Diabetes complications and screening US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diabetes complications and screening. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diabetes complications and screening US Medical PG Question 1: A 52-year-old man presents to his primary care physician to discuss laboratory results that were obtained during his annual checkup. He has no symptoms or concerns and denies changes in eating or urination patterns. Specifically, the physician ordered a panel of metabolic laboratory tests to look for signs of diabetes, hyperlipidemia, or other chronic disorders. A spot glucose check from a random blood sample showed a glucose level of 211 mg/dL. A hemoglobin A1c level was obtained at the same time that showed a level of 6.3%. A fasting blood glucose was obtained that showed a blood glucose level of 125 mg/dL. Finally, a 2-hour glucose level was obtained after an oral glucose tolerance test that showed a glucose level of 201 mg/dL. Which of the following statements is most accurate for this patient?
- A. This patient does not have type 2 diabetes
- B. This patient has type 2 diabetes as diagnosed by his fasting blood glucose
- C. This patient has type 2 diabetes as diagnosed by his oral tolerance blood glucose (Correct Answer)
- D. This patient has type 2 diabetes as diagnosed by his random blood glucose
- E. This patient has type 2 diabetes as diagnosed by his hemoglobin A1c
Diabetes complications and screening Explanation: **This patient has type 2 diabetes as diagnosed by his oral tolerance blood glucose**
- A 2-hour plasma glucose of **200 mg/dL or higher** during an Oral Glucose Tolerance Test (OGTT) is a diagnostic criterion for diabetes. This patient's 2-hour glucose level of **201 mg/dL** meets this criterion.
- The combination of this elevated OGTT result with a random glucose over 200 mg/dL further supports the diagnosis, even in an asymptomatic individual.
*This patient does not have type 2 diabetes*
- The patient has multiple laboratory values that meet or exceed diagnostic thresholds for diabetes, including a random glucose of **211 mg/dL**, an HbA1c of **6.3%**, and a 2-hour OGTT glucose of **201 mg/dL**.
- While one individual threshold might not be conclusive, the overall pattern of results clearly indicates diabetes.
*This patient has type 2 diabetes as diagnosed by his fasting blood glucose*
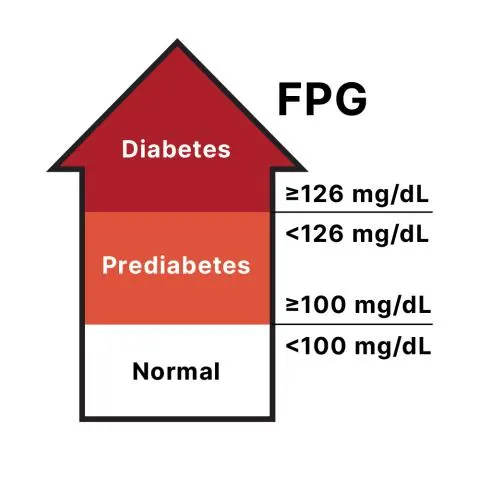
- A fasting plasma glucose (FPG) of **126 mg/dL or higher** is diagnostic for diabetes. This patient's FPG of **125 mg/dL** is just below this threshold.
- While concerning, an FPG of 125 mg/dL alone is considered **impaired fasting glucose** (pre-diabetes), not diabetes.
*This patient has type 2 diabetes as diagnosed by his random blood glucose*
- A random plasma glucose of **200 mg/dL or higher** in a symptomatic patient is diagnostic for diabetes. However, this patient is **asymptomatic**.
- In an asymptomatic patient, an elevated random glucose requires confirmation by another diagnostic test (e.g., FPG, OGTT, or HbA1c) on a subsequent day, or concurrent with another positive test (like the OGTT in this case).
*This patient has type 2 diabetes as diagnosed by his hemoglobin A1c*
- An HbA1c level of **6.5% or higher** is diagnostic for diabetes. This patient's HbA1c of **6.3%** is below this cutoff.
- An HbA1c between 5.7% and 6.4% indicates **pre-diabetes**, specifically increased risk for diabetes.
Diabetes complications and screening US Medical PG Question 2: A 62-year-old man comes to the physician in May for a routine health maintenance examination. He feels well. He underwent a right inguinal hernia repair 6 months ago. He has hypertension and type 2 diabetes mellitus. There is no family history of serious illness. Current medications include metformin, sitagliptin, enalapril, and metoprolol. He received the zoster vaccine 1 year ago. He received the PPSV23 vaccine 4 years ago. His last colonoscopy was 7 years ago and was normal. He smoked a pack of cigarettes a day for 20 years but quit 17 years ago. He drinks two to three alcoholic beverages on weekends. He is allergic to amoxicillin. He is scheduled to visit Australia and New Zealand in 2 weeks to celebrate his 25th wedding anniversary. He appears healthy. Vital signs are within normal limits. An S4 is heard at the apex. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate recommendation at this time?
- A. Colonoscopy
- B. Influenza vaccine (Correct Answer)
- C. Pneumococcal conjugate vaccine 13
- D. Cardiac stress test
- E. Abdominal ultrasound
Diabetes complications and screening Explanation: ***Influenza vaccine***
- Current guidelines recommend annual **influenza vaccination** for all adults, particularly those over 60 years old and those with chronic medical conditions like diabetes and hypertension.
- **Critical timing consideration**: The patient is traveling to Australia and New Zealand (Southern Hemisphere) in 2 weeks, where it will be **winter season** (May-September) with peak influenza activity.
- He is a **high-risk patient** (age >60, diabetes, hypertension, cardiovascular disease) who should receive influenza vaccine before travel to areas experiencing influenza season.
- This is the **most appropriate and time-sensitive recommendation** at this visit.
*Colonoscopy*
- The patient had a normal colonoscopy 7 years ago; current guidelines suggest a repeat colonoscopy every **10 years** for average-risk individuals.
- There are no new symptoms, family history, or risk factors that would necessitate an earlier repeat colonoscopy at this time.
*Pneumococcal conjugate vaccine 13*
- The patient received **PPSV23** four years ago at approximately age 58.
- Per **current CDC guidelines (2019+)**, PCV13 is **no longer routinely recommended** for immunocompetent adults ≥65 years old.
- PPSV23 alone is now the standard recommendation for adults ≥65, which this patient has already received.
- PCV13 may be considered through **shared decision-making** in specific circumstances, but is not a routine or urgent recommendation.
*Cardiac stress test*
- Although the patient has risk factors for cardiovascular disease (hypertension, diabetes, former smoker) and an **S4 heart sound** (indicating **left ventricular hypertrophy**), he is asymptomatic.
- Routine **screening stress tests** are not recommended for asymptomatic individuals without signs of active cardiac ischemia.
*Abdominal ultrasound*
- There are **no symptoms** or specific indications (e.g., abdominal aortic aneurysm screening criteria not met - would need age 65-75 with smoking history).
- The patient is 62 years old and quit smoking 17 years ago, so AAA screening criteria are not yet met.
- Routine screening abdominal ultrasounds are not indicated.
Diabetes complications and screening US Medical PG Question 3: A 53-year-old Asian woman comes to the physician because of a 2-month history of severe pain in her right leg while walking. She used to be able to walk a half-mile (800-m) to the grocery store but has been unable to walk 200 meters without stopping because of the pain over the past month. She can continue to walk after a break of around 5 minutes. She has hypertension, atrial fibrillation, and type 2 diabetes mellitus. She has smoked one pack of cigarettes daily for the past 32 years. Current medications include metformin, enalapril, aspirin, and warfarin. Vital signs are within normal limits. Examination shows an irregularly irregular pulse. The right lower extremity is cooler than the left lower extremity. The skin over the right leg appears shiny and dry. Femoral pulses are palpated bilaterally; pedal pulses are diminished on the right side. Which of the following is the most appropriate next step in management?
- A. MRI spine screening
- B. Duplex ultrasonography
- C. Ankle-brachial index (Correct Answer)
- D. Nerve conduction studies
- E. Biopsy of tibial artery
Diabetes complications and screening Explanation: ***Ankle-brachial index***
- The patient's symptoms of **intermittent claudication** (leg pain with exertion relieved by rest) and risk factors (smoking, diabetes, atrial fibrillation, hypertension) are highly suggestive of **peripheral artery disease (PAD)**. The **ankle-brachial index (ABI)** is the most appropriate initial diagnostic step as it is a quick, non-invasive, and reliable test to screen for PAD by comparing blood pressure in the ankles to blood pressure in the arms.
- A **diminished pedal pulse** on the right side and **cooler, shiny, dry skin** further support the suspicion of PAD, making ABI crucial for confirming the diagnosis and assessing its severity.
*MRI spine screening*
- While spinal pathology can cause leg pain, symptoms like **neurogenic claudication** typically improve with leaning forward or sitting and are not consistently relieved by standing still. The patient's pain relief with rest after walking points away from spinal stenosis.
- The patient's specific peripheral signs like a **cooler leg**, **diminished pedal pulses**, and **trophic changes** are not typical findings for spinal compression.
*Duplex ultrasonography*
- **Duplex ultrasonography** is a more advanced imaging technique used to visualize the blood vessels and assess blood flow, typically performed *after* an abnormal ABI confirms the presence of PAD.
- It helps in **localizing stenoses** and assessing their severity, but it is not the primary diagnostic screening tool in the initial evaluation of suspected PAD.
*Nerve conduction studies*
- **Nerve conduction studies (NCS)** are used to diagnose neuropathies. While diabetes is a risk factor for neuropathy, the patient's symptoms are classic for **vascular claudication** (pain with exertion, relieved by rest), rather than neuropathic pain, which is often described as burning, tingling, or numbing and does not typically resolve promptly with rest.
- The physical exam findings of a **cool leg** and **diminished pulses** are not consistent with a primary neurological problem.
*Biopsy of tibial artery*
- A **biopsy of the tibial artery** is an invasive procedure generally reserved for specific types of vasculitis (e.g., giant cell arteritis, polyarteritis nodosa) when other less invasive diagnostics have been inconclusive or raised suspicion for these conditions.
- It is not indicated for the initial workup of suspected **atherosclerotic peripheral artery disease**, which is the most likely diagnosis given the patient's risk factors and symptoms.
Diabetes complications and screening US Medical PG Question 4: A 41-year-old man presents to his primary care provider because of chest pain with activity for the past 6 months. Past medical history is significant for appendectomy at age 12 and hypertension, and diabetes mellitus type 2 that is poorly controlled. He takes metformin and lisinopril but admits that he is bad at remembering to take them everyday. His father had a heart attack at 41 and 2 stents were placed in his heart. His mother is healthy. He drinks alcohol occasionally and smokes a half of a pack of cigarettes a day. He is a sales executive and describes his work as stressful. Today, the blood pressure is 142/85 and the body mass index (BMI) is 28.5 kg/m2. A coronary angiogram shows > 75% narrowing of the left anterior descending coronary artery. Which of the following is most significant in this patient?
- A. Obesity
- B. Family history
- C. Hypertension
- D. Smoking
- E. Diabetes mellitus (Correct Answer)
Diabetes complications and screening Explanation: ***Diabetes mellitus***
- **Diabetes mellitus** is a significant risk factor for **atherosclerosis** and contributes to accelerated progression of **coronary artery disease (CAD)**, often leading to more widespread and severe disease.
- Poorly controlled diabetes can cause **endothelial dysfunction**, increasing oxidative stress and inflammation, which are key processes in **plaque formation** and destabilization.
*Obesity*
- **Obesity** (BMI 28.5 kg/m2) is a risk factor for **CAD** but often acts through associated conditions like **hypertension**, **diabetes**, and **dyslipidemia**.
- While it contributes to overall cardiovascular risk, it is less directly pathogenic than diabetes which independently accelerates **atherosclerosis**.
*Family history*
- The patient's father had a **heart attack at 41**, which is a significant risk factor for **early-onset CAD**.
- However, the patient has multiple modifiable risk factors (smoking, hypertension, diabetes) that are independently and more directly contributing to his current presentation.
*Hypertension*
- **Hypertension** (142/85 mmHg) is a major modifiable risk factor that causes **endothelial damage** and promotes **atherosclerosis**.
- While important, the patient's **poorly controlled diabetes mellitus** often creates a more aggressive environment for plaque formation and progression compared to hypertension alone.
*Smoking*
- **Smoking** is a potent, modifiable risk factor that causes direct vascular injury, promotes **thrombogenesis**, and contributes to **atherosclerosis**.
- Although highly detrimental, smoking is one of several significant risk factors; **diabetes mellitus**, with its systemic metabolic impact, can be considered more broadly influential in the severity and diffuse nature of **CAD**.
Diabetes complications and screening US Medical PG Question 5: A 27-year-old Hispanic G2P1 presents for a routine antepartum visit at 26 weeks gestation. She has no complaints. The vital signs are normal, the physical examination is within normal limits, and the gynecologic examination corresponds to 25 weeks gestation. The oral glucose tolerance test (OGTT) with a 75-g glucose load is significant for a glucose level of 177 mg/dL at 1 hour and 167 mg/dL at 2 hour. The fasting blood glucose level is 138 mg/dL (7.7 mmol/L), and the HbA1c is 7%. Which of the following represents the proper initial management?
- A. Sitagliptin
- B. Dietary and lifestyle modification
- C. Metformin
- D. Glyburide
- E. Insulin (Correct Answer)
Diabetes complications and screening Explanation: **Insulin**
- The patient's **fasting glucose of 138 mg/dL** and **HbA1c of 7%** indicate pre-existing **Type 2 Diabetes Mellitus**, not just gestational diabetes. Both values exceed the diagnostic thresholds for overt diabetes in pregnancy.
- **Insulin** is the preferred initial pharmacologic treatment for **overt diabetes in pregnancy** because it does not cross the placenta, ensuring fetal safety, and is highly effective in controlling maternal glucose levels.
*Sitagliptin*
- **Sitagliptin** is a **DPP-4 inhibitor** and is not recommended during pregnancy due to limited safety data and the availability of safer alternatives.
- Oral hypoglycemic agents are generally avoided as first-line therapy for established diabetes in pregnancy due to potential for placental transfer and adverse fetal effects.
*Dietary and lifestyle modification*
- While crucial, **dietary and lifestyle modification** alone are insufficient for managing overt diabetes with such high fasting glucose and HbA1c levels.
- These measures are usually the first step for **gestational diabetes**, but a patient with overt diabetes requires immediate pharmacologic intervention to prevent complications.
*Metformin*
- **Metformin** can be used in pregnancy but is primarily considered for **gestational diabetes** or as an alternative to insulin if the patient has milder hyperglycemia, or if insulin is poorly tolerated.
- Given the patient's significantly elevated fasting glucose and HbA1c, **insulin** is a more effective and immediate treatment to achieve glycemic control and reduce risks.
*Glyburide*
- **Glyburide** is an **oral sulfonylurea** that can cross the placenta, leading to potential fetal hyperinsulinemia and neonatal hypoglycemia.
- Its use in pregnancy is generally discouraged due to these risks, making **insulin** a safer and more appropriate choice.
Diabetes complications and screening US Medical PG Question 6: A 29-year-old woman presents to the primary care office for a recent history of falls. She has fallen 5 times over the last year. These falls are not associated with any preceding symptoms; she specifically denies dizziness, lightheadedness, or visual changes. However, she has started noticing that both of her legs feel weak. She's also noticed that her carpet feels strange beneath her bare feet. Her mother and grandmother have a history of similar problems. On physical exam, she has notable leg and foot muscular atrophy and 4/5 strength throughout her bilateral lower extremities. Sensation to light touch and pinprick is decreased up to the mid-calf. Ankle jerk reflex is absent bilaterally. Which of the following is the next best diagnostic test for this patient?
- A. MRI brain
- B. Ankle-brachial index
- C. Electromyography (including nerve conduction studies) (Correct Answer)
- D. Lumbar puncture
- E. Hemoglobin A1c
Diabetes complications and screening Explanation: ***Electromyography (including nerve conduction studies)***
- The patient's symptoms of **progressive weakness**, **sensory deficits** (carpet feels strange, decreased sensation up to mid-calf), **muscular atrophy**, and **absent ankle reflexes**, along with a **family history**, are highly suggestive of a **hereditary peripheral neuropathy** (e.g., Charcot-Marie-Tooth disease).
- **Electromyography (EMG)** and **nerve conduction studies (NCS)** are essential for confirming peripheral neuropathy, differentiating between demyelinating and axonal involvement, and localizing the lesion.
*MRI brain*
- An MRI brain would be indicated for central nervous system pathology, but the patient's symptoms (distal weakness, sensory loss with a "stocking-glove" distribution, absent reflexes) are highly suggestive of a **peripheral neuropathy**.
- There is no indication of upper motor neuron signs or other CNS involvement to warrant a brain MRI at this stage.
*Ankle-brachial index*
- Ankle-brachial index (ABI) is used to diagnose **peripheral artery disease (PAD)**, which typically presents with claudication (pain with exertion) and ischemic changes.
- The patient's symptoms of sensory changes and progressive weakness are not characteristic of PAD.
*Lumbar puncture*
- A lumbar puncture is primarily used to analyze **cerebrospinal fluid (CSF)** for inflammatory, infectious, or neoplastic conditions affecting the CNS or nerve roots (e.g., Guillain-Barré syndrome, which has acute onset).
- Given the chronic and progressive nature of her symptoms and a positive family history, it is less likely to be an acute inflammatory process of the nerve roots.
*Hemoglobin A1c*
- Hemoglobin A1c is used to screen for or monitor **diabetes mellitus**, which can cause a **diabetic neuropathy**.
- While diabetes can cause peripheral neuropathy, the patient's young age, lack of typical diabetic risk factors, and strong family history point more strongly towards a hereditary condition. Glycemic control does not fully explain her presentation.
Diabetes complications and screening US Medical PG Question 7: A 53-year-old woman with type 2 diabetes mellitus is admitted for evaluation of recurrent episodes of nausea, tremors, and excessive sweating. She works as a nurse and reports self-measured blood glucose levels below 50 mg/dL on several occasions. Her family history is positive for borderline personality disorder. The only medication listed in her history is metformin. Which of the following is the most appropriate next step in management?
- A. Measure serum C-peptide concentration
- B. Ask the patient if she is taking any medications other than metformin (Correct Answer)
- C. Search the patient's belongings for insulin
- D. Measure glycated hemoglobin concentration
- E. Report the patient to her employer
Diabetes complications and screening Explanation: ***Ask the patient if she is taking any medications other than metformin***
- The patient's presentation with recurrent **hypoglycemic symptoms** (nausea, tremors, sweating) and documented low blood glucose, while only being prescribed metformin (which does not cause hypoglycemia), strongly suggests **exogenous insulin or sulfonylurea use**.
- A direct question about other medications is a crucial initial step to ascertain the cause of her hypoglycemia and to rule out **factitious hypoglycemia**, especially given her profession as a nurse and a family history that might suggest psychological vulnerabilities, although not a direct diagnosis for the patient.
*Measure serum C-peptide concentration*
- While **low C-peptide** in the presence of hypoglycemia would suggest exogenous insulin administration, and high C-peptide might point to an insulinoma, this test should be done *after* ruling out common causes like the undisclosed use of other medications.
- This is a more invasive and less direct initial step compared to simply asking the patient about medication use, especially when a readily reversible cause (undisclosed medication) is possible.
*Search the patient's belongings for insulin*
- Searching a patient's belongings without their consent is a serious ethical breach and a violation of privacy.
- This action should only be considered as a last resort in extreme circumstances and with appropriate legal and ethical oversight, not as an initial diagnostic step.
*Measure glycated hemoglobin concentration*
- **Glycated hemoglobin (HbA1c)** reflects average blood glucose levels over the past 2-3 months and is used to monitor long-term glycemic control in diabetic patients.
- While useful for diabetes management, it will not directly identify the acute cause of recurrent hypoglycemic episodes or distinguish between endogenous and exogenous insulin sources.
*Report the patient to her employer*
- Reporting the patient to her employer prematurely, without a definitive diagnosis or understanding the full context of her condition, is unethical and unprofessional.
- The immediate priority is to diagnose and manage the patient's medical condition, ensuring her safety and well-being, before considering professional implications.
Diabetes complications and screening US Medical PG Question 8: A 59-year-old man presents to his primary care physician complaining of leg pain with exertion for the last 6 months. He has cramping in his calves when walking. He states that the cramping is worse on the right than the left and that the cramping resolves when he stops walking. He has had type 2 diabetes mellitus for 15 years and is not compliant with his medications. He has smoked 20–30 cigarettes daily for the past 30 years. On examination, the femoral pulses are diminished on both sides. Which of the following is the most likely cause of this patient’s condition?
- A. Segmental arterial occlusions due to non-atherosclerotic vasculitis
- B. Narrowing of the spinal canal
- C. Joint degeneration
- D. Venous thrombosis
- E. Atherosclerosis (Correct Answer)
Diabetes complications and screening Explanation: ***Atherosclerosis***
- The patient's presentation of **intermittent claudication** (leg pain with exertion, resolving with rest), history of **type 2 diabetes mellitus**, and **heavy smoking** are classic risk factors for atherosclerosis leading to peripheral artery disease (PAD).
- **Diminished femoral pulses** further support the diagnosis of arterial insufficiency caused by atherosclerotic plaque buildup.
*Segmental arterial occlusions due to non-atherosclerotic vasculitis*
- While vasculitis can cause arterial occlusions, conditions like **Takayasu arteritis** or **Buerger's disease** are less common in this age group and typically have different risk factors and clinical presentations compared to the patient's strong atherosclerotic risk profile.
- The patient's long-standing diabetes and smoking history strongly favor atherosclerosis over non-atherosclerotic vasculitis as the primary pathology.
*Narrowing of the spinal canal*
- This describes **neurogenic claudication**, which typically presents with leg pain that is often **position-dependent** (e.g., exacerbated by standing or extension of the spine) and may be relieved by leaning forward, rather than strictly by rest from walking.
- Neurogenic claudication usually involves **neurological symptoms** like numbness or weakness and does not typically present with diminished peripheral pulses.
*Joint degeneration*
- **Osteoarthritis** or joint degeneration would typically cause pain localized to the affected joint, which would worsen with joint movement and improve with rest from that movement, but it would not explain the **cramping nature** of the pain in the calves or the **diminished pulses**.
- Joint degeneration does not explain the systemic risk factors like diabetes and smoking contributing to vascular compromise.
*Venous thrombosis*
- A **venous thrombosis** (deep vein thrombosis) would typically cause acute onset leg pain, swelling, warmth, and erythema, often constant rather than exertional and resolving with rest.
- It would not lead to **diminished arterial pulses**; in fact, arterial pulses would typically be preserved.
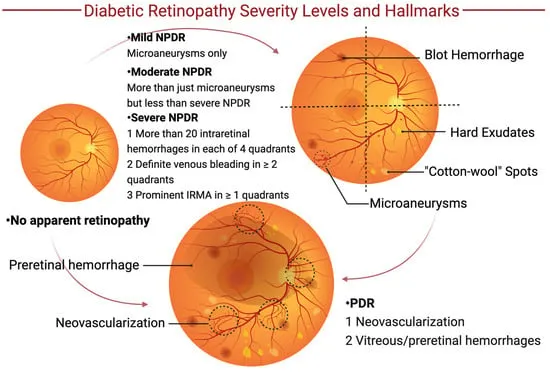
Diabetes complications and screening US Medical PG Question 9: A 76-year-old female with a past medical history of obesity, coronary artery disease status post stent placement, hypertension, hyperlipidemia, and insulin dependent diabetes comes to your outpatient clinic for regular checkup. She has not been very adherent to her diabetes treatment regimen. She has not been checking her sugars regularly and frequently forgets to administer her mealtime insulin. Her Hemoglobin A1c three months ago was 14.1%. As a result of her diabetes, she has developed worsening diabetic retinopathy and neuropathy. Based on her clinical presentation, which of the following is the patient most at risk for developing?
- A. Stress incontinence
- B. Hemorrhoids
- C. Rectal prolapse
- D. Overflow incontinence (Correct Answer)
- E. Uterine prolapse
Diabetes complications and screening Explanation: ***Overflow incontinence***
- The patient's **poorly controlled diabetes** can lead to **diabetic autonomic neuropathy**, affecting bladder function and causing **neurogenic bladder**.
- This results in the bladder not emptying completely, leading to **urinary retention** and leakage as the bladder overfills, which defines **overflow incontinence**.
*Stress incontinence*
- This type of incontinence is typically caused by **weakening of pelvic floor muscles** and **urethral sphincter**, leading to leakage with increased abdominal pressure (e.g., coughing, sneezing).
- While obesity is a risk factor, the patient's severe, uncontrolled diabetes points more strongly to neuropathy affecting bladder emptying rather than just sphincter weakness.
*Hemorrhoids*
- Hemorrhoids are **swollen veins in the rectum or anus**, often associated with straining during bowel movements, chronic constipation, or obesity.
- While common in this demographic, there is no direct link between uncontrolled diabetes and the development of hemorrhoids.
*Rectal prolapse*
- Rectal prolapse involves the **protrusion of the rectum through the anus**, often due to weakened pelvic floor muscles or chronic straining.
- Although the patient's age and obesity could be contributing factors, poorly controlled diabetes does not directly cause rectal prolapse.
*Uterine prolapse*
- Uterine prolapse occurs when the **uterus descends into the vagina**, typically due to weakened pelvic floor muscles, often following childbirth or with age and obesity.
- Uncontrolled diabetes does not directly cause uterine prolapse, although shared risk factors like obesity might be present.
Diabetes complications and screening US Medical PG Question 10: An 18-year-old Caucasian female presents to your clinic because of a recent increase in thirst and hunger. Urinalysis demonstrates elevated glucose. The patient's BMI is 20. Which of the following is the most common cause of death in persons suffering from this patient's illness?
- A. Coma
- B. Peripheral neuropathy
- C. Infection
- D. Renal failure
- E. Myocardial infarction (Correct Answer)
Diabetes complications and screening Explanation: ***Myocardial infarction***
- **Cardiovascular disease, particularly myocardial infarction, is the leading cause of death in Type 1 Diabetes Mellitus**, accounting for approximately 40% of mortality.
- Patients with Type 1 diabetes develop **accelerated atherosclerosis** due to chronic hyperglycemia, dyslipidemia, endothelial dysfunction, and increased oxidative stress.
- Even young patients with T1DM have significantly elevated cardiovascular risk compared to age-matched controls, with risk increasing proportionally with disease duration and glycemic control.
- While acute complications like DKA are immediately life-threatening, modern medical management has reduced DKA mortality to <1%, making chronic cardiovascular complications the predominant cause of death.
*Coma*
- **Diabetic ketoacidosis (DKA)** leading to coma is indeed a serious acute complication of Type 1 diabetes.
- However, with contemporary medical care and improved access to insulin, DKA mortality is less than 1% in developed countries.
- While DKA may be the presenting feature or an immediate threat, it is not the most common cause of death over the lifetime of T1DM patients.
*Peripheral neuropathy*
- Diabetic peripheral neuropathy is a common chronic complication affecting up to 50% of long-standing diabetics.
- While it significantly impacts quality of life and can lead to foot ulcers, infections, and amputations, it is not a direct cause of death.
- Autonomic neuropathy can contribute to sudden cardiac death, but this is still categorized under cardiovascular mortality.
*Infection*
- Diabetes does increase susceptibility to certain infections due to impaired neutrophil function, reduced chemotaxis, and hyperglycemia promoting bacterial growth.
- While infections can be serious (e.g., necrotizing fasciitis, mucormycosis), they are not the leading cause of mortality in T1DM.
- Infection-related deaths are far less common than cardiovascular deaths.
*Renal failure*
- **Diabetic nephropathy** is the second most common cause of death in Type 1 diabetes, affecting approximately 20-30% of patients.
- End-stage renal disease develops over many years and contributes significantly to mortality.
- However, cardiovascular disease remains more common, and many patients with diabetic nephropathy ultimately die from cardiovascular events rather than renal failure alone.
More Diabetes complications and screening US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.