Pericardial diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pericardial diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
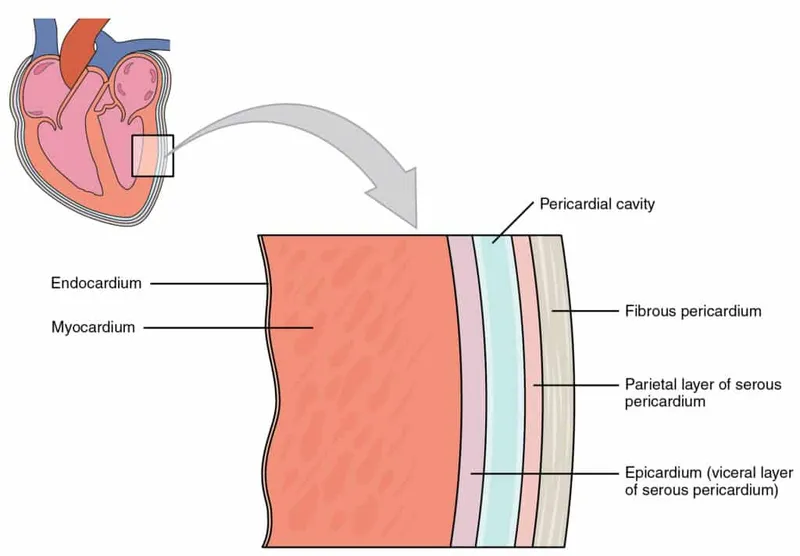
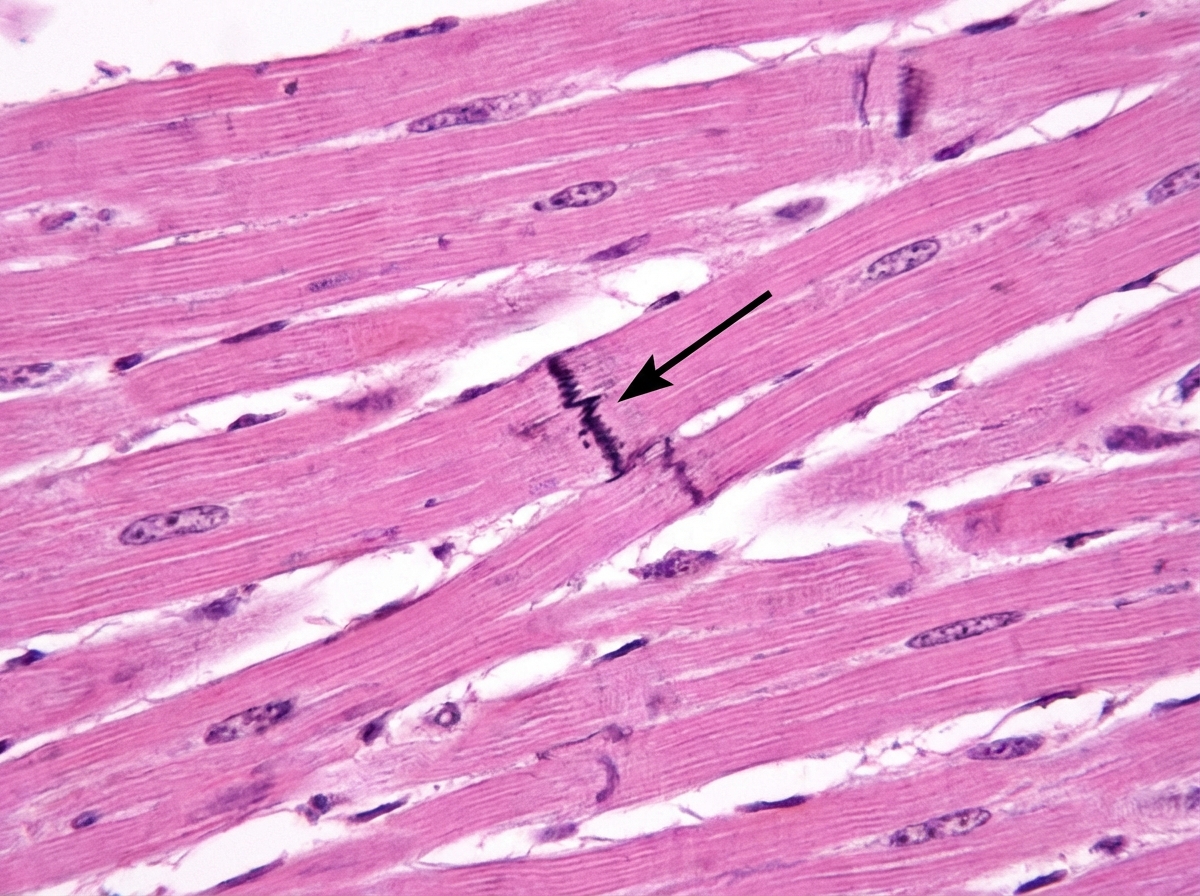
Pericardial diseases US Medical PG Question 1: Cardiac muscle serves many necessary functions, leading to a specific structure that serves these functions. The structure highlighted is an important histology component of cardiac muscle. What would be the outcome if this structure diffusely failed to function?
- A. Failure of potassium channels to appropriately open to repolarize the cell
- B. Failure of propagation of the action potential from the conduction system (Correct Answer)
- C. Ineffective excitation-contraction coupling due to insufficient calcium ions
- D. Inappropriate formation of cardiac valve leaflets
- E. Outflow tract obstruction
Pericardial diseases Explanation: ***Failure of propagation of the action potential from the conduction system***
- The highlighted structure, the **intercalated disc**, contains **gap junctions** which are crucial for the rapid, synchronized spread of **action potentials** between cardiac muscle cells.
- A diffuse failure of these structures would prevent the coordinated electrical activation of the myocardium, leading to a failure of impulse propagation and **compromised cardiac contraction**.
*Failure of potassium channels to appropriately open to repolarize the cell*
- This scenario describes a problem with **ion channel function** within individual cardiomyocytes, affecting their repolarization phase.
- While critical for a single cell's electrical activity, it does not directly relate to the primary function of **intercalated discs** in *propagating* action potentials across multiple cells.
*Ineffective excitation-contraction coupling due to insufficient calcium ions*
- This outcome would result from issues with **calcium handling** mechanisms, such as problems with the **sarcoplasmic reticulum** or **calcium channels**, which are internal to the cardiomyocyte.
- It is distinct from the role of **intercalated discs** in facilitating intercellular communication and electrical spread.
*Inappropriate formation of cardiac valve leaflets*
- The formation of cardiac valve leaflets is an intricate process during **embryological development** involving specific signaling pathways and cell migration.
- This structural defect is not directly related to the function of **intercalated discs** in mature cardiac muscle, which are involved in electrical and mechanical coupling.
*Outflow tract obstruction*
- **Outflow tract obstruction** is a congenital or acquired structural defect affecting the major arteries leaving the heart (e.g., aortic or pulmonary stenosis).
- This is a macroscopic structural anomaly that is not caused by a primary failure of **intercalated disc** function.
Pericardial diseases US Medical PG Question 2: On the 3rd day post-anteroseptal myocardial infarction (MI), a 55-year-old man who was admitted to the intensive care unit is undergoing an examination by his physician. The patient complains of new-onset precordial pain which radiates to the trapezius ridge. The nurse informs the physician that his temperature was 37.7°C (99.9°F) 2 hours ago. On physical examination, the vital signs are stable, but the physician notes the presence of a triphasic pericardial friction rub on auscultation. A bedside electrocardiogram shows persistent positive T waves in leads V1–V3 and an ST segment: T wave ratio of 0.27 in lead V6. Which of the following is the drug of choice to treat the condition the patient has developed?
- A. Clarithromycin
- B. Aspirin (Correct Answer)
- C. Furosemide
- D. Colchicine
- E. Prednisolone
Pericardial diseases Explanation: **Aspirin**
- The patient's symptoms (new-onset **precordial pain** radiating to the **trapezius ridge**, low-grade fever, and a **triphasic pericardial friction rub** after an **anteroseptal MI**) indicate **post-MI pericarditis** (early pericarditis).
- **Aspirin** is the recommended first-line treatment for post-MI pericarditis, especially in patients who have recently had an MI, due to its anti-inflammatory properties and safety profile in this context.
*Colchicine*
- While **colchicine** is effective for pericarditis, it is typically used as an adjunct to NSAIDs or aspirin, or as a monotherapy for recurrent pericarditis.
- It is not usually the primary drug of choice for acute post-MI pericarditis when aspirin can be used and the patient is stable.
*Prednisolone*
- **Glucocorticoids** like prednisolone should generally be avoided in post-MI pericarditis, as they can impair myocardial healing and potentially lead to ventricular remodeling and rupture.
- They are reserved for refractory cases or when other therapies are contraindicated, and always used with caution due to their side effect profile.
*Clarithromycin*
- **Clarithromycin** is an antibiotic and is indicated for bacterial infections.
- Pericarditis in this context is an inflammatory process, not an infection, so antibiotics would not be effective.
*Furosemide*
- **Furosemide** is a loop diuretic used to reduce fluid overload, often in conditions like heart failure or pulmonary edema.
- It has no role in treating the inflammation associated with pericarditis and would not address the patient's symptoms or underlying condition.
Pericardial diseases US Medical PG Question 3: A 16-year-old boy with a history of severe, persistent asthma presents to the emergency department with severe shortness of breath and cough. He states that he was outside playing basketball with his friends, forgot to take his inhaler, and began to have severe difficulty breathing. On exam, he is in clear respiratory distress with decreased air movement throughout all lung fields. He is immediately treated with beta-agonists which markedly improve his symptoms. Prior to treatment, which of the following was most likely observed in this patient?
- A. Kussmaul's sign
- B. Pulsus paradoxus (Correct Answer)
- C. Friction rub
- D. Inspiratory stridor
- E. Increased breath sounds
Pericardial diseases Explanation: ***Pulsus paradoxus***
* **Pulsus paradoxus** is a classic sign of **severe asthma exacerbation**, characterized by an abnormally large decrease in **systolic blood pressure** during inspiration.
* The marked improvement with **beta-agonists** confirms the likely diagnosis of acute severe asthma, making pulsus paradoxus a highly probable finding before treatment.
*Kussmaul's sign*
* **Kussmaul's sign** is a paradoxical rise in **jugular venous pressure (JVP)** during inspiration, typically seen in conditions like **constrictive pericarditis** or **right heart failure**.
* It is not associated with acute asthma exacerbations.
*Friction rub*
* A **friction rub** is a leathery or grating sound heard on auscultation, indicative of inflammation of the **pleura** (pleurisy) or **pericardium** (pericarditis).
* It is not a typical finding in asthma and would suggest an alternative or co-existing pathology.
*Inspiratory stridor*
* **Inspiratory stridor** is a harsh, high-pitched sound primarily heard during inspiration, caused by **upper airway obstruction** (e.g., croup, epiglottitis, foreign body aspiration).
* While severe shortness of breath is present, the symptom relief with beta-agonists points to **lower airway obstruction** characteristic of asthma rather than upper airway issues.
*Increased breath sounds*
* In **severe asthma exacerbations**, there is significant **bronchoconstriction** and **air trapping**, leading to markedly **decreased or absent breath sounds** on auscultation, not increased.
* Increased breath sounds might be heard in consolidation (pneumonia) or early stages of bronchiole inflammation, but not in severe asthma distress.
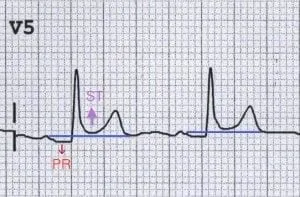
Pericardial diseases US Medical PG Question 4: A 29-year-old man presents to the emergency department with a sharp pain in the center of his chest. The pain is knife-like and constant. Sitting alleviates the pain and lying supine aggravates it. He denies the use of nicotine, alcohol or illicit drugs. Vital signs include: temperature 37.0°C (98.6°F), blood pressure 135/92 mm Hg, and pulse 97/min. On examination, a friction rub is heard at the left sternal border while the patient is leaning forward. His ECG is shown in the image. Which of the following can prevent recurrence of this patient’s condition?
- A. Ibuprofen
- B. Aspirin
- C. Colchicine (Correct Answer)
- D. Glucocorticoids
- E. Systemic antibiotics
Pericardial diseases Explanation: ***Colchicine***
- Colchicine is an **anti-inflammatory agent** that is highly effective in preventing recurrences of pericarditis, especially when used in conjunction with NSAIDs.
- It is recommended for initial treatment and for several months to reduce the risk of future episodes in cases of acute and recurrent pericarditis.
*Ibuprofen*
- Ibuprofen, a **NSAID**, is a first-line treatment for acute pericarditis to manage pain and inflammation.
- While effective for acute symptom relief, it is not primarily used for long-term prevention of recurrent pericarditis without an additional agent like colchicine.
*Aspirin*
- Aspirin, like other **NSAIDs**, is used to treat the acute inflammation and pain of pericarditis, particularly in patients with acute myocardial infarction.
- It does not offer superior anti-recurrent properties compared to other NSAIDs or colchicine for pericarditis.
*Glucocorticoids*
- Glucocorticoids are generally **reserved for refractory cases** of pericarditis or when NSAIDs and colchicine are contraindicated due to potential side effects and an increased risk of recurrence.
- Their use as a primary agent can actually **increase the risk of recurrence** once tapered, making them a less desirable option for prevention.
*Systemic antibiotics*
- Pericarditis is most commonly **viral or idiopathic**; therefore, systemic antibiotics are not indicated unless there is clear evidence of a bacterial infection.
- The presented symptoms and ECG findings are not suggestive of bacterial pericarditis, which is rare.
Pericardial diseases US Medical PG Question 5: A 41-year-old woman presents to the emergency room with chest pain. She has had progressive substernal chest pain accompanied by weakness and mild shortness of breath for the past 2 hours. Her past medical history is notable for poorly controlled systemic lupus erythematosus (SLE), Sjogren syndrome, and interstitial lung disease. She was hospitalized last year with pericarditis presumed to be from SLE. Her temperature is 98.6°F (37°C), blood pressure is 106/56 mmHg, pulse is 132/min, and respirations are 26/min. On exam, the skin overlying the internal jugular vein fills at 9 cm above the sternal angle and distant heart sounds are appreciated. There is no friction rub. She is given 1000cc of intravenous fluids with no appreciable change in her blood pressure. An electrocardiogram in this patient would most likely reveal which of the following findings?
- A. Polymorphic P waves
- B. ST elevations in leads II, III, and aVF
- C. Peaked T waves
- D. Wide QRS complexes with no P waves
- E. Electrical alternans (Correct Answer)
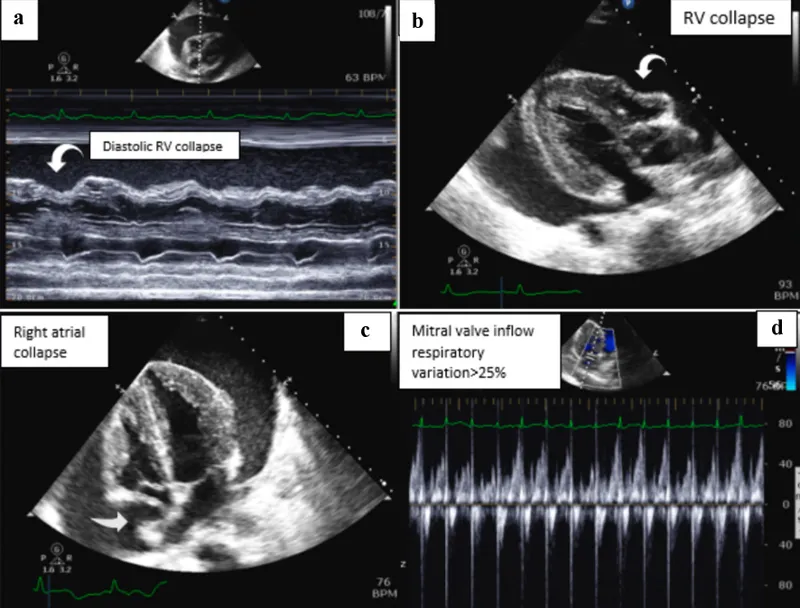
Pericardial diseases Explanation: ***Electrical alternans***
- The patient's symptoms (chest pain, shortness of breath, **hypotension**, **tachycardia**, **elevated JVP**, and **distant heart sounds**) in the context of a history of **pericarditis** and **SLE** are highly suggestive of **cardiac tamponade.**
- **Electrical alternans**, characterized by alternating QRS complex heights due to the swinging motion of the heart in a large pericardial effusion, is a classic EKG finding for cardiac tamponade.
- This finding reflects the mechanical swinging of the heart within the pericardial fluid, causing beat-to-beat variation in QRS amplitude.
*Polymorphic P waves*
- **Polymorphic P waves** (multifocal atrial tachycardia) occur when there are at least three different P wave morphologies on the EKG, indicating multiple ectopic atrial foci.
- This is typically seen in patients with severe lung disease or other conditions causing increased atrial stretch, but it is not a direct consequence or typical finding of cardiac tamponade.
*ST elevations in leads II, III, and aVF*
- **ST elevations in leads II, III, and aVF** indicate an **inferior myocardial infarction**, which is caused by coronary artery occlusion.
- While chest pain is present, the patient's other signs (elevated JVP, distant heart sounds, hypotension not responding to fluids, history of pericarditis/SLE) point away from an acute MI and strongly towards cardiac tamponade.
*Peaked T waves*
- **Peaked T waves** are characteristic of **hyperkalemia**, a condition of excessively high potassium levels in the blood.
- While hyperkalemia can cause cardiac symptoms, it does not typically present with the specific hemodynamic compromise and physical exam findings (elevated JVP, distant heart sounds) described, which are classic for cardiac tamponade.
*Wide QRS complexes with no P waves*
- **Wide QRS complexes with no P waves** are characteristic of a **ventricular arrhythmia**, such as ventricular tachycardia or idioventricular rhythm.
- While the patient is hypotensive and tachycardic, the presenting symptoms and physical exam findings are not directly indicative of a primary ventricular arrhythmia, but rather suggest an extracardiac compression of the heart due to tamponade.
Pericardial diseases US Medical PG Question 6: An 80-year-old man presents to the emergency department because of gnawing substernal chest pain that started an hour ago and radiates to his neck and left jaw. A 12-lead ECG is obtained and shows ST-segment elevation with newly developing Q waves. He is admitted for treatment. 4 days after hospitalization he suddenly develops altered mental status, and his blood pressure falls from 115/75 mm Hg to 80/40 mm Hg. Physical examination shows jugular venous distention, pulsus paradoxus, and distant heart sounds. What is the most likely cause of this patient's condition?
- A. Pericardial inflammation
- B. Compression of heart chambers by blood in the pericardial space (Correct Answer)
- C. Arrhythmia caused by ventricular fibrillation
- D. Rupture of papillary muscle
- E. Acute pulmonary edema from left heart failure
Pericardial diseases Explanation: ***Compression of heart chambers by blood in the pericardial space***
- The patient's initial presentation with ST-elevation myocardial infarction (STEMI) and subsequent development of **hypotension**, **jugular venous distention**, **pulsus paradoxus**, and **distant heart sounds** (Beck's triad) is highly indicative of **cardiac tamponade.**
- In the context of a recent MI, this constellation of symptoms strongly suggests a **cardiac free wall rupture**, leading to blood accumulation in the pericardial sac and compression of the heart.
- Free wall rupture typically occurs **3-7 days post-MI** and is a life-threatening mechanical complication.
*Pericardial inflammation*
- While pericardial inflammation (pericarditis) can occur post-MI, it typically manifests with **pleuritic chest pain** that is relieved by leaning forward and is often associated with a **pericardial friction rub.**
- It does not typically lead to acute, severe hypotension, pulsus paradoxus, or sudden circulatory collapse in this manner without significant effusion and tamponade physiology.
*Arrhythmia caused by ventricular fibrillation*
- **Ventricular fibrillation** would cause immediate cardiac arrest and loss of consciousness, not a gradual development of hypotension, JVD, and pulsus paradoxus.
- While arrhythmias are common post-MI, the specific physical findings point away from isolated VFib as the primary cause of hemodynamic collapse.
*Acute pulmonary edema from left heart failure*
- **Acute pulmonary edema** is a manifestation of **left heart failure**, characterized by severe dyspnea, orthopnea, and crackles on lung auscultation.
- While left heart failure can cause hypotension in cardiogenic shock, it would not typically present with the classic signs of cardiac tamponade such as pulsus paradoxus, distant heart sounds, and prominent JVD without pulmonary congestion findings.
*Rupture of papillary muscle*
- **Papillary muscle rupture** leads to severe **acute mitral regurgitation**, causing acute pulmonary edema, a new holosystolic murmur, and often cardiogenic shock.
- While it can lead to hypotension, it doesn't typically present with the classic signs of cardiac tamponade such as pulsus paradoxus and distant heart sounds; instead, a loud murmur would be prominent.
Pericardial diseases US Medical PG Question 7: A 54-year-old woman presents to the emergency ward with a chief complaint of chest pain. The pain is sharp and present in the anterior part of the chest. There is no radiation of the pain; however, the intensity is decreased while sitting and leaning forward. There is no associated shortness of breath. Vital signs are the following: blood pressure is 132/84 mm Hg; pulse rate is 82/min, rhythmic, and regular. Lungs are clear on auscultation and cardiovascular examination demonstrates scratchy and squeaking sounds at the left sternal border. Kussmaul sign is positive and ECG shows new widespread ST segment elevation and PR depression. The most likely cause for these findings in this patient is?
- A. Restrictive cardiomyopathy
- B. Acute pericarditis (Correct Answer)
- C. Pleurisy
- D. Right ventricular myocardial infarction
- E. Cardiac tamponade
Pericardial diseases Explanation: ***Acute pericarditis***
- The classic presentation includes **sharp, pleuritic chest pain** that **improves with leaning forward** and **worsens with lying down**. The presence of a **pericardial friction rub** (scratchy and squeaking sounds) and specific ECG findings like **widespread ST elevation** and **PR depression** are highly indicative.
- **Kussmaul sign** (paradoxical rise in jugular venous pressure on inspiration) is unusual in uncomplicated acute pericarditis but may suggest associated pericardial effusion or early constrictive physiology. The clinical picture remains most consistent with acute pericarditis given the characteristic chest pain, friction rub, and ECG changes.
*Restrictive cardiomyopathy*
- Characterized by **diastolic dysfunction** and impaired ventricular filling, leading to symptoms like dyspnea and edema. While Kussmaul sign can be present, the chest pain characteristics, friction rub, and widespread ST elevation with PR depression are not typical.
- The ECG findings in restrictive cardiomyopathy usually involve **low voltage** and non-specific ST-T wave changes, not diffuse ST elevation and PR depression.
*Pleurisy*
- Pleurisy causes **sharp, pleuritic chest pain** that can worsen with breathing and movement, similar to pericarditis. However, it does not typically present with a pericardial friction rub or the characteristic ECG changes of widespread ST elevation and PR depression.
- Pleurisy is an inflammation of the pleura, often indicated by **pleural friction rubs** and usually associated with pulmonary conditions, which are not suggested by this patient's findings.
*Right ventricular myocardial infarction*
- While it can cause chest pain and positive Kussmaul sign due to elevated right atrial pressure, the chest pain is typically more anginal-like and not relieved by leaning forward.
- The ECG would show **ST elevation primarily in right-sided leads (V4R)** and inferior leads (II, III, aVF), but would **not typically show widespread ST elevation or PR depression** in multiple lead distributions or a pericardial friction rub.
*Cardiac tamponade*
- Characterized by the **Beck's triad** (hypotension, muffled heart sounds, and elevated jugular venous pressure) and pulsus paradoxus. Chest pain can be present, but the pain's amelioration with leaning forward and the specific ECG changes with widespread ST elevation and PR depression are not typical.
- While a pericardial friction rub might precede tamponade, **cardiac tamponade itself typically develops from a significant pericardial effusion**, leading to compression of the heart and does not directly manifest with diffuse ST elevation and PR depression.
Pericardial diseases US Medical PG Question 8: A 74-year-old man comes to the physician for a 6-month history of progressively worsening fatigue and shortness of breath on exertion. He immigrated to the United States 35 years ago from India. His pulse is 89/min and blood pressure is 145/60 mm Hg. Crackles are heard at the lung bases. Cardiac examination shows a grade 3/6 early diastolic murmur loudest at the third left intercostal space. Further evaluation of this patient is most likely to show which of the following?
- A. Paradoxical splitting of S2
- B. Pulsus paradoxus
- C. Pulsus parvus et tardus
- D. Fixed splitting of S2
- E. Water hammer pulse (Correct Answer)
Pericardial diseases Explanation: ***Water hammer pulse***
- The patient's presentation with **fatigue**, **dyspnea**, **crackles**, and a **grade 3/6 early diastolic murmur** loudest at the **third left intercostal space** is highly suggestive of **aortic regurgitation (AR)**.
- A **water hammer pulse** (also known as a **Corrigan's pulse**) is a **bounding**, **collapsing pulse** characteristic of severe AR due to the rapid runoff of blood from the aorta into the left ventricle during diastole, causing a widened pulse pressure (145/60 mmHg in this case).
*Paradoxical splitting of S2*
- **Paradoxical splitting of S2** occurs when the aortic valve closes *after* the pulmonic valve, typically due to **left bundle branch block** or **severe aortic stenosis**, which are not indicated here.
- In such cases, the split narrows or disappears during inspiration.
*Pulsus paradoxus*
- **Pulsus paradoxus** is an exaggerated drop in systolic blood pressure (>10 mmHg) during inspiration, commonly seen in **cardiac tamponade**, **severe asthma**, or **constrictive pericarditis**.
- There are no features in the patient's history or examination to suggest these conditions.
*Pulsus parvus et tardus*
- **Pulsus parvus et tardus** (small and delayed pulse) is characteristic of **severe aortic stenosis**, where the pulse is weak and slow to rise due to obstruction of left ventricular outflow.
- The murmur described, an **early diastolic murmur**, is indicative of **aortic regurgitation**, not stenosis.
*Fixed splitting of S2*
- **Fixed splitting of S2** is typically associated with an **atrial septal defect (ASD)**, where the split between the aortic and pulmonic components of S2 remains constant during respiration.
- There is no clinical evidence to suggest an ASD in this patient.
Pericardial diseases US Medical PG Question 9: A 72-year-old man presents to the emergency department because of difficulty breathing and sharp chest pain. The chest pain increases in intensity with lying down, and it radiates to the scapular ridge. Approximately 3 weeks ago, he had an anterior ST-elevation myocardial infarction, which was treated with intravenous alteplase. He was discharged home in a stable condition. Current vital signs include a temperature of 38.1 (100.5°F), blood pressure of 131/91 mm Hg, and pulse of 99/min. On examination, heart sounds are distant and a scratching sound is heard on the left sternal border. ECG reveals widespread concave ST elevations in the precordial leads and PR depressions in leads V2-V6. Which of the following is the most likely cause of this patient condition?
- A. Recurrent infarction
- B. Myocarditis
- C. Aortic dissection
- D. Dressler’s syndrome (Correct Answer)
- E. Ventricular aneurysm
Pericardial diseases Explanation: ***Dressler’s syndrome***
- This syndrome, also known as **post-myocardial infarction syndrome**, typically presents weeks to months after an MI and is characterized by pleuritic chest pain, fever, and pericardial friction rub.
- The **widespread ST elevations (concave)** and **PR depressions** on ECG are classic findings of pericarditis, which is the underlying pathology of Dressler's syndrome.
*Recurrent infarction*
- While an MI can cause chest pain, the pain associated with infarction is typically **retrosternal, crushing**, and does not improve with leaning forward or worsen with lying down.
- ECG findings of recurrent MI would show **convex ST elevations** in a specific coronary artery territory, not widespread concave ST elevation.
*Myocarditis*
- Myocarditis can cause chest pain, fever, and ECG changes (including ST elevations), but it is primarily an **inflammation of the heart muscle** often due to viral infection.
- In this case, the **pericardial friction rub** and history of recent MI strongly point towards pericardial inflammation, not primarily myocardial inflammation.
*Aortic dissection*
- Aortic dissection presents with **severe, tearing chest pain** that often radiates to the back, but it typically has an abrupt onset and is not associated with a pericardial friction rub or widespread ST elevations.
- The ECG findings of pericarditis do not support acute aortic dissection.
*Ventricular aneurysm*
- A ventricular aneurysm is a late complication of MI and can lead to symptoms like heart failure or arrhythmias, but it does **not typically cause acute pericarditic chest pain** or associated ECG findings.
- While it can cause persistent ST elevation, it would not be widespread and concave, and it wouldn't be associated with a friction rub.
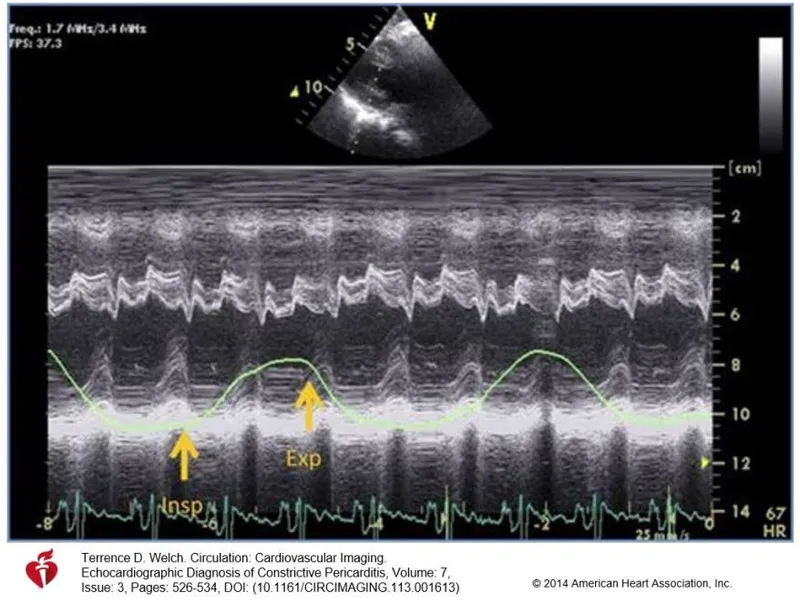
Pericardial diseases US Medical PG Question 10: A 77-year-old woman presents to her physician because of fatigue and progressive dyspnea despite receiving optimal treatment for heart failure. Her medical history is positive for heart failure, active tuberculosis, and chronic renal failure, for which she has been in long-term hemodialysis (13 years). The woman currently takes rifampin and isoniazid. Her physical exam shows the presence of hepatomegaly and jugular venous distention that fails to subside on inspiration (Kussmaul's sign) and an impalpable apical impulse. Her pulse is 122/min, respiratory rate 16/min, temperature 36.0°C (97.4°F), and blood pressure 120/60 mm Hg. Her cardiac monitor shows a prominent y descent in her jugular venous pulse. A cardiac ultrasound shows pericardial calcifications and small tubular-shaped ventricles. Which of the following is the most likely cause of this patient's current condition?
- A. Constrictive pericarditis (Correct Answer)
- B. Dilated cardiomyopathy
- C. Atrial fibrillation
- D. Restrictive cardiomyopathy
- E. Hypertrophic cardiomyopathy
Pericardial diseases Explanation: ***Constrictive pericarditis***
- The patient presents with **fatigue, dyspnea, hepatomegaly, jugular venous distention with Kussmaul's sign**, and an **impalpable apical impulse**, all classic signs of **right-sided heart failure** due to impaired ventricular filling.
- The history of **tuberculosis** and **chronic renal failure** (risk factors for pericardial disease), along with **pericardial calcifications** and **small, tubular-shaped ventricles** on ultrasound, strongly points to constrictive pericarditis.
*Dilated cardiomyopathy*
- This condition is characterized by **ventricular dilation** and **systolic dysfunction**, leading to signs of both left and right heart failure.
- The ultrasound finding of **small, tubular-shaped ventricles** contradicts the definition of dilated cardiomyopathy.
*Atrial fibrillation*
- While atrial fibrillation can cause **palpitations, fatigue, and dyspnea**, it is an arrhythmia primarily affecting cardiac rhythm.
- It does not directly explain the **pericardial calcifications, Kussmaul's sign**, or the specific ventricular morphology seen on ultrasound.
*Restrictive cardiomyopathy*
- This condition involves increased **ventricular stiffness**, leading to impaired diastolic filling and typically presents with signs of **diastolic heart failure**.
- Although it can cause similar symptoms to constrictive pericarditis, it is primarily a **myocardial** disease and would not typically show **pericardial calcifications** on imaging.
*Hypertrophic cardiomyopathy*
- This involves **thickening of the ventricular walls**, often leading to **outflow tract obstruction** and **diastolic dysfunction**.
- The imaging showing **small, tubular-shaped ventricles** and **pericardial calcifications** are inconsistent with hypertrophic cardiomyopathy, which would show thickened myocardium.
More Pericardial diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.