Hyperthyroidism and thyroiditis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hyperthyroidism and thyroiditis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hyperthyroidism and thyroiditis US Medical PG Question 1: A 48-year-old woman is brought to the emergency department by her family at her psychiatrist's recommendation. According to her family, she has been more restless than her baseline over the past week. The patient herself complains that she feels her mind is racing. Her past medical history is significant for bipolar disorder on lithium and type 1 diabetes mellitus. The family and the patient both assert that the patient has been taking her medications. She denies any recent illness or sick contacts. The patient's temperature is 100°F (37.8°C), blood pressure is 100/60 mmHg, pulse is 130/min, and respirations are 20/min. She appears diaphoretic, and her cardiac exam is notable for an irregularly irregular rhythm with a 2/6 early systolic murmur. Blood counts and metabolic panel are within normal limits. The patient's lithium level is within therapeutic range. Which of the following laboratory tests would be the most useful to include in the evaluation of this patient?
- A. Thyroglobulin level
- B. Thyroid stimulating hormone and total thyroxine levels
- C. Thyrotropin-releasing hormone stimulation test
- D. Triiodothyronine and thyroxine levels
- E. Thyroid stimulating hormone and free thyroxine levels (Correct Answer)
Hyperthyroidism and thyroiditis Explanation: ***Thyroid stimulating hormone and free thyroxine levels***
- This patient presents with symptoms highly suggestive of **hyperthyroidism**, including **restlessness**, **tachycardia** (pulse 130/min), **diaphoresis**, and a **racing mind**. These symptoms, particularly in a patient on lithium (which can induce thyroid dysfunction), necessitate a thorough thyroid evaluation.
- While total T4 can be influenced by protein binding, **free T4** is the active form of the hormone and provides a more accurate assessment of thyroid status, along with **TSH** as the primary screening test.
*Thyroglobulin level*
- **Thyroglobulin** is primarily used as a tumor marker in the follow-up of patients treated for differentiated thyroid cancer to detect recurrence.
- It is not a primary diagnostic test for hyperthyroidism and would not be the most useful initial test in this scenario.
*Thyroid stimulating hormone and total thyroxine levels*
- While TSH and total T4 are used, **total T4** levels can be affected by changes in **thyroid-binding globulin (TBG)**, which can be altered by various conditions or medications (e.g., estrogen, liver disease).
- Therefore, **free thyroxine** provides a more accurate reflection of thyroid function than total thyroxine.
*Thyrotropin-releasing hormone stimulation test*
- A **TRH stimulation test** is primarily used to investigate subtle abnormalities in the hypothalamic-pituitary-thyroid axis, often when other thyroid function tests are equivocal.
- It is not a first-line diagnostic test for overt hyperthyroidism and would be overly complex for initial evaluation of this patient's symptoms.
*Triiodothyronine and thyroxine levels*
- While T3 and T4 levels are part of thyroid function assessment, specifying **free thyroxine** versus total thyroxine is crucial for accuracy.
- **Free T4** levels, along with TSH, are generally the most informative initial tests for diagnosing conditions like hyperthyroidism.
Hyperthyroidism and thyroiditis US Medical PG Question 2: A 27-year-old G1P0 at 12 weeks estimated gestational age presents for prenatal care. The patient says she has occasional nausea and vomiting and a few episodes of palpitations and diarrhea this last week. Physical examination is unremarkable, except for a heart rate of 145/min. Basic thyroid function tests are shown in the table below. Which of the following additional laboratory tests would be most useful in assessing this patient's condition?
Thyroid-stimulating hormone (TSH)
0.28 mIU/L (0.3–4.5 mIU/L)
Total T4
12 µg/dL (5.4–11.5 µg/dL)
- A. Thyrotropin receptor antibodies (TRAb)
- B. Total triiodothyronine (T3) levels
- C. Thyroid peroxidase (TPO) antibodies
- D. Free thyroxine (T4) levels (Correct Answer)
- E. Thyroxine-binding globulin (TBG) levels
Hyperthyroidism and thyroiditis Explanation: ***Free thyroxine (T4) levels***
- In pregnancy, **estrogen increases thyroxine-binding globulin (TBG)**, leading to higher **total T4** levels even if free T4 is normal.
- Measuring **free T4 provides a more accurate assessment** of the biologically active thyroid hormone, which is crucial for distinguishing between physiological changes of pregnancy and true hyperthyroidism.
*Thyrotropin receptor antibodies (TRAb)*
- **TRAb are specific for Graves' disease**, which is a cause of hyperthyroidism, but their presence is a confirmatory test after hyperthyroidism has been established.
- The initial step is to confirm the diagnosis of **hyperthyroidism** by evaluating free hormone levels, particularly in pregnancy where total hormone levels are less reliable.
*Total triiodothyronine (T3) levels*
- Similar to total T4, **total T3 levels are also affected by increased TBG in pregnancy**, making them less reliable for initial diagnosis of thyroid dysfunction.
- While T3 is an important thyroid hormone, **free T4 is generally the primary screening test** for hyperthyroidism.
*Thyroid peroxidase (TPO) antibodies*
- **TPO antibodies are indicative of autoimmune thyroiditis**, such as Hashimoto's thyroiditis, which typically causes hypothyroidism, not hyperthyroidism, as suggested by the patient's symptoms and elevated T4.
- Although TPO antibodies can sometimes be positive in Graves' disease, they are **not the primary diagnostic test for active hyperthyroidism**, especially regarding the magnitude of the elevation.
*Thyroxine-binding globulin (TBG) levels*
- While **TBG levels are elevated in pregnancy**, measuring TBG itself doesn't directly assess thyroid function.
- Understanding the physiology of **TBG elevation explains why total T4 is high**, but it doesn't help in determining whether the patient is truly hyperthyroid; for that, free T4 is needed.
Hyperthyroidism and thyroiditis US Medical PG Question 3: A 39-year-old female presents to the clinic with the complaints of dry skin for a few months. She adds that she also has constipation for which she started eating vegetables and fruits but with no improvement. She lives with her husband and children who often complain when she turns the air conditioning to high as she cannot tolerate low temperatures. She has gained 5 kgs (11.2 lb) since her last visit 2 months back although her diet has not changed much. Her past medical history is relevant for cardiac arrhythmias and diabetes. She is on several medications currently. Her temperature is 98.6° F (37° C), respirations are 15/min, pulse is 57/min and blood pressure is 132/98 mm Hg. A physical examination is within normal limits. Thyroid function test results are given below:
Serum
TSH: 13.0 μU/mL
Thyroxine (T4): 3.0 μg/dL
Triiodothyronine (T3): 100 ng/dL
Which of the following medications is most likely to be responsible for her symptoms?
- A. Amiodarone (Correct Answer)
- B. Digoxin
- C. Metformin
- D. Theophylline
- E. Warfarin
Hyperthyroidism and thyroiditis Explanation: ***Amiodarone***
- Amiodarone is a known cause of both **hypothyroidism** and **hyperthyroidism** due to its iodine content and direct toxic effects on the thyroid gland. The patient's symptoms (dry skin, constipation, **cold intolerance**, **weight gain**, bradycardia) and thyroid function tests (high TSH, low T4, low T3) are highly consistent with drug-induced hypothyroidism.
- The patient's history of **cardiac arrhythmias** makes amiodarone a plausible medication she would be taking, as it is a common antiarrhythmic drug.
*Digoxin*
- Digoxin is primarily used to treat **heart failure** and certain arrhythmias, but it does not typically cause thyroid dysfunction.
- Its common side effects include gastrointestinal upset, visual disturbances, and various arrhythmias, which do not align with the patient's predominant symptoms of hypothyroidism.
*Metformin*
- Metformin is an oral hypoglycemic agent used to treat **Type 2 diabetes**, a condition the patient also has.
- It does not have substantial effects on thyroid hormone synthesis or metabolism and is not associated with hypothyroidism or hyperthyroidism.
*Theophylline*
- Theophylline is a bronchodilator used in the treatment of **asthma** and **COPD**.
- It is not known to cause thyroid dysfunction, and its side effects mainly involve the central nervous system, gastrointestinal tract, and cardiovascular system.
*Warfarin*
- Warfarin is an **anticoagulant** prescribed to prevent blood clots.
- It has no direct known interaction with thyroid hormone synthesis or metabolism and is not associated with thyroid dysfunction.
Hyperthyroidism and thyroiditis US Medical PG Question 4: A 37-year-old woman comes to the physician because of a 2-week history of palpitations and loose stools. She has had a 2.3-kg (5-lb) weight loss over the past month. She has had no change in appetite. She has no history of serious illness. She works in accounting and has been under more stress than usual lately. She takes no medications. She appears pale. Her temperature is 37.8°C (100.1°F), pulse is 110/min, respirations are 20/min, and blood pressure is 126/78 mm Hg. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and nontender. There is a bilateral hand tremor with outstretched arms and a palpable thyroid nodule in the left lobe. Serum laboratory studies show a thyroid stimulating hormone level of 0.03 μU/mL and a thyroxine level of 28 μg/dL. A radioactive iodine uptake scan shows enhancement in a 3-cm encapsulated nodule in the lower left lobe with decreased uptake in the remaining gland. Which of the following is the most likely diagnosis?
- A. Graves' disease
- B. Thyroid storm
- C. Toxic adenoma (Correct Answer)
- D. Papillary carcinoma
- E. Goiter
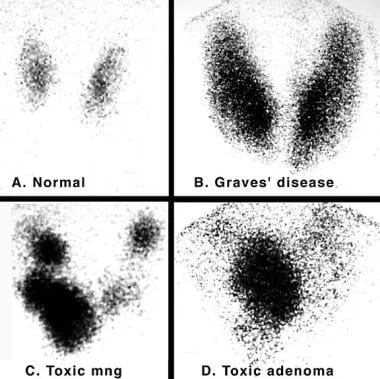
Hyperthyroidism and thyroiditis Explanation: ***Toxic adenoma***
- The combination of **hyperthyroidism** (low TSH, high thyroxine, palpitations, weight loss, tremor) and a **single, hot nodule** on radioactive iodine uptake scan with suppressed uptake in the surrounding gland is classic for a toxic adenoma.
- A **toxic adenoma** is a benign tumor that functions autonomously, producing thyroid hormones independent of TSH regulation.
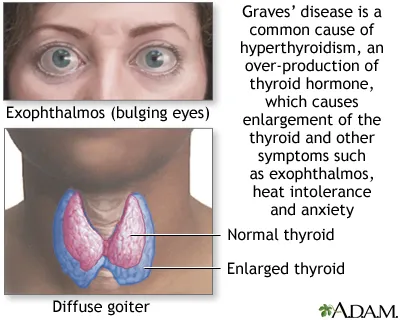
*Graves' disease*
- While Graves' disease also causes hyperthyroidism, it typically presents with **diffuse uptake** of radioactive iodine throughout the entire gland, not a single hot nodule.
- Classic features like **exophthalmos** or **pretibial myxedema** are also absent in this case.
*Thyroid storm*
- This is a **life-threatening exacerbation of hyperthyroidism** characterized by fever, marked tachycardia, arrhythmias, altered mental status, and potentially coma.
- While the patient has some hyperthyroid symptoms, her presentation is not severe enough to be classified as a thyroid storm.
*Papillary carcinoma*
- Thyroid cancers, including **papillary carcinoma**, are typically **"cold" nodules** on radioactive iodine uptake scans, meaning they do not take up iodine.
- The patient's nodule is "hot" and associated with hyperthyroidism, making carcinoma highly unlikely.
*Goiter*
- A **goiter** refers to any enlargement of the thyroid gland, which can be diffuse or nodular, and may or may not be associated with functional abnormalities.
- While the patient has a palpable nodule, "goiter" is a descriptive term and does not specify the underlying cause of her hyperthyroidism.
Hyperthyroidism and thyroiditis US Medical PG Question 5: A 29-year-old woman comes to the physician because of intermittent episodes of sharp chest pain and palpitations. She appears nervous. Her pulse is 115/min and irregularly irregular, and blood pressure is 139/86 mmHg. Examination shows a fine tremor on both hands and digital swelling; the extremities are warm. There is retraction of the right upper eyelid. Which of the following is the most appropriate next step in the management of this patient?
- A. Amiodarone
- B. Propylthiouracil
- C. Warfarin
- D. Methimazole
- E. Propranolol (Correct Answer)
Hyperthyroidism and thyroiditis Explanation: ***Propranolol***
- This patient presents with symptoms suggestive of **hyperthyroidism** (tachycardia, palpitations, tremor, warm extremities, eyelid retraction, and nervousness). **Propranolol** is a non-selective beta-blocker that would help manage the sympathetic symptoms of hyperthyroidism, such as tachycardia and tremor.
- While other treatments target the thyroid hormone production, propranolol provides **rapid symptomatic relief** and is often used as initial therapy alongside antithyroid medications or radioiodine.
*Amiodarone*
- **Amiodarone** is an antiarrhythmic medication and a known cause of both hyperthyroidism and hypothyroidism due to its high iodine content and direct thyroid effects.
- It would not be appropriate for treating existing hyperthyroidism and could potentially worsen the condition if it's the underlying cause or if the hyperthyroidism is related to iodine excess.
*Propylthiouracil*
- **Propylthiouracil (PTU)** is an antithyroid medication that inhibits thyroid hormone synthesis and the peripheral conversion of T4 to T3.
- While PTU is a definitive treatment for hyperthyroidism, it has a slower onset of action compared to beta-blockers for symptomatic relief and carries a risk of severe **hepatotoxicity**, making methimazole often preferred unless in specific situations like pregnancy or thyroid storm.
*Warfarin*
- **Warfarin** is an anticoagulant used to prevent blood clots. While patients with atrial fibrillation (which can be caused by hyperthyroidism and presents as an irregularly irregular pulse) may require anticoagulation, it is not the most immediate step for managing the acute symptoms of hyperthyroidism.
- The patient's pulse is 115/min and irregularly irregular, suggesting possible atrial fibrillation, but addressing the hyperadrenergic state with a beta-blocker is the primary immediate intervention.
*Methimazole*
- **Methimazole** is an antithyroid medication that inhibits thyroid hormone synthesis. It is a common first-line treatment for hyperthyroidism.
- Similar to PTU, methimazole has a slower onset of action for symptomatic relief and does not immediately address the acute adrenergic symptoms as effectively as a beta-blocker.
Hyperthyroidism and thyroiditis US Medical PG Question 6: A 32-year-old Caucasian woman presents with a three-month history of weight loss, anxiety, and tremors. She recalls frequent heart palpitations and new discomfort while being outside in the heat. Her labs include a TSH level of 0.1 mIU/L. Additionally, the patient’s serum is positive for antibodies that stimulate the TSH receptor. What process is unique to this patient’s diagnosis?
- A. Stimulation of retroorbital fibroblasts (Correct Answer)
- B. Elevated levels of cholesterol and low density lipoprotein (LDL)
- C. Binding of thyroid hormones to cardiac myocytes
- D. Hyperplasia of thyroid follicular cells
- E. Lymphocyte-mediated destruction of the thyroid gland
Hyperthyroidism and thyroiditis Explanation: ***Stimulation of retroorbital fibroblasts***
- This patient's symptoms (weight loss, anxiety, tremors, heat intolerance, palpitations, low TSH, positive TSH receptor antibodies) are highly classic for **Graves' disease**.
- Unique to Graves' disease among thyroid disorders is the **TSH receptor antibody** stimulation of retroorbital fibroblasts and adipocytes, leading to the characteristic symptom of **Graves' ophthalmopathy** (exophthalmos), which is a key distinguishing feature.
*Elevated levels of cholesterol and low density lipoprotein (LDL)*
- **Elevated cholesterol** and **LDL** are typically associated with **hypothyroidism**, where the metabolic rate is slowed down, leading to decreased clearance of lipids.
- In **hyperthyroidism** (Graves' disease), the metabolic rate is increased, often leading to **decreased cholesterol** and LDL levels.
*Binding of thyroid hormones to cardiac myocytes*
- While **thyroid hormones** do bind to receptors on **cardiac myocytes** in hyperthyroid states, leading to increased heart rate and contractility, this process is not unique to Graves' disease.
- This **binding** and its effects on the heart are a general feature of **hyperthyroidism**, regardless of its underlying cause (e.g., toxic multinodular goiter, thyroiditis).
*Hyperplasia of thyroid follicular cells*
- **Hyperplasia of thyroid follicular cells** occurs in various conditions, including other forms of **hyperthyroidism** and even in some forms of **goiter** without hyperthyroidism.
- While it is present in Graves' disease due to constant stimulation by TSH receptor antibodies, it is not a **unique pathological process** specific only to Graves' disease.
*Lymphocyte-mediated destruction of the thyroid gland*
- **Lymphocyte-mediated destruction** of the thyroid gland is characteristic of **Hashimoto's thyroiditis**, which typically leads to **hypothyroidism**.
- In contrast, Graves' disease involves **autoantibody stimulation** of the thyroid leading to hyperthyroidism, not destruction of the gland.
Hyperthyroidism and thyroiditis US Medical PG Question 7: A 26-year-old African-American woman presents to the clinic for a routine check-up. Review of systems reveals that she often feels nervous and has recently developed a slight tremor. Of note, she has lost 15 pounds in the past 3 months, despite an increased appetite. The patient’s temperature is 99°F (37.2°C), blood pressure is 130/78 mmHg, pulse is 85/min, and respirations are 14/min with an oxygen saturation of 98% on room air. On physical exam, her skin is warm and she has mild exophthalmos. Which of the following is the direct mechanism causing the patient's ophthalmologic findings?
- A. Decreased levels of T4/T3
- B. Anti-myelin antibodies
- C. Lymphocytic infiltration (Correct Answer)
- D. Anti-thyroglobulin antibodies
- E. Anti-thyroid peroxidase antibodies
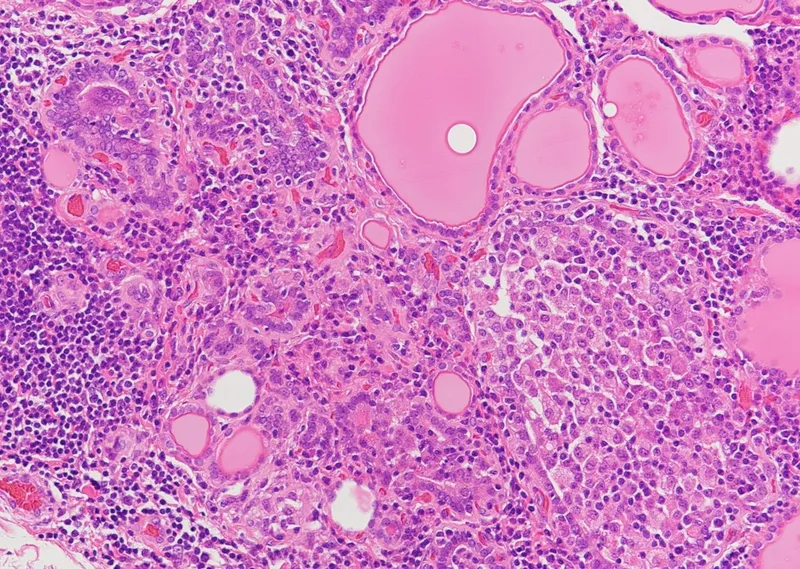
Hyperthyroidism and thyroiditis Explanation: ***Lymphocytic infiltration***
- **Exophthalmos** in Graves' disease is caused by an **autoimmune inflammatory process** involving the **extraocular muscles** and **orbital connective tissue**.
- This inflammation leads to **lymphocytic infiltration**, **fibrosis**, and the accumulation of **hyaluronic acid** and **glycosaminoglycans**, causing orbital tissue expansion and protrusion of the eyeballs.
*Decreased levels of T4/T3*
- **Decreased T4/T3 levels** are characteristic of **hypothyroidism**, not hyperthyroidism, as seen in this patient.
- Hypothyroidism does not directly cause exophthalmos; rather, it can lead to **periorbital edema** due to generalized fluid retention.
*Anti-myelin antibodies*
- **Anti-myelin antibodies** are associated with **demyelinating diseases** like **multiple sclerosis**, affecting the central nervous system.
- They are not involved in the pathogenesis of exophthalmos or thyroid-related ophthalmopathy.
*Anti-thyroglobulin antibodies*
- **Anti-thyroglobulin antibodies** are often seen in **Hashimoto's thyroiditis**, a cause of hypothyroidism, but can also be present in Graves' disease.
- While they are markers of thyroid autoimmunity, they do not directly cause the **ophthalmologic changes** of Graves' disease.
*Anti-thyroid peroxidase antibodies*
- **Anti-thyroid peroxidase antibodies (TPOAbs)** are also primarily associated with **Hashimoto's thyroiditis** and, less commonly, Graves' disease.
- Like anti-thyroglobulin antibodies, they indicate thyroid autoimmunity but are not the direct cause of the **orbital inflammation** and exophthalmos.
Hyperthyroidism and thyroiditis US Medical PG Question 8: A 25-year-old woman comes to the physician because of a 4-month history of anxiety and weight loss. She also reports an inability to tolerate heat and intermittent heart racing for 2 months. She appears anxious. Her pulse is 108/min and blood pressure is 145/87 mm Hg. Examination shows a fine tremor of her outstretched hands. After confirmation of the diagnosis, the patient is scheduled for radioactive iodine ablation. At a follow-up visit 2 months after the procedure, she reports improved symptoms but new-onset double vision. Examination shows conjunctival injections, proptosis, and a lid lag. Slit-lamp examination shows mild corneal ulcerations. The patient is given an additional medication that improves her diplopia and proptosis. Which of the following mechanisms is most likely responsible for the improvement in this patient's ocular symptoms?
- A. Replacement of thyroid hormones
- B. Decreased production of proinflammatory cytokines (Correct Answer)
- C. Decreased uptake of iodine
- D. Elimination of excess fluid
- E. Inhibition of iodide oxidation
Hyperthyroidism and thyroiditis Explanation: ***Decreased production of proinflammatory cytokines***
- The patient's initial symptoms are consistent with **hyperthyroidism due to Graves' disease**, which is an autoimmune condition. The new-onset double vision, conjunctival injection, proptosis, and lid lag suggest **Graves' ophthalmopathy**.
- **Graves' ophthalmopathy** is an autoimmune process characterized by **inflammation, fibrosis, and edema of the extraocular muscles and orbital soft tissues**. Medications like glucocorticoids, which reduce proinflammatory cytokines, are used to manage the inflammatory component of Graves' ophthalmopathy and improve symptoms like diplopia and proptosis.
*Replacement of thyroid hormones*
- While thyroid hormone replacement is necessary after radioactive iodine ablation to treat the induced hypothyroidism, it does not directly treat or improve the underlying inflammatory process of **Graves' ophthalmopathy**.
- Replacing thyroid hormones would address systemic symptoms of hypothyroidism but would not resolve the orbital inflammation and its ophthalmic manifestations.
*Decreased uptake of iodine*
- Radioactive iodine ablation works by destroying thyroid cells, thereby **decreasing the uptake of iodine** by the thyroid gland and reducing thyroid hormone production.
- While this addresses the hyperthyroidism, it does not directly manage the autoimmune inflammatory process of **Graves' ophthalmopathy**, which can even worsen after radioactive iodine ablation in some cases.
*Elimination of excess fluid*
- Although edema is a component of orbital involvement in Graves' ophthalmopathy, the primary treatment for improving diplopia and proptosis focuses on **reducing inflammation and fibrosis**, not merely eliminating excess fluid.
- Diuretics are not the primary treatment for the ocular symptoms of Graves' ophthalmopathy, which are driven by an autoimmune inflammatory response.
*Inhibition of iodide oxidation*
- Inhibition of iodide oxidation is the mechanism of **antithyroid drugs** like methimazole and propylthiouracil, which are used to treat hyperthyroidism by reducing thyroid hormone synthesis.
- This mechanism treats hyperthyroidism but does not address the autoimmune inflammation responsible for **Graves' ophthalmopathy** once it has developed, especially post-ablation.
Hyperthyroidism and thyroiditis US Medical PG Question 9: A 52-year-old male presents to clinic with complaints of anxiety and fatigue for 4 months. He has also been experiencing palpitations, muscle weakness, increased sweating, and an increase in the frequency of defecation. Past medical history is insignificant. He neither consumes alcohol nor smokes cigarettes. His pulse is 104/min and irregular, blood pressure is 140/80 mm Hg. On examination, you notice that he has bilateral exophthalmos. There are fine tremors in both hands. Which of the following results would you expect to see on a thyroid panel?
- A. High TSH; Low T4; Low T3
- B. High TSH; High T4; High T3
- C. Normal TSH; Low total T4; Normal Free T4 and T3
- D. Low TSH; High T4; High T3 (Correct Answer)
- E. Normal TSH; Low T4; Low T3
Hyperthyroidism and thyroiditis Explanation: ***Low TSH; High T4; High T3***
- The patient's symptoms (anxiety, fatigue, palpitations, muscle weakness, increased sweating, increased defecation frequency, tachycardia, hypertension, exophthalmos, fine tremors) are classic for **hyperthyroidism**, particularly **Graves' disease**.
- In primary hyperthyroidism, the thyroid gland overproduces T3 and T4, leading to **high levels of T4 and T3**. This then causes a negative feedback loop to the pituitary, resulting in **suppressed (low) TSH** levels.
*High TSH; Low T4; Low T3*
- This pattern is indicative of **primary hypothyroidism**, where the thyroid gland is underactive and cannot produce sufficient T4 and T3, leading to low levels of these hormones and a compensatory rise in TSH.
- The presented symptoms are directly opposite to those seen in hypothyroidism.
*High TSH; High T4; High T3*
- This combination is characteristic of **secondary hyperthyroidism**, which is much rarer and caused by a TSH-secreting pituitary adenoma.
- While it presents with hyperthyroid symptoms, the TSH level would be elevated or inappropriately normal, not suppressed.
*Normal TSH; Low total T4; Normal Free T4 and T3*
- This pattern is often seen in **euthyroid sick syndrome** or conditions causing a decrease in thyroid-binding globulin (TBG).
- The patient's clinical presentation is clearly that of hyperthyroidism, not a euthyroid state.
*Normal TSH; Low T4; Low T3*
- This result is atypical for any specific thyroid disorder and does not align with the patient's symptoms of hyperthyroidism, which demand high circulating thyroid hormone levels.
- A "normal TSH, low T4, low T3" might suggest central hypothyroidism if TSH was inappropriately normal for the low thyroid hormones, but this patient's symptoms definitively point to thyroid hormone excess.
Hyperthyroidism and thyroiditis US Medical PG Question 10: A 45-year-old woman comes to the physician because of a 4-month history of irritability and frequent bowel movements. During this time, she has had a 6.8-kg (15-lb) weight loss. She has not had a change in appetite or diet. She takes no medications. Her temperature is 37.4°C (99.4°F), pulse is 112/min, respirations are 16/min, and blood pressure is 126/74 mm Hg. Examination shows moist palms. The thyroid gland is diffusely enlarged; there are no palpable nodules. Serum studies show a thyroid-stimulating hormone (TSH) concentration of 0.2 μU/mL, thyroxine (T4) concentration of 22 μg/dL, and antibodies against the TSH receptor. Which of the following treatment modalities is associated with the lowest rate of recurrence for this patient's condition?
- A. Subtotal thyroidectomy
- B. Propranolol
- C. Potassium iodide
- D. Methimazole
- E. Radioactive iodine ablation (Correct Answer)
Hyperthyroidism and thyroiditis Explanation: ***Radioactive iodine ablation***
- **Radioactive iodine ablation** is the most definitive treatment for **Graves' disease**, leading to destruction of the overactive thyroid tissue and consequently the lowest recurrence rate.
- While it may result in **hypothyroidism**, this is generally manageable with lifelong **thyroid hormone replacement**.
*Subtotal thyroidectomy*
- **Subtotal thyroidectomy** involves surgical removal of part of the thyroid, which can also be effective but carries risks such as **anesthesia complications**, **hypoparathyroidism**, and **recurrent laryngeal nerve damage**.
- Recurrence rates with surgery can be higher than with radioactive iodine, as some thyroid tissue remains.
*Propranolol*
- **Propranolol** is a **beta-blocker** used to manage the **symptomatic effects** of hyperthyroidism, such as palpitations, tremor, and anxiety.
- It does not address the underlying overproduction of thyroid hormones and therefore has no impact on disease recurrence.
*Potassium iodide*
- **Potassium iodide** is typically used in the **short term** to block thyroid hormone release, particularly in preparation for thyroidectomy or during a **thyroid storm**.
- It is not a long-term treatment for **Graves' disease** and does not prevent recurrence.
*Methimazole*
- **Methimazole** is an **antithyroid medication** that reduces thyroid hormone synthesis by inhibiting **thyroid peroxidase**.
- While effective for controlling hyperthyroidism, relapse rates after discontinuing antithyroid medications are significant (up to 50-60%), making it less effective in preventing recurrence compared to definitive treatments.
More Hyperthyroidism and thyroiditis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.