Hypertension diagnosis and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypertension diagnosis and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypertension diagnosis and management US Medical PG Question 1: A previously healthy 61-year-old man comes to the physician because of a 6-month history of morning headaches. He also has fatigue and trouble concentrating on his daily tasks at work. He sleeps for 8 hours every night; his wife reports that he sometimes stops breathing for a few seconds while sleeping. His pulse is 71/min and blood pressure is 158/96 mm Hg. He is 178 cm (5 ft 10 in) tall and weighs 100 kg (220 lb); BMI is 31.6 kg/m2 . Which of the following is the most likely cause of this patient's hypertension?
- A. Proliferation of adrenal chromaffin cells
- B. Overproduction of cortisol
- C. Hypophyseal neoplasm
- D. Nocturnal upper airway obstruction (Correct Answer)
- E. Hypersecretion of aldosterone
Hypertension diagnosis and management Explanation: ***Nocturnal upper airway obstruction***
- The patient's **obesity (BMI 31.6)**, **morning headaches**, fatigue, difficulty concentrating, and spousal report of **witnessed apneic episodes during sleep** are classic signs of **obstructive sleep apnea (OSA)**.
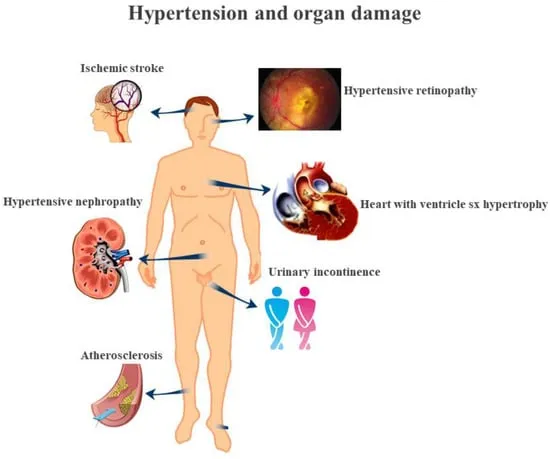
- OSA causes **intermittent hypoxia and hypercapnia** during sleep, leading to **sympathetic nervous system activation**, increased catecholamine release, and **sustained hypertension** even during waking hours.
- OSA is one of the most common **secondary causes of hypertension**, especially in obese patients.
*Proliferation of adrenal chromaffin cells*
- This describes a **pheochromocytoma**, which typically presents with **paroxysmal hypertension**, severe episodic headaches, palpitations, and diaphoresis (the classic "triad").
- While headaches are present, the **sleep-related breathing disturbances** and obesity are not consistent with pheochromocytoma.
*Overproduction of cortisol*
- This suggests **Cushing's syndrome**, which includes symptoms like central obesity, **moon facies, buffalo hump, purple striae**, muscle weakness, and easy bruising, along with hypertension.
- The patient lacks the classic cushingoid features, and the symptoms are more consistent with sleep-disordered breathing.
*Hypophyseal neoplasm*
- A pituitary tumor could cause hypertension if it leads to conditions like **Cushing's disease** (ACTH-secreting) or **acromegaly** (growth hormone excess).
- However, there are no specific symptoms pointing towards a pituitary tumor (no visual field defects, acromegalic features, or cushingoid appearance), and the prominent **witnessed apneas** fit OSA much better.
*Hypersecretion of aldosterone*
- This is characteristic of **primary hyperaldosteronism (Conn's syndrome)**, which commonly presents with hypertension, often accompanied by **hypokalemia**, muscle weakness, and polyuria.
- The patient's symptoms do not suggest electrolyte abnormalities or other classic signs of mineralocorticoid excess.
Hypertension diagnosis and management US Medical PG Question 2: A 54-year-old African American man presents to the clinic for his first annual well-check. He was unemployed for years but recently received health insurance from a new job. He reports feeling healthy and has no complaints. His blood pressure is 157/90 mmHg, pulse is 86/min, and respirations are 12/min. Routine urinalysis demonstrated a mild increase in albumin and creatinine. What medication is indicated at this time?
- A. Hydrochlorothiazide
- B. Metoprolol
- C. Furosemide
- D. Lisinopril (Correct Answer)
- E. Amlodipine
Hypertension diagnosis and management Explanation: ***Lisinopril***
- This patient presents with **hypertension (157/90 mmHg)** and **mild albuminuria with elevated creatinine**, indicating early chronic kidney disease (CKD). An **ACE inhibitor (e.g., lisinopril)** is the first-line treatment for hypertension in **any patient with CKD or proteinuria**, regardless of race or ethnicity.
- ACE inhibitors are **renoprotective** by reducing intraglomerular pressure and slowing progression of kidney disease. The presence of albuminuria represents a **compelling indication** that overrides other considerations for initial antihypertensive selection.
- Note: While ACE inhibitors are typically **less effective** as monotherapy in African Americans without compelling indications, the presence of CKD/proteinuria makes them the preferred agent.
*Hydrochlorothiazide*
- While a **thiazide diuretic** like hydrochlorothiazide would be an appropriate first-line agent for this African American patient with uncomplicated hypertension, it is **less effective** than an ACE inhibitor in patients with **proteinuria or kidney disease**.
- It does not offer the same degree of **renoprotection** as an ACE inhibitor in this clinical scenario with documented albuminuria.
*Metoprolol*
- **Beta-blockers** like metoprolol are effective antihypertensives but are generally **not considered first-line** for uncomplicated hypertension unless there are compelling indications like heart failure, angina, or history of myocardial infarction.
- They also do not provide the specific **renoprotective benefits** seen with ACE inhibitors in patients with albuminuria.
*Furosemide*
- **Loop diuretics** such as furosemide are potent diuretics primarily used for managing **symptoms of fluid overload** (e.g., heart failure, severe edema) and are not typically the first choice for chronic hypertension without such indications.
- For patients with **mild kidney impairment and hypertension without volume overload**, an ACE inhibitor is preferred for its renoprotective effects.
*Amlodipine*
- **Calcium channel blockers** like amlodipine are effective antihypertensives and would typically be an excellent first-line choice for an African American patient with hypertension.
- However, for this patient with **documented albuminuria**, an ACE inhibitor is preferred due to its **specific renoprotective effects** and proven benefit in slowing CKD progression, which amlodipine does not provide.
Hypertension diagnosis and management US Medical PG Question 3: A 67-year-old man with a history of diabetes mellitus type II and a previous myocardial infarction presents to your office for a routine examination. His blood pressure is found to be 180/100 mmHg. Which drug is the first-line choice of treatment for this patient's hypertension?
- A. Hydrochlorothiazide
- B. Prazosin
- C. Lisinopril (Correct Answer)
- D. Isoproterenol
- E. Amlodipine
Hypertension diagnosis and management Explanation: ***Lisinopril***
- **ACE inhibitors** (like lisinopril) are first-line for patients with hypertension and **diabetes mellitus** due to their **renal protective effects** and ability to slow the progression of diabetic nephropathy.
- They are also beneficial post-myocardial infarction as they **reduce ventricular remodeling** and improve long-term outcomes.
*Hydrochlorothiazide*
- While **thiazide diuretics** can be used for hypertension, they may **worsen glucose control** in diabetic patients and are not preferred as first-line in the presence of diabetes and a history of MI.
- They primarily act by reducing blood volume and peripheral resistance but lack the specific **cardio-renal protective benefits** of ACE inhibitors.
*Prazosin*
- **Alpha-1 blockers** like prazosin are generally not recommended as first-line monotherapy for hypertension due to potential side effects such as **orthostatic hypotension** and a higher risk of cardiovascular events compared to other classes.
- Their use is typically reserved for patients with concomitant **benign prostatic hyperplasia (BPH)** or as add-on therapy.
*Isoproterenol*
- **Isoproterenol** is a non-selective beta-agonist primarily used for **bradycardia** or **heart block**, not for the treatment of hypertension.
- It would actually **increase heart rate and contractility**, exacerbating hypertension rather than treating it.
*Amlodipine*
- **Calcium channel blockers** like amlodipine are effective antihypertensives and can be used in patients with diabetes, but **ACE inhibitors** are generally preferred as first-line in patients with both diabetes and a history of MI due to their direct **renoprotective** and **cardioprotective** benefits.
- While effective for blood pressure control, amlodipine does not offer the same degree of **renal benefit** in diabetic nephropathy or post-MI remodeling as ACE inhibitors.
Hypertension diagnosis and management US Medical PG Question 4: A 32-year-old woman comes to the physician because of a 2-month history of fatigue, muscle weakness, paresthesias, headache, and palpitations. Her pulse is 75/min and blood pressure is 152/94 mm Hg. Physical examination shows no abnormalities. Serum studies show:
Sodium 144 mEq/L
Potassium 2.9 mEq/L
Bicarbonate 31 mEq/L
Creatinine 0.7 mg/dL
Further evaluation shows low serum renin activity. Which of the following is the most likely diagnosis?
- A. Aldosteronoma (Correct Answer)
- B. Cushing syndrome
- C. Renal artery stenosis
- D. Pheochromocytoma
- E. Laxative abuse
Hypertension diagnosis and management Explanation: ***Aldosteronoma***
- The patient presents with **hypertension**, **hypokalemia**, and **metabolic alkalosis** (elevated bicarbonate), which are classic signs of primary hyperaldosteronism.
- **Low serum renin activity** in conjunction with these findings points directly to an **aldosterone-producing adenoma (aldosteronoma)** as the most likely cause.
*Cushing syndrome*
- While Cushing syndrome can cause **hypertension** and **hypokalemia**, it is primarily characterized by features of **hypercortisolism** such as central obesity, moon facies, striae, and muscle wasting, which are not described here.
- The primary defect in Cushing syndrome relates to cortisol excess, not primary aldosterone overproduction leading to low renin.
*Renal artery stenosis*
- **Renal artery stenosis** causes **secondary hyperaldosteronism**, typically presenting with **hypertension** and **elevated renin activity** due to decreased renal perfusion.
- This contradicts the patient's low serum renin activity, making it an unlikely diagnosis.
*Pheochromocytoma*
- **Pheochromocytoma** presents with paroxysmal or sustained **hypertension**, **palpitations**, **headaches**, and **sweating** due to catecholamine excess.
- It does not typically cause **hypokalemia** or **metabolic alkalosis** as seen in this patient.
*Laxative abuse*
- **Laxative abuse** can cause hypokalemia and metabolic alkalosis, but it is typically associated with **chronic diarrhea** and volume depletion, which are not mentioned.
- It does not directly cause **hypertension** and is not associated with low renin activity in the context of aldosterone excess.
Hypertension diagnosis and management US Medical PG Question 5: A 55-year-old man presents to his primary care physician for a wellness checkup. He states that he generally feels well and has no complaints at this time. The patient consumes alcohol frequently, eats a high sodium diet, and is sedentary. His temperature is 97.5°F (36.4°C), blood pressure is 167/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. The patient is 5'10" tall and weighs 220 lbs (BMI 31.5 kg/m²). The patient's blood pressure at his last 2 appointments were 159/100 mmHg and 162/99 mmHg, respectively. His physician wants to intervene to manage his blood pressure. Which of the following is the most effective lifestyle intervention for this patient's hypertension?
- A. Exercise
- B. DASH diet (Correct Answer)
- C. Reduce alcohol consumption
- D. Sodium restriction
- E. Weight loss
Hypertension diagnosis and management Explanation: ***DASH diet***
- The **DASH (Dietary Approaches to Stop Hypertension) diet** is a comprehensive dietary plan rich in fruits, vegetables, and low-fat dairy, and reduced in saturated and total fats. It is the most effective single lifestyle intervention for reducing **blood pressure (BP)**.
- This patient has **stage 2 hypertension** and multiple risk factors including obesity, frequent alcohol consumption, and a high-sodium diet, making a holistic dietary approach crucial for significant BP reduction.
*Exercise*
- While **regular exercise** is beneficial for overall cardiovascular health and can help manage hypertension, it is generally less effective than the DASH diet for initial, significant **blood pressure reduction** in a patient with stage 2 hypertension.
- The patient's **sedentary lifestyle** contributes to his hypertension, but exercise alone may not achieve the desired BP control as effectively as a comprehensive dietary change.
*Reduce alcohol consumption*
- **Excessive alcohol intake** is a risk factor for hypertension, and reducing consumption can lower blood pressure. However, its effect is typically less pronounced compared to the **DASH diet** in achieving major BP reductions.
- The patient's "frequent" alcohol consumption suggests this is an important area for intervention, but it's part of a broader lifestyle modification rather than the single most effective treatment.
*Sodium restriction*
- A **high sodium diet** is a significant contributor to hypertension, and **sodium restriction** is a key component of managing blood pressure. However, the DASH diet inherently incorporates sodium restriction along with other beneficial dietary changes.
- While important, focusing solely on sodium restriction often yields less comprehensive and sustained BP reduction compared to the **multi-faceted approach** of the DASH diet.
*Weight loss*
- Given the patient's **obesity (BMI 31.5 kg/m²)**, **weight loss** is a critical intervention for blood pressure control and overall health.
- However, achieving significant weight loss often requires a combination of dietary changes and increased physical activity, making the **DASH diet** a more direct and often more achievable initial step for BP reduction.
Hypertension diagnosis and management US Medical PG Question 6: A 51-year-old man presents to the urgent care center with a blood pressure of 201/111 mm Hg. He is complaining of a severe headache and chest pain. Physical examination reveals regular heart sounds and clear bilateral lung sounds. Ischemic changes are noted on his electrocardiogram (ECG). What is the most appropriate treatment for this patient’s high blood pressure?
- A. IV labetalol - lower mean arterial pressure no more than 25% over the 1st hour (Correct Answer)
- B. Oral clonidine - gradually lower blood pressure over 24–48 hours
- C. Oral beta-blocker - lower mean arterial pressure no more than 25% over the 1st hour
- D. IV labetalol - lower mean arterial pressure no more than 50% over the 1st hour
- E. IV labetalol - redose until blood pressure within normal limits
Hypertension diagnosis and management Explanation: ***IV labetalol - lower mean arterial pressure no more than 25% over the 1st hour***
- This patient presents with **hypertensive emergency**, indicated by severe hypertension (BP 201/111 mmHg) and evidence of **acute target organ damage** (severe headache, chest pain, ischemic ECG changes).
- **IV labetalol** is an appropriate first-line agent, and the goal is to **gradually reduce** the mean arterial pressure by no more than **25% within the first hour** to prevent hypoperfusion and ischemic events.
*Oral clonidine - gradually lower blood pressure over 24–48 hours*
- **Oral clonidine** has a slower onset of action and is not suitable for the **urgent reduction** required in a hypertensive emergency.
- This approach is more appropriate for **gradual blood pressure reduction** in less severe hypertension or as an adjunct in chronic management.
*Oral beta-blocker - lower mean arterial pressure no more than 25% over the 1st hour*
- **Oral medications** are generally not preferred for initial management of **hypertensive emergencies** due to their slower onset and less predictable dose titration compared to intravenous agents.
- While beta-blockers can be effective, the **oral route** is inappropriate for the acute, rapid control needed for this condition.
*IV labetalol - lower mean arterial pressure no more than 50% over the 1st hour*
- A rapid reduction of **50% in MAP** within the first hour is too aggressive and carries a significant risk of **hypoperfusion** to vital organs, potentially leading to **stroke**, **myocardial infarction**, or **renal failure**.
- The recommended initial reduction is **no more than 25%** in the first hour to maintain adequate organ perfusion.
*IV labetalol - redose until blood pressure within normal limits*
- Aggressively lowering blood pressure to **"normal limits"** too quickly can cause cerebral, cardiac, or renal **ischemia** due to loss of autoregulation in previously hypertensive patients.
- The goal is to first stabilize the patient by reducing the BP by a controlled amount, not to normalize it immediately.
Hypertension diagnosis and management US Medical PG Question 7: A 56-year-old Caucasian male presents to the clinic to establish care. He has never seen a physician and denies any known medical problems. Physical examination is notable for central obesity, but the patient has regular heart and lung sounds. He has a blood pressure of 157/95 mm Hg and heart rate of 92/min. He follows up 2 weeks later, and his blood pressure continues to be elevated. At this time, you diagnose him with essential hypertension and decide to initiate antihypertensive therapy. Per the Joint National Committee 8 guidelines for treatment of high blood pressure, of the following combinations of drugs, which can be considered for first-line treatment of high blood pressure in the Caucasian population?
- A. ACE inhibitor, ARB, CCB, or thiazide (Correct Answer)
- B. ACE inhibitor, angiotensin receptor blocker (ARB), beta-blocker (BB), or thiazide
- C. ACE inhibitor, ARB, CCB, or loop diuretic
- D. ACE inhibitor, ARB, alpha-blocker, or loop diuretic
- E. ACE inhibitor, ARB, alpha-blocker, or direct vasodilator
Hypertension diagnosis and management Explanation: **ACE inhibitor, ARB, CCB, or thiazide**
- The **JNC 8 guidelines** recommend **ACE inhibitors**, **ARBs**, **calcium channel blockers (CCBs)**, and **thiazide diuretics** as first-line agents for essential hypertension in the general non-Black population.
- These drug classes have demonstrated efficacy in reducing cardiovascular events and are generally well-tolerated.
*ACE inhibitor, angiotensin receptor blocker (ARB), beta-blocker (BB), or thiazide*
- While **ACE inhibitors**, **ARBs**, and **thiazides** are first-line, **beta-blockers** are generally not considered first-line for uncomplicated hypertension unless there are specific compelling indications (e.g., post-MI, heart failure).
- **Beta-blockers** are less effective than other first-line agents in preventing stroke in the elderly and may have more side effects in some populations.
*ACE inhibitor, ARB, CCB or loop diuretic*
- **ACE inhibitors**, **ARBs**, and **CCBs** are first-line options, but **loop diuretics** are typically reserved for patients with fluid overload or chronic kidney disease, not for initial management of essential hypertension.
- **Loop diuretics** have a shorter duration of action and a greater electrolyte-wasting effect compared to thiazide diuretics, making them less suitable for long-term monotherapy.
*ACE inhibitor, ARB, alpha-blocker, or loop diuretic*
- **Alpha-blockers** and **loop diuretics** are not considered first-line agents for essential hypertension. **Alpha-blockers** are typically used for benign prostatic hyperplasia or as add-on therapy for resistant hypertension.
- **Alpha-blockers** can cause significant orthostatic hypotension, particularly with the first dose, and have not shown the same cardiovascular protective benefits as true first-line agents.
*ACE inhibitor, ARB, alpha-blocker, or direct vasodilator*
- **Alpha-blockers** and **direct vasodilators** (e.g., hydralazine, minoxidil) are not first-line treatments for essential hypertension.
- **Direct vasodilators** are potent but often cause reflex tachycardia and fluid retention, requiring co-administration with other agents, and are typically reserved for severe or resistant hypertension.
Hypertension diagnosis and management US Medical PG Question 8: A 44-year-old man comes to the emergency department because of a severe headache and blurry vision for the past 3 hours. He has hypertension treated with hydrochlorothiazide. He has missed taking his medication for the past week as he was traveling. He is only oriented to time and person. His temperature is 37.1°C (98.8°F), pulse is 92/min and regular, and blood pressure is 245/115 mm Hg. Cardiopulmonary examination shows no abnormalities. Fundoscopy shows bilateral retinal hemorrhages and exudates. Neurologic examination shows no focal findings. A complete blood count and serum concentrations of electrolytes, glucose, and creatinine are within the reference range. A CT scan of the brain shows no abnormalities. Which of the following is the most appropriate pharmacotherapy?
- A. Sublingual nifedipine
- B. Oral captopril
- C. Intravenous nitroprusside (Correct Answer)
- D. Oral clonidine
- E. Intravenous mannitol
Hypertension diagnosis and management Explanation: ***Intravenous nitroprusside***
- The patient presents with **hypertensive emergency**, characterized by **severe hypertension** (245/115 mmHg) with **acute end-organ damage**, including altered mental status and retinal hemorrhages/exudates.
- **Intravenous nitroprusside** is a potent, rapidly acting vasodilator making it an excellent choice for immediate and controlled reduction of blood pressure in such critical situations.
*Sublingual nifedipine*
- **Sublingual nifedipine** can cause a sudden and uncontrolled drop in blood pressure, leading to **ischemia** due to inadequate perfusion of vital organs.
- It also has a less predictable and slower onset of action compared to intravenous agents, making it unsuitable for acute hypertensive emergencies.
*Oral captopril*
- **Oral captopril** has a slower onset of action and is less suitable for the acute management of a **hypertensive emergency** where immediate and precise blood pressure control is crucial.
- While an ACE inhibitor, its oral administration does not provide the rapid titratability needed to safely lower dangerously high blood pressures.
*Oral clonidine*
- **Oral clonidine** also has a relatively slow onset of action and its effects can be variable, making it less ideal for the acute, emergent management of **severe hypertension** with end-organ damage.
- It is more appropriate for urgent but non-emergent hypertension or chronic management, not for situations requiring immediate and controlled blood pressure reduction.
*Intravenous mannitol*
- **Intravenous mannitol** is an osmotic diuretic primarily used to reduce **intracranial pressure** or to promote diuresis.
- It does not directly lower blood pressure effectively in a hypertensive emergency and is not a primary antihypertensive agent.
Hypertension diagnosis and management US Medical PG Question 9: A 41-year-old African American man presents to his primary care physician a few months after being found to have a blood pressure of 152/95 mmHg. The patient denies any current symptoms, having any past medical history, or prior hospitalizations. He does not take any medications but takes one multivitamin daily. His blood pressures on three separate occasions have been 151/93 mmHg, 150/90 mmHg, and 155/97 mmHg. In today’s visit, his blood pressure is 149/91 mmHg despite exercise and dietary modifications. Physical examination is unremarkable. After extensive work-up he is started on appropriate monotherapy for his hypertension. Which of the following laboratory abnormalities may be found on follow-up testing?
- A. Hyperkalemia
- B. Hypermagnesemia
- C. Hypolipidemia
- D. Hypercalcemia (Correct Answer)
- E. Hypouricemia
Hypertension diagnosis and management Explanation: **Hypercalcemia**
- This African American patient with stage 2 hypertension unresponsive to lifestyle modifications requires pharmacologic therapy.
- **First-line options** for African American patients include **thiazide diuretics** or **calcium channel blockers** (per ACC/AHA guidelines).
- Given the question asks about hypercalcemia, the appropriate monotherapy is a **thiazide diuretic** (e.g., chlorthalidone, hydrochlorothiazide).
- Thiazide diuretics **inhibit calcium excretion** in the distal convoluted tubule, leading to increased calcium reabsorption and potential **hypercalcemia**.
- This is a well-known side effect that requires monitoring during thiazide therapy.
*Hyperkalemia*
- **Thiazide diuretics** cause **hypokalemia** (low potassium), not hyperkalemia, by increasing potassium excretion in the distal tubule.
- Hyperkalemia is associated with **potassium-sparing diuretics** (spironolactone, amiloride), **ACE inhibitors**, or **ARBs**.
*Hypermagnesemia*
- **Thiazide diuretics** increase urinary magnesium excretion, potentially causing **hypomagnesemia**, not hypermagnesemia.
- Hypermagnesemia is rare and typically seen with renal failure or excessive magnesium supplementation.
*Hypolipidemia*
- **Thiazide diuretics** can cause **mild dyslipidemia** (increased LDL cholesterol and triglycerides), not hypolipidemia.
- Hypolipidemia (abnormally low lipid levels) is not a recognized side effect of antihypertensive therapy.
*Hypouricemia*
- **Thiazide diuretics** decrease uric acid secretion in the proximal tubule, leading to **hyperuricemia** and potential gout precipitation.
- Hypouricemia would not be expected with thiazide therapy.
Hypertension diagnosis and management US Medical PG Question 10: A 65-year-old man presents to the emergency department for sudden weakness. The patient states that he was at home enjoying his morning coffee when his symptoms began. He says that his left arm suddenly felt very odd and weak thus prompting him to come to the ED. The patient has a past medical history of diabetes, COPD, hypertension, anxiety, alcohol abuse, and PTSD. He recently fell off a horse while horseback riding but claims to not have experienced any significant injuries. He typically drinks 5-7 drinks per day and his last drink was yesterday afternoon. His current medications include insulin, metformin, atorvastatin, lisinopril, albuterol, and fluoxetine. His temperature is 99.5°F (37.5°C), blood pressure is 177/118 mmHg, pulse is 120/min, respirations are 18/min, and oxygen saturation is 93% on room air. On physical exam, you note an elderly man who is mildly confused. Cardiopulmonary exam demonstrates bilateral expiratory wheezes and a systolic murmur along the right upper sternal border that radiates to the carotids. Neurological exam reveals cranial nerves II-XII as grossly intact with finger-nose exam mildly abnormal on the left and heel-shin exam within normal limits. The patient has 5/5 strength in his right arm and 3/5 strength in his left arm. The patient struggles to manipulate objects such as a pen with his left hand. The patient is given a dose of diazepam and started on IV fluids. Which of the following is the most likely diagnosis in this patient?
- A. Bridging vein tear
- B. Cerebellar bleeding
- C. Berry aneurysm rupture
- D. Hypertensive encephalopathy
- E. Lipohyalinosis (Correct Answer)
Hypertension diagnosis and management Explanation: ***Lipohyalinosis***
- This patient's history of **hypertension** and **diabetes** are major risk factors for **lipohyalinosis**, which leads to **lacunar infarcts** and presents with sudden onset **pure motor hemiparesis**, as seen with the left arm weakness.
- The elevated blood pressure of 177/118 mmHg further supports a diagnosis involving **cerebral small vessel disease** secondary to chronic hypertension.
*Bridging vein tear*
- A bridging vein tear would typically lead to a **subdural hematoma**, characterized by a **gradual onset of symptoms** like headache, confusion, and neurological deficits, often following trauma, which is inconsistent with the sudden onset in this case.
- While the patient recently fell off a horse, his symptoms are acute and focal, not typical of the delayed presentation often seen with subdural hematomas.
*Cerebellar bleeding*
- **Cerebellar bleeding** usually presents with symptoms such as **ataxia**, **nystagmus**, vertigo, and vomiting, along with potential truncal instability, which are not the primary symptoms observed here.
- While the patient has some mild abnormality on the finger-nose test, the predominant symptom is **pure motor weakness** of the left arm, making a cerebellar bleed less likely.
*Berry aneurysm rupture*
- A **berry aneurysm rupture** typically causes a **sudden, severe headache** (thunderclap headache), neck stiffness, photophobia, and altered mental status due to subarachnoid hemorrhage, which are not reported by the patient.
- The patient's primary complaint is **focal motor weakness** and mild confusion, not the classic diffuse hemorrhagic symptoms of aneurysm rupture.
*Hypertensive encephalopathy*
- **Hypertensive encephalopathy** presents with a more generalized and rapidly progressive decline in neurological function, including severe headache, altered mental status, seizures, and visual disturbances, usually with **diastolic blood pressure >120 mmHg**.
- While the patient's blood pressure is high, the presentation of **focal motor deficit without severe headache** or global neurological decline makes this less likely than a lacunar stroke due to lipohyalinosis.
More Hypertension diagnosis and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.