Peripheral arterial disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peripheral arterial disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Peripheral arterial disease US Medical PG Question 1: A 70-year-old man comes to the physician for the evaluation of pain, cramps, and tingling in his lower extremities over the past 6 months. The patient reports that the symptoms worsen with walking more than two blocks and are completely relieved by rest. Over the past 3 months, his symptoms have not improved despite his participating in supervised exercise therapy. He has type 2 diabetes mellitus. He had smoked one pack of cigarettes daily for the past 50 years, but quit 3 months ago. He does not drink alcohol. His current medications include metformin, atorvastatin, and aspirin. Examination shows loss of hair and decreased skin temperature in the lower legs. Femoral pulses are palpable; pedal pulses are absent. Which of the following is the most appropriate treatment for this patient?
- A. Compression stockings
- B. Endarterectomy
- C. Bypass surgery
- D. Percutaneous transluminal angioplasty
- E. Administration of cilostazol (Correct Answer)
Peripheral arterial disease Explanation: ***Administration of cilostazol***
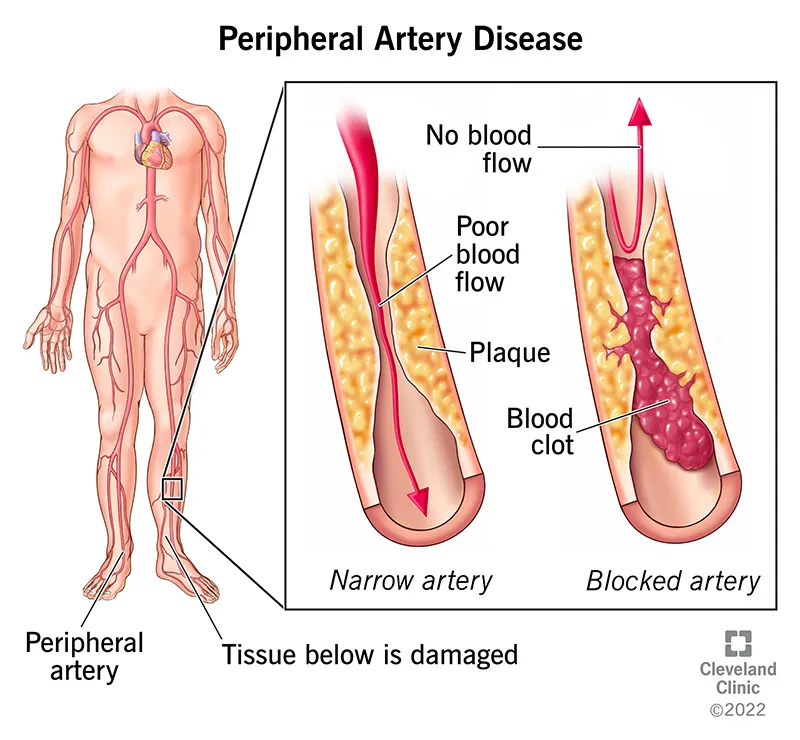
- The patient presents with classic symptoms of **peripheral artery disease (PAD)**, including **intermittent claudication** (pain with exertion, relieved by rest), **loss of hair**, **decreased skin temperature**, and **absent pedal pulses**.
- **Cilostazol** is a phosphodiesterase inhibitor that improves walking distance and reduces symptoms of claudication by causing **vasodilation** and inhibiting **platelet aggregation**.
*Compression stockings*
- Compression stockings are primarily used for conditions like **venous insufficiency** or **lymphedema**, which involve problems with venous return or lymphatic drainage.
- They are **contraindicated** in patients with significant PAD because they can further occlude already compromised arterial flow and worsen tissue ischemia.
*Endarterectomy*
- **Endarterectomy** is a surgical procedure to remove plaque from the inner lining of an artery. It is indicated for **localized, severe arterial stenosis** and is more invasive than other revascularization options.
- While it can be considered for PAD, less invasive options are usually tried first, especially in a patient who has not yet received optimal medical therapy.
*Bypass surgery*
- **Bypass surgery** involves rerouting blood flow around a blocked artery using a graft (vein or synthetic material). It is a more invasive revascularization procedure for PAD with significant, extensive arterial occlusions.
- It is typically reserved for **severe symptoms** refractory to medical management and less invasive procedures, or for critical limb ischemia.
*Percutaneous transluminal angioplasty*
- **Percutaneous transluminal angioplasty (PTA)** is a minimally invasive procedure that uses a balloon to widen a narrowed artery, often with stent placement.
- It is an effective revascularization option for PAD but is generally considered after lifestyle modifications and pharmacotherapy (like cilostazol) have failed to improve symptoms sufficiently.
Peripheral arterial disease US Medical PG Question 2: A 67-year-old man comes to the office due to pain in the lower part of his calves on his afternoon walk to get the mail. The pain is relieved by rest. It started slowly about 6 months ago and has become more painful over time. He has a history of hypertension, hyperlipidemia, diabetes mellitus, and a 20-pack-year smoking history. Medications include hydrochlorothiazide, atorvastatin, metformin, and a multivitamin that he takes daily. The patient quit smoking 2 years ago and only drinks socially. Today, his blood pressure is 145/90 mm Hg, pulse is 75/min, respiratory rate is 17/min, and temperature is 37.6°C (99.6°F). On physical exam, he appears mildly obese and healthy. His heart has a regular rate and rhythm, and his lungs are clear to auscultation bilaterally. Examination of the legs shows atrophic changes and diminished pedal pulses. A measure of his ankle brachial index (ABI) is 0.89. Which of the following is the most appropriate initial treatment?
- A. A recommendation to walk more
- B. Metoprolol
- C. A recommendation to perform pedal pumping exercises
- D. A referral to a supervised exercise program (Correct Answer)
- E. Enoxaparin
Peripheral arterial disease Explanation: ***A referral to a supervised exercise program***
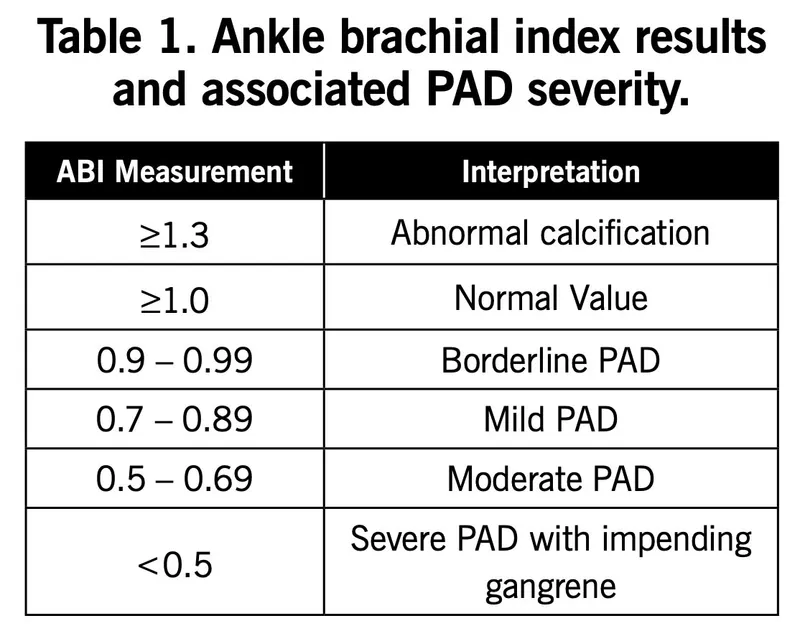
- The patient's symptoms (claudication, relief with rest), risk factors (**hypertension, hyperlipidemia, diabetes, smoking history**), physical exam findings (**atrophic changes, diminished pedal pulses**), and **ABI of 0.89** (indicating mild peripheral artery disease) all point to **peripheral arterial disease (PAD)**.
- A **supervised exercise program**, particularly walking, is the most effective initial non-pharmacological treatment for improving walking distance and quality of life in patients with claudication due to PAD.
*A recommendation to walk more*
- While walking is beneficial, simply recommending "walking more" without specific guidance or supervision is less effective than a structured program.
- An unsupervised general walking recommendation may not optimize the **duration**, **intensity**, or **frequency** needed for therapeutic benefit in PAD.
*Metoprolol*
- **Beta-blockers** like metoprolol can worsen claudication symptoms by decreasing blood flow to the extremities, especially in patients with PAD.
- They are generally **contraindicated** or used with caution in PAD patients experiencing claudication.
*A recommendation to perform pedal pumping exercises*
- **Pedal pumping exercises** are primarily used to prevent **venous stasis** and **deep vein thrombosis**, typically post-surgery or during prolonged immobility.
- They do not address the underlying arterial insufficiency causing claudication and are not an effective treatment for PAD.
*Enoxaparin*
- **Enoxaparin** is a low molecular weight heparin, an **anticoagulant** used for conditions like deep vein thrombosis or acute coronary syndromes.
- It is not indicated for the chronic management of stable claudication in peripheral artery disease, where antiplatelet therapy is generally preferred if medication is needed.
Peripheral arterial disease US Medical PG Question 3: A 53-year-old Asian woman comes to the physician because of a 2-month history of severe pain in her right leg while walking. She used to be able to walk a half-mile (800-m) to the grocery store but has been unable to walk 200 meters without stopping because of the pain over the past month. She can continue to walk after a break of around 5 minutes. She has hypertension, atrial fibrillation, and type 2 diabetes mellitus. She has smoked one pack of cigarettes daily for the past 32 years. Current medications include metformin, enalapril, aspirin, and warfarin. Vital signs are within normal limits. Examination shows an irregularly irregular pulse. The right lower extremity is cooler than the left lower extremity. The skin over the right leg appears shiny and dry. Femoral pulses are palpated bilaterally; pedal pulses are diminished on the right side. Which of the following is the most appropriate next step in management?
- A. MRI spine screening
- B. Duplex ultrasonography
- C. Ankle-brachial index (Correct Answer)
- D. Nerve conduction studies
- E. Biopsy of tibial artery
Peripheral arterial disease Explanation: ***Ankle-brachial index***
- The patient's symptoms of **intermittent claudication** (leg pain with exertion relieved by rest) and risk factors (smoking, diabetes, atrial fibrillation, hypertension) are highly suggestive of **peripheral artery disease (PAD)**. The **ankle-brachial index (ABI)** is the most appropriate initial diagnostic step as it is a quick, non-invasive, and reliable test to screen for PAD by comparing blood pressure in the ankles to blood pressure in the arms.
- A **diminished pedal pulse** on the right side and **cooler, shiny, dry skin** further support the suspicion of PAD, making ABI crucial for confirming the diagnosis and assessing its severity.
*MRI spine screening*
- While spinal pathology can cause leg pain, symptoms like **neurogenic claudication** typically improve with leaning forward or sitting and are not consistently relieved by standing still. The patient's pain relief with rest after walking points away from spinal stenosis.
- The patient's specific peripheral signs like a **cooler leg**, **diminished pedal pulses**, and **trophic changes** are not typical findings for spinal compression.
*Duplex ultrasonography*
- **Duplex ultrasonography** is a more advanced imaging technique used to visualize the blood vessels and assess blood flow, typically performed *after* an abnormal ABI confirms the presence of PAD.
- It helps in **localizing stenoses** and assessing their severity, but it is not the primary diagnostic screening tool in the initial evaluation of suspected PAD.
*Nerve conduction studies*
- **Nerve conduction studies (NCS)** are used to diagnose neuropathies. While diabetes is a risk factor for neuropathy, the patient's symptoms are classic for **vascular claudication** (pain with exertion, relieved by rest), rather than neuropathic pain, which is often described as burning, tingling, or numbing and does not typically resolve promptly with rest.
- The physical exam findings of a **cool leg** and **diminished pulses** are not consistent with a primary neurological problem.
*Biopsy of tibial artery*
- A **biopsy of the tibial artery** is an invasive procedure generally reserved for specific types of vasculitis (e.g., giant cell arteritis, polyarteritis nodosa) when other less invasive diagnostics have been inconclusive or raised suspicion for these conditions.
- It is not indicated for the initial workup of suspected **atherosclerotic peripheral artery disease**, which is the most likely diagnosis given the patient's risk factors and symptoms.
Peripheral arterial disease US Medical PG Question 4: A 75-year-old man presents to the emergency department because of pain in his left thigh and left calf for the past 3 months. The pain occurs at rest, worsens with walking, and is slightly improved by hanging his foot off the bed. He has had hypertension for 25 years and type 2 diabetes mellitus for 30 years. He has smoked 30–40 cigarettes per day for the past 45 years. On examination, the femoral, popliteal, and dorsalis pedis pulses are diminished, but detectable on both sides. The patient’s foot is shown in the image. Which of the following is the most likely diagnosis?
- A. Pseudogout
- B. Raynaud’s phenomenon
- C. Venous ulcer
- D. Critical limb ischemia (Correct Answer)
- E. Cellulitis
Peripheral arterial disease Explanation: **Critical limb ischemia**
- The patient exhibits classic symptoms of **critical limb ischemia (CLI)**, including **rest pain** in the lower extremities that is relieved by dependency (hanging foot off the bed), along with **diminished pulses** and significant risk factors like **smoking, hypertension, and diabetes**.
- The image further supports CLI by showing **ischemic changes** in the toes, such as **gangrene** of the second and third toes and **subungual hemorrhage** in the great toe, indicative of severe arterial insufficiency.
*Pseudogout*
- Pseudogout typically presents as acute, painful arthritis of a single joint, most commonly the **knee**, due to calcium pyrophosphate crystal deposition.
- It does not cause diffuse leg pain, diminished pulses, or ischemic changes in the toes as seen in this patient.
*Raynaud's phenomenon*
- Raynaud's phenomenon is characterized by episodic **vasospasm** leading to blanching, cyanosis, and redness, primarily affecting the fingers and toes, often triggered by cold or stress.
- While it involves digital ischemia, it is usually episodic, affects multiple digits symmetrically, and does not explain the chronic rest pain, diminished pulses, or gangrenous changes seen here.
*Venous ulcer*
- Venous ulcers are typically found around the **malleoli**, have irregular borders, and are associated with **edema**, **stasis dermatitis**, and normal pulses.
- The patient's symptoms of rest pain, relief with dependency, and digital gangrene, along with diminished arterial pulses, are not consistent with venous disease.
*Cellulitis*
- Cellulitis is a bacterial skin infection characterized by **erythema**, **warmth**, **swelling**, and pain, often with a rapidly spreading border.
- Although the image shows some redness, the patient's chronic symptoms, diminished pulses, and clear signs of tissue necrosis in the toes are inconsistent with primary cellulitis and point towards an underlying vascular etiology.
Peripheral arterial disease US Medical PG Question 5: A 58-year-old man comes to the physician because of a 3-month history of intermittent pain in his right calf that occurs after walking up more than 2 flights of stairs. He reports that the pain is associated with a tingling sensation and lasts for about 10 minutes. He is otherwise healthy. He has smoked 2 packs of cigarettes daily for 30 years and drinks 1 alcoholic beverage daily. He currently takes no medications. His pulse is 78/min, and blood pressure is 180/110 mm Hg. Physical examination shows yellow plaques below the lower eyelids bilaterally, loss of hair on the distal third of the right leg, and brittle toenails on the right foot. Femoral pulses are palpable bilaterally; right popliteal and pedal pulses are absent. Which of the following is the most appropriate management to prevent future morbidity and mortality of this patient's condition?
- A. Clopidogrel therapy (Correct Answer)
- B. Percutaneous transluminal angioplasty
- C. Cilostazol therapy
- D. Graded exercise therapy
- E. Pentoxifylline therapy
Peripheral arterial disease Explanation: ***Clopidogrel therapy***
- **Antiplatelet therapy** with clopidogrel (or aspirin) is crucial for **preventing future morbidity and mortality** in PAD patients by reducing the risk of **myocardial infarction**, stroke, and cardiovascular death.
- PAD is a manifestation of systemic atherosclerosis, and these patients have significantly elevated cardiovascular risk. Antiplatelet therapy addresses this systemic risk and is a cornerstone of medical management.
- Current guidelines (ACC/AHA) strongly recommend antiplatelet therapy for all patients with symptomatic PAD to reduce adverse cardiovascular events.
*Graded exercise therapy*
- **Graded exercise therapy** is highly effective for improving walking distance and reducing claudication symptoms by promoting collateral circulation and improving endothelial function.
- While exercise is essential for symptom management and quality of life, it is **not the primary intervention for preventing mortality** in PAD patients, which is what this question specifically asks about.
- Exercise should be recommended alongside antiplatelet therapy and risk factor modification.
*Pentoxifylline therapy*
- **Pentoxifylline** may improve red blood cell flexibility and microcirculation, but it has shown limited efficacy for symptom relief and **no proven benefit for reducing cardiovascular mortality**.
- Its use is generally reserved for patients who cannot tolerate other treatments.
*Percutaneous transluminal angioplasty*
- **Revascularization** (PTA or surgical bypass) is typically reserved for patients with severe, lifestyle-limiting claudication unresponsive to medical therapy, or for critical limb ischemia.
- This patient has intermittent claudication with moderate symptoms, making conservative medical management more appropriate initially.
- Revascularization improves symptoms but does not reduce mortality compared to medical therapy alone.
*Cilostazol therapy*
- **Cilostazol** is a phosphodiesterase-3 inhibitor that improves walking distance and claudication symptoms through vasodilation and antiplatelet effects.
- While effective for symptomatic relief, it does **not reduce cardiovascular mortality** and has a contraindication in heart failure patients.
- It is used as an adjunct for symptom management, not as primary prevention of morbidity and mortality.
Peripheral arterial disease US Medical PG Question 6: A 75-year-old man presents to the emergency department because of pain in his left thigh and left calf for the past 3 months. The pain occurs at rest, increases with walking, and is mildly improved by hanging the foot off the bed. He has had hypertension for 25 years and type 2 diabetes mellitus for 30 years. He has smoked 30–40 cigarettes per day for the past 45 years. On examination, femoral, popliteal, and dorsalis pedis pulses are faint on both sides. The patient’s foot is shown in the image. Resting ankle-brachial index (ABI) is found to be 0.30. Antiplatelet therapy and aggressive risk factors modifications are initiated. Which of the following is the best next step for this patient?
- A. Cilostazol
- B. Exercise therapy
- C. Urgent assessment for revascularization (Correct Answer)
- D. Amputation
- E. Systemic anticoagulation with heparin
Peripheral arterial disease Explanation: ***Urgent assessment for revascularization***
- The patient presents with **critical limb ischemia (CLI)**, indicated by rest pain, non-healing wounds, and an extremely low ankle-brachial index (ABI) of 0.30. CLI requires urgent revascularization to prevent limb loss.
- The clinical picture (rest pain relieved by dependency, long-standing risk factors like smoking, hypertension, diabetes, and faint pulses) points to severe **peripheral arterial disease (PAD)** that has progressed to a limb-threatening stage.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used to improve walking distance in patients with intermittent claudication, but it is **contraindicated in patients with heart failure** and not indicated for critical limb ischemia.
- It is not effective for relieving rest pain or preventing limb loss in severe PAD and would delay necessary definitive treatment.
*Exercise therapy*
- **Supervised exercise therapy** is recommended for patients with intermittent claudication to improve walking distance and quality of life.
- However, for patients with **critical limb ischemia** and rest pain, exercise is typically too painful and not the primary intervention for limb salvage.
*Amputation*
- **Amputation** is a last resort when revascularization attempts have failed or are not feasible, and the limb is unsalvageable or poses an immediate threat to the patient's life.
- It is premature to consider amputation before assessing the possibility of revascularization, which aims to restore blood flow and save the limb.
*Systemic anticoagulation with heparin*
- **Systemic anticoagulation with heparin** is primarily used for acute limb ischemia due to emboli or acute thrombosis, to prevent further clot propagation.
- While this patient has severe PAD, which is a chronic condition, there's no indication of acute arterial occlusion necessitating systemic heparin; the immediate need is to address the chronic severe ischemia via revascularization.
Peripheral arterial disease US Medical PG Question 7: A 66-year-old woman presents to the emergency department with lower extremity pain. She reports that she has had worsening pain in her left calf over the past year while walking. The pain improves with rest, but the patient notes that she now has to stop walking more frequently than in the past to relieve the pain. The patient’s past medical history is otherwise notable for hypertension and coronary artery disease. Her home medications include hydrochlorothiazide and lisinopril. Her family history is significant for diabetes mellitus in her father. On physical exam, her left lower extremity is slightly cool to the touch with palpable distal pulses. The skin of the left lower extremity appears smooth and shiny below the mid-calf. Laboratory testing is performed and reveals the following:
Serum:
High-density lipoprotein (HDL): 60 mg/dL
Low-density lipoprotein (LDL): 96 mg/dL
Triglycerides: 140 mg/dL
This patient should be started on which of the following medication regimens?
- A. Aspirin and cilostazol
- B. Aspirin only
- C. Aspirin and atorvastatin (Correct Answer)
- D. Atorvastatin and cilostazol
- E. Atorvastatin only
Peripheral arterial disease Explanation: ***Aspirin and atorvastatin***
- The patient presents with classic symptoms and signs of **peripheral artery disease (PAD)**, including **intermittent claudication** (pain with walking, relieved by rest), **cool extremity**, and **trophic skin changes** (smooth, shiny skin).
- Both **aspirin** (for antiplatelet activity to reduce thrombotic events) and a **statin** like atorvastatin (for lipid lowering and plaque stabilization) are crucial for managing PAD and reducing cardiovascular risk due to her history of hypertension and coronary artery disease.
*Aspirin and cilostazol*
- **Aspirin** is appropriate for its antiplatelet effects, but **cilostazol** is primarily used to improve claudication symptoms and does not address the underlying lipid abnormalities or the need for cardiovascular risk reduction as comprehensively as a statin.
- While cilostazol can alleviate symptoms, it's not a first-line agent for overall cardiovascular risk reduction in PAD when dyslipidemia is also a concern.
*Aspirin only*
- **Aspirin** is essential for secondary prevention of cardiovascular events in PAD, but it does not address the patient's **lipid profile** which, while within "normal" limits by some metrics, warrants statin therapy given her high-risk cardiovascular history (hypertension, CAD, PAD).
- Optimal management of PAD involves both antiplatelet therapy and intensive lipid lowering.
*Atorvastatin and cilostazol*
- **Atorvastatin** is appropriate for lipid lowering and cardiovascular risk reduction in PAD. However, omitting **aspirin** means missing a crucial component of antiplatelet therapy for PAD, which significantly reduces the risk of serious thrombotic events.
- **Cilostazol** helps with symptoms but does not replace aspirin's role in preventing cardiovascular morbidity and mortality.
*Atorvastatin only*
- **Atorvastatin** is vital for its pleiotropic effects, including plaque stabilization and lipid lowering, in a patient with PAD and other cardiovascular risk factors.
- However, managing PAD optimally requires concurrent **antiplatelet therapy** (e.g., aspirin) to reduce the risk of thrombotic events, which is not included in this regimen.
Peripheral arterial disease US Medical PG Question 8: A 58-year-old man presents to the emergency department with severe right leg pain accompanied by tingling and weakness. His condition started suddenly 3 hours ago when he was watching a movie. His medical history is remarkable for type 2 diabetes mellitus and hypertension. He has been smoking 20–30 cigarettes per day for the past 35 years. His vital signs include a blood pressure of 149/85 mm Hg, a temperature of 36.9°C (98.4°F), and an irregular pulse of 96/min. On physical examination, his right popliteal and posterior tibial pulses are absent. His right leg is pale and cold. Which of the following is the most likely diagnosis?
- A. Buerger's disease
- B. Leriche syndrome
- C. Acute limb ischemia (Correct Answer)
- D. CREST syndrome
- E. Deep vein thrombosis
Peripheral arterial disease Explanation: ***Acute limb ischemia***
- The sudden onset of **severe leg pain**, **tingling**, **weakness**, and the **six P's** (pain, pallor, pulselessness, paresthesias, poikilothermia, and paralysis) are classic signs of acute limb ischemia.
- The patient's history of **smoking**, **hypertension**, **diabetes**, and an **irregular pulse** (suggesting atrial fibrillation) are significant risk factors for **thromboembolism**, which is a common cause of acute limb ischemia.
*Buerger's disease*
- This condition primarily affects **small and medium-sized arteries and veins** in the limbs and is strongly associated with **heavy tobacco use**.
- However, it typically presents with **distal extremity ischemia**, superficial phlebitis, and Raynaud's phenomenon, rather than the sudden, severe, large vessel occlusion described here.
*Leriche syndrome*
- This syndrome involves **atherosclerotic occlusion of the distal aorta** at or just below the renal arteries, affecting both lower limbs.
- It classically presents with a triad of **bilateral buttock/thigh claudication**, **impotence**, and **absent femoral pulses**, which does not align with the unilateral symptoms and specific pulse deficits described in the case.
*CREST syndrome*
- CREST (Calcinosis, Raynaud's phenomenon, Esophageal dysmotility, Sclerodactyly, Telangiectasias) is a subtype of **systemic sclerosis**, a **connective tissue disease**.
- Its symptoms are unrelated to the acute vascular event presented, which involves sudden limb ischemia.
*Deep vein thrombosis*
- DVT primarily involves the formation of a **blood clot in a deep vein**, leading to symptoms like **swelling**, **pain**, and **redness** in the affected limb.
- It does not typically cause the **acute pallor**, **coldness**, **pulselessness**, and severe neurologic deficits (tingling, weakness) seen with arterial occlusion.
Peripheral arterial disease US Medical PG Question 9: A 65-year-old man comes to the physician because of a 10-month history of crampy left lower extremity pain that is exacerbated by walking and relieved by rest. The pain is especially severe when he walks on an incline. He has a 20-year history of type 2 diabetes mellitus, for which he takes metformin. He has smoked 1 pack of cigarettes daily for 40 years. His blood pressure is 140/92 mm Hg. Physical examination shows dry and hairless skin over the left foot. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Osteophytic compression of the lumbar spinal canal
- B. Intimal plaque in the posterior tibial artery (Correct Answer)
- C. Systemic hyperplastic arteriolosclerosis
- D. Thrombosing vasculitis of the popliteal artery
- E. Fibrin clot in the left popliteal vein
Peripheral arterial disease Explanation: ***Intimal plaque in the posterior tibial artery***
- The patient's symptoms of **crampy left lower extremity pain** exacerbated by walking and relieved by rest (**intermittent claudication**) are classic for **peripheral arterial disease (PAD)**.
- Risk factors like **diabetes mellitus**, **smoking**, and **hypertension** strongly predispose to **atherosclerosis** and **intimal plaque formation** in peripheral arteries, such as the posterior tibial artery, leading to reduced blood flow.
*Osteophytic compression of the lumbar spinal canal*
- While this can cause leg pain (**neurogenic claudication**), the pain typically **improves with leaning forward** and can be exacerbated by standing still, not necessarily relieved by rest of the legs.
- The patient's symptoms would not typically manifest with **dry and hairless skin** over the foot, which is indicative of chronic ischemia.
*Systemic hyperplastic arteriolosclerosis*
- This condition is usually associated with **severe hypertension** and primarily affects **small arterioles**, leading to **organ damage** (e.g., kidney failure, hypertensive retinopathy).
- It would not typically cause isolated, **crampy leg pain** that is specifically exacerbated by walking and relieved by rest, which is a hallmark of large vessel occlusive disease.
*Thrombosing vasculitis of the popliteal artery*
- **Vasculitis** typically involves **inflammation of blood vessel walls** and can cause a variety of symptoms including pain, skin lesions, and systemic signs.
- While it can lead to thrombosis, it's less common than atherosclerosis in a 65-year-old with multiple risk factors, and the presentation of isolated claudication is more characteristic of atherosclerotic disease.
*Fibrin clot in the left popliteal vein*
- A fibrin clot in a vein would cause **deep vein thrombosis (DVT)**, presenting with **swelling**, **redness**, and **tenderness** in the leg, not typically claudication.
- The pain associated with DVT usually **worsens with activity** and does not improve with rest in the same way as arterial claudication.
Peripheral arterial disease US Medical PG Question 10: A 49-year-old man comes to the physician because of increasing difficulty achieving an erection for 6 months. During this period, he has had to reduce his hours as a construction worker because of pain in his lower back and thighs and a progressive lower limb weakness when walking for longer distances. His pain resolves after resting for a few minutes, but it recurs when he returns to work. He also reports that his pain is improved by standing still. He is sexually active with 4 female partners and uses condoms irregularly. His father has coronary artery disease and his mother died of a ruptured intracranial aneurysm at the age of 53 years. He has smoked one pack of cigarettes daily for 35 years. He has recently taken sildenafil, given to him by a friend, with no improvement in his symptoms. His only other medication is ibuprofen as needed for back pain. His last visit to a physician was 25 years ago. He is 172.5 cm (5 ft 8 in) tall and weighs 102 kg (225 lb); BMI is 34.2 kg/m2. His temperature is 36.9°C (98.4°F), pulse is 76/min, and blood pressure is 169/98 mm Hg. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. His hemoglobin A1c is 6.2%. Which of the following is the most likely finding on physical examination?
- A. Internuclear ophthalmoplegia
- B. Decreased bilateral femoral pulses (Correct Answer)
- C. Decreased anal tone
- D. Jugular venous distention
- E. Papular rash over the palms and soles
Peripheral arterial disease Explanation: ***Decreased bilateral femoral pulses***
- This patient's symptoms of **erectile dysfunction**, **claudication**-like leg pain (worsens with activity, improves with rest), and **lower limb weakness** are highly suggestive of **peripheral artery disease (PAD)**, specifically **aortoiliac occlusion** (Leriche syndrome). The absence of femoral pulses would be a key physical sign reflecting the reduced blood flow.
- Risk factors like **smoking**, **obesity**, **hypertension**, and **elevated HbA1c** (prediabetes) further support a vascular etiology.
*Internuclear ophthalmoplegia*
- This condition is characterized by impaired adduction of one eye during conjugate gaze with nystagmus of the abducting eye, typically caused by a lesion in the **medial longitudinal fasciculus**.
- It is often associated with **multiple sclerosis** or brainstem stroke and does not align with the patient's presenting symptoms of claudication and erectile dysfunction.
*Decreased anal tone*
- **Decreased anal tone** usually indicates a lesion affecting the **sacral spinal cord** or cauda equina, potentially leading to bowel/bladder dysfunction, saddle anesthesia, and lower limb weakness.
- While the patient has lower limb weakness and back pain, the episodic nature of the leg pain related to exertion and resolution with rest, along with erectile dysfunction, points more strongly to a vascular issue rather than a neurological one causing decreased anal tone.
*Jugular venous distention*
- **Jugular venous distention (JVD)** is a sign of **elevated central venous pressure**, primarily associated with **right-sided heart failure**, fluid overload, or other conditions impairing venous return to the heart.
- The patient's symptoms are localized to lower limb ischemia and erectile dysfunction, not systemic fluid retention or heart failure.
*Papular rash over the palms and soles*
- A **papular rash over the palms and soles** is a classic sign of **secondary syphilis**.
- While the patient reports irregular condom use and multiple partners, this rash is a dermatological finding not directly related to or explaining his primary symptoms of erectile dysfunction and exertional leg pain/weakness, which are indicative of vascular insufficiency.
More Peripheral arterial disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.