Adrenal disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adrenal disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adrenal disorders US Medical PG Question 1: A 32-year-old woman comes to the physician because of a 2-month history of fatigue, muscle weakness, paresthesias, headache, and palpitations. Her pulse is 75/min and blood pressure is 152/94 mm Hg. Physical examination shows no abnormalities. Serum studies show:
Sodium 144 mEq/L
Potassium 2.9 mEq/L
Bicarbonate 31 mEq/L
Creatinine 0.7 mg/dL
Further evaluation shows low serum renin activity. Which of the following is the most likely diagnosis?
- A. Aldosteronoma (Correct Answer)
- B. Cushing syndrome
- C. Renal artery stenosis
- D. Pheochromocytoma
- E. Laxative abuse
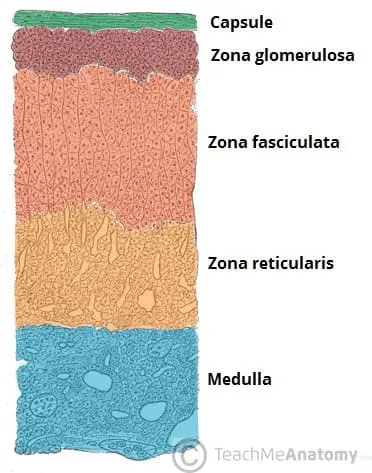
Adrenal disorders Explanation: ***Aldosteronoma***
- The patient presents with **hypertension**, **hypokalemia**, and **metabolic alkalosis** (elevated bicarbonate), which are classic signs of primary hyperaldosteronism.
- **Low serum renin activity** in conjunction with these findings points directly to an **aldosterone-producing adenoma (aldosteronoma)** as the most likely cause.
*Cushing syndrome*
- While Cushing syndrome can cause **hypertension** and **hypokalemia**, it is primarily characterized by features of **hypercortisolism** such as central obesity, moon facies, striae, and muscle wasting, which are not described here.
- The primary defect in Cushing syndrome relates to cortisol excess, not primary aldosterone overproduction leading to low renin.
*Renal artery stenosis*
- **Renal artery stenosis** causes **secondary hyperaldosteronism**, typically presenting with **hypertension** and **elevated renin activity** due to decreased renal perfusion.
- This contradicts the patient's low serum renin activity, making it an unlikely diagnosis.
*Pheochromocytoma*
- **Pheochromocytoma** presents with paroxysmal or sustained **hypertension**, **palpitations**, **headaches**, and **sweating** due to catecholamine excess.
- It does not typically cause **hypokalemia** or **metabolic alkalosis** as seen in this patient.
*Laxative abuse*
- **Laxative abuse** can cause hypokalemia and metabolic alkalosis, but it is typically associated with **chronic diarrhea** and volume depletion, which are not mentioned.
- It does not directly cause **hypertension** and is not associated with low renin activity in the context of aldosterone excess.
Adrenal disorders US Medical PG Question 2: A 45-year-old woman comes to the physician because of fatigue, irregular menses, and recurrent respiratory infections for the past 6 months. Her blood pressure is 151/82 mm Hg. Physical examination shows a round face, thinning of the skin, and multiple bruises on her arms. Further studies confirm the diagnosis of an ACTH-secreting pituitary adenoma. This patient is at greatest risk for which of the following?
- A. Weight loss
- B. Eosinophilia
- C. Bitemporal hemianopsia
- D. Hypoglycemia
- E. Pathologic fracture (Correct Answer)
Adrenal disorders Explanation: ***Pathologic fracture***
- This patient has **Cushing's disease** due to an **ACTH-secreting pituitary adenoma**, leading to excess cortisol.
- **Excess cortisol** causes **osteoporosis** by increasing bone resorption and decreasing bone formation, significantly raising the risk of **pathologic fractures**.
- This is the **greatest risk** because **all patients** with chronic hypercortisolism develop bone loss, making fractures highly likely.
*Weight loss*
- Patients with Cushing's disease typically experience **weight gain**, particularly centrally (truncal obesity), due to **cortisol-induced fat redistribution**.
- **Fatigue** is common, but weight loss is not a characteristic feature of Cushing's syndrome.
*Eosinophilia*
- **Hypercortisolism** (Cushing's syndrome) usually causes **eosinopenia** (decreased eosinophil count) and **lymphopenia**, not eosinophilia.
- Cortisol has an anti-inflammatory and immunosuppressive effect, leading to a reduction in circulating eosinophils and lymphocytes.
*Bitemporal hemianopsia*
- While an **ACTH-secreting pituitary adenoma** is present, **bitemporal hemianopsia** occurs only when a pituitary tumor becomes a **macroadenoma** (>10mm) and compresses the **optic chiasm**.
- Most ACTH-secreting adenomas are **microadenomas** (<10mm) that cause symptoms through **hormonal excess**, not mass effect.
- The clinical picture here reflects **Cushing's syndrome** from hypercortisolism, which affects **all patients** regardless of tumor size, whereas visual field defects occur only with large tumors.
*Hypoglycemia*
- **Excess cortisol** **increases gluconeogenesis** and **insulin resistance**, leading to **hyperglycemia**, not hypoglycemia.
- This is a common metabolic complication of Cushing's syndrome, often progressing to **steroid-induced diabetes mellitus**.
Adrenal disorders US Medical PG Question 3: A 69-year-old woman is brought to the emergency department because of fatigue and lethargy for 5 days. She has also had weakness and nausea for the last 3 days. She has sarcoidosis, major depressive disorder, and hypertension. She had a stroke 5 years ago. Current medications include aspirin, nifedipine, prednisolone, fluoxetine, and rosuvastatin, but she has not taken any of her medications for 7 days due to international travel. Her temperature is 36.1°C (96.9°F), pulse is 95/min, and blood pressure is 85/65 mm Hg. She is lethargic but oriented. Examination shows no other abnormalities. Her hemoglobin concentration is 13.4 g/dL and leukocyte count is 9,600/mm3. Both serum cortisol and ACTH levels are decreased. This patient is most likely to have which of the following additional laboratory abnormalities?
- A. Hyperglycemia
- B. Hyperkalemia
- C. Hyponatremia (Correct Answer)
- D. Hypokalemia
- E. Normal anion gap metabolic acidosis
Adrenal disorders Explanation: ***Hyponatremia***
- This patient has **secondary adrenal insufficiency** due to **HPA axis suppression** from chronic prednisolone use, precipitated by abrupt withdrawal after 7 days without medication.
- **Both decreased cortisol and ACTH** confirm secondary (central) adrenal insufficiency, distinguishing it from primary adrenal insufficiency where ACTH would be elevated.
- **Hyponatremia** develops due to **cortisol deficiency** impairing free water excretion, leading to dilutional hyponatremia—a hallmark laboratory finding in adrenal insufficiency.
- Clinical features include **fatigue, lethargy, hypotension, nausea, and weakness**, consistent with adrenal crisis.
*Hyperglycemia*
- While **glucocorticoids** cause hyperglycemia, **cortisol deficiency** in adrenal insufficiency leads to **impaired gluconeogenesis** and a tendency toward **hypoglycemia**, not hyperglycemia.
- The patient's presentation with hypotension and weakness is consistent with adrenal crisis, not hyperglycemia.
*Hyperkalemia*
- **Hyperkalemia** is characteristic of **primary adrenal insufficiency** (Addison's disease) due to **aldosterone deficiency** affecting the renin-angiotensin-aldosterone system.
- In **secondary adrenal insufficiency**, the hypothalamic-pituitary axis is suppressed but the **renin-angiotensin-aldosterone system remains intact**, so aldosterone secretion is preserved and significant hyperkalemia does not occur.
*Hypokalemia*
- **Hypokalemia** is not a typical feature of adrenal insufficiency and is more commonly associated with diuretic use, primary hyperaldosteronism, or other conditions not present in this case.
- The patient's condition reflects cortisol deficiency with preserved aldosterone function.
*Normal anion gap metabolic acidosis*
- **Normal anion gap metabolic acidosis** occurs in conditions like **renal tubular acidosis** or **diarrhea**, but is not a direct or common consequence of secondary adrenal insufficiency.
- The acute presentation with hypotension and electrolyte disturbance (hyponatremia) is the primary metabolic derangement in this case.
Adrenal disorders US Medical PG Question 4: A 63-year-old woman presents to your outpatient clinic complaining of headaches, blurred vision, and fatigue. She has a blood pressure of 171/91 mm Hg and heart rate of 84/min. Physical examination is unremarkable. Her lab results include K+ of 3.1mEq/L and a serum pH of 7.51. Of the following, which is the most likely diagnosis for this patient?
- A. Pheochromocytoma
- B. Renal artery stenosis
- C. Cushing’s syndrome
- D. Primary hyperaldosteronism (Conn’s syndrome) (Correct Answer)
- E. Addison’s disease
Adrenal disorders Explanation: ***Primary hyperaldosteronism (Conn’s syndrome)***
- The combination of **hypertension**, **hypokalemia (K+ 3.1 mEq/L)**, and **metabolic alkalosis (pH 7.51)** is highly characteristic of primary hyperaldosteronism.
- Excess aldosterone leads to increased sodium reabsorption and potassium/hydrogen ion excretion, causing these electrolyte imbalances.
*Pheochromocytoma*
- This condition involves episodic **hypertension**, palpitations, sweating, and anxiety due to catecholamine excess.
- While hypertension is present, the absence of paroxysmal symptoms and the specific electrolyte abnormalities (hypokalemia, alkalosis) make it less likely.
*Renal artery stenosis*
- This can cause **secondary hypertension** and occasionally hypokalemia, but it typically presents with **renal bruits**, and the metabolic alkalosis is not a direct or prominent feature.
- The elevated renin-angiotensin-aldosterone axis would lead to secondary hyperaldosteronism, but primary hyperaldosteronism is suggested by the overall clinical picture.
*Cushing’s syndrome*
- Cushing's syndrome is characterized by **central obesity**, striae, moon facies, and **hyperglycemia**, among other symptoms.
- While hypertension and hypokalemia can occur in severe cases, the predominant clinical features are not aligned with this patient's presentation.
*Addison’s disease*
- This condition is characterized by **adrenal insufficiency**, leading to hypoglycemia, **hyponatremia**, **hyperkalemia**, and **hypotension**.
- The patient's hypertension and hypokalemia directly contradict the typical presentation of Addison’s disease.
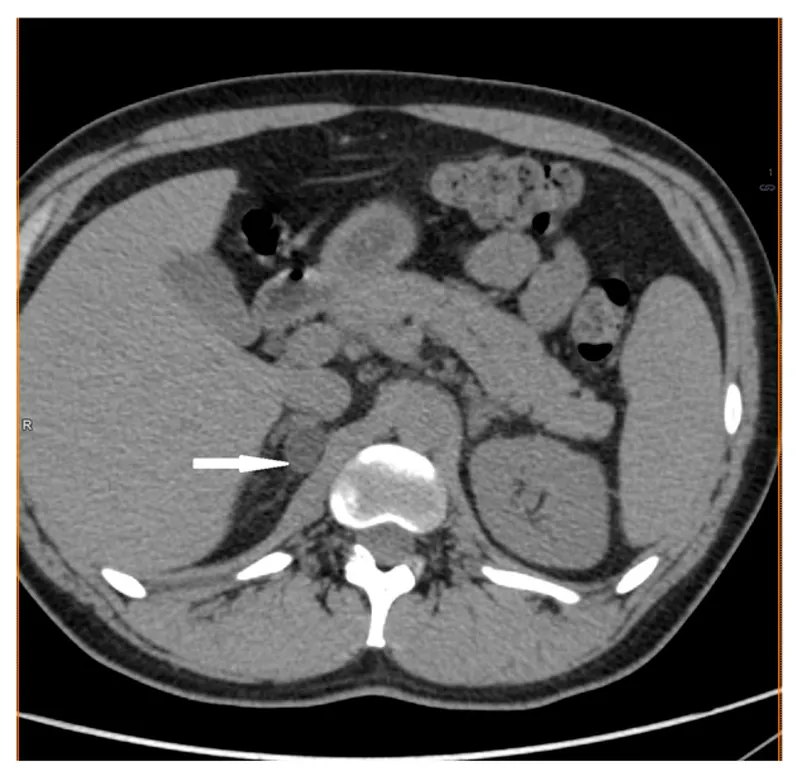
Adrenal disorders US Medical PG Question 5: A 32-year-old woman comes to the physician because of weight gain, generalized weakness, and irregular menstrual cycles for the past 16 months. She began having symptoms of insomnia and depression 10 months ago. More recently, she has been having difficulties rising from a chair. She has a 2-year history of hypertension. Current medications include citalopram and hydrochlorothiazide. She is 168 cm (5 ft 6 in) tall and weighs 100 kg (220 lb). BMI is 36 kg/m2. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. She appears tired and has a full, plethoric face and central obesity. Examination of the skin shows violaceous linear striations on her lower abdomen. Two midnight serum cortisol studies show measurements of 288 μg/L and 253 μg/L (N < 90); a 24-hour urinary cortisol measurement was 395 μg (N < 300). Upon follow-up laboratory examination, the patient's serum ACTH levels were also elevated at 136 pg/mL (N = 7–50). Which of the following is the most appropriate next step in evaluation?
- A. MRI of the head with contrast
- B. High-dose dexamethasone suppression test (Correct Answer)
- C. Measure ACTH levels in inferior petrosal sinuses
- D. Bilateral adrenalectomy
- E. CT scan of the abdomen with contrast
Adrenal disorders Explanation: ***High-dose dexamethasone suppression test***
- Elevated **midnight serum cortisol** and **24-hour urinary cortisol**, combined with elevated **ACTH levels**, confirm **ACTH-dependent Cushing's syndrome**.
- A high-dose dexamethasone suppression test helps **differentiate** between a pituitary adenoma (Cushing's disease), which typically suppresses with high-dose dexamethasone, and ectopic ACTH production, which usually does not.
*MRI of the head with contrast*
- While an MRI of the head might eventually be performed to localize a pituitary adenoma, it is **not the immediate next step** after establishing ACTH dependency.
- The high-dose dexamethasone suppression test provides crucial **functional information** about the source of ACTH prior to imaging.
*Measure ACTH levels in inferior petrosal sinuses*
- **Inferior petrosal sinus sampling (IPSS)** is used to **confirm and lateralize** a pituitary source of ACTH when imaging studies are equivocal or negative.
- This is an **invasive procedure** typically reserved for after the high-dose dexamethasone suppression test has been performed and further distinction is needed.
*Bilateral adrenalectomy*
- **Bilateral adrenalectomy** is a treatment option for Cushing's syndrome, particularly for severe cases or when other treatments fail.
- It is an **irreversible surgical procedure** and would only be considered after a definitive diagnosis and localization of the source of excess cortisol.
*CT scan of the abdomen with contrast*
- A CT scan of the abdomen is primarily used to evaluate for **adrenal adenomas or carcinomas** in cases of **ACTH-independent Cushing's syndrome**.
- Given the **elevated ACTH levels**, an adrenal etiology is less likely, making this an inappropriate next step.
Adrenal disorders US Medical PG Question 6: A 41-year-old woman comes to the physician because of a 1-year history of fatigue, irregular menstrual cycles, and recurrent sinus infections. Examination shows hirsutism and hypopigmented linear striations on the abdomen. Serum studies show hypernatremia, hypokalemia, and metabolic alkalosis. A 24-hour urinary cortisol level is elevated. Serum ACTH is also elevated. High-dose dexamethasone does not suppress serum cortisol levels. Which of the following is the most likely underlying cause of this patient's condition?
- A. Pheochromocytoma
- B. Adrenal adenoma
- C. Pituitary adenoma
- D. Adrenal carcinoma
- E. Small cell lung cancer (Correct Answer)
Adrenal disorders Explanation: ***Small cell lung cancer***
- The combination of **elevated ACTH** and **failure to suppress cortisol** with high-dose dexamethasone suggests an **ectopic ACTH-producing tumor**.
- **Small cell lung cancer** is the most common cause of **ectopic ACTH syndrome**, leading to severe Cushing's syndrome with rapid onset and significant metabolic derangements like **hypernatremia**, **hypokalemia**, and **metabolic alkalosis**.
*Pheochromocytoma*
- This condition causes episodic or sustained **hypertension** and symptoms related to catecholamine excess (e.g., palpitations, sweating, headaches).
- It does not primarily lead to the cortisol excess and distinct metabolic disturbances observed in this patient.
*Adrenal adenoma*
- An **adrenal adenoma** producing cortisol would lead to **Cushing's syndrome** with **low ACTH** due to negative feedback.
- The patient's **elevated ACTH** rules out a primary adrenal cause of cortisol excess.
*Pituitary adenoma*
- A **pituitary adenoma** (Cushing's disease) often shows **partial suppression** of cortisol with high-dose dexamethasone (though not always complete suppression).
- While it causes elevated ACTH, the prominent **metabolic derangements** and strong resistance to suppression are more typical of ectopic ACTH production.
*Adrenal carcinoma*
- An **adrenal carcinoma** producing cortisol would also lead to **Cushing's syndrome** with **low ACTH** due to negative feedback.
- The patient's **elevated ACTH** is inconsistent with a primary adrenal tumor.
Adrenal disorders US Medical PG Question 7: A 47-year-old woman complains of weight gain and irregular menses for the past 2 years. She has gained 13 kg (28.6 lb) and feels that most of the weight gain is in her abdomen and face. She has type 2 diabetes and hypertension for 1 year, and they are difficult to control with medications. Vital signs include a temperature of 36.9°C (98.4°F), blood pressure of 160/100 mm Hg, and pulse of 95/min. The patient's late-night salivary cortisol is elevated. Morning plasma ACTH is high. Brain magnetic resonance imaging shows a 2 cm pituitary adenoma. Which of the following is the optimal therapy for this patient?
- A. Unilateral adrenalectomy
- B. Bilateral adrenalectomy
- C. Pituitary radiotherapy
- D. Medical therapy
- E. Transsphenoidal pituitary adenomectomy (Correct Answer)
Adrenal disorders Explanation: ***Transsphenoidal pituitary adenomectomy***
- This patient presents with **Cushing's disease**, characterized by **elevated late-night salivary cortisol** and **high morning plasma ACTH**, coupled with a **pituitary adenoma** on MRI. **Transsphenoidal pituitary adenomectomy** is the first-line and most effective treatment for Cushing's disease, offering the highest chance of remission by directly removing the adenoma.
- Successful surgical removal of the tumor can quickly normalize **ACTH** and **cortisol** levels, leading to significant improvement in symptoms like **weight gain**, **hypertension**, **diabetes**, and **menstrual irregularities**.
*Unilateral adrenalectomy*
- This procedure treats **adrenal adenomas** causing Cushing's syndrome (primary adrenal hypercortisolism), which is characterized by **low or undetectable ACTH levels**. This patient has **high ACTH**, indicating a pituitary source.
- Performing a unilateral adrenalectomy in this case would not address the underlying **pituitary tumor** and would not cure Cushing's disease.
*Bilateral adrenalectomy*
- This is a treatment for severe, refractory Cushing's disease, or as a palliative measure, when **pituitary surgery** has failed or is contraindicated.
- While it effectively removes the source of **cortisol**, it leads to **adrenal insufficiency**, requiring lifelong corticosteroid replacement, and carries the risk of **Nelson's Syndrome** (rapid pituitary tumor growth due to loss of negative feedback).
*Pituitary radiotherapy*
- **Pituitary radiotherapy** is a secondary treatment option, typically used when **transsphenoidal surgery** fails to achieve remission, or if there is residual tumor.
- It has a slower onset of action (months to years) compared to surgery, and the patient's severe symptoms require more immediate control.
*Medical therapy*
- **Medical therapies** (e.g., **ketoconazole**, **mifepristone**, **pasireotide**) are often used as bridging therapy before surgery, when surgery is contraindicated, or for patients with persistent disease after surgery.
- They help control **hypercortisolism** but do not cure the underlying **pituitary adenoma**, making **surgical removal** the preferred definitive treatment.
Adrenal disorders US Medical PG Question 8: A 45-year-old woman comes to the physician because of fatigue, lightheadedness, dizziness upon standing, abdominal pain, and muscle pain over the past 6 months. She has also had an unintended weight loss of 5.8 kg (12.8 lb) over the past 3 years. She has had a history of hypoparathyroidism since she was a teenager. Her current medications include calcitriol and calcium carbonate. Her pulse is 85/min and blood pressure is 81/45 mm Hg. Physical examination shows tanned skin, as well as sparse axillary and pubic hair. Which of the following is the most likely cause of this patient's symptoms?
- A. Enzyme disorder
- B. Abdominal neoplasia
- C. Occult hemorrhage
- D. Autoimmune destruction (Correct Answer)
- E. Amyloid deposition
Adrenal disorders Explanation: ***Autoimmune destruction***
- The constellation of **fatigue, lightheadedness, orthostatic hypotension, weight loss, tanned skin, and sparse axillary/pubic hair** in a patient with a history of another autoimmune condition (hypoparathyroidism) is highly suggestive of **Addison's disease** (primary adrenal insufficiency), which is most commonly caused by autoimmune destruction of the adrenal glands.
- The skin tanning is due to increased **ACTH** (adrenocorticotropic hormone) and **melanocyte-stimulating hormone (MSH)** production as the pituitary tries to compensate for insufficient cortisol from the damaged adrenal glands.
*Enzyme disorder*
- While enzyme disorders can cause chronic symptoms, they typically do not present with the specific combination of **orthostatic hypotension, hyperpigmentation, and sparse secondary sexual hair** seen here.
- This presentation is a classic endocrine pattern, not typically associated with an isolated enzyme deficiency.
*Abdominal neoplasia*
- **Neoplasia** could explain weight loss and fatigue, but it typically doesn't cause **hyperpigmentation** or **sparse secondary sexual hair**, and it's less likely to directly cause **orthostatic hypotension** in this manner.
- The patient's symptoms are more consistent with an endocrine dysfunction rather than a localized abdominal mass effect or paraneoplastic syndrome that would mimic this exact presentation.
*Occult hemorrhage*
- Occult hemorrhage would likely cause **anemia**, leading to fatigue and lightheadedness, and potentially orthostatic changes.
- However, it would not explain the **tanned skin** (hyperpigmentation) or the **loss of axillary/pubic hair**, which are key features pointing to adrenal insufficiency.
*Amyloid deposition*
- Amyloidosis can affect various organs, including the adrenals, leading to adrenal insufficiency and other symptoms like fatigue and weight loss.
- While it's a possibility, **hyperpigmentation** and **sparse axillary/pubic hair** are more characteristic of autoimmune Addison's disease due to the specific hormonal changes (increased ACTH/MSH and decreased adrenal androgens).
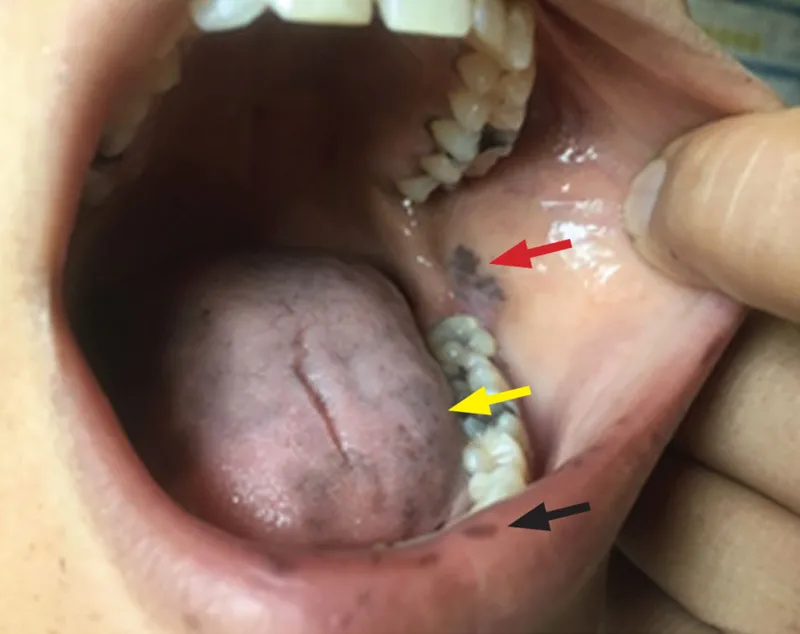
Adrenal disorders US Medical PG Question 9: A 48-year-old woman presents to her primary care physician with the complaints of persistent fatigue, dizziness, and weight loss for the past 3 months. She has hypothyroidism for 15 years and takes thyroxine replacement. Her blood pressure is 90/60 mm Hg in a supine position and 65/40 mm Hg while sitting, temperature is 36.8°C (98.2°F) and pulse is 75/min. On physical examination, there is a mild increase in thyroid size, with a rubbery consistency. Her skin shows diffuse hyperpigmentation, more pronounced in the oral mucosa and palmar creases. The morning serum cortisol test is found to be 3 µg/dL. Which of the following is the best next step in this case?
- A. Serum adrenocorticotropic hormone (ACTH)
- B. Plasma aldosterone
- C. 21-hydroxylase antibodies
- D. Adrenal imaging
- E. Adrenocorticotropic hormone (ACTH) stimulation test (Correct Answer)
Adrenal disorders Explanation: ***Adrenocorticotropic hormone (ACTH) stimulation test***
- The patient's symptoms (fatigue, dizziness, weight loss, orthostatic hypotension, hyperpigmentation) and a very low morning cortisol level (3 µg/dL) are highly suggestive of **adrenal insufficiency**.
- An **ACTH stimulation test** (cosyntropin test) is the gold standard for officially diagnosing adrenal insufficiency by measuring the adrenal glands' response to synthetic ACTH.
*Serum adrenocorticotropic hormone (ACTH)*
- While measuring **ACTH levels** is crucial to differentiate between primary and secondary adrenal insufficiency, it should be done after confirming adrenal insufficiency with an ACTH stimulation test.
- A high ACTH level in conjunction with low cortisol confirms **primary adrenal insufficiency**, whereas a low ACTH indicates **secondary adrenal insufficiency**.
*Plasma aldosterone*
- **Aldosterone measurements** are useful in evaluating primary adrenal insufficiency, as it can be affected in this condition (leading to salt wasting).
- However, the primary concern is cortisol deficiency, and confirming adrenal insufficiency takes precedence for immediate management and diagnosis.
*21-hydroxylase antibodies*
- **21-hydroxylase antibodies** are markers for **autoimmune adrenal insufficiency**, which is the most common cause of primary adrenal insufficiency.
- While relevant for etiology, this test is performed after the diagnosis of adrenal insufficiency has been established by the ACTH stimulation test.
*Adrenal imaging*
- **Adrenal imaging** (e.g., CT or MRI) is typically performed to investigate the cause of adrenal insufficiency, especially after biochemical confirmation.
- It helps in identifying adrenal masses, atrophy, or hemorrhage, but it is not the initial diagnostic step for functional assessment.
Adrenal disorders US Medical PG Question 10: A 35-year-old male is brought to the emergency room after he was found to have a blood pressure of 180/100 mm Hg during a routine health check-up with his family physician. Past medical history is insignificant and both of his parents are healthy. He currently does not take any medication. The patient's blood pressure normalizes before the emergency department physician can evaluate him. During the physical examination, his blood pressure is 148/80 mm Hg, heart rate is 65/min, temperature is 36.8°C (98.2°F), and respirations are 14/min. He has a round face, centripetal obesity, and striae on the skin with atrophy over the abdomen and thighs. On visual field examination, he is found to have loss of vision in the lateral visual fields bilaterally. You order a low dose dexamethasone suppression test, which is positive, and you proceed to measure ACTH and obtain a high-dose dexamethasone suppression test. If this is a pituitary gland disorder, which of the following lab abnormalities is most likely present in this patient?
- A. Before test: ACTH low, after test: cortisol elevation
- B. Before test: ACTH high, after test: aldosterone suppression
- C. Before test: ACTH high, after test: cortisol suppression (Correct Answer)
- D. Before test: ACTH low, after test: aldosterone normalizes
- E. Before test: ACTH high, after test: cortisol elevation
Adrenal disorders Explanation: ***Before test: ACTH high, after test: cortisol suppression***
- A diagnosis of **Cushing's disease** (pituitary ACTH overproduction) is supported by **high ACTH** levels before the high-dose dexamethasone suppression test.
- **Cortisol suppression** after a high-dose dexamethasone test helps differentiate Cushing's disease from ectopic ACTH production or adrenal tumors, as pituitary adenomas retain some sensitivity to feedback inhibition.
*Before test: ACTH low, after test: cortisol elevation*
- **Low ACTH** levels would indicate an adrenal etiology of Cushing's syndrome (e.g., adrenal adenoma), not a pituitary disorder.
- **Cortisol elevation** after the high-dose test would suggest an ectopic ACTH-producing tumor or adrenal tumor, as these are typically resistant to suppression.
*Before test: ACTH high, after test: aldosterone suppression*
- While ACTH may be high in Cushing's disease, the high-dose dexamethasone test primarily evaluates **cortisol suppression**, not aldosterone.
- Aldosterone levels are primarily regulated by the **renin-angiotensin-aldosterone system**, and its suppression is not a direct diagnostic feature of Cushing's disease in this context.
*Before test: ACTH low, after test: aldosterone normalizes*
- **Low ACTH** contradicts a pituitary origin, pointing towards an adrenal cause where adrenal cortisol overproduction suppresses ACTH.
- Normalization of aldosterone is not the expected or primary diagnostic outcome of a high-dose dexamethasone suppression test for Cushing's syndrome.
*Before test: ACTH high, after test: cortisol elevation*
- Although ACTH would be high before the test in a pituitary disorder, **cortisol elevation** *after* the high-dose dexamethasone test would indicate resistance to suppression.
- Resistance to suppression with high ACTH usually points towards **ectopic ACTH production** (e.g., from small cell lung cancer), not a pituitary adenoma.
More Adrenal disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.