Metabolic bone disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metabolic bone disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metabolic bone disease US Medical PG Question 1: A 65-year-old female with chronic renal failure presents with recent onset of bone pain. Serum analysis reveals decreased levels of calcium and elevated levels of parathyroid hormone. One of the mechanisms driving the elevated PTH is most similar to that seen in:
- A. Decreased functioning of the calcium-sensing receptor (CASR)
- B. Sarcoidosis
- C. Parathyroid adenoma
- D. End stage liver failure
- E. Insufficient Ca intake (Correct Answer)
Metabolic bone disease Explanation: ***Insufficient Ca intake***
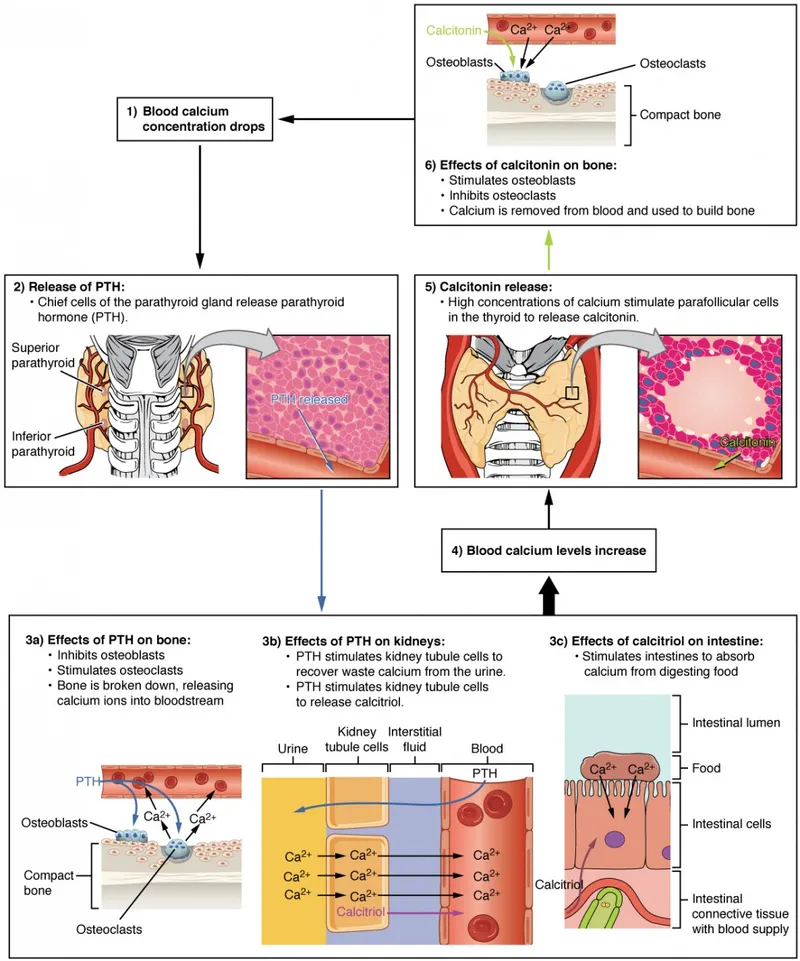
- **Chronic renal failure** impairs the kidney's ability to activate **vitamin D**, leading to **decreased calcium absorption** from the gut.
- This resulting **hypocalcemia** stimulates the parathyroid glands to increase **PTH secretion** to normalize calcium, a response similar to that seen with insufficient dietary calcium intake.
*Decreased functioning of the calcium-sensing receptor (CASR)*
- A dysfunctional CASR would lead to **hypercalcemia** and inappropriately normal or elevated PTH, as the parathyroid gland would not recognize normal or high calcium levels.
- In chronic renal failure, the primary issue is **hypocalcemia** leading to secondary hyperparathyroidism, not a problem with calcium sensing itself.
*Sarcoidosis*
- Sarcoidosis can cause **hypercalcemia** due to extrarenal production of **1,25-dihydroxyvitamin D** (calcitriol) by activated macrophages.
- This condition would typically lead to **suppressed PTH levels**, which is the opposite of the elevated PTH seen in the patient's case.
*Parathyroid adenoma*
- A parathyroid adenoma causes **primary hyperparathyroidism**, characterized by **hypercalcemia** and inappropriately high PTH levels.
- The patient in the vignette presents with **hypocalcemia**, making primary hyperparathyroidism less likely as the direct cause of the elevated PTH.
*End stage liver failure*
- Liver failure can impair **vitamin D hydroxylation** in the liver, leading to **decreased 25-hydroxyvitamin D** levels.
- While this can contribute to hypocalcemia and elevated PTH (secondary hyperparathyroidism), it is distinct from the primary mechanism in renal failure involving the kidney's crucial role in **1-alpha hydroxylation** of vitamin D.
Metabolic bone disease US Medical PG Question 2: A 70-year-old woman presents to the office for a yearly physical. She states she has recently started experiencing pain in her legs and her back. Last year, she experienced a fracture of her left arm while trying to lift groceries. The patient states that she does not consume any dairy and does not go outside often because of the pain in her legs and back. Of note, she takes carbamazepine for seizures. On exam, her vitals are within normal limits. You suspect the patient might have osteomalacia. Testing for which of the following is the next best step to confirm your suspicion?
- A. Vitamin D2 (ergocalciferol)
- B. 25-hydroxyvitamin D (Correct Answer)
- C. Pre-vitamin D3
- D. 1,25-hydroxyvitamin D
- E. 7-dehydrocholesterol
Metabolic bone disease Explanation: ***25-hydroxyvitamin D***
- This is the **best initial test** for evaluating vitamin D deficiency, which leads to **osteomalacia**.
- It reflects the circulating levels of vitamin D and is the **most accurate indicator** of the body's vitamin D stores.
*Vitamin D2 (ergocalciferol)*
- While D2 is a form of vitamin D, measuring only D2 levels is **not sufficient** to assess overall vitamin D status.
- The standard test measures total circulating vitamin D, which includes both D2 and D3, but specifically **25-hydroxyvitamin D** reflects the active usable form.
*Pre-vitamin D3*
- **Pre-vitamin D3** is a precursor molecule formed in the skin from 7-dehydrocholesterol upon UV exposure, and it rapidly isomerizes to vitamin D3.
- It is **not a stable measurable form** in the blood for assessing vitamin D status or diagnosing osteomalacia.
*1,25-hydroxyvitamin D*
- This is the **active hormonal form of vitamin D**, primarily regulated by parathyroid hormone (PTH) and kidney function.
- Levels can be normal or even elevated in early vitamin D deficiency due to increased PTH, making it **less reliable** for initial assessment of deficiency.
*7-dehydrocholesterol*
- **7-dehydrocholesterol** is a precursor molecule in the skin that is converted to pre-vitamin D3 by UV radiation.
- Measuring this precursor is **not clinically significant** for diagnosing osteomalacia or assessing vitamin D deficiency.
Metabolic bone disease US Medical PG Question 3: A 47-year-old African-American woman presents to her primary care physician for a general checkup appointment. She works as a middle school teacher and has a 25 pack-year smoking history. She has a body mass index (BMI) of 22 kg/m^2 and is a vegetarian. Her last menstrual period was 1 week ago. Her current medications include oral contraceptive pills. Which of the following is a risk factor for osteoporosis in this patient?
- A. Smoking history (Correct Answer)
- B. Race
- C. Estrogen therapy
- D. Age
- E. Body mass index
Metabolic bone disease Explanation: ***Smoking history***
- **Smoking** is a well-established risk factor for osteoporosis due to its negative effects on bone density and **calcium absorption**.
- Smokers have lower bone density and increased fracture risk due to direct toxic effects on osteoblasts and accelerated estrogen metabolism.
*Race*
- **African-American women** typically have higher bone mineral density and a lower risk of osteoporosis compared to Caucasians and Asians.
- This patient's racial background is considered a protective factor, not a risk factor, for osteoporosis.
*Estrogen therapy*
- **Oral contraceptive pills** contain estrogen, which helps maintain bone density and is protective against osteoporosis.
- Estrogen deficiency, not estrogen therapy, is a risk factor for osteoporosis, especially after menopause.
*Age*
- While **advancing age** is a significant risk factor for osteoporosis, this patient is 47 years old and still having regular menstrual periods, indicating pre-menopausal status.
- The effects of age on bone density become more pronounced after menopause due to declining estrogen levels.
*Body mass index*
- A **BMI of 22 kg/m^2** is within the normal range, and higher BMI is generally associated with greater bone density due to increased weight bearing and higher estrogen levels in adipose tissue.
- Being underweight (low BMI) is a risk factor for osteoporosis, as it often correlates with poorer nutritional status and lower bone mass.
Metabolic bone disease US Medical PG Question 4: An investigator is studying the effects of hyperphosphatemia on calcium homeostasis. A high-dose phosphate infusion is administered intravenously to a healthy subject over the course of 3 hours. Which of the following sets of changes is most likely to occur in response to the infusion?
$$$ Serum parathyroid hormone %%% Serum total calcium %%% Serum calcitriol %%% Urine phosphate $$$
- A. ↑ ↓ ↓ ↑
- B. ↓ ↑ ↑ ↓
- C. ↑ ↑ ↑ ↑
- D. ↓ ↓ ↓ ↓
- E. ↑ ↑ ↑ ↓
- F. ↑ ↓ ↑ ↑ (Correct Answer)
Metabolic bone disease Explanation: ***↑ ↓ ↑ ↑***
- A high-dose phosphate infusion causes **hyperphosphatemia**, which leads to binding of ionized calcium and results in **hypocalcemia** (decreased serum total calcium).
- The hypocalcemia stimulates the parathyroid glands to secrete **increased PTH**.
- Elevated PTH stimulates 1α-hydroxylase in the kidneys, leading to **increased calcitriol** (active vitamin D) production to enhance intestinal calcium absorption and renal calcium reabsorption.
- Both the high filtered load of phosphate and **PTH's phosphaturic effect** lead to **increased urinary phosphate excretion** as the kidneys attempt to restore phosphate balance.
*↑ ↓ ↓ ↑*
- This option correctly predicts increased PTH and increased urinary phosphate, but incorrectly suggests **decreased calcitriol**.
- PTH stimulation would increase 1α-hydroxylase activity, leading to **increased calcitriol production**, not decreased.
*↓ ↑ ↑ ↓*
- This option incorrectly predicts **decreased PTH** following hyperphosphatemia.
- Hyperphosphatemia causes hypocalcemia, which **stimulates PTH release**, not suppresses it.
- An increase in serum total calcium is also incorrect, as phosphate binds calcium acutely.
*↑ ↑ ↑ ↑*
- While this option correctly predicts increased PTH and calcitriol, it incorrectly suggests **increased serum total calcium**.
- Acute hyperphosphatemia causes calcium-phosphate binding, leading to **decreased ionized and total calcium**, which is the trigger for PTH release.
- However, urinary phosphate would correctly increase in this scenario.
*↓ ↓ ↓ ↓*
- This option is completely incorrect as it suggests all parameters decrease.
- Hyperphosphatemia triggers compensatory mechanisms including **increased PTH and calcitriol**, not decreases.
- Urinary phosphate must **increase** to excrete the excess phosphate load, not decrease.
*↑ ↑ ↑ ↓*
- This option incorrectly combines increased serum total calcium with **decreased urinary phosphate**.
- In hyperphosphatemia, urinary phosphate excretion **must increase** due to both the filtered load and PTH's phosphaturic effect.
- Additionally, acute phosphate binding would **decrease** serum calcium initially, though compensatory mechanisms attempt to restore it.
Metabolic bone disease US Medical PG Question 5: A 64-year-old female presents to her primary care physician for an annual checkup. She states that her health is adequate, but she has not been doing well since her husband died last year. She is able to get by but admits to having trouble caring for herself, cooking, cleaning, and paying her bills. The patient complains of diffuse muscle aches and pains. She has a past medical history of anxiety and seasonal affective disorder. She is not currently taking any medications. On physical exam, you note a gaunt woman with a depressed affect. You note that her body mass index (BMI) and height have both decreased since her last annual visit. On physical exam, her cardiac, pulmonary, and abdominal exams are within normal limits. Lab work is drawn and is as follows:
Serum:
Na+: 135 mEq/L
K+: 3.7 mEq/L
Cl-: 100 mEq/L
HCO3-: 23 mEq/L
Urea nitrogen: 7 mg/dL
Glucose: 70 mg/dL
Creatinine: 0.8 mg/dL
Ca2+: 8.0 mg/dL
Mg2+: 1.5 mEq/L
Parathyroid hormone: 855 pg/mL
Alkaline phosphatase: 135 U/L
Phosphorus: 2.6 mg/dL
Hemoglobin: 14 g/dL
Hematocrit: 36%
Platelet count: 187,000/mm^3
Leukocyte count: 4,700/mm^3
What is the most likely diagnosis?
- A. Hyperparathyroidism
- B. Osteoporosis
- C. Clinical malnutrition
- D. Osteopenia
- E. Osteomalacia (Correct Answer)
Metabolic bone disease Explanation: ***Osteomalacia***
- This patient presents with **diffuse muscle aches and pains**, decreased BMI and height, and laboratory findings of **low calcium (8.0 mg/dL)**, **low phosphorus (2.6 mg/dL)**, and **elevated PTH (855 pg/mL)** and **alkaline phosphatase (135 U/L)**. These are classic signs of osteomalacia, which is often caused by **vitamin D deficiency** leading to impaired bone mineralization.
- The patient's inability to care for herself, cook, and clean following her husband's death may suggest **poor nutritional intake**, increasing her risk for vitamin D deficiency.
*Hyperparathyroidism*
- While **elevated PTH** is present, primary hyperparathyroidism typically causes **hypercalcemia**, not the hypocalcemia seen in this patient.
- Secondary hyperparathyroidism can occur in osteomalacia, but it is a compensatory response to low calcium and vitamin D, not the primary diagnosis.
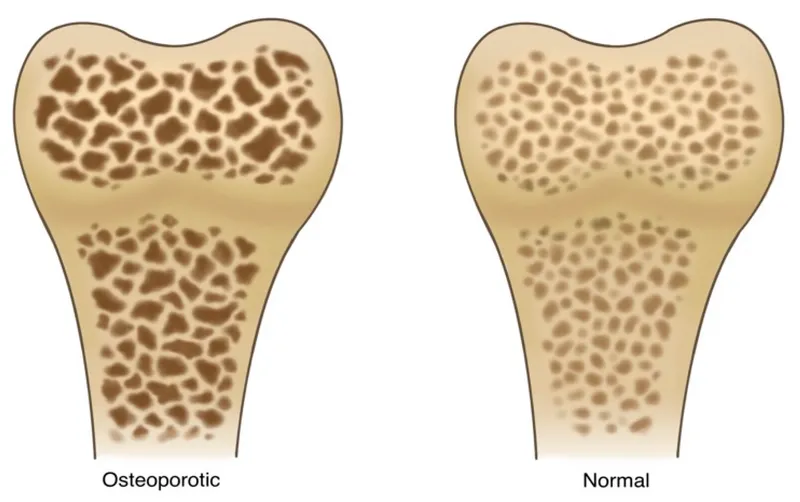
*Osteoporosis*
- Osteoporosis is characterized by **reduced bone density** and increased fracture risk, but it does **not typically involve abnormal calcium, phosphorus, or PTH levels** in this pattern.
- The diffuse muscle aches and pains (myopathy) are more indicative of osteomalacia.
*Clinical malnutrition*
- While the patient exhibits signs of **malnutrition (decreased BMI, poor self-care)**, this is a contributing factor to the underlying bone disease, not the definitive diagnosis explaining the specific biochemical abnormalities.
- Malnutrition can predispose to osteomalacia due to **insufficient vitamin D intake**.
*Osteopenia*
- Osteopenia refers to **lower-than-normal bone mineral density** that is not as severe as osteoporosis.
- Similar to osteoporosis, osteopenia itself does not explain the **hypocalcemia, hypophosphatemia, and markedly elevated PTH** and alkaline phosphatase levels observed in this patient.
Metabolic bone disease US Medical PG Question 6: A 58-year-old man comes to the physician because of a 6-month history of headaches and back pain. Examination shows mild sensorineural hearing loss. Serum concentration of alkaline phosphatase is increased. An x-ray of the skull is shown. The most appropriate pharmacotherapy for this patient is a drug that has which of the following mechanisms of action?
- A. Inhibition of proteasomes
- B. Inhibition of tubulin polymerization
- C. Apoptosis of osteoclasts (Correct Answer)
- D. Formation of DNA strand breaks
- E. Inhibition of nuclear factor-κB
Metabolic bone disease Explanation: ***Apoptosis of osteoclasts***
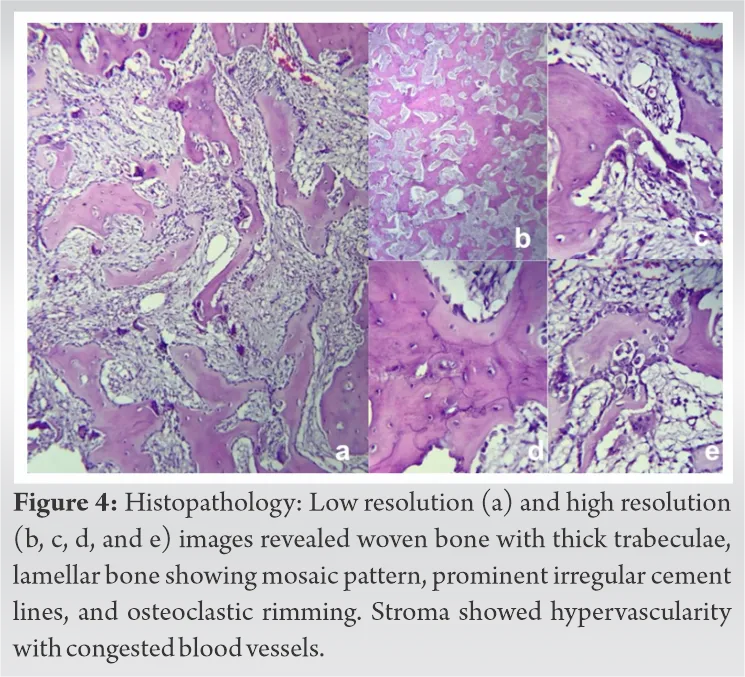
- The patient's symptoms (headaches, back pain, sensorineural hearing loss, elevated alkaline phosphatase) and the skull X-ray showing diffuse sclerosis (\"cotton wool\" appearance) are classic for **Paget's disease of bone**.
- **Bisphosphonates** (which induce osteoclast apoptosis) are the first-line treatment for Paget's disease by reducing abnormal bone turnover.
*Inhibition of proteasomes*
- This mechanism of action is characteristic of drugs like **bortezomib**, which are primarily used in the treatment of **multiple myeloma**.
- Multiple myeloma causes osteolytic lesions and hypercalcemia, but the X-ray findings and overall clinical picture are not consistent with this diagnosis.
*Inhibition of tubulin polymerization*
- Drugs that inhibit tubulin polymerization, such as **colchicine** (for gout) or **vincristine/vinblastine** (for various cancers), prevent cell division and migration.
- This mechanism is not relevant to the pathophysiology or treatment of Paget's disease.
*Formation of DNA strand breaks*
- This is the mechanism of action for certain **chemotherapeutic agents** (e.g., alkylating agents, platinum compounds) that damage DNA to kill rapidly dividing cancer cells.
- Paget's disease is a disorder of bone remodeling, not a primary malignancy requiring such aggressive therapy.
*Inhibition of nuclear factor-κB*
- **NF-κB** is a protein complex that controls transcription of DNA and is involved in immune responses and inflammation.
- While NF-κB inhibitors are being investigated for various inflammatory conditions and cancers, they are not the primary pharmacotherapy for Paget's disease of bone.
Metabolic bone disease US Medical PG Question 7: A 67-year-old male presents with left hip pain. Examination reveals mild effusions in both knees, with crepitus in both patellofemoral joints. He states his hearing has worsened recently and that he feels like his hats don't fit anymore. Bone scan reveals diffuse uptake in the calvarium, right proximal femur, and left ilium. Which of the following laboratory abnormalities would be expected in this patient?
- A. Increased serum calcium
- B. Increased serum alkaline phosphatase (Correct Answer)
- C. Decreased serum alkaline phosphatase
- D. Increased serum parathyroid hormone
- E. Decreased serum parathyroid hormone
Metabolic bone disease Explanation: ***Increased serum alkaline phosphatase***
- The clinical picture (hip pain, worsened hearing, hats not fitting, diffuse bone uptake on scan) is highly suggestive of **Paget's disease of bone**.
- In Paget's disease, there is increased bone turnover with excessive osteoclastic activity followed by compensatory, disorganized osteoblastic activity, leading to a marked elevation in **serum alkaline phosphatase (ALP)**, a marker of osteoblastic activity.
*Increased serum calcium*
- While bone breakdown occurs in Paget's disease, hypercalcemia is uncommon; it usually only occurs in immobilized patients.
- The bone remodeling is typically balanced, with increased formation countering increased resorption.
*Decreased serum alkaline phosphatase*
- Paget's disease is characterized by significantly *increased* bone turnover and osteoblastic activity, leading to **elevated** rather than decreased serum alkaline phosphatase.
- A decreased ALP level would suggest conditions like hypophosphatasia, not Paget's disease.
*Increased serum parathyroid hormone*
- **Primary hyperparathyroidism** would lead to increased PTH, causing hypercalcemia and bone resorption, but the widespread, disorganized bone changes and localized uptake on a bone scan are more consistent with Paget's disease.
- Increased PTH is not a direct consequence or feature of uncomplicated Paget's disease.
*Decreased serum parathyroid hormone*
- This would typically be seen in states of hypercalcemia not driven by PTH, or in conditions like primary hypoparathyroidism.
- There is no direct mechanism in Paget's disease that would cause decreased PTH levels.
Metabolic bone disease US Medical PG Question 8: A 61-year-old woman comes to the physician because of a constant, dull headache and generalized body pains for the past 8 months. She has also had difficulty hearing from her left side, which started a month after the onset of the headaches. Five months ago, she had surgery to correct a fracture of the right femur that occurred without a fall or any significant trauma. Five years ago, she underwent a total thyroidectomy for localized thyroid carcinoma. She takes levothyroxine and calcium supplements, which she started after menopause. Physical examination reveals a prominent forehead and irregular, tender skull surface. Bony tenderness is present over bilateral hip and knee joints, with decreased range of motion of the right hip joint and increased anterior curvature of both tibias. Laboratory studies show a highly elevated level of alkaline phosphatase, with vitamin D, calcium and PTH levels within normal limits. A plain x-ray of the head is most likely to show which of the following findings?
- A. Mixed lytic and sclerotic lesions (Correct Answer)
- B. Periosteal trabeculations with radiolucent marrow hyperplasia
- C. Generalized dense, sclerotic bone
- D. Multiple, well-defined, punched out lytic lesions
- E. Lytic lesions with no sclerotic margin
Metabolic bone disease Explanation: ***Mixed lytic and sclerotic lesions***
- The patient's symptoms (headache, hearing loss, pathological fracture, bony pain, prominent forehead, enlarged skull, increased tibial curvature, and elevated alkaline phosphatase with normal calcium and PTH) are classic for **Paget's disease of bone**.
- **Paget's disease** is characterized by disorganized bone remodeling, which radiographically appears as a mixture of osteolytic (bone destruction) and osteosclerotic (bone formation) lesions, often described as a "cotton wool" appearance in the skull.
*Periosteal trabeculations with radiolucent marrow hyperplasia*
- This finding is more characteristic of conditions like **myelofibrosis**, where there is marrow replacement and extramedullary hematopoiesis, leading to bony changes.
- While Paget's can affect bone structure, it primarily involves remodeling within the bone itself rather than periosteal trabeculations and marrow hyperplasia as a primary radiological feature.
*Generalized dense, sclerotic bone*
- **Osteopetrosis** (Albers-Schönberg disease) is characterized by excessively dense, brittle bones due to defective osteoclast function, leading to generalized sclerosis.
- The clinical presentation with mixed lytic and sclerotic phases, hearing loss, and characteristic bone deformities points away from uniform bone sclerosis.
*Multiple, well-defined, punched out lytic lesions*
- This finding is most suggestive of **multiple myeloma**, a plasma cell malignancy that causes discrete areas of bone destruction without much osteoblastic (bone-forming) activity.
- The patient's symptoms, particularly the prominent forehead, increased tibial curvature, and highly elevated alkaline phosphatase, are not typical of multiple myeloma.
*Lytic lesions with no sclerotic margin*
- This pattern can be seen in aggressive **metastatic bone disease** (e.g., from renal cell carcinoma or thyroid carcinoma, although the patient had a thyroidectomy 5 years ago for localized cancer, making widespread metastases less likely to present this way).
- While Paget's does have lytic phases, the entire clinical picture and the eventual mixed lytic-sclerotic appearance differentiate it from purely lytic, unsclerofed lesions of aggressive metastatic disease.
Metabolic bone disease US Medical PG Question 9: A 55-year-old woman comes to the physician because of a 6-month history of worsening shortness of breath on exertion and fatigue. She has type 1 diabetes mellitus, hypertension, hypercholesterolemia, and chronic kidney disease. Her mother was diagnosed with colon cancer at the age of 65 years. Her blood pressure is 145/92 mm Hg. Examination shows conjunctival pallor. Laboratory studies show:
Hemoglobin 9.2 g/dL
Mean corpuscular volume 88 μm3
Reticulocyte count 0.6 %
Serum
Ferritin 145 ng/mL
Creatinine 3.1 mg/dL
Calcium 8.8 mg/dL
A fecal occult blood test is pending. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Decreased erythropoietin production (Correct Answer)
- B. Chronic occult blood loss
- C. Deficient vitamin B12 intake
- D. Hematopoietic progenitor cell mutation
- E. Autoantibodies against the thyroid gland
Metabolic bone disease Explanation: ***Decreased erythropoietin production***
- The patient's **chronic kidney disease** (CKD) with a creatinine of 3.1 mg/dL is the most likely cause of her **normocytic anemia** and low reticulocyte count. The kidneys produce **erythropoietin (EPO)**, and in CKD, this production is impaired, leading to insufficient stimulation of red blood cell production.
- Her **normocytic anemia** (MCV 88 μm3) and **low reticulocyte count** (0.6%) indicate an underproduction of red blood cells, rather than a problem with cell size or destruction, which is characteristic of anemia of chronic kidney disease.
*Chronic occult blood loss*
- While chronic blood loss can cause anemia, it typically leads to **iron deficiency anemia**, characterized by **microcytic anemia** (low MCV) and **low ferritin** levels. This patient has a normocytic MCV and a normal ferritin level.
- The patient's presentation with **normocytic anemia** and **normal ferritin** makes chronic occult blood loss less likely as the primary cause, even though a fecal occult blood test is pending.
*Deficient vitamin B12 intake*
- Vitamin B12 deficiency causes **macrocytic (megaloblastic) anemia**, characterized by an **elevated MCV** (Mean Corpuscular Volume). This patient has a normocytic MCV (88 μm3).
- Symptoms of vitamin B12 deficiency can also include neurological manifestations, which are not mentioned in this patient's presentation.
*Hematopoietic progenitor cell mutation*
- A **hematopoietic progenitor cell mutation** could lead to conditions like myelodysplastic syndromes or aplastic anemia, which often present with pancytopenia or characteristic abnormal blood cell morphologies.
- The isolated normocytic anemia with a clear underlying cause (CKD) makes a primary bone marrow disorder less likely, especially with a normal ferritin and MCV.
*Autoantibodies against the thyroid gland*
- **Hypothyroidism** due to autoantibodies can cause fatigue, but it typically causes **anemia that is normocytic or macrocytic**, and often linked to iron deficiency or pernicious anemia, or less commonly, directly due to decreased erythropoiesis.
- While fatigue can be a symptom, it would not explain the specific laboratory findings of **normocytic anemia with low reticulocytes in a patient with significant renal failure** as well as decreased erythropoietin production does.
Metabolic bone disease US Medical PG Question 10: An investigator is studying bone metabolism and compares the serum studies and bone biopsy findings of a cohort of women 25–35 years of age with those from a cohort of women 55–65 years of age. Which of the following processes is most likely to be increased in the cohort of older women?
- A. Urinary excretion of cyclic AMP
- B. Expression of RANK ligand (Correct Answer)
- C. Demineralization of bone with normal osteoid matrix
- D. Activation of fibroblast growth factor receptor 3
- E. Urinary excretion of osteocalcin
Metabolic bone disease Explanation: ***Expression of RANK ligand***
- As women age, especially after **menopause**, estrogen levels decline, leading to an **increase in pro-resorptive cytokines**.
- This imbalance promotes increased **RANK ligand (RANKL)** expression, which stimulates **osteoclast differentiation and activity**, resulting in increased bone resorption.
*Urinary excretion of cyclic AMP*
- **Urinary cyclic AMP (cAMP)** is primarily regulated by **parathyroid hormone (PTH)**, which stimulates its excretion.
- While PTH levels can change with age, a direct and significant increase in urinary cAMP excretion is not the most consistent or specific finding representing increased **bone resorption** in older women compared to other options.
*Demineralization of bone with normal osteoid matrix*
- This finding, specifically **normal osteoid matrix** but decreased mineralization, is characteristic of **osteomalacia** (in adults) or rickets (in children).
- This condition is primarily due to **vitamin D deficiency** or impaired phosphate metabolism, not directly due to age-related bone loss in the absence of other underlying pathology.
*Activation of fibroblast growth factor receptor 3*
- **Fibroblast growth factor receptor 3 (FGFR3)** plays a significant role in **endochondral ossification** and is primarily associated with conditions like **achondroplasia** when hyperactivated.
- It does not significantly increase in activity as a normal physiological change in older women contributing to age-related bone loss.
*Urinary excretion of osteocalcin*
- **Osteocalcin** is a marker of **bone formation**, produced by **osteoblasts**.
- While bone turnover increases with age, net bone loss in older women is due to resorption exceeding formation, meaning markers of formation would not typically be *increased* compared to earlier adulthood, or at least not reflect the primary pathology of bone loss.
More Metabolic bone disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.