Cardiac imaging modalities US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac imaging modalities. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiac imaging modalities US Medical PG Question 1: A 57-year-old man presents to his family physician for a routine exam. He feels well and reports no new complaints since his visit last year. Last year, he had a colonoscopy which showed no polyps, a low dose chest computerized tomography (CT) scan that showed no masses, and routine labs which showed a fasting glucose of 93 mg/dL. He is relatively sedentary and has a body mass index (BMI) of 24 kg/m^2. He has a history of using methamphetamines, alcohol (4-5 drinks per day since age 30), and tobacco (1 pack per day since age 18), but he joined Alcoholics Anonymous and has been in recovery, not using any of these for the past 7 years. Which of the following is indicated at this time?
- A. Colonoscopy
- B. Chest computerized tomography (CT) scan (Correct Answer)
- C. Abdominal ultrasound
- D. Chest radiograph
- E. Fasting glucose
Cardiac imaging modalities Explanation: ***Chest computerized tomography (CT) scan***
- This patient has a significant **smoking history** (1 pack per day since age 18 = **39 pack-years**) and is 57 years old, placing him in a high-risk group for **lung cancer**.
- Annual low-dose CT screening for lung cancer is recommended for individuals aged 50-80 with a 20 pack-year smoking history who currently smoke or have quit within the past 15 years.
- He meets all criteria: age 57, 39 pack-years, and quit only 7 years ago (within the 15-year window).
- Since he had screening **last year** with no masses, this year's visit represents the appropriate time for his **annual follow-up screening**.
*Colonoscopy*
- The patient had a colonoscopy last year with **no polyps**, suggesting he is at average risk for colorectal cancer.
- For individuals at average risk with normal findings, repeat screening colonoscopy is typically recommended every **10 years** (or every 5 years for flexible sigmoidoscopy), not annually.
*Abdominal ultrasound*
- One-time abdominal ultrasound screening for **abdominal aortic aneurysm (AAA)** is recommended for men aged 65-75 who have ever smoked.
- This patient is only 57 years old and does not yet meet the age criteria for AAA screening.
*Chest radiograph*
- While a chest radiograph can identify some lung abnormalities, a **low-dose CT scan** is far more sensitive and specific for detecting early-stage lung cancer in high-risk populations.
- Chest radiography is **not recommended** as a screening tool for lung cancer due to its lower sensitivity and lack of mortality benefit in trials.
*Fasting glucose*
- The patient had a **normal fasting glucose** of 93 mg/dL last year, and there are no new symptoms suggestive of diabetes.
- For asymptomatic adults with normal glucose, diabetes screening is typically repeated every **3 years**.
- Annual re-screening is not indicated without new risk factors or symptoms.
Cardiac imaging modalities US Medical PG Question 2: A 41-year-old man presents to his primary care provider because of chest pain with activity for the past 6 months. Past medical history is significant for appendectomy at age 12 and hypertension, and diabetes mellitus type 2 that is poorly controlled. He takes metformin and lisinopril but admits that he is bad at remembering to take them everyday. His father had a heart attack at 41 and 2 stents were placed in his heart. His mother is healthy. He drinks alcohol occasionally and smokes a half of a pack of cigarettes a day. He is a sales executive and describes his work as stressful. Today, the blood pressure is 142/85 and the body mass index (BMI) is 28.5 kg/m2. A coronary angiogram shows > 75% narrowing of the left anterior descending coronary artery. Which of the following is most significant in this patient?
- A. Obesity
- B. Family history
- C. Hypertension
- D. Smoking
- E. Diabetes mellitus (Correct Answer)
Cardiac imaging modalities Explanation: ***Diabetes mellitus***
- **Diabetes mellitus** is a significant risk factor for **atherosclerosis** and contributes to accelerated progression of **coronary artery disease (CAD)**, often leading to more widespread and severe disease.
- Poorly controlled diabetes can cause **endothelial dysfunction**, increasing oxidative stress and inflammation, which are key processes in **plaque formation** and destabilization.
*Obesity*
- **Obesity** (BMI 28.5 kg/m2) is a risk factor for **CAD** but often acts through associated conditions like **hypertension**, **diabetes**, and **dyslipidemia**.
- While it contributes to overall cardiovascular risk, it is less directly pathogenic than diabetes which independently accelerates **atherosclerosis**.
*Family history*
- The patient's father had a **heart attack at 41**, which is a significant risk factor for **early-onset CAD**.
- However, the patient has multiple modifiable risk factors (smoking, hypertension, diabetes) that are independently and more directly contributing to his current presentation.
*Hypertension*
- **Hypertension** (142/85 mmHg) is a major modifiable risk factor that causes **endothelial damage** and promotes **atherosclerosis**.
- While important, the patient's **poorly controlled diabetes mellitus** often creates a more aggressive environment for plaque formation and progression compared to hypertension alone.
*Smoking*
- **Smoking** is a potent, modifiable risk factor that causes direct vascular injury, promotes **thrombogenesis**, and contributes to **atherosclerosis**.
- Although highly detrimental, smoking is one of several significant risk factors; **diabetes mellitus**, with its systemic metabolic impact, can be considered more broadly influential in the severity and diffuse nature of **CAD**.
Cardiac imaging modalities US Medical PG Question 3: A 54-year-old woman is diagnosed with locally-advanced invasive ductal carcinoma of the breast. She undergoes surgical resection, radiation therapy, and is now being started on adjunctive chemotherapy with cyclophosphamide and doxorubicin. The patient is scheduled for follow up by her primary care provider. Which of the following tests should be performed regularly to monitor her current treatment regimen?
- A. No regular monitoring indicated
- B. Chest radiograph
- C. Cardiac MRI
- D. ECG
- E. Echocardiography (Correct Answer)
Cardiac imaging modalities Explanation: ***Echocardiography***
- **Doxorubicin** is an anthracycline chemotherapy agent known for its dose-dependent **cardiotoxicity**, which can lead to **dilated cardiomyopathy** and heart failure.
- Regular echocardiography is crucial to monitor **left ventricular ejection fraction (LVEF)** and detect early signs of cardiac dysfunction, allowing for timely intervention or adjustment of treatment.
*No regular monitoring indicated*
- This is incorrect as **doxorubicin**, a component of the chemotherapy regimen, has significant cardiotoxic effects that require close monitoring to prevent severe cardiac complications.
- Neglecting monitoring could lead to irreversible cardiac damage.
*Chest radiograph*
- A chest radiograph primarily assesses lung fields and cardiac silhouette, but it is not sensitive enough to detect early-stage **doxorubicin-induced myocardial damage** or changes in **LVEF**.
- While useful for detecting pulmonary complications or metastases, it is not the primary tool for monitoring cardiotoxicity.
*Cardiac MRI*
- Cardiac MRI is a highly sensitive and specific imaging modality for assessing cardiac function and structure, but it is typically reserved for cases where echocardiography findings are equivocal or more detailed assessment is needed.
- It is not the routine or initial test for monitoring cardiotoxicity due to its higher cost and complexity.
*ECG*
- An ECG assesses the electrical activity of the heart and can detect arrhythmias or signs of ischemia, but it is generally not sufficient for monitoring **doxorubicin-induced cardiotoxicity**.
- While it can show nonspecific changes, it does not directly measure changes in **LVEF** or structural heart damage, which are key indicators of cardiotoxicity.
Cardiac imaging modalities US Medical PG Question 4: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
Cardiac imaging modalities Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
Cardiac imaging modalities US Medical PG Question 5: A 79-year-old woman with type 2 diabetes mellitus and hypertension undergoes 99mTc cardiac scintigraphy for the evaluation of a 3-month history of retrosternal chest tightness on exertion. The patient's symptoms are reproduced following the administration of dipyridamole. A repeat ECG shows new ST depression and T wave inversion in leads V5 and V6. Which of the following is the most likely underlying mechanism of this patient's signs and symptoms during the procedure?
- A. Dilation of coronary vasculature
- B. Ruptured cholesterol plaque within a coronary vessel
- C. Increased myocardial oxygen demand
- D. Reduced left ventricular preload
- E. Coronary steal phenomenon (Correct Answer)
Cardiac imaging modalities Explanation: ***Correct: Coronary steal phenomenon***
- **Dipyridamole** is a **coronary vasodilator** that preferentially dilates **healthy coronary arteries** with intact endothelium and normal vasodilatory capacity.
- In patients with **coronary artery stenosis**, the vessels distal to the stenosis are already maximally dilated at baseline due to autoregulation.
- When dipyridamole causes further vasodilation of healthy vessels, blood flow is redistributed **away from** the ischemic areas supplied by stenotic vessels toward the healthy myocardium—this is the **"steal" phenomenon**.
- The patient's **ST depression and T wave inversion** in V5-V6 indicate lateral wall ischemia due to this maldistribution of coronary blood flow, not from increased oxygen demand.
- This mechanism makes dipyridamole useful for **pharmacologic stress testing** in patients who cannot exercise, as it reveals flow-limiting coronary stenoses without increasing heart rate or contractility.
*Incorrect: Increased myocardial oxygen demand*
- This is the mechanism of **exercise stress testing** or **dobutamine stress testing**, which increase heart rate, contractility, and blood pressure.
- **Dipyridamole does NOT increase myocardial oxygen demand**—it is a pure vasodilator that does not have positive inotropic or chronotropic effects.
- The ischemia induced by dipyridamole is due to **supply maldistribution** (steal), not increased demand.
- This distinction is clinically important: dipyridamole is chosen for patients who cannot exercise precisely because it avoids increasing cardiac workload.
*Incorrect: Ruptured cholesterol plaque within a coronary vessel*
- This describes the pathophysiology of **acute coronary syndrome (ACS)**, including unstable angina, NSTEMI, or STEMI.
- ACS typically presents with **sudden-onset chest pain at rest**, prolonged symptoms, and more dramatic ECG changes (ST elevation or deep T wave inversions).
- This patient has **chronic stable angina** with reproducible exertional symptoms over 3 months, and the ECG changes occurred during a controlled stress test—not consistent with acute plaque rupture.
*Incorrect: Dilation of coronary vasculature*
- While dipyridamole does cause **coronary vasodilation**, this is not itself the mechanism of ischemia—it's the **differential** vasodilation that causes the problem.
- The phrase "dilation of coronary vasculature" describes the drug's action but not the pathophysiologic consequence.
- The specific mechanism by which this vasodilation causes ischemia is the **coronary steal phenomenon**, making that the more precise and complete answer.
*Incorrect: Reduced left ventricular preload*
- Dipyridamole can cause mild systemic vasodilation and slight reduction in preload, but this is **not the mechanism of myocardial ischemia** in this case.
- Reduced preload typically causes symptoms of **hypotension** (lightheadedness, dizziness) rather than ischemic chest pain and ST-T wave changes.
- The **lateral wall ischemia** pattern (V5-V6) indicates regional myocardial oxygen supply-demand mismatch due to coronary artery disease, not a global reduction in preload.
Cardiac imaging modalities US Medical PG Question 6: A 58-year-old man presents to the emergency department for evaluation of intermittent chest pain over the past 6 months. His history reveals that he has had moderate exertional dyspnea and 2 episodes of syncope while working at his factory job. These episodes of syncope were witnessed by others and lasted roughly 30 seconds. The patient states that he did not have any seizure activity. His vital signs include: blood pressure 121/89 mm Hg, heart rate 89/min, temperature 37.0°C (98.6°F), and respiratory rate 16/min. Physical examination reveals a crescendo-decrescendo systolic murmur in the right second intercostal area. An electrocardiogram is performed, which shows left ventricular hypertrophy. Which of the following is the best next step for this patient?
- A. Transthoracic echocardiography (Correct Answer)
- B. Chest radiograph
- C. Computed tomography (CT) chest scan without contrast
- D. Cardiac chamber catheterization
- E. Transesophageal echocardiography
Cardiac imaging modalities Explanation: ***Transthoracic echocardiography***
- The patient's symptoms (chest pain, exertional dyspnea, syncope) and physical exam findings (**crescendo-decrescendo systolic murmur at the right second intercostal space**, ECG showing **left ventricular hypertrophy**) are highly suggestive of **aortic stenosis**.
- **Transthoracic echocardiography** is the gold standard for diagnosing and assessing the severity of valvular heart diseases like aortic stenosis, quantifying valve area, pressure gradients, and ventricular function.
*Chest radiograph*
- A chest radiograph provides information about lung fields, cardiac size, and aortic calcification, but it cannot directly visualize or assess the function of heart valves.
- While it may show signs of heart failure (e.g., **pulmonary congestion**) or **cardiomegaly**, it is insufficient for a definitive diagnosis or severity assessment of valvular lesions.
*Computed tomography (CT) chest scan without contrast*
- A CT scan can detect calcification of the aortic valve, but it is not the primary imaging modality for assessing valvular function or the severity of stenotic lesions.
- CT is more useful for evaluating the **aorta for aneurysm** or dissection, or for **pulmonary pathology**, neither of which is the most likely diagnosis given the presenting symptoms.
*Cardiac chamber catheterization*
- Cardiac catheterization is an **invasive procedure** that is typically reserved for cases where non-invasive imaging is inconclusive or when planning for intervention (e.g., prior to valve replacement).
- It involves risks and is not the initial best step for diagnosis when a less invasive and highly informative test like echocardiography is available.
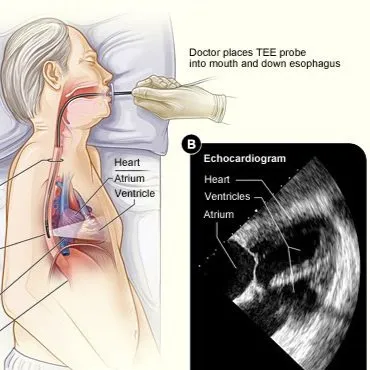
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** provides more detailed images of the heart and valves compared to TTE because it avoids acoustic shadowing from the ribs and lungs.
- However, TEE is more invasive than TTE and is usually reserved for situations where TTE is inadequate or when a higher resolution view is needed, such as for infective endocarditis, prosthetic valve dysfunction, or before/during surgical procedures.
Cardiac imaging modalities US Medical PG Question 7: A 62-year-old man with a past medical history of previous myocardial infarction, angina, hypertension, hyperlipidemia, diabetes mellitus, peripheral vascular disease, and below knee amputation has developed new chest pain. His medication includes insulin, hydrochlorothiazide, lisinopril, metoprolol, daily aspirin, atorvastatin, and nitroglycerin as needed. His vitals include: blood pressure 135/87 mm Hg, pulse 52/min, and respirations 17/min. Coronary arteriography shows a reduced ejection fraction, a 65% stenosis of the left anterior descending artery, and a 75% stenosis of the left circumflex artery. Which of the following is the recommended treatment for the patient?
- A. Increased beta blocker dosage
- B. Coronary artery bypass grafting (CABG) (Correct Answer)
- C. Angioplasty with stent placement
- D. Extended release nitrate therapy
- E. Heparin
Cardiac imaging modalities Explanation: ***Coronary artery bypass grafting (CABG)***
- This patient has complex **multivessel coronary artery disease** (LAD and circumflex stenosis) with a **reduced ejection fraction** and a history of multiple comorbidities, making CABG the preferred revascularization strategy for improved outcomes.
- CABG offers a more complete revascularization in patients with significant disease burden and reduced left ventricular function, leading to better long-term survival and symptom relief compared to PCI in this population.
*Increased beta blocker dosage*
- The patient's current heart rate is 52/min, which is already at the lower end of the target range for beta-blocker therapy in cardiac patients, and further increasing the dose could lead to **bradycardia** and worsening symptoms.
- While beta-blockers are crucial for managing angina and improving outcomes post-MI, increasing the dose wouldn't address the underlying anatomical severe multi-vessel coronary artery disease.
*Angioplasty with stent placement*
- Although PCI (angioplasty with stent placement) can be used for coronary stenosis, in patients with **multivessel disease**, **reduced ejection fraction**, and **diabetes mellitus**, CABG generally offers superior long-term results and survival benefits.
- The complexity of the lesions (65% LAD, 75% circumflex) in a patient with significant comorbidities and extensive atherosclerotic disease makes PCI a less optimal choice here.
*Extended release nitrate therapy*
- Nitrates primarily provide **symptomatic relief** by causing vasodilation, but they do not address the severe underlying coronary stenoses or improve long-term outcomes in patients with complex, multivessel disease.
- The patient is already on PRN nitroglycerin, and while extended-release nitrates could help with angina, they are not a definitive treatment for significant arterial blockages requiring revascularization.
*Heparin*
- Heparin is an **anticoagulant** that may be used as part of initial management of acute coronary syndromes, but it provides only temporary stabilization and does not address the **definitive need for revascularization**.
- While anticoagulation plays a role in acute management, this patient requires **definitive anatomical correction** of his multivessel disease with significant stenoses, which only surgical or percutaneous revascularization can provide, with CABG being superior given his clinical profile.
Cardiac imaging modalities US Medical PG Question 8: A 69-year-old man is scheduled to undergo radical retropubic prostatectomy for prostate cancer in 2 weeks. He had a myocardial infarction at the age of 54 years. He has a history of GERD, unstable angina, hyperlipidemia, and severe osteoarthritis in the left hip. He is unable to climb up stairs or walk fast because of pain in his left hip. He had smoked one pack of cigarettes daily for 30 years but quit 25 years ago. He drinks one glass of wine daily. Current medications include aspirin, metoprolol, lisinopril, rosuvastatin, omeprazole, and ibuprofen as needed. His temperature is 36.4°C (97.5°F), pulse is 90/min, and blood pressure is 136/88 mm Hg. Physical examination shows no abnormalities. A 12-lead ECG shows Q waves and inverted T waves in leads II, III, and aVF. His B-type natriuretic protein is 84 pg/mL (N < 125). Which of the following is the most appropriate next step in management to assess this patient's perioperative cardiac risk?
- A. No further testing
- B. 24-hour ambulatory ECG monitoring
- C. Radionuclide myocardial perfusion imaging (Correct Answer)
- D. Treadmill stress test
- E. Resting echocardiography
Cardiac imaging modalities Explanation: ***Radionuclide myocardial perfusion imaging***
- This patient requires **perioperative cardiac risk assessment** before intermediate-risk surgery (radical prostatectomy).
- Key factors include: history of **myocardial infarction**, current cardiac risk factors, and **inability to exercise** due to severe osteoarthritis.
- Since he cannot perform exercise stress testing, **pharmacologic stress testing** with radionuclide myocardial perfusion imaging (using agents like adenosine, dipyridamole, or regadenoson) is the most appropriate test to assess for **inducible myocardial ischemia**.
- This provides functional assessment of coronary perfusion under pharmacologic stress, helping guide perioperative risk stratification and management.
- *Note: The presence of unstable angina would typically require cardiac stabilization first; this question focuses on selecting the appropriate stress test modality for a patient unable to exercise.*
*No further testing*
- This patient has significant cardiac risk factors including **prior MI**, ongoing cardiac medications, and ECG changes suggesting old infarction.
- Proceeding directly to surgery without functional cardiac assessment would be **inappropriate** given his risk profile and the intermediate-risk nature of the planned surgery.
*24-hour ambulatory ECG monitoring*
- Holter monitoring detects arrhythmias and silent ischemic episodes but does not provide **functional capacity assessment** or evaluation of inducible ischemia under stress conditions.
- It is not the primary tool for **perioperative cardiac risk stratification** before major surgery.
*Treadmill stress test*
- The patient's **severe osteoarthritis** prevents him from climbing stairs or walking fast, making him unable to achieve adequate exercise workload for a treadmill stress test.
- This functional limitation makes **exercise stress testing contraindicated**; pharmacologic stress testing is required instead.
*Resting echocardiography*
- Resting echocardiography assesses **baseline left ventricular function**, wall motion abnormalities from prior infarction, and valvular disease.
- While useful for structural assessment, it does **not evaluate for exercise-induced or stress-induced ischemia**, which is critical for perioperative risk assessment in patients with coronary artery disease.
- His normal BNP (84 pg/mL) suggests adequate baseline ventricular function, making functional ischemia assessment more relevant than structural evaluation alone.
Cardiac imaging modalities US Medical PG Question 9: A 35-year-old woman with a medical history significant for asthma, hypertension, and occasional IV drug use comes to the emergency department with fever. On physical exam, there are findings depicted in figure A, for which the patient cannot account. What test will be most helpful to establish the diagnosis?
- A. Echocardiography (Correct Answer)
- B. Electrocardiogram (EKG)
- C. Chest X-ray
- D. CT pulmonary angiography
- E. Pulmonary function tests
Cardiac imaging modalities Explanation: ***Echocardiography***
- The image depicts signs consistent with **septic emboli**, specifically **Janeway lesions** (painless, hemorrhagic macules on palms/soles) and potentially **Osler nodes** (painful nodules) or **splinter hemorrhages** (linear hemorrhages under nails), all highly suggestive of **infective endocarditis** in an IV drug user with fever.
- **Echocardiography** is crucial for visualizing **vegetations** on heart valves, assessing valve damage, and detecting complications like abscesses or emboli source, making it the most diagnostic test for infective endocarditis.
*Electrocardiogram (EKG)*
- An EKG may show cardiac arrhythmias or conduction abnormalities, but it does not directly visualize vegetations or valvular damage definitive for endocarditis.
- While it can be part of the initial workup for cardiac symptoms, it's not the primary diagnostic tool for infective endocarditis.
*Chest X-ray*
- A chest X-ray can reveal signs of pulmonary involvement, such as **septic pulmonary emboli** (if right-sided endocarditis is present), but it cannot directly diagnose infective endocarditis itself or visualize the heart valves.
- It would not show the vegetations or structural heart changes characteristic of the disease.
*CT pulmonary angiography*
- This test is primarily used to diagnose **pulmonary embolism**, which is a possible complication of right-sided endocarditis.
- However, it does not confirm the presence of endocarditis or identify vegetations on heart valves.
*Pulmonary function tests*
- Pulmonary function tests assess lung function and are relevant for conditions like asthma or other respiratory diseases, but they are not indicated for the diagnosis of infective endocarditis.
- They provide no diagnostic information regarding cardiac vegetations or systemic emboli.
Cardiac imaging modalities US Medical PG Question 10: A 75-year-old man comes to the physician because of a 4-month history of progressive shortness of breath and chest pressure with exertion. Cardiac examination shows a crescendo-decrescendo systolic murmur that is heard best in the second right intercostal space. Radial pulses are decreased and delayed bilaterally. Transesophageal echocardiography shows hypertrophy of the left ventricle and a thick, calcified aortic valve. The area of the left ventricular outflow tract is 30.6 mm2. Using continuous-wave Doppler measurements, the left ventricular outflow tract velocity is 1.0 m/s, and the peak aortic valve velocity is 3.0 m/s. Which of the following values most closely represents the area of the stenotic aortic valve?
- A. 16.0 mm2
- B. 23 mm2
- C. 10.2 mm2 (Correct Answer)
- D. 2.0 mm2
- E. 6.2 mm2
Cardiac imaging modalities Explanation: ***10.2 mm2***
- This value is calculated using the **continuity equation**, which states that the product of the area and velocity at one point in a tube must equal the product of the area and velocity at another point. The formula is: A1 × V1 = A2 × V2, where A1 is the **left ventricular outflow tract (LVOT) area**, V1 is the **LVOT velocity**, A2 is the **aortic valve area (AVA)**, and V2 is the **peak aortic valve velocity**.
- Using the given values: 30.6 mm² × 1.0 m/s = A2 × 3.0 m/s. Solving for A2 gives A2 = (30.6 × 1.0) / 3.0 = **10.2 mm²** (approximately **0.1 cm²**).
- A normal aortic valve area is generally > 2.0 cm² (200 mm²). Severe stenosis is defined as ≤ 1.0 cm² (100 mm²), and this calculated value of 0.1 cm² represents **critical aortic stenosis**, consistent with the patient's symptoms and physical examination findings.
*16.0 mm2*
- This value would be obtained if there was an error in calculation or if one of the velocity or area measurements was significantly different. It does not fit the continuity equation with the given parameters.
- It suggests a higher aortic valve area than calculated, despite the clinical presentation and other measurements pointing towards critical stenosis.
*23 mm2*
- This value is significantly higher than the calculated aortic valve area and would suggest a less severe degree of stenosis than indicated by the patient's symptoms and other findings.
- An error in applying the continuity equation or using incorrect values for velocity or area would lead to this result.
*2.0 mm2*
- This value indicates **extremely severe/critical aortic stenosis** beyond what is calculated. While the patient does have critical stenosis, the continuity equation with the provided data yields 10.2 mm², not 2.0 mm².
- This would imply a much greater velocity ratio or different LVOT measurements than observed.
*6.2 mm2*
- While indicating very severe stenosis, this value is lower than what the continuity equation yields with the given data.
- This result suggests a potential calculation error or misinterpretation of the provided velocities and areas.
More Cardiac imaging modalities US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.