Hypothyroidism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypothyroidism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypothyroidism US Medical PG Question 1: A 43-year-old woman presents to the physician with the complaint of worsening fatigue over the past several months. She has found that she requires nearly double the amount of coffee consumption each day to stay awake at work and that despite maintaining a balanced, healthy diet, she has experienced significant weight gain. A blood test confirms the presence of anti-thyroid peroxidase antibodies. Which of the following additional findings would be most consistent with the underlying pathophysiology of her condition?
- A. Galactorrhea (Correct Answer)
- B. Constipation
- C. Brisk deep tendon reflexes
- D. Diarrhea
- E. Heat intolerance
Hypothyroidism Explanation: ***Galactorrhea***
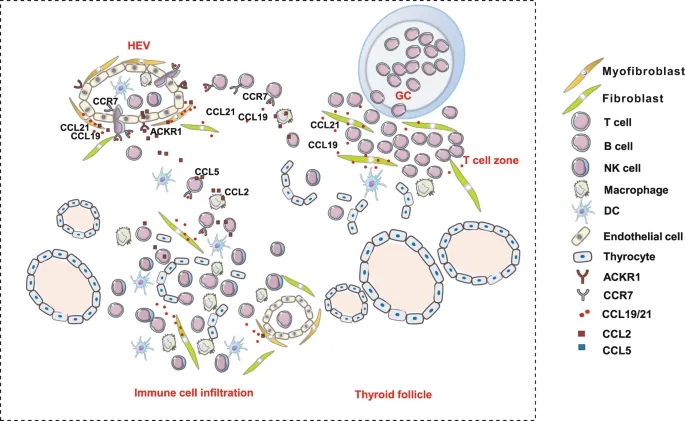
- This patient has **Hashimoto's thyroiditis**, an autoimmune hypothyroidism, given the fatigue, weight gain, and positive **anti-thyroid peroxidase antibodies**.
- **Hypothyroidism** can lead to **hyperprolactinemia** due to increased **TRH** (thyrotropin-releasing hormone), which stimulates both TSH and prolactin release from the anterior pituitary.
- Elevated prolactin can manifest as **galactorrhea**, representing a less commonly recognized endocrine consequence of primary hypothyroidism.
*Constipation*
- **Constipation** is a common symptom of **hypothyroidism** due to decreased gastrointestinal motility.
- While consistent with hypothyroidism, it is a direct consequence of reduced metabolic activity rather than a secondary endocrine effect.
- This is a well-known, expected finding rather than an additional pathophysiologic manifestation.
*Brisk deep tendon reflexes*
- **Hypothyroidism** typically causes **delayed relaxation of deep tendon reflexes** (hung-up reflexes), not brisk reflexes.
- **Brisk reflexes** are characteristic of **hyperthyroidism** due to increased neuromuscular excitability.
*Diarrhea*
- **Diarrhea** is typically associated with **hyperthyroidism** due to increased gastrointestinal motility from elevated metabolic rate.
- **Hypothyroidism** more commonly causes **constipation** due to decreased GI motility.
*Heat intolerance*
- **Heat intolerance** is a classic symptom of **hyperthyroidism** due to an elevated metabolic rate and increased thermogenesis.
- Patients with **hypothyroidism** usually experience **cold intolerance** due to decreased metabolic heat production.
Hypothyroidism US Medical PG Question 2: A 45-year-old woman presents to her primary care provider complaining of daytime drowsiness and fatigue. She reports that she can manage at most a couple of hours of work before needing a nap. She has also noted impaired memory and a 6.8 kg (15 lb) weight gain. She denies shortness of breath, chest pain, lightheadedness, or blood in her stool. At the doctor’s office, the vital signs include: pulse 58/min, blood pressure 104/68 mm Hg, and oxygen saturation 99% on room air. The physical exam is notable only for slightly dry skin. The complete blood count (CBC) is within normal limits. Which of the following is a likely additional finding in this patient?
- A. Tremor
- B. Anxiety
- C. Hypercholesterolemia (Correct Answer)
- D. Lid lag
- E. Palpitations
Hypothyroidism Explanation: ***Hypercholesterolemia***
- The patient's symptoms of **fatigue, weight gain, impaired memory, daytime drowsiness, dry skin, and bradycardia** are classic for **hypothyroidism**.
- **Hypothyroidism** leads to a decrease in the breakdown of **lipids**, resulting in elevated **LDL cholesterol and triglycerides**.
*Tremor*
- A **fine tremor** is commonly associated with **hyperthyroidism**, not hypothyroidism, due to sympathetic overactivity.
- It is a sign of an **overactive metabolic state**, which is the opposite of the patient's presentation.
*Anxiety*
- While anxiety can be a symptom of many conditions, it is more typically associated with **hyperthyroidism** due to increased metabolic activity and sympathetic tone.
- Patients with **hypothyroidism** tend to experience **depression, lethargy, and slowed mentation** rather than anxiety.
*Lid lag*
- **Lid lag** (Graefe's sign) is a classic ophthalmic sign of **hyperthyroidism**, often seen in **Graves' ophthalmopathy**.
- It is caused by increased sympathetic stimulation of the **levator palpebrae superioris muscle**, not a feature of hypothyroidism.
*Palpitations*
- **Palpitations** are a common symptom of **hyperthyroidism** due to increased heart rate and contractility.
- In contrast, **hypothyroidism** is usually associated with **bradycardia** and a *slowed heart rate*, as seen in this patient.
Hypothyroidism US Medical PG Question 3: A 27-year-old G1P0 at 12 weeks estimated gestational age presents for prenatal care. The patient says she has occasional nausea and vomiting and a few episodes of palpitations and diarrhea this last week. Physical examination is unremarkable, except for a heart rate of 145/min. Basic thyroid function tests are shown in the table below. Which of the following additional laboratory tests would be most useful in assessing this patient's condition?
Thyroid-stimulating hormone (TSH)
0.28 mIU/L (0.3–4.5 mIU/L)
Total T4
12 µg/dL (5.4–11.5 µg/dL)
- A. Thyrotropin receptor antibodies (TRAb)
- B. Total triiodothyronine (T3) levels
- C. Thyroid peroxidase (TPO) antibodies
- D. Free thyroxine (T4) levels (Correct Answer)
- E. Thyroxine-binding globulin (TBG) levels
Hypothyroidism Explanation: ***Free thyroxine (T4) levels***
- In pregnancy, **estrogen increases thyroxine-binding globulin (TBG)**, leading to higher **total T4** levels even if free T4 is normal.
- Measuring **free T4 provides a more accurate assessment** of the biologically active thyroid hormone, which is crucial for distinguishing between physiological changes of pregnancy and true hyperthyroidism.
*Thyrotropin receptor antibodies (TRAb)*
- **TRAb are specific for Graves' disease**, which is a cause of hyperthyroidism, but their presence is a confirmatory test after hyperthyroidism has been established.
- The initial step is to confirm the diagnosis of **hyperthyroidism** by evaluating free hormone levels, particularly in pregnancy where total hormone levels are less reliable.
*Total triiodothyronine (T3) levels*
- Similar to total T4, **total T3 levels are also affected by increased TBG in pregnancy**, making them less reliable for initial diagnosis of thyroid dysfunction.
- While T3 is an important thyroid hormone, **free T4 is generally the primary screening test** for hyperthyroidism.
*Thyroid peroxidase (TPO) antibodies*
- **TPO antibodies are indicative of autoimmune thyroiditis**, such as Hashimoto's thyroiditis, which typically causes hypothyroidism, not hyperthyroidism, as suggested by the patient's symptoms and elevated T4.
- Although TPO antibodies can sometimes be positive in Graves' disease, they are **not the primary diagnostic test for active hyperthyroidism**, especially regarding the magnitude of the elevation.
*Thyroxine-binding globulin (TBG) levels*
- While **TBG levels are elevated in pregnancy**, measuring TBG itself doesn't directly assess thyroid function.
- Understanding the physiology of **TBG elevation explains why total T4 is high**, but it doesn't help in determining whether the patient is truly hyperthyroid; for that, free T4 is needed.
Hypothyroidism US Medical PG Question 4: A 49-year-old woman presents to the office because of tremors for 2 months. She says that her hands have been shaking a lot, especially when she feels stressed. In addition, she has been sweating more than usual and has lost 8 kg (17.6 lb) in the last 2 months. She has a past medical history of vitiligo. Her vital signs are a heart rate of 98/min, a respiratory rate of 14/min, a temperature of 37.6°C (99.7°F), and a blood pressure of 115/75 mm Hg. Physical examination shows a fine, bilateral hand tremor and a diffuse goiter. Which of the following hormonal imbalances is most likely present?
- A. Low TSH, high free T4, and high free T3 (Correct Answer)
- B. High TSH, high free T4, and high free T3
- C. High TSH, normal free T4, and normal free T3
- D. Low TSH, normal free T4, and normal free T3
- E. High TSH, low free T4, and low free T3
Hypothyroidism Explanation: ***Low TSH, high free T4, and high free T3***
- The patient's symptoms (tremors, sweating, weight loss, tachycardia, goiter) are classic for **hyperthyroidism**, which is typically characterized by **low TSH** due to negative feedback and **elevated free T4 and T3** levels.
- Her history of **vitiligo**, an autoimmune condition, further supports an autoimmune thyroid disorder like **Graves' disease**, a common cause of hyperthyroidism.
*High TSH, high free T4, and high free T3*
- This pattern would indicate **secondary hyperthyroidism**, caused by a TSH-secreting pituitary adenoma.
- While TSH would be high, it is a much rarer cause of hyperthyroidism compared to primary causes.
*High TSH, normal free T4, and normal free T3*
- This hormonal profile is characteristic of **subclinical hypothyroidism** or a **compensated primary hypothyroidism** early in its course.
- The patient's symptoms are inconsistent with hypothyroidism.
*Low TSH, normal free T4, and normal free T3*
- This suggests **subclinical hyperthyroidism**, where TSH is suppressed but thyroid hormone levels are still within the normal range.
- The patient's prominent and severe symptoms (tremors, significant weight loss, goiter) indicate overt hyperthyroidism, not subclinical disease.
*High TSH, low free T4, and low free T3*
- This is the classic hormonal profile for **primary hypothyroidism**, where the thyroid gland is failing to produce sufficient hormones, leading to elevated TSH.
- The patient's symptoms of nervousness, weight loss, and tremors are directly opposite to those seen in hypothyroidism.
Hypothyroidism US Medical PG Question 5: A 44-year-old woman comes to the physician because of a 6-month history of fatigue, constipation, and a 7-kg (15.4-lb) weight gain. Menses occur irregularly in intervals of 40–50 days. Her pulse is 51/min, and blood pressure is 145/86 mm Hg. Examination shows conjunctival pallor and cool, dry skin. There is mild, nonpitting periorbital edema. Serum thyroid-stimulating hormone concentration is 8.1 μU/mL. Treatment with the appropriate pharmacotherapy is initiated. After several weeks of therapy with this drug, which of the following hormonal changes is expected?
- A. Increased TRH
- B. Increased T3
- C. Decreased T4
- D. Increased T4
- E. Decreased TSH (Correct Answer)
Hypothyroidism Explanation: ***Decreased TSH***
- The patient has **primary hypothyroidism** (elevated TSH 8.1 μU/mL, symptoms of fatigue, constipation, bradycardia, weight gain, cool dry skin) and is treated with **levothyroxine (synthetic T4)**.
- The phrase **"after several weeks of therapy"** is key: while T4 levels rise within days of starting levothyroxine, **TSH takes 6-8 weeks to normalize** due to the negative feedback loop.
- As circulating thyroid hormone levels are restored, the **hypothalamic-pituitary-thyroid axis** re-establishes negative feedback, leading to **decreased TSH secretion** from the pituitary.
- **Decreased TSH is the primary clinical marker** used to assess adequacy of thyroid hormone replacement after several weeks of therapy.
*Increased T4*
- While T4 levels do increase with levothyroxine therapy, this occurs **rapidly (within days)**, not over "several weeks."
- The question's timeframe of "several weeks" directs attention to the **delayed TSH response**, which is what clinicians monitor at 6-8 weeks to adjust dosing.
- T4 elevation is immediate; TSH normalization takes weeks and is the endpoint being tested.
*Increased T3*
- T3 levels will increase as **T4 is peripherally converted to the active form T3**, but this is not the primary hormonal change being monitored after several weeks.
- The question asks about expected hormonal changes in the context of treatment monitoring, where **TSH is the gold standard**.
*Increased TRH*
- **Thyrotropin-releasing hormone (TRH)** from the hypothalamus stimulates TSH release. In primary hypothyroidism, both TRH and TSH are elevated.
- With thyroid hormone replacement, negative feedback would lead to **decreased TRH**, not increased.
*Decreased T4*
- This is the opposite of what occurs with levothyroxine therapy.
- The goal of treatment is to **increase** deficient T4 levels to the physiological range.
Hypothyroidism US Medical PG Question 6: A 54-year-old woman is brought to the emergency department by a nurse 30 minutes after receiving scheduled radiation therapy for papillary thyroid cancer. After the radioisotope was ingested, the physician realized that a much larger fixed dose was given instead of the appropriate dose based on radiation dosimetry. Which of the following pharmacotherapies should be administered immediately to prevent complications from this exposure?
- A. Dexrazoxane
- B. Methimazole
- C. Propylthiouracil
- D. Potassium iodide (Correct Answer)
- E. Mercaptoethanesulfonate
Hypothyroidism Explanation: ***Potassium iodide***
- **Potassium iodide (KI)** is the immediate treatment for **radioactive iodine exposure** and works by saturating the thyroid gland with stable, non-radioactive iodine.
- This **competitive inhibition** prevents the uptake of radioactive iodine-131 by the thyroid, thereby reducing the risk of radiation-induced thyroid damage and cancer.
- **Timing is critical**: KI is most effective when given immediately (within hours) after exposure to radioactive iodine.
- The patient received an overdose of **radioactive iodine-131** (commonly used for papillary thyroid cancer treatment), making immediate KI administration the definitive thyroid protective measure.
*Dexrazoxane*
- **Dexrazoxane** is a **cardioprotective agent** used to reduce cardiotoxicity associated with **anthracycline chemotherapy** (e.g., doxorubicin).
- It chelates iron and prevents formation of anthracycline-iron complexes that generate free radicals.
- It has no role in preventing complications from radioactive iodine exposure.
*Methimazole*
- **Methimazole** is an **antithyroid drug** that inhibits thyroid peroxidase, thereby blocking the **iodination and coupling of tyrosyl residues** in thyroid hormone synthesis.
- While it reduces thyroid hormone production, it does **not prevent uptake** of radioactive iodine by the thyroid gland.
- It is ineffective for acute radiation protection in this scenario.
*Propylthiouracil*
- **Propylthiouracil (PTU)** is another **antithyroid drug** that inhibits thyroid peroxidase and also blocks peripheral conversion of **T4 to T3**.
- Like methimazole, PTU does **not prevent radioactive iodine uptake** by the thyroid.
- It is not indicated for acute radioactive iodine exposure management.
*Mercaptoethanesulfonate*
- **Mercaptoethanesulfonate (MESNA)** is a **uroprotective agent** used to prevent hemorrhagic cystitis caused by **oxazaphosphorine chemotherapy agents** (cyclophosphamide and ifosfamide).
- MESNA binds to and detoxifies acrolein, the toxic metabolite responsible for bladder toxicity.
- It has no role in managing radioactive iodine exposure.
Hypothyroidism US Medical PG Question 7: A 23-year-old woman is brought to the emergency department by her friend because of a 1-hour episode of confusion. Earlier that night, they were at a dance club, and the patient was very energetic and euphoric. Thirty minutes after arriving, she became agitated and nauseous. She no longer seemed to know where she was or how she got there, and she began talking to herself. She has no major medical illness. She is an undergraduate student at a local college. She does not smoke but drinks 10–14 mixed drinks each week. Her temperature is 38.3°C (100.9°F), pulse is 115/min and regular, respirations are 16/min, and blood pressure is 138/84 mm Hg. She oriented to self but not to time or place. Throughout the examination, she grinds her teeth. Her pupils are 7 mm in diameter and minimally reactive. Her skin is diffusely flushed and diaphoretic. Cardiopulmonary examination shows no abnormalities. Serum studies show:
Na+ 129 mEq/L
K+ 3.7 mEq/L
HCO3- 22 mEq/L
Creatinine 1.2 mg/dL
Glucose 81 mg/dL
Which of the following substances is the most likely cause of this patient's presentation?
- A. Ecstasy (Correct Answer)
- B. Cocaine
- C. Acetaminophen
- D. Diphenhydramine
- E. Codeine
Hypothyroidism Explanation: **Ecstasy**
- The patient's **euphoria, confusion, agitation, teeth grinding (bruxism), mydriasis (7 mm pupils), hyperthermia, tachycardia, hypertension, and hyponatremia** are all characteristic of **MDMA (Ecstasy)** intoxication. These symptoms are consistent with its stimulant and serotonergic effects.
- **Hyponatremia** can occur due to increased antidiuretic hormone (ADH) secretion induced by MDMA, combined with excessive fluid intake (often water) by users trying to combat hyperthermia and dehydration.
*Cocaine*
- While cocaine intoxication can cause **euphoria, agitation, tachycardia, hypertension, and mydriasis**, it typically does not cause the prominent **hyponatremia** seen in this patient.
- **Bruxism** and the specific progression to **confusion and talking to herself** are more suggestive of MDMA's serotonergic effects rather than pure dopaminergic stimulation from cocaine.
*Acetaminophen*
- **Acetaminophen overdose** primarily causes **hepatic toxicity**, which would manifest as elevated liver enzymes, nausea, vomiting, and later jaundice.
- It does not induce the **acute neurological symptoms** (euphoria, agitation, confusion, teeth grinding) or the distinctive **vital sign derangements** (hyperthermia, tachycardia, hypertension) observed in this patient.
*Diphenhydramine*
- **Diphenhydramine overdose** (an antihistamine with anticholinergic properties) would typically present with **anticholinergic toxidrome** symptoms, including dry mouth, blurred vision, urinary retention, dilated pupils, fever, and altered mental status (delirium, hallucinations).
- While it can cause confusion and dilated pupils, the prominent **diaphoresis**, **tachycardia**, and **hyponatremia** are less characteristic of isolated diphenhydramine toxicity.
*Codeine*
- **Codeine** is an opioid, and overdose would cause symptoms of **opioid toxidrome**, such as **respiratory depression, miosis (pinpoint pupils)**, central nervous system depression (sedation, coma), and hypotension.
- The patient's symptoms of alertness, agitation, dilated pupils, hypertension, and tachycardia are directly opposite to what would be expected from codeine intoxication.
Hypothyroidism US Medical PG Question 8: Four days into hospitalization for severe pneumonia, a 76-year-old woman suddenly becomes unresponsive. She has no history of heart disease. She is on clarithromycin and ceftriaxone. Her carotid pulse is not detected. A single-lead ECG strip is shown. Previous ECG shows QT prolongation. Laboratory studies show:
Serum
Na+ 145 mEq/L
K+ 6.1 mEq/L
Ca2+ 10.5 mEq/L
Mg2+ 1.8 mEq/L
Thyroid-stimulating hormone 0.1 μU/mL
Cardiopulmonary resuscitation has been initiated. Which of the following is the most likely underlying cause of this patient’s recent condition?
- A. Clarithromycin (Correct Answer)
- B. Hypercalcemia
- C. Thyrotoxicosis
- D. Septic shock
- E. Hyperkalemia
Hypothyroidism Explanation: ***Clarithromycin***
- The patient presents with sudden unresponsiveness and unpalpable carotid pulse, characteristic of **cardiac arrest**, specifically likely due to **Torsades de Pointes (TdP)**, given the history of **QT prolongation** and the ECG findings (not shown but implied by the clinical context).
- **Clarithromycin** is a macrolide antibiotic known to prolong the QT interval and increase the risk of TdP, especially in patients with pre-existing QT prolongation or electrolyte abnormalities.
*Hypercalcemia*
- While **hypercalcemia** can cause cardiac arrhythmias, the provided calcium level (10.5 mEq/L) is only mildly elevated and typically does not precipitate TdP or sudden cardiac arrest in this manner.
- More significant hypercalcemia is usually required to cause severe cardiac manifestations, and its effect on the QT interval is generally to **shorten** it, not prolong it.
*Thyrotoxicosis*
- The patient's **TSH of 0.1 µU/mL** indicates suppressed TSH, consistent with hyperthyroidism or thyrotoxicosis. While thyrotoxicosis can cause arrhythmias, it typically manifests as **atrial fibrillation** or **sinus tachycardia**, not TdP or sudden cardiac arrest in this acute presentation.
- The primary concern here is QT prolongation leading to TdP, which is not a direct or common complication of thyrotoxicosis.
*Septic shock*
- The patient has severe pneumonia and could be at risk of **septic shock**, which can cause cardiovascular collapse. However, the presentation with sudden unresponsiveness, unpalpable pulse, and context of QT prolongation points more specifically to an **arrhythmic cause** rather than generalized circulatory failure as the primary etiology of this acute event.
- While shock can lead to electrolyte disturbances and contribute to cardiac instability, the immediate cause of unresponsiveness is likely an arrhythmia like TdP, which is directly linked to the medication.
*Hyperkalemia*
- The patient's **potassium level of 6.1 mEq/L** indicates significant hyperkalemia, which can indeed cause severe cardiac arrhythmias, including **ventricular fibrillation** and **asystole**.
- However, hyperkalemia typically **shortens the QT interval** and widens the QRS complex, which is opposite to the pre-existing QT prolongation observed before the event.
Hypothyroidism US Medical PG Question 9: A 42-year-old man presents to the clinic for a several-month history of fatigue, and it is starting to affect his work. He often needs to sneak away in the middle of the day to take naps or else he cannot focus and is at risk of falling asleep at his desk. He has been feeling like this for approximately 1 year. Otherwise, he feels healthy and takes no medications. On further questioning, he also had constipation and thinks he has gained some weight. He denies shortness of breath, chest pain, lightheadedness, or blood in his stool. The vital signs include: pulse 56/min, blood pressure 124/78 mm Hg, and oxygen saturation 99% on room air. The physical exam is notable only for slightly dry skin. The complete blood count (CBC) is within normal limits, and the thyroid-stimulating hormone (TSH) is 8.0 μU/mL. Which of the following is the next best treatment for this patient?
- A. Erythropoietin
- B. Prednisone
- C. Packed red blood cell (RBC) transfusion
- D. Levothyroxine (Correct Answer)
- E. Inhaled fluticasone plus salmeterol
Hypothyroidism Explanation: ***Levothyroxine***
- The patient's symptoms of **fatigue**, **weight gain**, **constipation**, **dry skin**, and **bradycardia** are classic for **hypothyroidism**.
- A **TSH level of 8.0 μU/mL**, while not extremely high, indicates **subclinical hypothyroidism** in a symptomatic patient, warranting treatment with **thyroid hormone replacement**.
*Erythropoietin*
- **Erythropoietin** is used to treat **anemia**, particularly in chronic kidney disease, but the patient's **CBC is normal**, making this an inappropriate treatment.
- The patient's fatigue is not due to anemia, as evidenced by a normal CBC.
*Prednisone*
- **Prednisone** is a corticosteroid used for various inflammatory and autoimmune conditions.
- There are no signs or symptoms in this patient to suggest an inflammatory or autoimmune process that would require corticosteroid therapy.
*Packed red blood cell (RBC) transfusion*
- **RBC transfusions** are indicated for severe anemia or acute blood loss.
- The patient's **CBC is normal**, indicating no anemia and therefore no need for a transfusion.
*Inhaled fluticasone plus salmeterol*
- This combination is used to treat **asthma** and **COPD**, which are respiratory conditions.
- The patient denies **shortness of breath** or other respiratory symptoms, making this treatment irrelevant.
Hypothyroidism US Medical PG Question 10: A 41-year-old woman comes to the physician because of a 3-month history of anxiety, difficulty falling asleep, heat intolerance, and a 6-kg (13.2-lb) weight loss. The patient's nephew, who is studying medicine, mentioned that her symptoms might be caused by a condition that is due to somatic activating mutations of the genes for the TSH receptor. Examination shows warm, moist skin and a 2-cm, nontender, subcutaneous mass on the anterior neck. Which of the following additional findings should most raise concern for a different underlying etiology of her symptoms?
- A. Atrial fibrillation
- B. Hyperreflexia
- C. Nonpitting edema (Correct Answer)
- D. Fine tremor
- E. Lid lag
Hypothyroidism Explanation: ***Nonpitting edema***
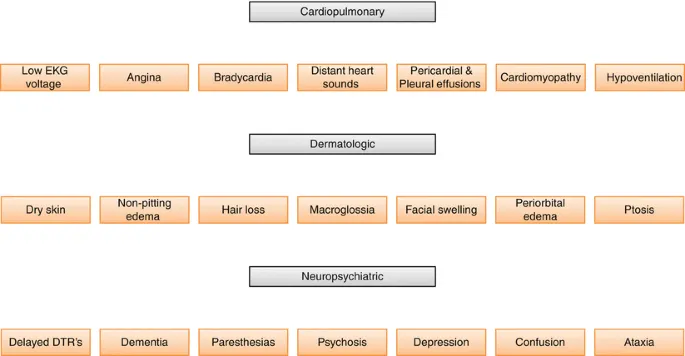
- Nonpitting edema, often referred to as **myxedema**, is a classic sign of **hypothyroidism**, not hyperthyroidism.
- The patient's symptoms (anxiety, insomnia, heat intolerance, weight loss) are indicative of **hyperthyroidism**, making myxedema an inconsistent finding that suggests a different underlying etiology.
*Atrial fibrillation*
- **Atrial fibrillation** is a common cardiovascular manifestation of **hyperthyroidism** due to the direct effects of thyroid hormones on the heart.
- Its presence would support, rather than contradict, the suspected diagnosis of hyperthyroidism.
*Hyperreflexia*
- **Hyperreflexia** is a neurological finding often associated with the hypermetabolic state of **hyperthyroidism**.
- Increased thyroid hormone levels can enhance neural excitability, making hyperreflexia an expected finding.
*Fine tremor*
- A **fine tremor** is a common and characteristic symptom of **hyperthyroidism**, resulting from increased adrenergic activity.
- This finding would be consistent with the patient's other symptoms of thyroid overactivity.
*Lid lag*
- **Lid lag** is an ocular sign of **hyperthyroidism**, caused by sympathetic overstimulation of the Müller's muscle in the eyelid.
- While not indicative of Graves' ophthalmopathy, it is a common finding in thyrotoxicosis and would be consistent with the patient's clinical picture.
More Hypothyroidism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.