Cardiac tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiac tumors US Medical PG Question 1: A 68-year-old man comes to the emergency department because of a 1-week history of difficulty breathing. He has had recurrent palpitations over the past 2 years. During this time, he has also had several episodes of anxiety despite no change in his daily life. He has occasional sharp chest pain localized to the left upper sternal border. He has no abdominal pain or leg swelling. Two years ago, he had streptococcal pharyngitis, which was promptly treated with a 10-day course of penicillin. He has never traveled outside of the country. His temperature is 36.5°C (97.7°F), pulse is 82/min, and blood pressure is 140/85 mm Hg. Physical examination shows a 3/6 holosystolic murmur that is loudest at the apex and radiates to the axilla with a mid-systolic click. Bilateral fine crackles are heard on lung auscultation. Which of the following is the most likely cause of this patient's symptoms?
- A. Inflammatory valve degeneration
- B. Ectopic production of serotonin
- C. Myxomatous valve degeneration (Correct Answer)
- D. Calcific valve degeneration
- E. Overproduction of catecholamines
Cardiac tumors Explanation: ***Myxomatous valve degeneration***
- The presence of a **mid-systolic click** followed by a **holosystolic murmur** at the apex radiating to the axilla is highly characteristic of **mitral valve prolapse (MVP)** with **mitral regurgitation (MR)**.
- MVP is most commonly caused by **myxomatous degeneration** of the mitral valve leaflets, leading to their billowing into the left atrium during systole. The patient's recurrent palpitations, anxiety, and non-exertional chest pain are common symptoms associated with MVP, while difficulty breathing and crackles suggest **heart failure** from chronic MR.
*Inflammatory valve degeneration*
- **Inflammatory valve degeneration**, such as that seen in rheumatic heart disease, typically presents with a history of recurrent streptococcal infections leading to valvular scarring and dysfunction (e.g., mitral stenosis).
- While the patient had streptococcal pharyngitis, it was treated, and the clinical presentation with a mid-systolic click is more indicative of myxomatous changes rather than rheumatic inflammation.
*Ectopic production of serotonin*
- **Ectopic production of serotonin** occurs in settings like **carcinoid syndrome**, which typically involves flushing, diarrhea, bronchospasm, and can affect the right-sided heart valves primarily.
- The patient's symptoms are centered on left-sided heart issues and do not align with the broader systemic features of carcinoid syndrome.
*Calcific valve degeneration*
- **Calcific valve degeneration** commonly affects the **aortic valve** leading to **aortic stenosis** in older adults, characterized by a systolic ejection murmur heard at the right upper sternal border.
- It does not typically cause a mid-systolic click or affect the mitral valve in this manner, and the murmur description is inconsistent with aortic stenosis.
*Overproduction of catecholamines*
- **Overproduction of catecholamines**, as seen in conditions like **pheochromocytoma**, causes symptoms such as paroxysmal hypertension, palpitations, sweating, and anxiety.
- While some symptoms like palpitations and anxiety overlap, the specific cardiac murmur and signs of heart failure are not directly explained by catecholamine excess alone; a structural heart problem is more likely.
Cardiac tumors US Medical PG Question 2: A 38-year-old woman comes to the physician because of a 10-month history of nonbloody diarrhea and recurrent episodes of flushing and wheezing. She does not take any medications. Physical examination shows a hyperpigmented rash around the base of her neck. Cardiac examination shows a grade 4/6, holosystolic murmur in the 5th intercostal space at the left midclavicular line. Echocardiography shows left-sided endocardial and valvular fibrosis with moderate mitral regurgitation; there are no septal defects or right-sided valvular defects. Urinalysis shows increased 5-hydroxyindoleacetic acid concentration. Further evaluation of this patient is most likely to show which of the following findings?
- A. Tumor in the descending colon with hepatic metastasis
- B. Tumor in the left atrium with hepatic metastasis
- C. Tumor in the pancreas without metastasis
- D. Tumor in the lung without metastasis (Correct Answer)
- E. Tumor in the appendix without metastasis
Cardiac tumors Explanation: ***Tumor in the lung without metastasis***
- The patient presents with **carcinoid syndrome** symptoms (flushing, wheezing, diarrhea, hyperpigmented rash, increased 5-HIAA), but the **left-sided valvular fibrosis** (mitral regurgitation) is atypical for classic carcinoid, which usually affects the right heart.
- Left-sided heart involvement in carcinoid syndrome occurs when a **primary bronchial carcinoid tumor** directly releases serotonin into the pulmonary veins and systemic circulation, bypassing both hepatic metabolism and the right heart, allowing it to reach the left heart valves before inactivation.
- This is the key distinguishing feature: only bronchial/lung carcinoids can cause left-sided cardiac disease because they drain into pulmonary veins rather than the portal or systemic venous system.
*Tumor in the descending colon with hepatic metastasis*
- A tumor in the descending colon would release serotonin into the **portal circulation**, which would then be **metabolized by the liver** before reaching the systemic circulation.
- Even with liver metastases releasing serotonin into hepatic veins, it would enter the **right heart first** via the IVC, causing **right-sided valvular disease** (tricuspid regurgitation, pulmonary stenosis), not left-sided mitral regurgitation.
- The lungs inactivate serotonin, protecting the left heart in GI carcinoid cases.
*Tumor in the left atrium with hepatic metastasis*
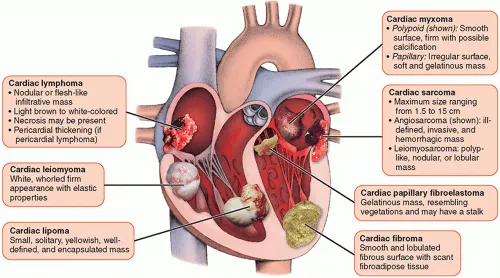
- Primary cardiac tumors (myxomas) do not produce serotonin and would not explain the systemic symptoms of **carcinoid syndrome**, such as flushing, wheezing, or elevated 5-HIAA.
- This combination is anatomically and pathophysiologically implausible for carcinoid syndrome.
*Tumor in the pancreas without metastasis*
- A pancreatic neuroendocrine tumor (PNET) can produce serotonin, but without hepatic metastases, the serotonin released into the portal system would be **metabolized by the liver**, preventing systemic carcinoid syndrome.
- Even with metastases, it would typically cause **right-sided heart disease** as serotonin from liver metastases enters the right heart first.
- The absence of metastasis makes this highly unlikely to cause the clinical syndrome.
*Tumor in the appendix without metastasis*
- Appendiceal carcinoid tumors, especially without metastasis, are generally **asymptomatic** or cause only local symptoms, as the serotonin produced drains into the portal system and is effectively metabolized by the liver.
- They would not cause systemic carcinoid syndrome, and certainly not isolated left-sided cardiac involvement.
Cardiac tumors US Medical PG Question 3: A 48-year-old woman comes to the physician because of progressively worsening dyspnea on exertion and fatigue for the past 2 months. She had Hodgkin lymphoma as an adolescent, which was treated successfully with chemotherapy and radiation. Her father died from complications related to amyloidosis. She does not smoke or drink alcohol. Her temperature is 36.7°C (98°F), pulse is 124/min, respirations are 20/min, and blood pressure is 98/60 mm Hg. Cardiac examination shows no murmurs. Coarse crackles are heard at the lung bases bilaterally. An ECG shows an irregularly irregular rhythm with absent P waves. An x-ray of the chest shows globular enlargement of the cardiac shadow with prominent hila and bilateral fluffy infiltrates. Transthoracic echocardiography shows a dilated left ventricle with an ejection fraction of 40%. Which of the following is the most likely cause of this patient's condition?
- A. Postradiation fibrosis
- B. Coronary artery occlusion
- C. Amyloid deposition
- D. Acute psychological stress
- E. Chronic tachycardia (Correct Answer)
Cardiac tumors Explanation: ***Chronic tachycardia***
- The **irregularly irregular rhythm with absent P waves** on ECG is characteristic of **atrial fibrillation**, which can lead to **tachycardia-induced cardiomyopathy** if sustained. The pulse of 124/min supports this.
- A sustained elevated heart rate like 124/min, especially in the context of atrial fibrillation, can cause **ventricular dilation** and reduced ejection fraction, leading to symptoms like dyspnea and fatigue observed in the patient.
*Postradiation fibrosis*
- While the patient has a history of radiation therapy for Hodgkin lymphoma, **radiation-induced cardiac damage** typically manifests as perivascular **fibrosis**, leading to **restrictive cardiomyopathy** or pericardial disease, not primarily dilated cardiomyopathy with an irregularly irregular rhythm.
- This condition is often associated with a **reduced diastolic filling** and **normal systolic function** initially, which contradicts the dilated left ventricle and reduced ejection fraction described.
*Amyloid deposition*
- The family history of amyloidosis is a red herring in this clinical picture. While **cardiac amyloidosis** can cause heart failure, it typically presents as **restrictive cardiomyopathy** with **thickened ventricular walls** and normal or reduced ventricular cavity size, not a dilated left ventricle.
- ECG findings in amyloidosis often include **low voltage QRS complexes** despite thickened walls, which is not described.
*Coronary artery occlusion*
- **Coronary artery occlusion** (e.g., myocardial infarction) can lead to dilated cardiomyopathy and reduced ejection fraction, but it usually presents with chest pain or specific ECG changes (e.g., ST elevation/depression, Q waves) that are not mentioned.
- The **irregularly irregular rhythm** (atrial fibrillation) and absence of murmurs make a primary ischemic event less likely as the sole explanation for the global cardiac changes.
*Acute psychological stress*
- **Acute psychological stress** can trigger **takotsubo cardiomyopathy** (stress-induced cardiomyopathy), which presents with left ventricular dysfunction and apical ballooning.
- However, this is typically an acute event with different ECG patterns (often ST elevation) and would not explain the chronic, sustained tachycardia and atrial fibrillation leading to dilated cardiomyopathy.
Cardiac tumors US Medical PG Question 4: A 62-year-old woman presents to the emergency department with a 2-hour history of sharp chest pain. She says that the pain is worse when she inhales and is relieved by sitting up and leaning forward. Her past medical history is significant for rheumatoid arthritis, myocardial infarction status post coronary artery bypass graft, and radiation for breast cancer 20 years ago. Physical exam reveals a rubbing sound upon cardiac auscultation as well as increased jugular venous distention on inspiration. Pericardiocentesis is performed revealing grossly bloody fluid. Which of the following is most specifically associated with this patient's presentation?
- A. Myocardial infarction
- B. Malignancy (Correct Answer)
- C. Uremia
- D. Rheumatoid arthritis
- E. Viral illness
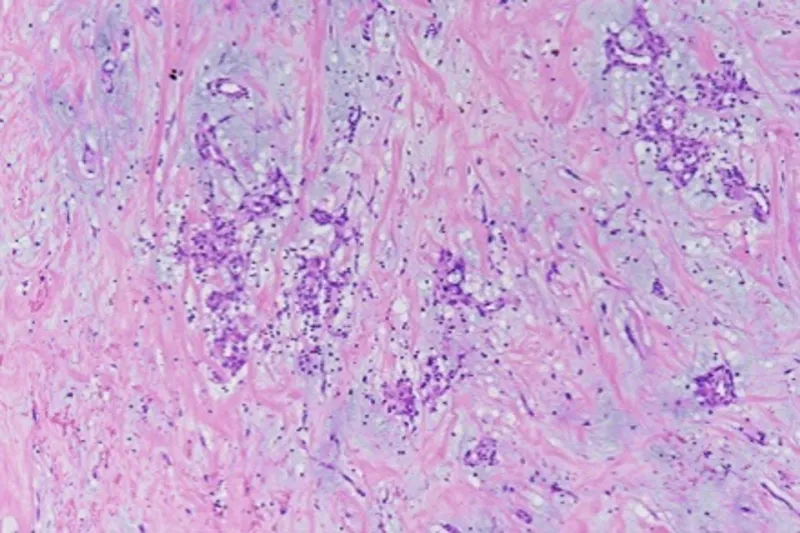
Cardiac tumors Explanation: ***Malignancy***
- The presence of **grossly bloody (hemorrhagic) pericardial fluid** is the key finding that most specifically points to **malignancy** as the underlying cause.
- **Hemorrhagic pericardial effusion** is most commonly associated with: (1) malignancy, (2) tuberculosis, or (3) trauma. Given the patient's **history of radiation therapy for breast cancer 20 years ago**, malignancy (either metastatic breast cancer or radiation-induced secondary malignancy) is the most likely cause.
- Clinical features like **chest pain** worse on inspiration and relieved by leaning forward, a **pericardial friction rub**, and **increased jugular venous distention on inspiration (Kussmaul sign)** indicate pericarditis with possible cardiac tamponade.
*Myocardial infarction*
- While myocardial infarction can lead to pericarditis (acute post-MI pericarditis or delayed Dressler's syndrome), the pericardial fluid is typically **serous or serosanguinous, not grossly bloody**.
- The patient's history of prior MI and CABG makes this less likely to be the cause of this acute presentation with hemorrhagic effusion.
- Post-MI pericarditis usually occurs within days to weeks after the MI event.
*Uremia*
- **Uremic pericarditis** occurs in patients with severe kidney failure (uremia) and typically presents with **serofibrinous exudate**, not grossly bloody effusion.
- There is no clinical indication of renal failure or uremia in this patient's presentation.
*Rheumatoid arthritis*
- **Rheumatoid pericarditis** can occur in patients with RA, but the pericardial effusion is usually **sterile and serofibrinous**, rarely resulting in frankly hemorrhagic fluid.
- While this patient has RA, the **grossly bloody fluid** and **history of breast cancer radiation** make malignancy a much more specific and likely diagnosis.
*Viral illness*
- **Viral pericarditis** is a common cause of acute pericarditis and typically presents with chest pain and a pericardial friction rub.
- However, viral pericarditis usually produces **serous or serofibrinous effusions, not grossly bloody fluid**.
- There is no mention of prodromal viral symptoms, and the hemorrhagic nature of the fluid strongly argues against a viral etiology.
Cardiac tumors US Medical PG Question 5: A previously healthy 20-year-old man is brought to the emergency department 15 minutes after collapsing while playing basketball. He has no history of serious illness. On arrival, there is no palpable pulse or respiratory effort observed. He is declared dead. The family agrees to an autopsy. Cardiac workup prior to this patient's death would most likely have shown which of the following findings?
- A. Systolic anterior motion of the mitral valve (Correct Answer)
- B. Narrowing of the left main coronary artery
- C. Bicuspid aortic valve
- D. Asymmetric septal hypertrophy
- E. Ventricular septal defect
Cardiac tumors Explanation: ***Systolic anterior motion of the mitral valve***
- This finding is characteristic of **hypertrophic cardiomyopathy (HCM)**, the most common cause of sudden cardiac death in young athletes.
- **Systolic anterior motion (SAM)** of the mitral valve leads to **left ventricular outflow tract (LVOT) obstruction**, which can precipitate fatal arrhythmias during exertion.
- While asymmetric septal hypertrophy is the underlying anatomical abnormality in HCM, **SAM is the dynamic functional finding** on echocardiography that directly explains the mechanism of sudden death during exercise due to LVOT obstruction.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** is a congenital heart defect that typically presents with a **murmur** and may lead to heart failure or pulmonary hypertension if large.
- While VSDs can cause complications, they are not typically associated with sudden cardiac death in a previously healthy young adult collapsing during exertion without prior symptoms.
*Narrowing of the left main coronary artery*
- Significant **coronary artery disease (CAD)**, especially of the left main, is a common cause of sudden cardiac death but is rare in a **20-year-old** without significant risk factors.
- When coronary anomalies occur in young individuals causing sudden death, it's typically due to **anomalous coronary artery origin** rather than atherosclerotic narrowing.
*Bicuspid aortic valve*
- A **bicuspid aortic valve** is a congenital malformation that can lead to **aortic stenosis** or **regurgitation**, or an increased risk of aortic dissection.
- While it can be associated with sudden cardiac events, it is less commonly implicated in sudden cardiac death in an otherwise healthy young athlete during exertion compared to HCM.
*Asymmetric septal hypertrophy*
- This describes the **morphological hallmark** of **hypertrophic cardiomyopathy (HCM)** where the **interventricular septum** is disproportionately thickened (≥15 mm or septal-to-free wall ratio ≥1.3).
- While this is the diagnostic anatomical finding for HCM, **systolic anterior motion (SAM) of the mitral valve** is the specific *dynamic functional abnormality* seen on cardiac workup that directly causes LVOT obstruction and explains the mechanism of sudden death during exercise in this clinical scenario.
Cardiac tumors US Medical PG Question 6: A 53-year-old woman comes to the physician because of increasing shortness of breath on exertion for 5 months. She reports that she can not climb more than 2 flights of stairs and she is no longer able to run her errands as usual. One year ago, she was diagnosed with triple-negative breast cancer. She underwent a right-sided modified radical mastectomy and adjuvant chemotherapy. Cardiac examination shows a laterally displaced point of maximal impulse. Coarse inspiratory crackles are heard in both lower lung fields. Echocardiography shows a left ventricular ejection fraction of 30%. The physician informs the patient that her symptoms are most likely due to an adverse effect of her chemotherapy. The drug most likely responsible for the patient's current symptoms belongs to which of the following groups of agents?
- A. Antimetabolites
- B. Monoclonal antibodies
- C. Alkylating agents
- D. Topoisomerase I inhibitors
- E. Anthracyclines (Correct Answer)
Cardiac tumors Explanation: ***Anthracyclines***
- The patient's presentation of **dilated cardiomyopathy** (shortness of breath, laterally displaced PMI, coarse crackles, reduced ejection fraction) following chemotherapy for breast cancer is characteristic of **anthracycline-induced cardiotoxicity**.
- **Anthracyclines** such as doxorubicin and epirubicin are known to cause **dose-dependent cardiotoxicity**, leading to irreversible myocardial damage and heart failure.
*Antimetabolites*
- **Antimetabolites** (e.g., methotrexate, 5-fluorouracil) primarily interfere with DNA synthesis and repair.
- While they can have side effects like myelosuppression and mucositis, **significant cardiotoxicity** leading to dilated cardiomyopathy is not their primary or most common adverse effect.
*Monoclonal antibodies*
- Some **monoclonal antibodies**, particularly trastuzumab (Herceptin), used in HER2-positive breast cancer, can cause cardiotoxicity, but it is typically **reversible** and not seen with triple-negative breast cancer unless used in combination with anthracyclines.
- The type of cardiomyopathy with trastuzumab is usually **reversible cardiac dysfunction** rather than irreversible dilated cardiomyopathy.
*Alkylating agents*
- **Alkylating agents** (e.g., cyclophosphamide, cisplatin) primarily damage DNA, leading to cell death.
- While they can cause various side effects, **dilated cardiomyopathy** is not a hallmark or common cardiotoxic effect, unlike anthracyclines, though high-dose cyclophosphamide can cause acute pericarditis or myocarditis.
*Topoisomerase I inhibitors*
- **Topoisomerase I inhibitors** (e.g., irinotecan, topotecan) typically cause gastrointestinal side effects (diarrhea), myelosuppression, and fatigue.
- **Cardiotoxicity** leading to dilated cardiomyopathy is not a prominent or common side effect associated with this class of drugs.
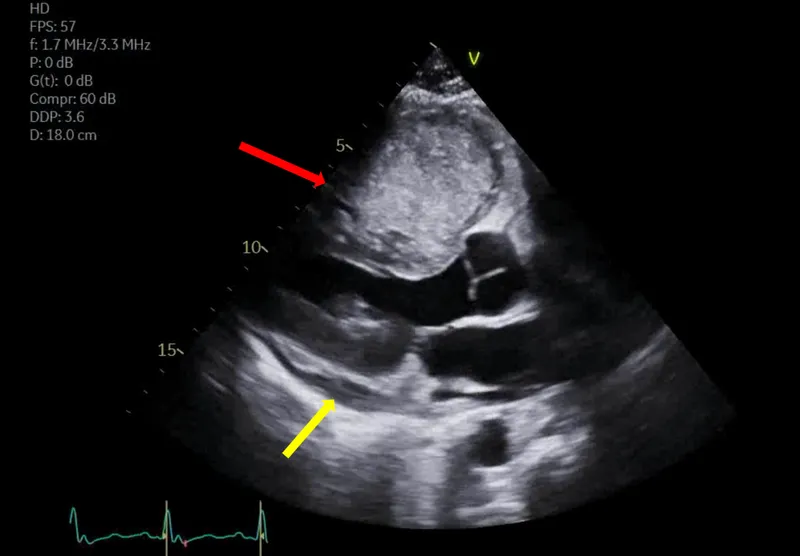
Cardiac tumors US Medical PG Question 7: A 52-year-old woman comes to the physician because of a 1-month history of mild fever, fatigue, and shortness of breath. She has no history of serious medical illness and takes no medications. Cardiopulmonary examination shows a mid-diastolic plopping sound heard best at the apex and bilateral rales at the base of the lungs. Echocardiography shows a pedunculated, heterogeneous mass in the left atrium. A biopsy of the mass shows clusters of mesenchymal cells surrounded by gelatinous material. Further evaluation of this patient is most likely to show which of the following?
- A. Malignant pleural effusion
- B. Axillary lymphadenopathy
- C. Increased S100 protein serum concentration
- D. Increased IL-6 serum concentration (Correct Answer)
- E. Ash-leaf skin lesions
Cardiac tumors Explanation: ***Increased IL-6 serum concentration***
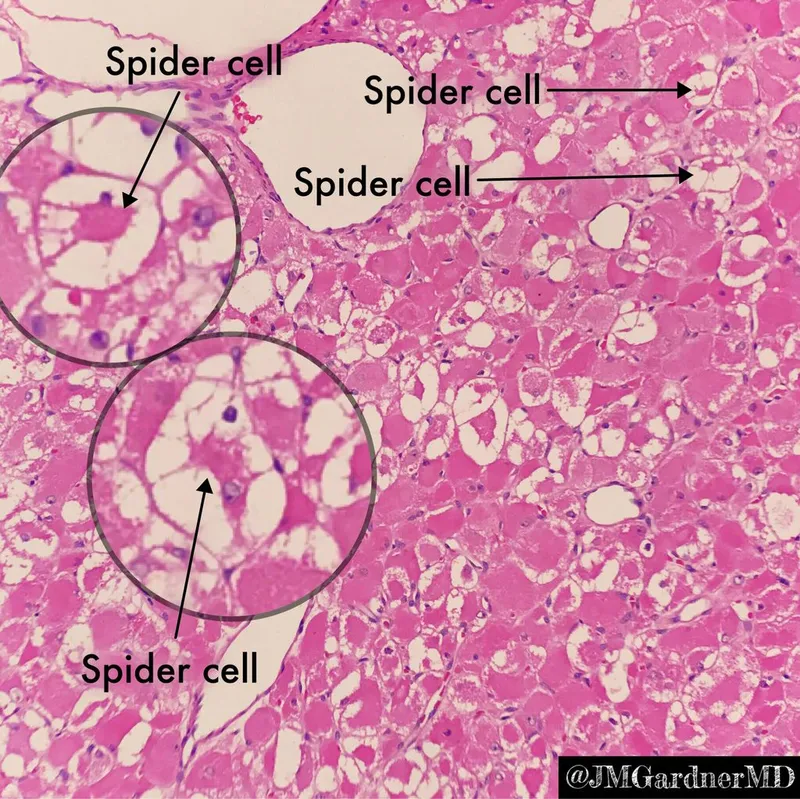
- This patient's presentation with **fever**, **fatigue**, **shortness of breath**, and a **pedunculated left atrial mass** on echocardiography is highly suggestive of a **cardiac myxoma**.
- **Cardiac myxomas** are known to secrete various cytokines, including **IL-6**, which can cause constitutional symptoms such as fever, fatigue, and weight loss.
*Malignant pleural effusion*
- While pleural effusions can cause shortness of breath, a **malignant pleural effusion** is usually associated with an underlying malignancy, and the described cardiac mass is benign.
- The patient's symptoms are more directly attributable to the **obstructive effects** and **cytokine secretion** of the left atrial myxoma.
*Axillary lymphadenopathy*
- **Axillary lymphadenopathy** would suggest an infection or malignancy in the upper extremity or breast, which is not supported by the patient's presentation focusing on cardiac and systemic symptoms related to an atrial mass.
- Myxomas do not typically metastasize or cause regional lymph node involvement.
*Increased S100 protein serum concentration*
- **S100 protein** is a marker primarily associated with **melanoma** and **neural crest tumors**.
- It is not a characteristic finding in patients with **cardiac myxomas**.
*Ash-leaf skin lesions*
- **Ash-leaf spots** are hypopigmented macules characteristic of **tuberous sclerosis**, a genetic disorder.
- This condition is not related to **cardiac myxomas** and would present with different neurological and dermatological findings.
Cardiac tumors US Medical PG Question 8: A 69-year-old man is scheduled to undergo radical retropubic prostatectomy for prostate cancer in 2 weeks. He had a myocardial infarction at the age of 54 years. He has a history of GERD, unstable angina, hyperlipidemia, and severe osteoarthritis in the left hip. He is unable to climb up stairs or walk fast because of pain in his left hip. He had smoked one pack of cigarettes daily for 30 years but quit 25 years ago. He drinks one glass of wine daily. Current medications include aspirin, metoprolol, lisinopril, rosuvastatin, omeprazole, and ibuprofen as needed. His temperature is 36.4°C (97.5°F), pulse is 90/min, and blood pressure is 136/88 mm Hg. Physical examination shows no abnormalities. A 12-lead ECG shows Q waves and inverted T waves in leads II, III, and aVF. His B-type natriuretic protein is 84 pg/mL (N < 125). Which of the following is the most appropriate next step in management to assess this patient's perioperative cardiac risk?
- A. No further testing
- B. 24-hour ambulatory ECG monitoring
- C. Radionuclide myocardial perfusion imaging (Correct Answer)
- D. Treadmill stress test
- E. Resting echocardiography
Cardiac tumors Explanation: ***Radionuclide myocardial perfusion imaging***
- This patient requires **perioperative cardiac risk assessment** before intermediate-risk surgery (radical prostatectomy).
- Key factors include: history of **myocardial infarction**, current cardiac risk factors, and **inability to exercise** due to severe osteoarthritis.
- Since he cannot perform exercise stress testing, **pharmacologic stress testing** with radionuclide myocardial perfusion imaging (using agents like adenosine, dipyridamole, or regadenoson) is the most appropriate test to assess for **inducible myocardial ischemia**.
- This provides functional assessment of coronary perfusion under pharmacologic stress, helping guide perioperative risk stratification and management.
- *Note: The presence of unstable angina would typically require cardiac stabilization first; this question focuses on selecting the appropriate stress test modality for a patient unable to exercise.*
*No further testing*
- This patient has significant cardiac risk factors including **prior MI**, ongoing cardiac medications, and ECG changes suggesting old infarction.
- Proceeding directly to surgery without functional cardiac assessment would be **inappropriate** given his risk profile and the intermediate-risk nature of the planned surgery.
*24-hour ambulatory ECG monitoring*
- Holter monitoring detects arrhythmias and silent ischemic episodes but does not provide **functional capacity assessment** or evaluation of inducible ischemia under stress conditions.
- It is not the primary tool for **perioperative cardiac risk stratification** before major surgery.
*Treadmill stress test*
- The patient's **severe osteoarthritis** prevents him from climbing stairs or walking fast, making him unable to achieve adequate exercise workload for a treadmill stress test.
- This functional limitation makes **exercise stress testing contraindicated**; pharmacologic stress testing is required instead.
*Resting echocardiography*
- Resting echocardiography assesses **baseline left ventricular function**, wall motion abnormalities from prior infarction, and valvular disease.
- While useful for structural assessment, it does **not evaluate for exercise-induced or stress-induced ischemia**, which is critical for perioperative risk assessment in patients with coronary artery disease.
- His normal BNP (84 pg/mL) suggests adequate baseline ventricular function, making functional ischemia assessment more relevant than structural evaluation alone.
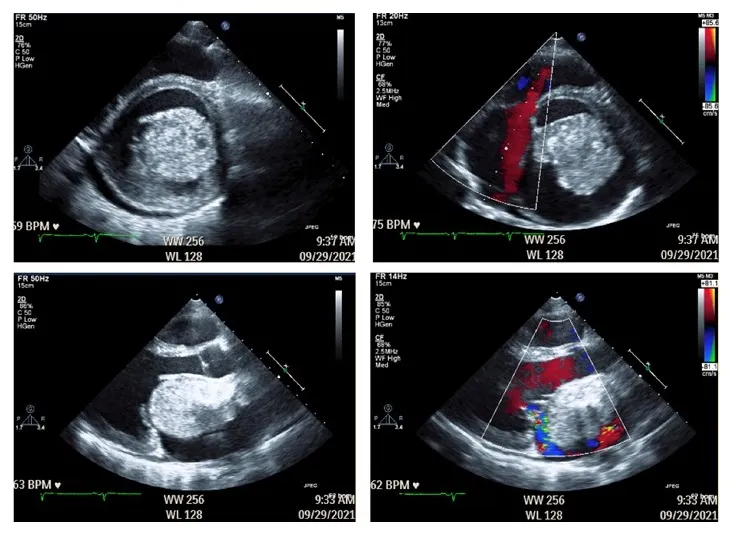
Cardiac tumors US Medical PG Question 9: A 38-year-old woman is referred to a cardiologist for evaluation of syncope. Over the past year she has experienced 2 syncopal events. The first event occurred while she was standing, and the second when she laid down on her side. She denies bowel or bladder incontinence during the episodes or palpitations. However, she reports the presence of a low-grade fever over the past 3 months and a recent visit to the emergency department for a transient ischemic attack. She has a history of intravenous drug use but reports not having used in over 5 years. Temperature is 100.0°F (37.8°C), blood pressure is 115/72 mmHg, pulse is 90/min, and respirations are 20/min and regular. A detailed neurologic examination reveals no focal deficits. Cardiac auscultation demonstrates a diastolic "plop" at the cardiac apex. Which of the following findings will most likely be demonstrated on transthoracic echocardiography?
- A. Flail mitral valve leaflet
- B. Left ventricular mass
- C. Decreased left ventricular ejection fraction
- D. Left atrial pedunculated mass (Correct Answer)
- E. Patent foramen ovale
Cardiac tumors Explanation: ***Left atrial pedunculated mass***
- The patient's presentation with **syncope** in varying positions (standing and lying down), a **low-grade fever**, history of **transient ischemic attack (TIA)**, and a **diastolic "plop"** strongly suggests a **left atrial myxoma**.
- A left atrial myxoma is a **pedunculated tumor** that can intermittently obstruct mitral valve flow, leading to syncope, and can embolize, causing TIAs.
*Flail mitral valve leaflet*
- A flail mitral valve leaflet typically causes severe **mitral regurgitation**, characterized by a **systolic murmur**.
- While it can lead to syncope due to reduced cardiac output, it would not typically present with a "diastolic plop" or TIA in this manner.
*Decreased left ventricular ejection fraction*
- A decreased left ventricular ejection fraction would cause syncope due to **heart failure** or **arrhythmias**, but it does not explain the "diastolic plop" or the TIA, especially with a history of fever.
- The "plop" sound is highly specific for an **intracardiac mass** obstructing flow.
*Left ventricular mass*
- A left ventricular mass, such as a thrombus or tumor, could cause syncope and embolization (TIA).
- However, it is unlikely to produce a **diastolic "plop"** sound, which is characteristic of a mass prolapsing into the mitral orifice during diastole.
*Patent foramen ovale*
- A patent foramen ovale (PFO) can cause **paradoxical emboli** leading to TIA, especially in the context of intravenous drug use history.
- However, a PFO does not explain the recurrent syncope in various positions, the **low-grade fever**, or the specific **diastolic "plop"** on auscultation.
Cardiac tumors US Medical PG Question 10: A 65-year-old man with hypertension comes to the physician for a routine health maintenance examination. Current medications include atenolol, lisinopril, and atorvastatin. His pulse is 86/min, respirations are 18/min, and blood pressure is 145/95 mm Hg. Cardiac examination is shown. Which of the following is the most likely cause of this physical examination finding?
- A. Myxomatous degeneration of the mitral valve
- B. Inflammation of the pericardium
- C. Thickening of the mitral valve leaflets
- D. Decreased compliance of the left ventricle (Correct Answer)
- E. Dilation of the aortic root
Cardiac tumors Explanation: ***Decrease in compliance of the left ventricle***
- The patient's **uncontrolled hypertension** for a long time can lead to **left ventricular hypertrophy** and **stiffening** of the heart muscle, resulting in **decreased compliance**.
- A decrease in left ventricular compliance can result in a **diastolic dysfunction**, leading to **heart failure with preserved ejection fraction (HFpEF)**.
*Myxomatous degeneration of the mitral valve*
- This condition is typically associated with **mitral valve prolapse**, which causes a **mid-systolic click** and a **late systolic murmur**.
- There is no information in the question about associated findings to suggest mitral valve prolapse, such as valvular disease or specific murmurs.
*Inflammation of the pericardium*
- **Pericarditis** typically presents with **sharp chest pain** that is relieved by leaning forward and a characteristic **friction rub** on auscultation.
- While inflammation can affect cardiac function, it's not the most direct consequence of chronic hypertension in the absence of other symptoms.
*Thickening of the mitral valve leaflets*
- **Mitral valve leaflet thickening** often results from **rheumatic fever** or age-related calcification, leading to **mitral stenosis** or **regurgitation**.
- The patient's history of long-standing hypertension does not directly indicate thickening of the mitral valve leaflets.
*Dilation of the aortic root*
- Aortic root dilation is associated with conditions like **Marfan syndrome**, **Ehlers-Danlos syndrome**, or uncontrolled hypertension leading to **aortic aneurysm** or **dissection**.
- While chronic hypertension can contribute to aortic dilation, this finding isn't directly supported by the current clinical picture suggesting a primary cause for a physical finding.
More Cardiac tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.