Pituitary disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pituitary disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pituitary disorders US Medical PG Question 1: A 27-year-old woman, gravida 1, para 1, presents to the obstetrics and gynecology clinic because of galactorrhea, fatigue, cold intolerance, hair loss, and unintentional weight gain for the past year. She had placenta accreta during her first pregnancy with an estimated blood loss of 2,000 mL. Her past medical history is otherwise unremarkable. Her vital signs are all within normal limits. Which of the following is the most likely cause of her symptoms?
- A. Addison’s disease
- B. Sheehan’s syndrome (Correct Answer)
- C. Pituitary adenoma
- D. Hashimoto thyroiditis
- E. Cushing syndrome
Pituitary disorders Explanation: ***Sheehan’s syndrome***
- The patient's history of **placenta accreta** with significant **hemorrhage (2,000 mL)**, followed by symptoms like **galactorrhea, fatigue, cold intolerance, hair loss, and weight gain**, are highly suggestive of Sheehan's syndrome.
- **Sheehan's syndrome** is **ischemic necrosis** of the **pituitary gland** due to massive postpartum hemorrhage, leading to **hypopituitarism** and deficiency of pituitary hormones including **prolactin** (leading to failure of lactation, though galactorrhea can occur if other pituitary hormones are affected), **thyroid-stimulating hormone (TSH)**, and **adrenocorticotropic hormone (ACTH)**.
*Addison’s disease*
- While **fatigue** and **weight loss** can occur, Addison's disease (primary adrenal insufficiency) typically causes **hyperpigmentation**, **hypotension**, and **salt craving**, none of which are mentioned.
- It is due to adrenal gland destruction and does not directly explain galactorrhea or a history linked to postpartum hemorrhage.
*Pituitary adenoma*
- A **prolactin-secreting pituitary adenoma** (prolactinoma) can cause galactorrhea, but the constellation of other symptoms like **cold intolerance** and **fatigue** points to widespread hypopituitarism rather than isolated pituitary dysfunction.
- Although some adenomas can cause hypopituitarism, the history of postpartum hemorrhage is a strong indicator for Sheehan's syndrome.
*Hashimoto thyroiditis*
- **Hashimoto thyroiditis** can explain **fatigue, cold intolerance, hair loss, and weight gain** due to **hypothyroidism**.
- However, it does not typically cause **galactorrhea** or have a direct etiological link to **postpartum hemorrhage**.
*Cushing syndrome*
- **Cushing syndrome** is characterized by symptoms like **central obesity, moon facies, buffalo hump, and striae**, which are not described in this patient.
- It is a state of **cortisol excess**, whereas many of the patient's symptoms (fatigue, cold intolerance, weight gain) are consistent with **hormone deficiencies**.
Pituitary disorders US Medical PG Question 2: A 42-year-old man who is employed as a construction worker presents to his primary care physician with complaints of moderate headaches and profuse sweating. He reports the need to carry up to 3 additional shirt changes to work because they drench quickly even with tasks of low physical exertion. His coworkers have commented about his changing glove and boot sizes, which have increased at least 4 times since he joined the company 10 years ago. Physical examination is unremarkable except for blood pressure of 160/95 mm Hg, hyperhidrosis, noticeably large pores, hypertrichosis, widely spaced teeth, and prognathism. Which of the following best explains the patient’s clinical manifestations?
- A. Increased serum cortisol
- B. Increased thyroid-stimulating hormone
- C. Increased serum metanephrines
- D. Increased serum insulin-like growth factor 1 (IGF-1) (Correct Answer)
- E. Increased serum testosterone
Pituitary disorders Explanation: ***Increased serum insulin-like growth factor 1 (IGF-1)***
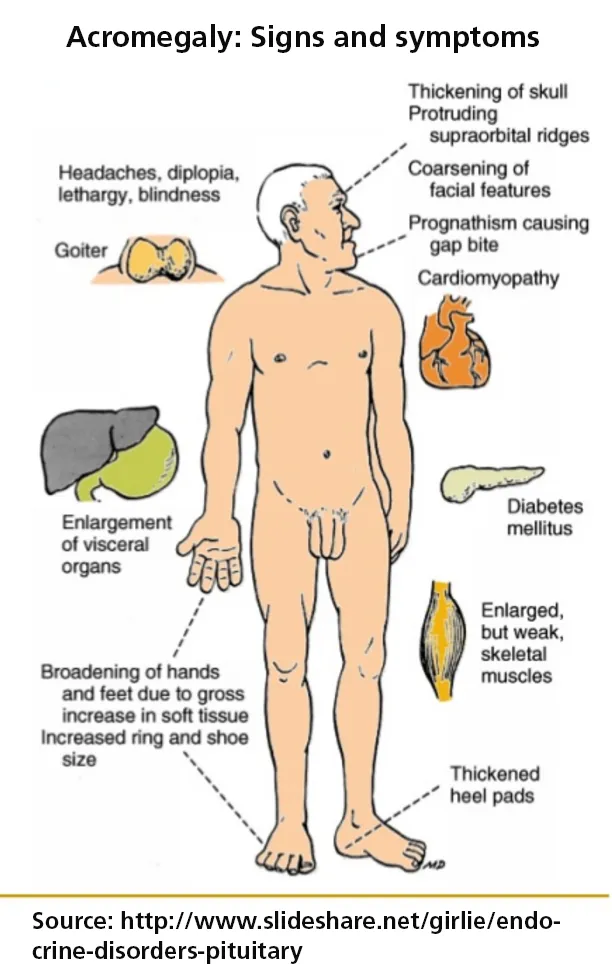
- Elevated **IGF-1** levels are indicative of **acromegaly**, a condition caused by excess growth hormone (GH) secretion, which explains the gradual changes in glove and boot sizes, prognathism, widely spaced teeth, and large pores.
- The symptoms of **profuse sweating**, **hypertrichosis**, **headaches**, and **hypertension** are common clinical manifestations of acromegaly due to the systemic effects of chronic GH excess.
*Increased serum cortisol*
- **Increased cortisol** (Cushing's syndrome) would present with central obesity, moon facies, buffalo hump, and striae, which are not described in the patient.
- While hypertension and hyperhidrosis can occur in Cushing's, the characteristic physical changes related to growth are absent.
*Increased thyroid-stimulating hormone*
- Elevated **TSH** suggests **hypothyroidism**, which would typically cause fatigue, weight gain, cold intolerance, and bradycardia, rather than profuse sweating and hypertension.
- **Hyperthyroidism** (low TSH, high thyroid hormones) can cause sweating and hypertension, but it would not explain the gradual increase in body and appendage size.
*Increased serum metanephrines*
- Elevated **metanephrines** are a hallmark of **pheochromocytoma**, which typically presents with paroxysmal episodes of hypertension, palpitations, and sweating.
- While sweating and hypertension are present, the absence of episodic symptoms and the long-term changes in body size make pheochromocytoma less likely.
*Increased serum testosterone*
- **Increased testosterone** in a male would typically lead to increased muscle mass, acne, and potentially male-pattern baldness, but not the specific skeletal and soft tissue growth patterns observed, such as increased shoe and glove size or prognathism.
- While some skin changes might occur, **hyperhidrosis** and the dramatic facial and extremity changes are not characteristic features of testosterone excess.
Pituitary disorders US Medical PG Question 3: A 61-year-old male presents to an urgent care clinic with the complaints of pain in his joints and recurrent headaches for a month. He is also currently concerned about sweating excessively even at room temperature. His wife, who is accompanying him, adds that his facial appearance has changed over the past few years as he now has a protruding jaw and a prominent forehead and brow ridge. His wedding ring no longer fits his finger despite a lack of weight gain over the last decade. His temperature is 98.6° F (37° C), respirations are 15/min, pulse is 67/min and blood pressure is 122/88 mm Hg. A general physical exam does not show any abnormality. What lab findings are most likely to be seen in this patient?
- A. Elevated cortisol level
- B. Low insulin levels
- C. Elevated TSH and low FT4
- D. Elevated insulin-like growth factor (IGF1) and growth hormone (GH) (Correct Answer)
- E. Elevated prolactin levels
Pituitary disorders Explanation: ***Elevated insulin-like growth factor (IGF1) and growth hormone (GH)***
- The patient's presentation with **acral enlargement** (wedding ring no longer fits), **facial changes** (protruding jaw, prominent forehead), **arthralgias**, **headaches**, and **hyperhidrosis** are classic signs of **acromegaly**, which is caused by excessive growth hormone (GH) secretion, typically from a pituitary adenoma.
- **Elevated IGF-1** is the most reliable screening test for acromegaly because its levels remain stable throughout the day, unlike GH which fluctuates significantly. A **glucose suppression test** for GH is used to confirm the diagnosis.
*Elevated cortisol level*
- **Elevated cortisol** is characteristic of **Cushing's syndrome**, which presents with features such as central obesity, moon facies, buffalo hump, and striae. These signs are not prominent in this patient's presentation.
- While headaches can occur in Cushing's, the **acral and facial changes** are highly specific for acromegaly, not Cushing's.
*Low insulin levels*
- **Low insulin levels** are typically found in **Type 1 diabetes mellitus** due to autoimmune destruction of pancreatic beta cells, or in later stages of Type 2 diabetes.
- The patient's symptoms are not consistent with uncontrolled diabetes, and **high GH** in acromegaly can actually lead to **insulin resistance** and elevated insulin levels, not low.
*Elevated TSH and low FT4*
- This pattern of labs indicates **primary hypothyroidism**, as the thyroid gland is underactive, leading to low thyroid hormone (FT4) and compensatory elevated TSH from the pituitary.
- Symptoms of hypothyroidism include fatigue, cold intolerance, weight gain, and dry skin, which are different from the patient's presentation of **hyperhidrosis** and **acral growth**.
*Elevated prolactin levels*
- **Hyperprolactinemia** can cause symptoms such as **headaches**, galactorrhea, menstrual irregularities (in women), and hypogonadism.
- While headaches are present, the characteristic **acral growth** and **facial changes** seen in this patient are not associated with elevated prolactin, making acromegaly a more fitting diagnosis.
Pituitary disorders US Medical PG Question 4: A 28-year-old patient comes to the physician’s office with complaints of headaches and difficulty seeing out of the corner of her eye. She gave birth to her son 1 year ago. Further visual testing reveals the patient has bitemporal hemianopsia. The patient undergoes brain MRI which shows an anterior pituitary mass, likely adenoma. The patient has her blood tested to see if the adenoma is secreting extra hormone. The patient is found to have a slight excess of a hormone that uptakes a basophilic stain. Which of the following is most likely to be the hormone detected in her blood?
- A. Prolactin
- B. Growth hormone
- C. Thyroid stimulating hormone (Correct Answer)
- D. Antidiuretic hormone
- E. Oxytocin
Pituitary disorders Explanation: ***Thyroid stimulating hormone***
- **Thyroid-stimulating hormone (TSH)** is synthesized by **thyrotroph cells** which are basophilic, making it the most likely hormone to stain basophilically in this context.
- An excess of TSH from a pituitary adenoma could lead to clinical symptoms of **hyperthyroidism**, although the question states it's only a "slight excess."
*Prolactin*
- **Prolactin** is secreted by **lactotrophs**, which are acidophilic and would not take up a basophilic stain.
- While **prolactinomas** are the most common pituitary adenomas, their cells are not basophilic, and this patient does not exhibit common symptoms of hyperprolactinemia (galactorrhea, amenorrhea).
*Growth hormone*
- **Growth hormone (GH)** is produced by **somatotrophs**, which are acidophilic and would not take up a basophilic stain.
- Excess GH typically causes **acromegaly** in adults, characterized by distinctive physical changes not mentioned in the patient's presentation.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)**, also known as vasopressin, is synthesized in the **hypothalamus** and released from the posterior pituitary, not secreted by basophilic cells of the anterior pituitary.
- Overproduction of ADH leads to **SIADH**, characterized by hyponatremia and concentrated urine, none of which are described.
*Oxytocin*
- **Oxytocin** is also produced in the **hypothalamus** and released from the posterior pituitary, not by basophilic cells in the anterior pituitary.
- Its primary functions relate to uterine contractions and milk ejection and are not associated with pituitary adenomas causing bitemporal hemianopsia.
Pituitary disorders US Medical PG Question 5: Four months after giving birth, a young woman presents to the hospital complaining of lack of breast milk secretion. The patient complains of constantly feeling tired. Physical exam reveals that she is slightly hypotensive and has lost a significant amount of weight since giving birth. The patient states that she has not experienced menstruation since the birth. Which of the following is likely to have contributed to this patient's presentation?
- A. Primary empty sella syndrome
- B. Increased anterior pituitary perfusion
- C. Obstetric hemorrhage (Correct Answer)
- D. Pregnancy-induced decrease in anterior pituitary size
- E. Prolactinoma
Pituitary disorders Explanation: ***Obstetric hemorrhage***
- This patient's presentation with **lack of breast milk secretion** (agalactia), **fatigue**, **hypotension**, **weight loss**, and **amenorrhea** after childbirth is characteristic of **Sheehan's syndrome**.
- **Sheehan's syndrome** is caused by ischemic necrosis of the pituitary gland due to **massive obstetric hemorrhage** and subsequent hypovolemic shock, which sensitizes the already hypertrophied pituitary gland to ischemia.
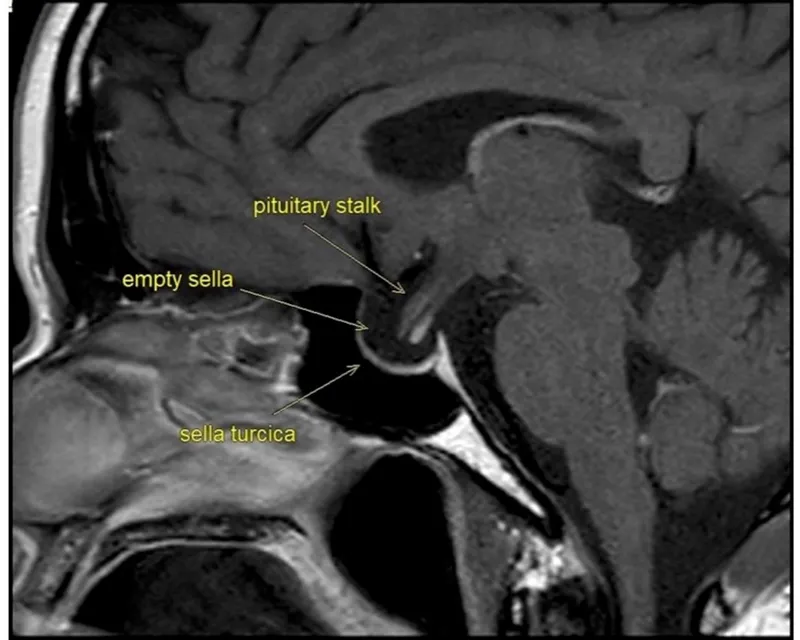
*Primary empty sella syndrome*
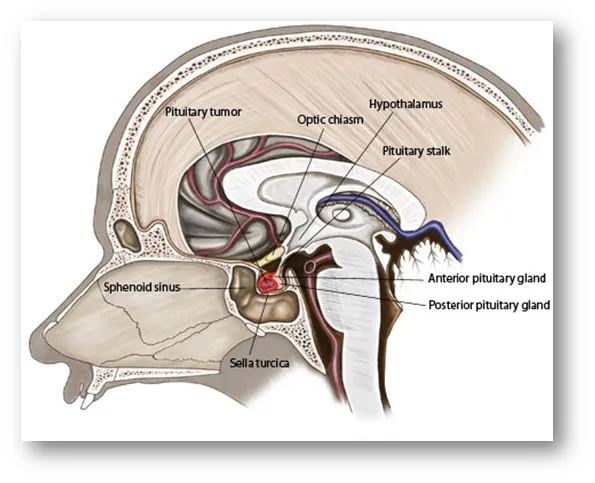
- This condition involves herniation of the **arachnoid mater** and cerebrospinal fluid into the sella turcica, compressing the pituitary gland, but it is typically not associated with a **postpartum hemorrhage**.
- Symptoms are often non-specific or mild, and while it can cause pituitary dysfunction, the timeline and specific symptoms (e.g., agalactia, profound hypotension) do not align with a post-hemorrhage ischemic event.
*Increased anterior pituitary perfusion*
- **Increased perfusion** would generally lead to a healthier, more functional pituitary gland, rather than one suffering from ischemic damage and subsequent hormone deficiencies.
- The symptoms described are indicative of **insufficient pituitary hormone production**, which would be worsened by decreased or compromised perfusion.
*Pregnancy-induced decrease in anterior pituitary size*
- During pregnancy, the anterior pituitary actually **increases significantly in size** (hypertrophy) due to estrogen stimulation to produce prolactin.
- This **enlarged gland** becomes more vulnerable to ischemia if blood supply is compromised, as seen in Sheehan's syndrome.
*Prolactinoma*
- A **prolactinoma** is a benign tumor that would lead to **excessive prolactin production**, causing **galactorrhea** (inappropriate milk production) rather than a lack of breast milk secretion.
- While it can cause amenorrhea due to inhibition of GnRH, the other symptoms like hypotension, weight loss, and fatigue point to widespread pituitary hormone deficiencies, not isolated prolactin excess.
Pituitary disorders US Medical PG Question 6: A 34-year-old woman, who had her first child 2 weeks ago, visits her family physician with concerns about constant fatigue and difficulty with breastfeeding. She was discharged from the intensive care unit after hospitalization for severe postpartum hemorrhage. Since then, she has tried multiple pumps and self-stimulation to encourage breast milk production; however, neither of these strategies has worked. Her blood pressure is 88/56 mm Hg and heart rate is 120/min. Which of the following best explains the underlying condition of this patient?
- A. Pituitary infarction (Correct Answer)
- B. Pituitary infection
- C. Pituitary hemorrhage
- D. Pituitary infiltration by histiocytes
- E. Pituitary stalk epithelial tumor
Pituitary disorders Explanation: ***Pituitary infarction***
- The patient's history of **severe postpartum hemorrhage** causing hypovolemic shock, followed by **fatigue**, **difficulty breastfeeding**, **hypotension**, and **tachycardia**, are classic signs of **Sheehan syndrome**, which is caused by ischemic necrosis (infarction) of the pituitary gland.
- The **lactotroph cells** in the anterior pituitary enlarge significantly during pregnancy, making them more vulnerable to ischemia when blood supply is compromised during hemorrhage.
*Pituitary infection*
- **Pituitary infections** (e.g., abscess) are rare and typically present with symptoms of inflammation such as fever, severe headaches, and meningeal signs, which are not described here.
- While an infection could potentially affect pituitary function, it is not the classic presentation following postpartum hemorrhage.
*Pituitary hemorrhage*
- While postpartum hemorrhage is the cause of the pituitary injury, the **pituitary itself is not hemorrhaging** in Sheehan's syndrome; rather, it is undergoing infarction due to global hypoperfusion.
- **Pituitary apoplexy** (hemorrhage into the pituitary) is an acute event with sudden onset of severe headache, visual disturbances, and rapid endocrine dysfunction, typically not related to postpartum hemorrhage directly in this manner.
*Pituitary infiltration by histiocytes*
- **Histiocytic infiltration** can occur in conditions like Langerhans cell histiocytosis or sarcoidosis, affecting pituitary function.
- However, these conditions have distinct clinical features and are not directly linked to a recent history of postpartum hemorrhage as the precipitating event.
*Pituitary stalk epithelial tumor*
- A **pituitary stalk epithelial tumor** would typically cause symptoms due to mass effect or hormonal imbalances, which might include galactorrhea (if prolactin-secreting) or hypopituitarism over time.
- This scenario does not fit the acute onset of symptoms following postpartum hemorrhage, which points to an ischemic event.
Pituitary disorders US Medical PG Question 7: A 48-year-old female presents to the emergency room with mental status changes.
Laboratory analysis of the patient's serum shows:
Na 122 mEq/L
K 3.9 mEq/L
HCO3 24 mEq/L
BUN 21 mg/dL
Cr 0.9 mg/dL
Ca 8.5 mg/dL
Glu 105 mg/dL
Urinalysis shows:
Osmolality 334 mOsm/kg
Na 45 mEq/L
Glu 0 mg/dL
Which of the following is the most likely diagnosis?
- A. Diabetes insipidus
- B. Aspirin overdose
- C. Primary polydipsia
- D. Diarrhea
- E. Lung cancer (Correct Answer)
Pituitary disorders Explanation: ***Lung cancer***
- The patient presents with **hyponatremia** (Na 122 mEq/L) and **mental status changes**, along with a **euvolemic state** (normal BUN, creatinine, and potassium), which are characteristic of **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **Small cell lung cancer** is a common cause of **ectopic ADH production**, leading to SIADH.
*Diabetes insipidus*
- Characterized by **hypernatremia** and the excretion of **large volumes of dilute urine** (low urine osmolality), which contradicts the patient's hyponatremia and relatively concentrated urine (334 mOsm/kg).
- This condition involves insufficient ADH or renal unresponsiveness to ADH, leading to free water loss, not retention.
*Aspirin overdose*
- Typically causes an **acid-base disturbance**, often a mixed respiratory alkalosis and metabolic acidosis, and may lead to **tinnitus** and **hyperthermia**.
- While it can affect mental status, it does not directly explain the specific pattern of **hyponatremia** and urine osmolality observed.
*Primary polydipsia*
- Usually results in **hyponatremia** due to excessive water intake, but the urine would be **maximally dilute** (urine osmolality < 100 mOsm/kg) as the kidneys try to excrete the excess water.
- The patient's urine osmolality of 334 mOsm/kg indicates that the kidneys are still able to concentrate urine somewhat, making primary polydipsia less likely.
*Diarrhea*
- Causes **volume depletion** and can lead to various electrolyte abnormalities, but typically results in **hypernatremia** or isotonic hyponatremia with signs of dehydration.
- The patient's lab values do not show signs of dehydration or a primary gastrointestinal disturbance.
Pituitary disorders US Medical PG Question 8: A 42-year-old man comes to the physician for the evaluation of episodic headaches involving both temples for 5 months. The patient has been taking acetaminophen, but it has not provided relief. He has also had double vision. Ophthalmic examination shows impaired peripheral vision bilaterally. Contrast MRI of the head shows a 14 x 10 x 8-mm intrasellar mass. Further evaluation is most likely to show which of the following findings?
- A. Polyuria
- B. Impotence (Correct Answer)
- C. Galactorrhea
- D. Macroglossia
- E. Diarrhea
Pituitary disorders Explanation: ***Impotence***
- The patient's symptoms of **headaches**, **double vision**, and **impaired peripheral vision** with a **14x10x8 mm intrasellar mass** are consistent with a **prolactinoma**, the most common functional pituitary adenoma.
- In **men**, hyperprolactinemia from prolactinomas most commonly presents with **hypogonadotropic hypogonadism**, causing **decreased libido**, **erectile dysfunction (impotence)**, and **infertility**.
- Elevated prolactin suppresses **GnRH secretion**, leading to decreased **LH and FSH**, resulting in low testosterone levels and sexual dysfunction.
- **Impotence is the most likely finding** in a male patient with a prolactinoma of this size.
*Galactorrhea*
- While galactorrhea is a classic manifestation of hyperprolactinemia in **women**, it is **rare in men** due to lack of developed breast tissue.
- When it occurs in men, it is usually with very high prolactin levels and is less common than sexual dysfunction.
- This would not be the "most likely" finding in a male patient with prolactinoma.
*Polyuria*
- Polyuria suggests **diabetes insipidus** from posterior pituitary dysfunction or compression of the pituitary stalk.
- While large pituitary masses can cause this, it is not the primary manifestation of a **prolactinoma**.
- More commonly seen with infiltrative lesions or after pituitary surgery.
*Macroglossia*
- **Macroglossia** is a feature of **acromegaly**, caused by excess **growth hormone** secretion from a GH-secreting pituitary adenoma.
- The patient shows no other acromegalic features (frontal bossing, hand/foot enlargement, prognathism).
- Not consistent with the clinical presentation of a prolactinoma.
*Diarrhea*
- Diarrhea is not a typical manifestation of pituitary adenomas including prolactinomas.
- No direct pathophysiologic link between hyperprolactinemia and gastrointestinal symptoms exists.
Pituitary disorders US Medical PG Question 9: A 48-year-old man is brought to the emergency department by his neighbor, who found him lying unconscious at the door of his house. The patient lives alone and no further history is available. On physical examination, his temperature is 37.2ºC (98.9ºF), pulse rate is 114/min, blood pressure is 116/78 mm Hg, and respiratory rate is 22/min. His Glasgow Coma Scale score is 7 and the patient is intubated. A stat serum osmolality is reported at 260 mmol/kg. Based on the provided information, which of the following conditions is most likely present in this patient?
- A. Syndrome of inappropriate antidiuretic hormone (Correct Answer)
- B. Diabetic ketoacidosis
- C. Acute ethanol intoxication
- D. Central diabetes insipidus
- E. Nonketotic hyperosmolar hyperglycemic coma
Pituitary disorders Explanation: ***Syndrome of inappropriate antidiuretic hormone (SIADH)***
- The patient's **unconsciousness** and Glasgow Coma Scale of 7 suggest significant neurological impairment. A serum osmolality of **260 mmol/kg** is low, indicating **hypotonicity** which is characteristic of SIADH due to excess water retention.
- While other causes of altered consciousness exist, the combination of **hyponatremia** (implied by low osmolality) and neurological symptoms points strongly towards SIADH, especially in an unknown medical history setting where various conditions can trigger ADH release.
*Diabetic ketoacidosis (DKA)*
- DKA typically presents with **hyperglycemia**, **acidosis**, and **ketonuria**, which would result in a high serum osmolality, not the low osmolality seen in this patient.
- While DKA can cause altered mental status, the **serum osmolality of 260 mmol/kg** rules it out as the primary cause here.
*Acute ethanol intoxication*
- Acute ethanol intoxication can cause **unconsciousness** and respiratory depression. However, it usually leads to **mild or no change in serum osmolality**, or occasionally a slightly elevated osmolality due to ethanol itself and associated dehydration, not a significantly low value of 260 mmol/kg.
- The physiological changes associated with pure ethanol intoxication do not typically include the marked **hypotonicity** indicated by such a low serum osmolality.
*Central diabetes insipidus*
- Central diabetes insipidus is characterized by an inability to produce ADH, leading to **polyuria**, **polydipsia**, and frequently **hypernatremia** and **high serum osmolality** due to free water loss.
- It would not cause the **hypotonic state** with a serum osmolality of 260 mmol/kg, making it inconsistent with the clinical picture.
*Nonketotic hyperosmolar hyperglycemic coma (NKHHC)*
- NKHHC is characterized by **extreme hyperglycemia** and **severe dehydration**, leading to a much **higher serum osmolality** (typically >320 mOsm/kg) than observed in this patient.
- Although it causes altered mental status, the reported **low serum osmolality of 260 mmol/kg** makes NKHHC an unlikely diagnosis.
Pituitary disorders US Medical PG Question 10: A 38-year-old woman, gravida 2, para 2, is brought to the emergency department by her husband after an episode of unconsciousness. She delivered a healthy infant two weeks ago and the postpartum course was complicated by severe vaginal bleeding, for which she required 4 units of packed red blood cells. Since the blood transfusion, she has had decreased milk production and has felt fatigued. Her pulse is 118/min and blood pressure is 104/63 mm Hg. Her finger-stick glucose concentration is 34 mg/dL. Serum thyroid-stimulating hormone and thyroxine levels are low and the serum sodium level is 132 mEq/L. Which of the following is the most likely cause of this patient's condition?
- A. Lactotrophic adenoma
- B. Hypothalamic infarction
- C. Pituitary ischemia (Correct Answer)
- D. Postpartum thyroiditis
- E. Adrenal hemorrhage
Pituitary disorders Explanation: ***Pituitary ischemia***
- This patient's symptoms are highly suggestive of **Sheehan syndrome**, which results from **ischemic necrosis of the pituitary gland** following massive postpartum hemorrhage. The **severe vaginal bleeding** and subsequent blood transfusion directly support this.
- The **decreased milk production (agalactia)** is due to lack of prolactin, **fatigue** and **low blood pressure** are consistent with adrenal insufficiency (due to ACTH deficiency), and **hypoglycemia** (finger-stick glucose 34 mg/dL), **low TSH and thyroxine** (hypothyroidism), and **hyponatremia** (serum sodium 132 mEq/L) all point to **panhypopituitarism**.
*Lactotrophic adenoma*
- A lactotrophic adenoma (prolactinoma) typically causes **hyperprolactinemia**, leading to **galactorrhea** (milk production outside of lactation) and menstrual irregularities, which is the opposite of this patient's decreased milk production.
- While it can cause headaches and visual field defects, it does not explain the widespread hormonal deficiencies such as hypothyroidism or adrenal insufficiency seen here.
*Hypothalamic infarction*
- Hypothalamic infarction could cause symptoms similar to pituitary dysfunction, as the hypothalamus regulates the pituitary. However, it is a much **rarer cause** of such a constellation of symptoms, especially in the context of recent postpartum hemorrhage.
- The direct connection between **postpartum hemorrhage** and pituitary ischemia makes Sheehan syndrome a more specific and likely diagnosis.
*Postpartum thyroiditis*
- Postpartum thyroiditis is characterized by inflammation of the thyroid gland after delivery, often presenting with a **transient hyperthyroid phase** followed by a hypothyroid phase.
- While it can cause fatigue and mood changes, it would not explain the **decreased milk production**, **hypoglycemia**, **low blood pressure**, or general multi-hormone deficiencies seen in this patient.
*Adrenal hemorrhage*
- Adrenal hemorrhage would lead to **primary adrenal insufficiency** (Addison's crisis), characterized by hypotension, hyponatremia, and hyperkalemia.
- While this patient has hypotension and hyponatremia consistent with adrenal insufficiency, adrenal hemorrhage **does not explain** the **decreased milk production** or the **central hypothyroidism** (low TSH and thyroxine) observed.
More Pituitary disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.