is not a direct cause** of altered thyroid lab values.
- It is also not a common side effect of oral contraceptives, nor is it related to the specific pattern of elevated total T4/T3 with normal free hormones.
*Lithium*
- Lithium is known to **cause hypothyroidism** (elevated TSH, low T4/T3) or, less commonly, hyperthyroidism, but not isolated elevated total T4/T3 with normal free hormones due to increased TBG.
- The patient's normal free thyroid hormones and only slightly elevated TSH are not consistent with significant lithium-induced thyroid dysfunction.
*Surreptitious use of levothyroxine*
- Surreptitious use of exogenous **levothyroxine** would typically result in suppressed TSH and elevated free T4, as the gland would be overstimulated or shut down.
- The patient's normal free T4 and elevated total T4/T3 are not indicative of levothyroxine abuse.
Thyroid function testing US Medical PG Question 2: A 35-year-old woman presents to the clinic for a several-month history of heat intolerance. She lives in a small apartment with her husband and reports that she always feels hot and sweaty, even when their air conditioning is on high. On further questioning, she's also had a 4.5 kg (10 lb) unintentional weight loss. The vital signs include: heart rate 102/min and blood pressure 150/80 mm Hg. The physical exam is notable for warm and slightly moist skin. She also exhibits a fine tremor in her hands when her arms are outstretched. Which of the following laboratory values is most likely low in this patient?
- A. Triiodothyronine (T3)
- B. Thyroxine (T4)
- C. Calcitonin
- D. Glucose
- E. Thyroid-stimulating hormone (Correct Answer)
Thyroid function testing Explanation: ***Thyroid-stimulating hormone***
- The patient's symptoms (heat intolerance, weight loss, tachycardia, hypertension, warm/moist skin, fine tremor) are classic for **hyperthyroidism**.
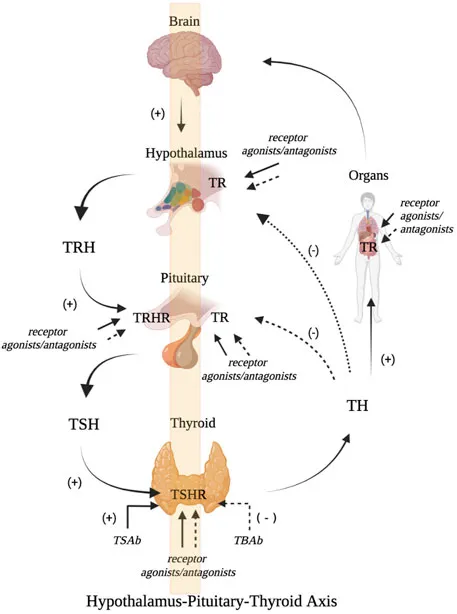
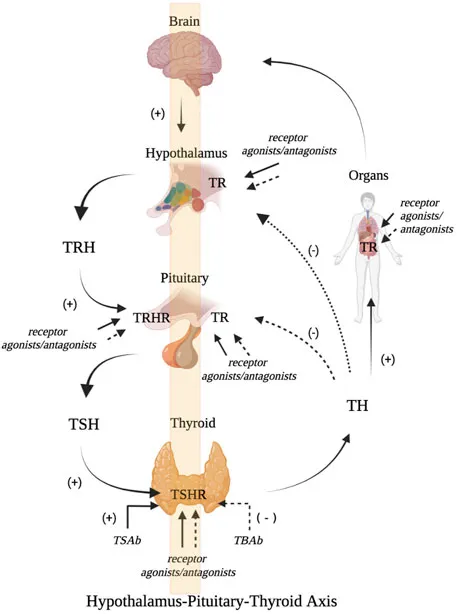
- In primary hyperthyroidism, the thyroid gland overproduces T3 and T4, which **negatively feedbacks** on the pituitary, leading to a **low TSH** level.
*Triiodothyronine (T3)*
- In hyperthyroidism, **T3 levels are typically elevated**, not low, as the thyroid gland is overactive.
- T3 is one of the primary thyroid hormones responsible for the patient's metabolic symptoms.
*Thyroxine (T4)*
- In hyperthyroidism, **T4 levels are typically elevated**, not low, alongside T3.
- T4 is the other key thyroid hormone produced in excess, contributing to the hypermetabolic state.
*Calcitonin*
- Calcitonin is a hormone involved in **calcium regulation** and is produced by the parafollicular C cells of the thyroid gland.
- Its levels are not directly affected by hyperthyroidism and would not be consistently low in this scenario.
*Glucose*
- While hyperthyroidism can affect glucose metabolism, causing increased gluconeogenesis and glycogenolysis, it more commonly leads to **elevated or normal glucose levels**, not consistently low levels.
- Low glucose would typically suggest other conditions like insulinoma or adrenal insufficiency.
Thyroid function testing US Medical PG Question 3: A 30-year-old woman presents to her primary care physician for evaluation of irregular and heavy periods. She also complains of recent fatigue, joint pain, and constipation. Physical exam is notable for thinning eyebrows and recent weight gain. Her temperature is 98.0°F (36.7°C), blood pressure is 140/90 mmHg, 51/min, and respirations are 19/min.
Laboratory studies reveal the following:
Serum:
Na+: 141 mEq/L
K+: 4.3 mEq/L
Cl-: 102 mEq/L
BUN: 15 mg/dL
Glucose: 115 mg/dL
Creatinine: 1.0 mg/dL
Thyroid-stimulating hormone: 11.2 µU/mL
Total T4: 2 ug/dL
Thyroglobulin antibodies: Positive
Anti-thyroid peroxidase antibodies: Positive
Which of the following is this patient at increased risk of in the future?
- A. Papillary carcinoma (Correct Answer)
- B. Subacute thyroiditis
- C. Thyroid lymphoma
- D. Parathyroid adenoma
- E. Thyroid storm
Thyroid function testing Explanation: ***Papillary carcinoma***
- Patients with **Hashimoto's thyroiditis**, as indicated by the elevated **TSH**, low **T4**, and positive **thyroglobulin** and **anti-thyroid peroxidase antibodies**, have an increased risk of developing **papillary thyroid carcinoma**.
- Longstanding stimulation of thyroid follicular cells by elevated TSH levels in Hashimoto's can promote neoplastic changes and increase the risk of thyroid cancer.
*Subacute thyroiditis*
- **Subacute thyroiditis** (De Quervain's thyroiditis) typically presents with **painful thyroid enlargement** and often follows an upper respiratory infection, none of which are described [1].
- It often has a triphasic course with initial hyperthyroidism, followed by hypothyroidism, and then recovery, which is different from this patient's chronic hypothyroid state.
*Thyroid lymphoma*
- While there is an association between **Hashimoto's thyroiditis** and **thyroid lymphoma**, the risk is significantly lower than that for papillary carcinoma.
- Thyroid lymphoma usually presents with a rapidly enlarging, firm thyroid mass and symptoms of compression, which are not present here.
*Parathyroid adenoma*
- A **parathyroid adenoma** causes primary **hyperparathyroidism**, leading to elevated calcium levels and symptoms like bone pain, renal stones, and psychiatric overtone [2].
- The patient's blood pressure is elevated and she has weight gain and fatigue but no signs of hypercalcemia are mentioned, and her current presentation points towards a thyroid disorder.
*Thyroid storm*
- **Thyroid storm** is a life-threatening exacerbation of **hyperthyroidism**, characterized by fever, tachycardia, delirium, and gastrointestinal symptoms [3].
- This patient presents with clear signs and lab findings of **hypothyroidism** (elevated TSH, low T4), making thyroid storm highly unlikely.
Thyroid function testing US Medical PG Question 4: A 48-year-old woman is brought to the emergency department by her family at her psychiatrist's recommendation. According to her family, she has been more restless than her baseline over the past week. The patient herself complains that she feels her mind is racing. Her past medical history is significant for bipolar disorder on lithium and type 1 diabetes mellitus. The family and the patient both assert that the patient has been taking her medications. She denies any recent illness or sick contacts. The patient's temperature is 100°F (37.8°C), blood pressure is 100/60 mmHg, pulse is 130/min, and respirations are 20/min. She appears diaphoretic, and her cardiac exam is notable for an irregularly irregular rhythm with a 2/6 early systolic murmur. Blood counts and metabolic panel are within normal limits. The patient's lithium level is within therapeutic range. Which of the following laboratory tests would be the most useful to include in the evaluation of this patient?
- A. Thyroglobulin level
- B. Thyroid stimulating hormone and total thyroxine levels
- C. Thyrotropin-releasing hormone stimulation test
- D. Triiodothyronine and thyroxine levels
- E. Thyroid stimulating hormone and free thyroxine levels (Correct Answer)
Thyroid function testing Explanation: ***Thyroid stimulating hormone and free thyroxine levels***
- This patient presents with symptoms highly suggestive of **hyperthyroidism**, including **restlessness**, **tachycardia** (pulse 130/min), **diaphoresis**, and a **racing mind**. These symptoms, particularly in a patient on lithium (which can induce thyroid dysfunction), necessitate a thorough thyroid evaluation.
- While total T4 can be influenced by protein binding, **free T4** is the active form of the hormone and provides a more accurate assessment of thyroid status, along with **TSH** as the primary screening test.
*Thyroglobulin level*
- **Thyroglobulin** is primarily used as a tumor marker in the follow-up of patients treated for differentiated thyroid cancer to detect recurrence.
- It is not a primary diagnostic test for hyperthyroidism and would not be the most useful initial test in this scenario.
*Thyroid stimulating hormone and total thyroxine levels*
- While TSH and total T4 are used, **total T4** levels can be affected by changes in **thyroid-binding globulin (TBG)**, which can be altered by various conditions or medications (e.g., estrogen, liver disease).
- Therefore, **free thyroxine** provides a more accurate reflection of thyroid function than total thyroxine.
*Thyrotropin-releasing hormone stimulation test*
- A **TRH stimulation test** is primarily used to investigate subtle abnormalities in the hypothalamic-pituitary-thyroid axis, often when other thyroid function tests are equivocal.
- It is not a first-line diagnostic test for overt hyperthyroidism and would be overly complex for initial evaluation of this patient's symptoms.
*Triiodothyronine and thyroxine levels*
- While T3 and T4 levels are part of thyroid function assessment, specifying **free thyroxine** versus total thyroxine is crucial for accuracy.
- **Free T4** levels, along with TSH, are generally the most informative initial tests for diagnosing conditions like hyperthyroidism.
Thyroid function testing US Medical PG Question 5: A 39-year-old female presents to the clinic with the complaints of dry skin for a few months. She adds that she also has constipation for which she started eating vegetables and fruits but with no improvement. She lives with her husband and children who often complain when she turns the air conditioning to high as she cannot tolerate low temperatures. She has gained 5 kgs (11.2 lb) since her last visit 2 months back although her diet has not changed much. Her past medical history is relevant for cardiac arrhythmias and diabetes. She is on several medications currently. Her temperature is 98.6° F (37° C), respirations are 15/min, pulse is 57/min and blood pressure is 132/98 mm Hg. A physical examination is within normal limits. Thyroid function test results are given below:
Serum
TSH: 13.0 μU/mL
Thyroxine (T4): 3.0 μg/dL
Triiodothyronine (T3): 100 ng/dL
Which of the following medications is most likely to be responsible for her symptoms?
- A. Amiodarone (Correct Answer)
- B. Digoxin
- C. Metformin
- D. Theophylline
- E. Warfarin
Thyroid function testing Explanation: ***Amiodarone***
- Amiodarone is a known cause of both **hypothyroidism** and **hyperthyroidism** due to its iodine content and direct toxic effects on the thyroid gland. The patient's symptoms (dry skin, constipation, **cold intolerance**, **weight gain**, bradycardia) and thyroid function tests (high TSH, low T4, low T3) are highly consistent with drug-induced hypothyroidism.
- The patient's history of **cardiac arrhythmias** makes amiodarone a plausible medication she would be taking, as it is a common antiarrhythmic drug.
*Digoxin*
- Digoxin is primarily used to treat **heart failure** and certain arrhythmias, but it does not typically cause thyroid dysfunction.
- Its common side effects include gastrointestinal upset, visual disturbances, and various arrhythmias, which do not align with the patient's predominant symptoms of hypothyroidism.
*Metformin*
- Metformin is an oral hypoglycemic agent used to treat **Type 2 diabetes**, a condition the patient also has.
- It does not have substantial effects on thyroid hormone synthesis or metabolism and is not associated with hypothyroidism or hyperthyroidism.
*Theophylline*
- Theophylline is a bronchodilator used in the treatment of **asthma** and **COPD**.
- It is not known to cause thyroid dysfunction, and its side effects mainly involve the central nervous system, gastrointestinal tract, and cardiovascular system.
*Warfarin*
- Warfarin is an **anticoagulant** prescribed to prevent blood clots.
- It has no direct known interaction with thyroid hormone synthesis or metabolism and is not associated with thyroid dysfunction.
Thyroid function testing US Medical PG Question 6: A 52-year-old male presents to clinic with complaints of anxiety and fatigue for 4 months. He has also been experiencing palpitations, muscle weakness, increased sweating, and an increase in the frequency of defecation. Past medical history is insignificant. He neither consumes alcohol nor smokes cigarettes. His pulse is 104/min and irregular, blood pressure is 140/80 mm Hg. On examination, you notice that he has bilateral exophthalmos. There are fine tremors in both hands. Which of the following results would you expect to see on a thyroid panel?
- A. High TSH; Low T4; Low T3
- B. High TSH; High T4; High T3
- C. Normal TSH; Low total T4; Normal Free T4 and T3
- D. Low TSH; High T4; High T3 (Correct Answer)
- E. Normal TSH; Low T4; Low T3
Thyroid function testing Explanation: ***Low TSH; High T4; High T3***
- The patient's symptoms (anxiety, fatigue, palpitations, muscle weakness, increased sweating, increased defecation frequency, tachycardia, hypertension, exophthalmos, fine tremors) are classic for **hyperthyroidism**, particularly **Graves' disease**.
- In primary hyperthyroidism, the thyroid gland overproduces T3 and T4, leading to **high levels of T4 and T3**. This then causes a negative feedback loop to the pituitary, resulting in **suppressed (low) TSH** levels.
*High TSH; Low T4; Low T3*
- This pattern is indicative of **primary hypothyroidism**, where the thyroid gland is underactive and cannot produce sufficient T4 and T3, leading to low levels of these hormones and a compensatory rise in TSH.
- The presented symptoms are directly opposite to those seen in hypothyroidism.
*High TSH; High T4; High T3*
- This combination is characteristic of **secondary hyperthyroidism**, which is much rarer and caused by a TSH-secreting pituitary adenoma.
- While it presents with hyperthyroid symptoms, the TSH level would be elevated or inappropriately normal, not suppressed.
*Normal TSH; Low total T4; Normal Free T4 and T3*
- This pattern is often seen in **euthyroid sick syndrome** or conditions causing a decrease in thyroid-binding globulin (TBG).
- The patient's clinical presentation is clearly that of hyperthyroidism, not a euthyroid state.
*Normal TSH; Low T4; Low T3*
- This result is atypical for any specific thyroid disorder and does not align with the patient's symptoms of hyperthyroidism, which demand high circulating thyroid hormone levels.
- A "normal TSH, low T4, low T3" might suggest central hypothyroidism if TSH was inappropriately normal for the low thyroid hormones, but this patient's symptoms definitively point to thyroid hormone excess.
Thyroid function testing US Medical PG Question 7: A 37-year-old woman comes to the physician because of a 2-week history of palpitations and loose stools. She has had a 2.3-kg (5-lb) weight loss over the past month. She has had no change in appetite. She has no history of serious illness. She works in accounting and has been under more stress than usual lately. She takes no medications. She appears pale. Her temperature is 37.8°C (100.1°F), pulse is 110/min, respirations are 20/min, and blood pressure is 126/78 mm Hg. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and nontender. There is a bilateral hand tremor with outstretched arms and a palpable thyroid nodule in the left lobe. Serum laboratory studies show a thyroid stimulating hormone level of 0.03 μU/mL and a thyroxine level of 28 μg/dL. A radioactive iodine uptake scan shows enhancement in a 3-cm encapsulated nodule in the lower left lobe with decreased uptake in the remaining gland. Which of the following is the most likely diagnosis?
- A. Graves' disease
- B. Thyroid storm
- C. Toxic adenoma (Correct Answer)
- D. Papillary carcinoma
- E. Goiter
Thyroid function testing Explanation: ***Toxic adenoma***
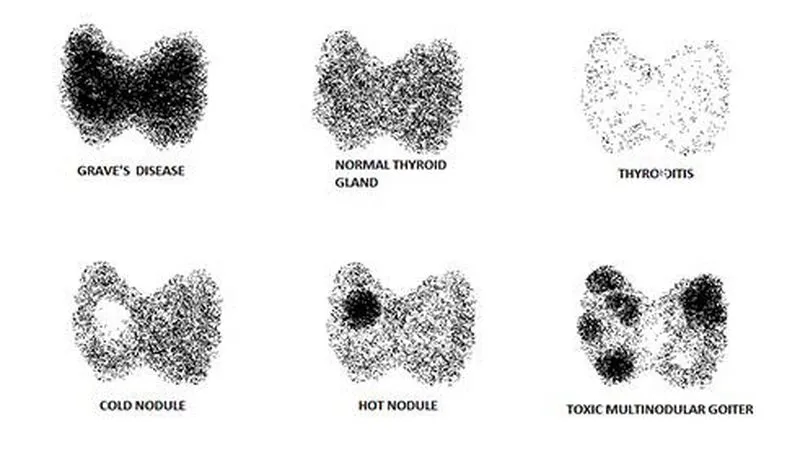
- The combination of **hyperthyroidism** (low TSH, high thyroxine, palpitations, weight loss, tremor) and a **single, hot nodule** on radioactive iodine uptake scan with suppressed uptake in the surrounding gland is classic for a toxic adenoma.
- A **toxic adenoma** is a benign tumor that functions autonomously, producing thyroid hormones independent of TSH regulation.
*Graves' disease*
- While Graves' disease also causes hyperthyroidism, it typically presents with **diffuse uptake** of radioactive iodine throughout the entire gland, not a single hot nodule.
- Classic features like **exophthalmos** or **pretibial myxedema** are also absent in this case.
*Thyroid storm*
- This is a **life-threatening exacerbation of hyperthyroidism** characterized by fever, marked tachycardia, arrhythmias, altered mental status, and potentially coma.
- While the patient has some hyperthyroid symptoms, her presentation is not severe enough to be classified as a thyroid storm.
*Papillary carcinoma*
- Thyroid cancers, including **papillary carcinoma**, are typically **"cold" nodules** on radioactive iodine uptake scans, meaning they do not take up iodine.
- The patient's nodule is "hot" and associated with hyperthyroidism, making carcinoma highly unlikely.
*Goiter*
- A **goiter** refers to any enlargement of the thyroid gland, which can be diffuse or nodular, and may or may not be associated with functional abnormalities.
- While the patient has a palpable nodule, "goiter" is a descriptive term and does not specify the underlying cause of her hyperthyroidism.
Thyroid function testing US Medical PG Question 8: A 23-year-old male presents with complaints of polydipsia and frequent, large-volume urination. Laboratory testing does not demonstrate any evidence of diabetes; however, a reduced urine osmolality of 120 mOsm/L is measured. Which of the following findings on a desmopressin test would be most consistent with a diagnosis of central diabetes insipidus?
- A. Reduction in urine osmolality to 60 mOsm/L following desmopressin administration
- B. No detectable change in urine osmolality following desmopressin administration
- C. Increase in urine osmolality to 400 mOsm/L following desmopressin administration (Correct Answer)
- D. Increase in urine osmolality to 130 mOsm/L following desmopressin administration
- E. Reduction in urine osmolality to 110 mOsm/L following desmopressin administration
Thyroid function testing Explanation: ***Increase in urine osmolality to 400 mOsm/L following desmopressin administration***
- In **central diabetes insipidus**, the kidneys are still able to respond to **vasopressin** (ADH), but the body doesn't produce enough of it. Therefore, administering **desmopressin** (a synthetic ADH analog) will significantly increase **urine osmolality** as the kidneys resorb more water.
- A significant increase, such as from 120 mOsm/L to 400 mOsm/L, indicates that the underlying problem is a lack of ADH production, characteristic of **central diabetes insipidus**.
*Increase in urine osmolality to 130 mOsm/L following desmopressin administration*
- A minor increase from 120 mOsm/L to 130 mOsm/L following desmopressin administration would suggest that the kidneys are largely **unresponsive** to ADH, which is characteristic of **nephrogenic diabetes insipidus**.
- In central diabetes insipidus, a more substantial increase in **urine osmolality** is expected, as the kidney's ability to respond to ADH is intact.
*Reduction in urine osmolality to 60 mOsm/L following desmopressin administration*
- A reduction in **urine osmolality** after desmopressin administration would be an unexpected and contradictory finding.
- Desmopressin is meant to increase water reabsorption, leading to concentrated urine, not more dilute urine.
*Reduction in urine osmolality to 110 mOsm/L following desmopressin administration*
- Similar to the previous option, a reduction in **urine osmolality** following desmopressin administration is clinically inconsistent with the expected action of ADH.
- This result would not align with either central nor nephrogenic diabetes insipidus scenarios, where an increase or no change, respectively, would be anticipated.
*No detectable change in urine osmolality following desmopressin administration*
- If there is no detectable change or only a very small change in **urine osmolality** after desmopressin administration, it suggests that the kidneys are not responding to ADH.
- This would be consistent with **nephrogenic diabetes insipidus**, where the kidneys themselves are resistant to ADH, rather than central DI, where the problem is ADH deficiency.
Thyroid function testing US Medical PG Question 9: A 29-year-old woman comes to her primary care physician hoping she is pregnant. She reports that she had been taking oral contraceptive pills, but she stopped when she began trying to get pregnant about 7 months ago. Since then she has not had her period. She took a few home pregnancy tests that were negative, but she feels they could be wrong. She says she has gained 4 lbs in the past month, and her breasts feel full. Today, she expressed milk from her nipples. She complains of fatigue, which she attributes to stress at work, and headaches, to which she says “my sister told me she had headaches when she was pregnant.” She denies spotting or vaginal discharge. Her last menstrual period was at age 22, prior to starting oral contraceptive pills. Her medical and surgical history are non-significant. She has no history of sexually transmitted infections. She reports she and her husband are having intercourse 3-4 times a week. Her family history is significant for breast cancer in her mother and an aunt who died of ovarian cancer at 55. On physical examination, no breast masses are appreciated, but compression of the nipples produces whitish discharge bilaterally. A bimanual pelvic examination is normal. A urine pregnancy test is negative. Which of the following is the best initial step in management for this patient?
- A. Magnetic resonance imaging of the head
- B. Pelvic ultrasound
- C. Serum follicle-stimulating hormone/luteinizing hormone ratio
- D. Serum thyroid-stimulating hormone level (Correct Answer)
- E. Mammogram
Thyroid function testing Explanation: ***Serum thyroid-stimulating hormone level***
- The patient presents with **amenorrhea**, **galactorrhea**, and non-specific symptoms like **fatigue** and **headaches**. These symptoms can be indicative of **hypothyroidism**, which can cause hyperprolactinemia and subsequently lead to galactorrhea and menstrual irregularities due to its impact on the hypothalamic-pituitary-gonadal axis.
- **Thyroid-stimulating hormone (TSH)** is a crucial initial test as thyroid dysfunction is a common and treatable cause of these symptoms.
*Magnetic resonance imaging of the head*
- While **prolactinoma** causing hyperprolactinemia could lead to these symptoms and would eventually warrant an MRI, obtaining an MRI too early, before ruling out simpler and more common etiologies like hypothyroidism, is not the best initial step.
- An MRI would be indicated if **prolactin levels are elevated** and other causes, such as hypothyroidism, have been ruled out.
*Pelvic ultrasound*
- A pelvic ultrasound is primarily used to evaluate the **uterus and ovaries** for structural abnormalities.
- Given the patient's symptoms of **galactorrhea** and **amenorrhea** (without a positive pregnancy test), and the normal bimanual exam, a pelvic ultrasound is less likely to identify the primary cause compared to endocrine investigations.
*Serum follicle-stimulating hormone/luteinizing hormone ratio*
- This ratio is typically assessed in cases of **amenorrhea** to evaluate ovarian function or **polycystic ovary syndrome (PCOS)**.
- While relevant for amenorrhea, it does not directly address the prominent symptom of **galactorrhea** which points more towards a pituitary or thyroid issue.
*Mammogram*
- A mammogram is a screening tool for **breast cancer**, and while the patient has a family history, her current symptoms are related to **milk production (galactorrhea)** and **menstrual irregularities**, not suspicious breast masses.
- The physical exam showed no breast masses, and the discharge was bilateral and whitish, making breast cancer less likely as the primary cause of these specific symptoms.
Thyroid function testing US Medical PG Question 10: A 40-year-old woman with a past medical history significant for pernicious anemia and vitiligo presents to the physician with the chief complaints of heat intolerance and frequent palpitations. The patient does not take birth control and her urine pregnancy test is negative today. Physical exam reveals a patient that is hyper-reflexive with a non-tender symmetrically enlarged thyroid gland. You order thyroid function tests for workup. What thyroid function values are most expected?
- A. T4 decreased, free T4 decreased, T3 decreased, TSH decreased
- B. T4 elevated, free T4 normal, T3 elevated, thyroid stimulating hormone (TSH) normal
- C. T4 elevated, free T4 elevated, T3 elevated, TSH elevated
- D. T4 normal, free T4 normal, T3 normal, TSH elevated
- E. T4 elevated, free T4 elevated, T3 elevated, TSH decreased (Correct Answer)
Thyroid function testing Explanation: ***T4 elevated, free T4 elevated, T3 elevated, TSH decreased***
- The patient's symptoms (heat intolerance, palpitations, hyper-reflexia) and signs (non-tender symmetrically enlarged thyroid gland) are classic for **hyperthyroidism**, specifically **Graves' disease** given the autoimmune comorbidities (pernicious anemia, vitiligo).
- In primary hyperthyroidism, the thyroid gland overproduces T3 and T4, leading to **elevated T3 and T4 levels**, which in turn suppress TSH secretion, resulting in a **decreased TSH**.
*T4 decreased, free T4 decreased, T3 decreased, TSH decreased*
- This pattern (low T3, T4, and TSH) is indicative of **central hypothyroidism** (secondary or tertiary hypothyroidism), where the pituitary or hypothalamus is unable to produce sufficient TSH.
- This contrasts with the patient's symptoms and signs, which are clearly suggestive of an overactive thyroid gland.
*T4 elevated, free T4 normal, T3 elevated, thyroid stimulating hormone (TSH) normal*
- This combination is not consistent with a typical thyroid disorder scenario. While T4 and T3 could be elevated in hyperthyroidism, a **normal TSH** alongside elevated thyroid hormones is generally anomalous unless there is resistance to thyroid hormones or a TSH-secreting pituitary adenoma.
- The elevated T3 and T4 would typically suppress TSH in primary hyperthyroidism, making a normal TSH unlikely.
*T4 elevated, free T4 elevated, T3 elevated, TSH elevated*
- This pattern (elevated TSH with elevated T3 and T4) is characteristic of **secondary hyperthyroidism**, such as a **TSH-secreting pituitary adenoma**.
- While it represents hyperthyroidism, the patient's presentation with a symmetrically enlarged thyroid and autoimmune history strongly points towards Graves' disease, which is primary hyperthyroidism with suppressed TSH.
*T4 normal, free T4 normal, T3 normal, TSH elevated*
- This profile represents **subclinical hypothyroidism**, where the thyroid hormone levels are within the normal range, but the pituitary is working harder (elevated TSH) to maintain this normal state.
- This contradicts the patient's overt symptoms of hyperthyroidism (heat intolerance, palpitations, hyper-reflexia).
More Thyroid function testing US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.