Stable coronary artery disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Stable coronary artery disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
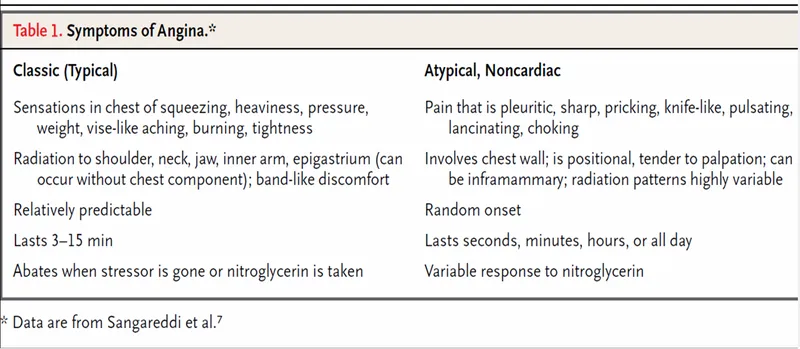
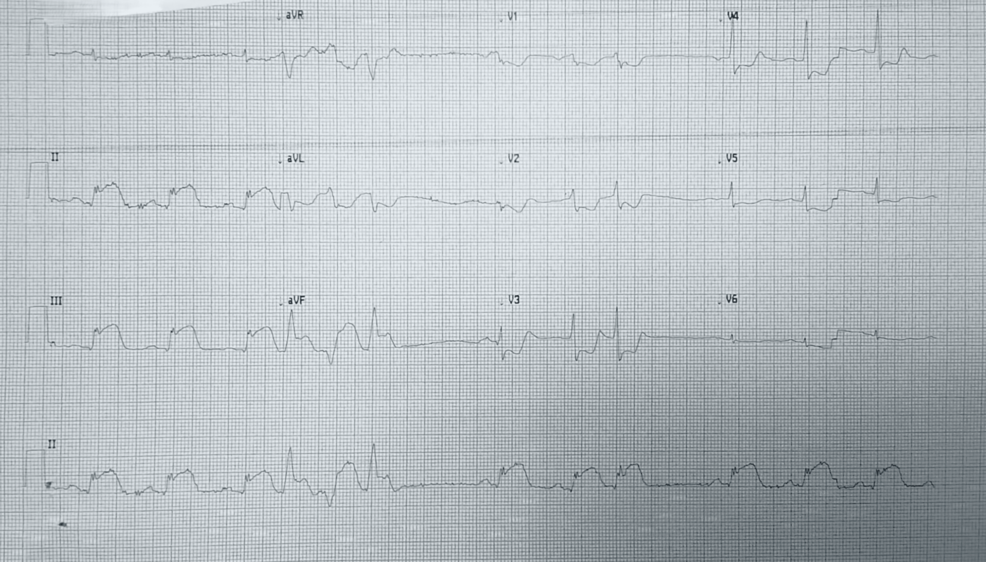
Stable coronary artery disease US Medical PG Question 1: A 64-year-old man presents to the emergency department with sudden onset of chest pain and an episode of vomiting. He also complains of ongoing nausea and heavy sweating (diaphoresis). He denies having experienced such symptoms before and is quite upset. Medical history is significant for hypertension and types 2 diabetes mellitus. He currently smokes and has smoked at least half a pack daily for the last 40 years. Vitals show a blood pressure of 80/50 mm Hg, pulse of 50/min, respirations of 20/min, temperature of 37.2°C (98.9°F), and oximetry is 99% before oxygen by facemask. Except for the patient being visibly distressed and diaphoretic, the examination is unremarkable. ECG findings are shown in the picture. Where is the most likely obstruction in this patient’s cardiac blood supply?
- A. Left anterior descending artery
- B. There is no obstruction
- C. Left circumflex artery
- D. Left main coronary artery
- E. Right coronary artery (Correct Answer)
Stable coronary artery disease Explanation: ***Right coronary artery***
- The ECG shows significant **ST elevation in leads II, III, and aVF**, indicating an **inferior wall myocardial infarction**. This region of the heart is typically supplied by the **right coronary artery (RCA)**.
- The patient's presentation with **bradycardia (pulse 50/min)**, **hypotension (BP 80/50 mmHg)**, and **nausea/vomiting** is classic for an inferior MI, often due to RCA occlusion compromising blood supply to the **SA and AV nodes** (which are frequently supplied by the RCA).
*Left anterior descending artery*
- Obstruction of the **LAD** typically causes **ST elevation in anterior leads (V1-V4)**, which is not seen here.
- An LAD occlusion would present as an **anterior MI**, usually without the severe bradycardia and hypotension often seen with inferior MIs caused by RCA occlusion.
*There is no obstruction*
- The patient's symptoms of **sudden onset chest pain, nausea, diaphoresis**, and particularly the **ECG findings of ST elevation** are highly indicative of an **acute myocardial infarction**, which is caused by coronary artery obstruction.
- The severe hemodynamic instability (hypotension, bradycardia) further points towards a significant cardiac event due to occlusion.
*Left circumflex artery*
- **LCx occlusion** usually leads to **lateral wall MI**, characterized by ST elevation in leads **I, aVL, V5, and V6**, which is not the primary pattern observed in this ECG.
- While LCx can sometimes supply the inferior wall, the classic inferior pattern seen here is more commonly associated with RCA occlusion.
*Left main coronary artery*
- **Left main coronary artery** occlusion is a catastrophic event leading to extensive myocardial ischemia and typically presents with widespread ST depressions or elevation in aVR, reflecting global ischemia and often causing **cardiogenic shock** or **sudden cardiac death**.
- The ECG pattern here is localized to the inferior leads, making a left main occlusion an unlikely primary cause.
Stable coronary artery disease US Medical PG Question 2: A 73-year-old man presents to the emergency department with acute substernal chest pain that began a few hours ago. The pain is described as a "pressure" that radiates to his left arm. His past medical history is significant for hypertension and hyperlipidemia. He is on chlorthalidone for his hypertension and simvastatin for hyperlipidemia. He has a 30 pack-year history of smoking and drinks 1-2 beers on weekends. His EKG shows ST depressions in the anterior precordial leads and he is given the proper medications and sent for emergency revascularization. Seven days later, he develops dyspnea that worsens in the supine position. Bibasilar crackles are heard on pulmonary auscultation. Cardiac exam reveals a new 3/6 holosystolic murmur best heard at the apex with radiation to the axilla. What is the most likely etiology of this patient's new symptoms?
- A. Ventricular wall aneurysm
- B. Restrictive pericarditis
- C. Papillary muscle rupture (Correct Answer)
- D. Aortic stenosis
- E. Arrhythmia
Stable coronary artery disease Explanation: ***Papillary muscle rupture***
- The sudden onset of **dyspnea**, **bibasilar crackles**, and a **new holosystolic murmur** after an acute myocardial infarction (MI) strongly suggests **mitral regurgitation**, often caused by papillary muscle rupture.
- This complication typically occurs **3-7 days post-MI** and leads to acute left heart failure, as described by the patient's worsening symptoms in the supine position and pulmonary edema.
*Ventricular wall aneurysm*
- A ventricular aneurysm is a late complication of MI, typically developing **weeks to months** later, not within 7 days.
- While it can cause heart failure and arrhythmias, a **new holosystolic murmur** is not a characteristic finding.
*Restrictive pericarditis*
- This condition involves the stiffening of the pericardium, leading to impaired ventricular filling, but it is typically a more **chronic process** and is not an acute complication of MI.
- The classic physical finding of a new holosystolic murmur with acute dyspnea is not consistent with restrictive pericarditis.
*Aortic stenosis*
- Aortic stenosis is a chronic valvular disease, usually presenting with a **systolic ejection murmur** best heard at the right upper sternal border, not a holosystolic murmur post-MI.
- While it can cause dyspnea, the acute onset following an MI with a new murmur suggests a different etiology.
*Arrhythmia*
- An arrhythmia can cause dyspnea and heart failure symptoms, but it would not explain the presence of a **new holosystolic murmur**, which indicates a structural cardiac issue.
- While common post-MI, the specific constellation of symptoms points to a mechanical complication.
Stable coronary artery disease US Medical PG Question 3: A 55-year-old man comes to the physician because of a 4-month history of episodic, pressure-like chest pain. The chest pain occurs when he is walking up stairs and improves with rest. He has hypertension and type 2 diabetes mellitus. His father died from a myocardial infarction at the age of 50 years. Current medications include hydrochlorothiazide and metformin. His pulse is 85/min, respirations are 12/min, and blood pressure is 140/90 mm Hg. Cardiac examination shows normal heart sounds without any murmurs, rubs, or gallops. An ECG shows high amplitude of the S wave in lead V3. An exercise stress test is performed but stopped after 4 minutes because the patient experiences chest pain. An ECG obtained during the stress test shows sinus tachycardia and ST-segment depressions in leads V1–V4. Which of the following is the most appropriate long-term pharmacotherapy to reduce the frequency of symptoms in this patient?
- A. Metoprolol (Correct Answer)
- B. Clopidogrel
- C. Aspirin
- D. Nitroglycerin
- E. Isosorbide mononitrate
Stable coronary artery disease Explanation: ***Metoprolol***
- **Beta-blockers** like metoprolol are first-line agents for **symptom relief** in stable angina by reducing myocardial oxygen demand.
- They decrease **heart rate**, **blood pressure**, and **myocardial contractility**, thereby reducing the frequency and severity of anginal episodes.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent used primarily to prevent **thrombotic events** in patients with established cardiovascular disease or acute coronary syndromes.
- It does not directly reduce the frequency of anginal symptoms, but rather prevents progression to **myocardial infarction** or **stroke**.
*Aspirin*
- **Aspirin** is an antiplatelet medication used for **secondary prevention** of cardiovascular events by inhibiting platelet aggregation.
- While crucial for reducing cardiovascular risk, it does not directly alleviate the **frequency of anginal symptoms** themselves.
*Nitroglycerin*
- **Nitroglycerin** is a short-acting nitrate used to provide **immediate relief** of anginal pain during an acute episode.
- It is not a long-term pharmacotherapy for reducing the *frequency* of symptoms.
*Isosorbide mononitrate*
- **Isosorbide mononitrate** is a long-acting nitrate used to *prevent* angina, but it is typically a **second-line agent** after beta-blockers due to potential for **tolerance** and side effects.
- While it can reduce symptom frequency, beta-blockers are generally preferred as initial long-term therapy for symptom control.
Stable coronary artery disease US Medical PG Question 4: A 50-year-old man comes to the physician for his annual health maintenance examination. The patient feels well. He has a history of hypertension, for which he currently takes lisinopril. He has smoked a pack of cigarettes daily for 20 years. He drinks 5–6 beers on weekends. He is 181 cm tall (5 ft 11 in), weighs 80 kg (176.4 lbs); BMI is 24.6 kg/m2. His pulse is 75/min, blood pressure is 140/85 mm Hg, and respirations are 18/min. Physical examination is unremarkable. Laboratory studies show:
Total cholesterol 263 mg/dL
High-density lipoprotein cholesterol 36 mg/dL
Triglycerides 180 mg/dL
In addition to dietary and lifestyle modification, administration of which of the following agents is the most appropriate next step in management?
- A. Peroxisome proliferator-activated receptor alpha activator
- B. Proprotein convertase subtilisin kexin 9 inhibitor
- C. Bile acid resins
- D. HMG-CoA reductase inhibitor (Correct Answer)
- E. Cholesterol absorption inhibitor
Stable coronary artery disease Explanation: ***HMG-CoA reductase inhibitor***
- This patient has multiple **cardiovascular risk factors** (hypertension, smoking, low HDL, elevated LDL-c calculated from total cholesterol and triglycerides) and elevated LDL-c. An **HMG-CoA reductase inhibitor (statin)** is the first-line pharmacotherapy in such cases to reduce the risk of atherosclerotic cardiovascular disease events.
- Statins effectively lower **LDL-c**, which is the primary target for cholesterol reduction in patients at high risk for cardiovascular disease.
*Peroxisome proliferator-activated receptor alpha activator*
- **Fibrates** (PPAR-α activators) are primarily used to lower **triglycerides** and increase HDL, and are not the first-line choice for lowering elevated LDL-c in high-risk patients.
- They are typically reserved for severe hypertriglyceridemia not controlled by statins, or in patients intolerant to statins whose primary lipid issue is hypertriglyceridemia.
*Proprotein convertase subtilisin kexin 9 inhibitor*
- **PCSK9 inhibitors** are potent LDL-c lowering agents, but they are typically used as **adjunctive therapy** in patients with high cardiovascular risk who have not achieved adequate LDL-c reduction with maximum tolerated statin therapy, or in patients with familial hypercholesterolemia.
- Given that this patient has not yet started statin therapy, a PCSK9 inhibitor is not the initial treatment strategy.
*Bile acid resins*
- **Bile acid resins** (e.g., cholestyramine) lower LDL-c by binding to bile acids in the intestine, but they are **less effective** than statins and can sometimes increase triglycerides.
- They are generally not the first-line choice for primary LDL-c reduction due to their side effect profile (e.g., GI upset) and lower efficacy compared to statins.
*Cholesterol absorption inhibitor*
- **Ezetimibe** (a cholesterol absorption inhibitor) reduces cholesterol absorption in the small intestine, leading to lower LDL-c.
- It is often used as an **add-on therapy** to statins or as monotherapy in statin-intolerant patients, but not as the initial drug of choice when a statin is indicated and tolerated.
Stable coronary artery disease US Medical PG Question 5: A 59-year-old man presents to his primary care provider complaining of bilateral calf cramping with walking for the past 7 months. His pain goes away when he stops walking; however, his condition affects his work as a mail carrier. His medical history is remarkable for type 2 diabetes mellitus, hyperlipidemia, and 25-pack-year smoking history. His ankle-brachial index (ABI) is found to be 0.70. The patient is diagnosed with mild to moderate peripheral artery disease. A supervised exercise program for 3 months, aspirin, and cilostazol are started. Which of the following is the best next step if the patient has no improvement?
- A. Revascularization (Correct Answer)
- B. Heparin
- C. Surgical decompression
- D. Pentoxifylline
- E. Amputation
Stable coronary artery disease Explanation: ***Revascularization***
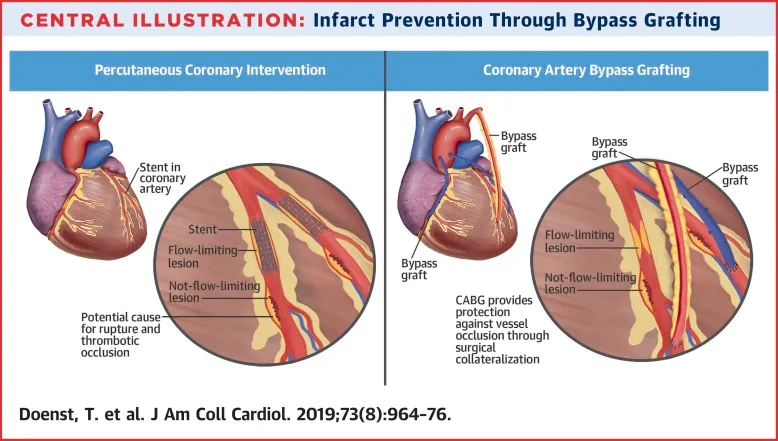
- For patients with **peripheral artery disease (PAD)** who fail to improve with conservative management (**supervised exercise, aspirin, and cilostazol**), **revascularization** is the next appropriate step to improve blood flow.
- This can be achieved through **endovascular procedures** (e.g., angioplasty with stenting) or **surgical bypass**, depending on the location and severity of the arterial blockage.
*Heparin*
- **Heparin** is an **anticoagulant** primarily used for acute thrombotic events or deep vein thrombosis (DVT), not for chronic management of stable claudication in PAD.
- It would not address the underlying **chronic arterial stenosis** causing the claudication symptoms.
*Surgical decompression*
- **Surgical decompression** is a treatment for conditions like **spinal stenosis** or **compartment syndrome**, not for peripheral arterial disease.
- The patient's symptoms (calf cramping with walking, resolving at rest) and **ABI of 0.70** are classic for **vascular claudication**, not nerve or muscle compression.
*Pentoxifylline*
- **Pentoxifylline** is an alternative medication used in PAD to improve blood flow by reducing blood viscosity.
- However, it is generally **less effective** than cilostazol and is typically considered when cilostazol is contraindicated or not tolerated, rather than as a next step after initial medical therapy failure with cilostazol.
*Amputation*
- **Amputation** is a last resort, usually reserved for **critical limb ischemia** with non-healing ulcers, gangrene, or intractable rest pain, where revascularization is not feasible or has failed.
- The patient's current symptoms are **intermittent claudication**, which is not immediately limb-threatening.
Stable coronary artery disease US Medical PG Question 6: A 59-year-old man presents to a clinic with exertional chest pain for the past several months. He says the pain is central in his chest and relieved with rest. The physical examination is unremarkable. An electrocardiogram is normal, but an exercise tolerance test revealed ST-segment depression in chest leads V1-V4. He is prescribed nitroglycerin to be taken in the first half of the day. Which of the following statements best describes the reason behind the timing of this medication?
- A. To prevent methemoglobinemia
- B. More effective in patients with angina due to anemia
- C. To avoid nitrate tolerance (Correct Answer)
- D. To prevent collapse
- E. To avoid nitrate headache
Stable coronary artery disease Explanation: ***To avoid nitrate tolerance***
- Chronic or continuous exposure to nitrates leads to **nitrate tolerance**, where therapeutic effectiveness diminishes over time.
- A **nitrate-free interval** (typically 10-14 hours, such as overnight or during the latter half of the day) allows restoration of nitrate sensitivity and maintains therapeutic efficacy.
- This is the primary reason for timing nitrate administration to the first half of the day.
*To prevent methemoglobinemia*
- **Methemoglobinemia** is a rare, dose-related complication typically seen with nitrate overdose or very high doses, not standard therapeutic use.
- The timing of nitroglycerin administration is not designed to prevent this rare adverse effect.
*More effective in patients with angina due to anemia*
- This statement is **not medically accurate**. Nitroglycerin timing is unrelated to whether angina is caused by anemia or coronary artery disease.
- Anemia-related angina is managed by correcting the underlying anemia, and nitrate efficacy does not vary based on anemia status.
*To prevent collapse*
- While nitroglycerin can cause **hypotension** and potential syncope due to vasodilation, this is an acute effect managed by dose titration and patient education.
- The nitrate-free interval strategy addresses **tolerance prevention**, not acute hemodynamic side effects.
*To avoid nitrate headache*
- **Nitrate-induced headache** is a common acute side effect caused by cerebral vasodilation, typically occurring shortly after administration.
- The timing strategy (nitrate-free interval) is designed to prevent tolerance, not to avoid this acute side effect, which usually diminishes with continued use.
Stable coronary artery disease US Medical PG Question 7: A 39-year-old woman comes to the physician because of a 5-month history of episodic retrosternal chest pain. She currently feels well. The pain is unrelated to exercise and does not radiate. The episodes typically last less than 15 minutes and lead to feelings of anxiety; resting relieves the pain. She has not had dyspnea or cough. She has hyperlipidemia treated with simvastatin. She does not smoke, drink alcohol, or use illicit drugs. Her temperature is 37°C (98.6°F), pulse is 104/min, respirations are 17/min, and blood pressure is 124/76 mm Hg. Cardiopulmonary examination shows no abnormalities. An ECG shows sinus tachycardia. Which of the following is the most appropriate next step in the evaluation of coronary artery disease in this patient?
- A. Nuclear exercise stress test
- B. No further testing needed
- C. Troponin I measurement
- D. Dobutamine stress echocardiography
- E. Coronary CT angiogram (Correct Answer)
Stable coronary artery disease Explanation: ***Coronary CT angiogram***
- This patient has symptoms (non-exertional chest pain) raising suspicion for coronary artery disease (CAD), but her pre-test probability is low due to young age, female gender, and non-anginal features, making **coronary CT angiogram** an appropriate non-invasive first-line test.
- CT angiogram offers high sensitivity for detecting **coronary atherosclerosis** and can rule out CAD in patients with low-to-intermediate pretest probability.
*Nuclear exercise stress test*
- This test is typically reserved for patients with a **higher pre-test probability of CAD** or those with equivocal initial findings, as it involves radiation exposure and is more resource-intensive.
- The patient's chest pain is **unrelated to exercise**, making an exercise-based stress test less directly relevant as a first-line diagnostic.
*No further testing needed*
- While the patient's symptoms are atypical, her risk factor (hyperlipidemia) and recurrent retrosternal pain warrant further evaluation to **rule out CAD**, even with a low pre-test probability.
- Dismissing symptoms without further testing could miss early or atypical presentations of CAD.
*Troponin I measurement*
- **Troponin I** is used to diagnose **acute myocardial infarction** and indicates active myocardial necrosis; it is not for evaluating chronic, episodic chest pain in a patient who currently feels well.
- Her current well-being and the episodic nature of her pain make acute cardiac injury unlikely, and a normal troponin would not rule out underlying CAD.
*Dobutamine stress echocardiography*
- **Dobutamine stress echocardiography** is typically used for patients who cannot perform an exercise stress test (e.g., due to mobility issues) or when an exercise ECG is non-diagnostic.
- Given the patient's ability to exert herself (implied by no known mobility issues) and a non-exertional pain pattern, a CT angiogram offers superior anatomical detail for initial investigation.
Stable coronary artery disease US Medical PG Question 8: A 60-year-old male presents for a routine health check-up. The patient complains of reduced exercise tolerance for the past 2 years. Also, in the past year, he has noticed chest pain after climbing the stairs in his home. He has no significant past medical history or current medications. The patient reports a 45-pack-year smoking history. The vital signs include temperature 37.0°C (98.6°F), blood pressure 160/100 mm Hg, pulse 72/min, respiratory rate 15/min, and oxygen saturation 99% on room air. His body mass index (BMI) is 34 kg/m2. Physical examination is unremarkable. Laboratory studies show:
Serum total cholesterol 265 mg/dL
HDL 22 mg/dL
LDL 130 mg/dL
Triglycerides 175 mg/dL
HDL: high-density lipoprotein; LDL: low-density lipoprotein
Which of the following vascular pathologies is most likely present in this patient?
- A. Medial calcific sclerosis
- B. Deep venous thrombosis
- C. Lymphedema
- D. Atherosclerosis (Correct Answer)
- E. Hyperplastic arteriosclerosis
Stable coronary artery disease Explanation: ***Atherosclerosis***
- This patient presents with multiple **risk factors for atherosclerosis**, including **hyperlipidemia** (elevated total cholesterol, LDL, and triglycerides with low HDL), **hypertension**, **obesity**, and a significant **smoking history**.
- His symptoms of **reduced exercise tolerance** and **exertional chest pain** are classic manifestations of **angina pectoris**, which is caused by narrowed coronary arteries due to atherosclerosis.
*Medial calcific sclerosis*
- Also known as **Mönckeberg arteriosclerosis**, involves calcification of the **tunica media** of muscular arteries, without significant luminal narrowing.
- While it can lead to **artery hardening**, it typically does not obstruct blood flow or cause angina, and is more common in **elderly** and **diabetic** individuals.
*Deep venous thrombosis*
- This condition involves the formation of a **blood clot in a deep vein**, usually in the legs, leading to symptoms like **leg swelling, pain, and redness**.
- The patient's symptoms of chest pain and reduced exercise tolerance are not characteristic of DVT.
*Lymphedema*
- Characterized by **swelling** in one or more limbs due to an impaired **lymphatic drainage system**.
- It does not present with chest pain or reduced exercise tolerance and is distinct from vascular pathologies affecting blood flow.
*Hyperplastic arteriosclerosis*
- This is a form of **arteriolar sclerosis** primarily seen in severe **hypertension**, characterized by **concentric thickening of arteriolar walls** due to smooth muscle cell proliferation and basement membrane duplication.
- While the patient has hypertension, his symptoms point towards obstruction of larger coronary arteries rather than widespread arteriolar changes, and his lipid profile is more indicative of atherosclerosis.
Stable coronary artery disease US Medical PG Question 9: A 72-year-old man comes to the physician because of a 2-month history of intermittent retrosternal chest pain and tightness on exertion. He has type 2 diabetes mellitus, osteoarthritis of the right hip, and hypertension. Current medications include insulin, ibuprofen, enalapril, and hydrochlorothiazide. Vital signs are within normal limits. His troponin level is within the reference range. An ECG at rest shows a right bundle branch block and infrequent premature ventricular contractions. The patient's symptoms are reproduced during adenosine stress testing. Repeat ECG during stress testing shows new ST depression of > 1 mm in leads V2, V3, and V4. Which of the following is the most important underlying mechanism of this patient's ECG changes?
- A. Diversion of blood flow from stenotic coronary arteries (Correct Answer)
- B. Transient atrioventricular nodal blockade
- C. Reduced left ventricular preload
- D. Ruptured cholesterol plaque within a coronary vessel
- E. Increased myocardial oxygen demand
Stable coronary artery disease Explanation: ***Diversion of blood flow from stenotic coronary arteries***
- The **adenosine stress test** induces **submaximal coronary vasodilation** in healthy vessels, diverting blood flow away from stenosed areas that are already maximally dilated, a phenomenon known as **coronary steal**.
- This **relative hypoperfusion** in areas supplied by stenotic arteries leads to myocardial ischemia, manifested as **new ST depression** on the ECG due to **subendocardial oxygen supply-demand mismatch**.
*Transient atrioventricular nodal blockade*
- While adenosine can cause transient AV nodal blockade, leading to AV blocks, this would manifest as specific changes in **PR interval** or **QRS drop-out**, not ST segment depression indicative of ischemia.
- The patient's symptoms and ECG changes point towards myocardial ischemia, not an AV conduction disturbance.
*Reduced left ventricular preload*
- Reduced preload can occur in certain cardiac conditions but is not the primary mechanism behind ST depression during an adenosine stress test.
- ECG changes due to reduced preload are usually nonspecific, such as **sinus tachycardia** or **low voltage**, and do not typically cause new ST depression in specific leads.
*Ruptured cholesterol plaque within a coronary vessel*
- A ruptured plaque with subsequent **thrombus formation** would lead to **acute coronary syndrome (ACS)**, characterized by persistent chest pain, **elevated troponins**, and potentially **ST elevation** or new **pathologic Q waves** if complete occlusion occurs.
- The patient's troponin level is normal, and his symptoms are intermittent and reproducible on stress testing, which is more consistent with **stable angina**.
*Increased myocardial oxygen demand*
- While increased myocardial oxygen demand is a component of angina pectoris, adenosine primarily causes **coronary vasodilation**, which can worsen ischemia in stenotic areas by diverting blood flow, rather than directly increasing myocardial oxygen demand itself.
- **Dobutamine stress testing** would be the test that primarily increases myocardial oxygen demand.
Stable coronary artery disease US Medical PG Question 10: A 57-year-old man presents to his primary care provider because of chest pain for the past 3 weeks. The chest pain occurs after climbing more than 2 flight of stairs or walking for more than 10 minutes and resolves with rest. He is obese, has a history of type 2 diabetes mellitus, and has smoked 15-20 cigarettes a day for the past 25 years. His father died from a myocardial infarction at 52 years of age. Vital signs reveal a temperature of 36.7 °C (98.06°F), a blood pressure of 145/93 mm Hg, and a heart rate of 85/min. The physical examination is unremarkable. Which of the following best represents the most likely etiology of the patient’s condition?
- A. Hypertrophy of the interventricular septum
- B. Multivessel atherosclerotic disease with or without a nonocclusive thrombus
- C. Intermittent coronary vasospasm with or without coronary atherosclerosis
- D. Fixed, atherosclerotic coronary stenosis (> 70%) (Correct Answer)
- E. Sudden disruption of an atheromatous plaque, with a resulting occlusive thrombus
Stable coronary artery disease Explanation: ***Fixed, atherosclerotic coronary stenosis (> 70%)***
- The patient's presentation with **exertional chest pain** that resolves with rest (stable angina), along with multiple **cardiovascular risk factors** (obesity, type 2 diabetes mellitus, smoking, family history of early MI, hypertension), strongly points towards **stable ischemic heart disease**.
- This clinical picture is typically caused by a **fixed, hemodynamically significant stenosis** in one or more coronary arteries, usually greater than 70%, that limits blood flow during increased demand.
*Multivessel atherosclerotic disease with or without a nonocclusive thrombus*
- While the patient likely has **multivessel atherosclerosis**, the phrase "with or without a nonocclusive thrombus" leans towards **unstable angina** or NSTEMI, which typically involves a sudden change in symptoms or rest angina.
- The patient's symptoms are **stable and reproducible** with exertion, resolving with rest, which is characteristic of stable angina rather than a thrombotic event.
*Sudden disruption of an atheromatous plaque, with a resulting occlusive thrombus*
- This mechanism describes an **acute coronary syndrome (ACS)**, such as an **ST-elevation myocardial infarction (STEMI)** or **non-ST-elevation myocardial infarction (NSTEMI)**.
- ACS typically presents with new-onset, worsening, or rest angina, which is different from the stable, exertional pattern described in the patient.
*Intermittent coronary vasospasm with or without coronary atherosclerosis*
- **Coronary vasospasm** (e.g., Prinzmetal angina) typically causes chest pain that occurs **at rest**, often at night or in the early morning, and is not necessarily related to exertion.
- While the patient could have underlying atherosclerosis, the **predictable exertional nature** of his symptoms makes vasospasm less likely as the primary etiology.
*Hypertrophy of the interventricular septum*
- **Interventricular septal hypertrophy** is characteristic of **hypertrophic cardiomyopathy (HCM)**, which can cause exertional chest pain due to outflow tract obstruction or myocardial ischemia.
- However, HCM is less likely to be the primary etiology in a 57-year-old with multiple classic **atherosclerotic risk factors** and no mention of a heart murmur or family history of HCM.
More Stable coronary artery disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.