Aortic diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Aortic diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Aortic diseases US Medical PG Question 1: A 62-year-old man is brought to the emergency department with a sudden onset of severe chest pain, that he describes as tearing. The pain started 90 minutes back and is now referring to the upper back. There is a history of essential hypertension for the past 17 years. The patient has smoked 20–30 cigarettes daily for the past 27 years. Vital signs reveal: temperature 36.8°C (98.2°F), heart rate 105/min, and blood pressure 192/91 mm Hg in the right arm and 159/81 mm Hg in the left arm. Pulses are absent in the right leg and diminished in the left. ECG shows sinus tachycardia, and chest X-ray shows a widened mediastinum. Transthoracic echocardiography shows an intimal flap arising from the ascending aorta and extended to the left subclavian artery. Intravenous morphine sulfate is started. Which of the following is the best next step in the management of this patient condition?
- A. Intravenous metoprolol (Correct Answer)
- B. Intravenous hydralazine
- C. Chest magnetic resonance imaging
- D. Oral aspirin
- E. D-dimer
Aortic diseases Explanation: ***Intravenous metoprolol***
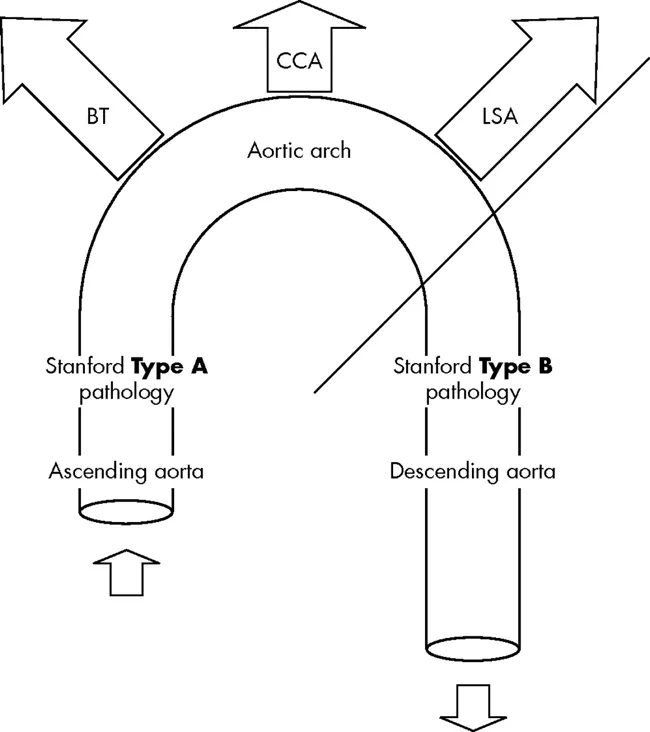
- This patient presents with an **acute aortic dissection** (type A given the involvement of the ascending aorta), which is a medical emergency requiring immediate management to reduce stress on the aorta and prevent rupture.
- **Beta-blockers** like metoprolol are the **first-line therapy** to rapidly **lower heart rate** and **blood pressure**, thereby reducing the shear stress on the aortic wall and limiting the propagation of the dissection.
*Intravenous hydralazine*
- Hydralazine is a direct **vasodilator** that can cause **reflex tachycardia**, which would increase the shear stress on the dissected aorta and worsen the condition.
- While it lowers blood pressure, it does not address the crucial need to reduce heart rate and myocardial contractility in aortic dissection.
*Chest magnetic resonance imaging*
- While MRI can provide detailed imaging of aortic dissection, the **diagnosis is already confirmed** by transthoracic echocardiography showing the intimal flap.
- Further diagnostic imaging is **not the priority**; immediate **medical stabilization** with beta-blockade to reduce aortic stress is the essential next step before considering definitive surgical management.
- MRI is also **time-consuming** and generally avoided in unstable patients requiring urgent intervention.
*Oral aspirin*
- Aspirin is an **antiplatelet agent** primarily used to prevent arterial thrombosis in conditions like myocardial infarction or stroke.
- It is **not indicated** for the acute management of aortic dissection and would not address the immediate hemodynamic goals of reducing heart rate and blood pressure.
*D-dimer*
- **D-dimer** is a marker of fibrin degradation products used as a screening tool for conditions like **pulmonary embolism** or deep vein thrombosis.
- While an elevated D-dimer can be seen in aortic dissection, it is a **non-specific test** and is not the best next step in immediate management, especially when the **diagnosis is already confirmed** by echocardiography.
Aortic diseases US Medical PG Question 2: A 24-year-old man presents with a complaint of breathlessness while jogging. He says that he recently started marathon training. He does not have any family history of asthma nor has any allergies. He currently takes no medication. The blood pressure is 120/80 mm Hg, and the heart rate is 67/min. With each heartbeat, he experiences pounding in his chest, and his head bobs. On physical examination, he has long fingers, funnel chest, and disproportionate body proportions with a decreased upper-to-lower segment ratio. On auscultation over the 2nd right intercostal space, an early diastolic murmur is heard, and 3rd and 4th heart sounds are heard. Echocardiography shows aortic root dilatation. The patient is scheduled for surgery. Which of the following is associated with this patient's condition?
- A. Klinefelter syndrome
- B. Intravenous drug abuse
- C. Marfan's Syndrome (Correct Answer)
- D. Kawasaki syndrome
- E. Gonorrhea
Aortic diseases Explanation: ***Marfan's Syndrome***
- The patient presents with **tall stature**, **long fingers (arachnodactyly)**, **funnel chest (pectus excavatum)**, and **aortic root dilation** with **aortic regurgitation** (early diastolic murmur, head bobbing, pounding in the chest), all classic features of Marfan syndrome.
- This is a **connective tissue disorder** caused by a mutation in the **FBN1 gene**, leading to defective **fibrillin-1**, which is crucial for structural integrity in the heart, blood vessels, eyes, and skeleton.
*Klinefelter syndrome*
- Characterized by a **47, XXY karyotype** and typically presents with infertility, small testes, gynecomastia, and tall stature, but not the specific cardiovascular or skeletal features described.
- While it can cause tall stature, it does not explain the **arachnodactyly**, **pectus excavatum**, or the severe **aortic root dilation** and regurgitation.
*Intravenous drug abuse*
- Primarily associated with **infective endocarditis**, particularly affecting the **tricuspid valve**, leading to heart murmurs related to infection, not the skeletal and aortic root abnormalities seen here.
- This history would lead to a different clinical presentation, potentially involving fever, chills, and vegetations on valve leaflets, none of which are mentioned.
*Kawasaki syndrome*
- An **acute inflammatory vasculitis** primarily affecting young children, characterized by fever, rash, conjunctivitis, lymphadenopathy, and oral mucosal changes.
- While it can cause **coronary artery aneurysms**, it does not explain the skeletal abnormalities or the specific presentation of aortic root dilation with regurgitation in an adult.
*Gonorrhea*
- A **sexually transmitted infection** that can lead to disseminated gonococcal infection, causing arthritis, tenosynovitis, and dermatitis.
- It does not cause the specific skeletal abnormalities or the primary cardiac pathology of aortic root dilation and regurgitation described in this patient.
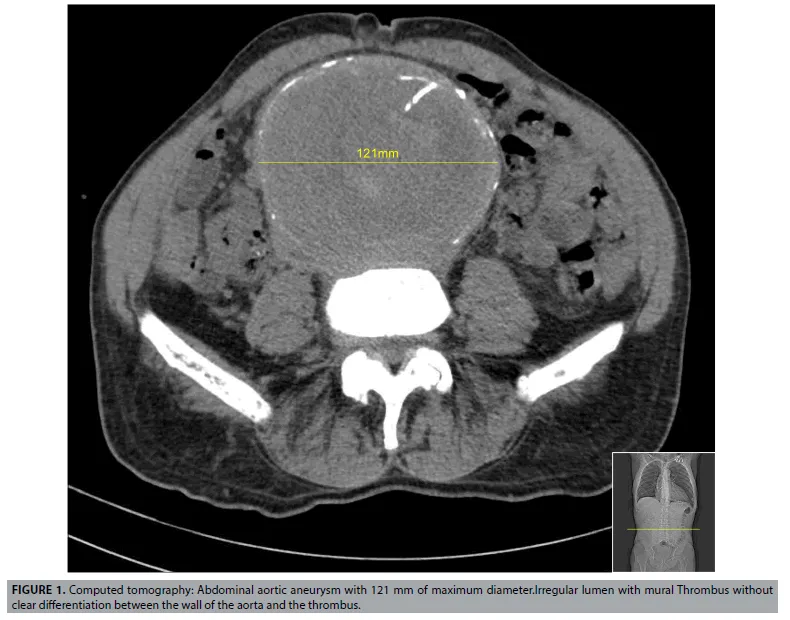
Aortic diseases US Medical PG Question 3: A 75-year-old Caucasian man presents to the emergency department with abdominal pain. The patient states he was at home eating dinner when he began to experience severe abdominal pain. The patient has a past medical history of diabetes, hypertension, and atherosclerosis. He lives at home alone, smokes cigarettes, and drinks 1 to 2 alcoholic drinks per day. The patient is given IV morphine and an ultrasound is obtained demonstrating a dilated abdominal aorta. The patient states that his father died of a similar finding and is concerned about his prognosis. Which of the following is the greatest risk factor for this patient's presentation?
- A. Male gender and age
- B. Caucasian race
- C. Cigarette smoking (Correct Answer)
- D. Family history
- E. Atherosclerosis
Aortic diseases Explanation: ***Cigarette smoking***
- **Cigarette smoking** is the most significant modifiable risk factor for the development and expansion of **abdominal aortic aneurysms (AAAs)**, directly contributing to vascular inflammation and degradation.
- The patient's history of smoking suggests a strong causal link to his current presentation of a dilated aorta, which is highly indicative of an AAA.
*Male gender and age*
- While **male gender** and **advanced age (over 65)** are significant demographic risk factors for AAA, they are considered non-modifiable and less impactful than smoking in terms of risk magnitude.
- These factors increase predisposition but do not exert the same direct, damaging effect on the arterial wall as chronic smoking.
*Caucasian race*
- **Caucasian race** is a known demographic risk factor for AAA, with higher prevalence rates compared to other ethnic groups.
- However, this is a non-modifiable genetic predisposition and contributes less to the overall risk than modifiable lifestyle factors like smoking.
*Family history*
- A **family history** of AAA, as suggested by the patient's father having a similar condition, increases an individual's susceptibility.
- This is a significant non-modifiable risk factor, indicating genetic predisposition, but its overall impact on aneurysm formation and progression is typically less than that of active smoking.
*Atherosclerosis*
- **Atherosclerosis** is a strong associated condition with AAA, as both share common risk factors and pathology related to arterial wall degeneration.
- While atherosclerosis contributes to the overall vascular compromise, smoking specifically has a more direct and potent effect on promoting aneurysm formation and rupture independently.
Aortic diseases US Medical PG Question 4: A 32-year-old woman who recently emigrated to the USA from Japan comes to the physician because of a 3-month history of night sweats, malaise, and joint pain. During this time, she has also had a 6-kg (13-lb) weight loss. Physical examination shows weak brachial and radial pulses. There are tender subcutaneous nodules on both legs. Carotid bruits are heard on auscultation bilaterally. Laboratory studies show an erythrocyte sedimentation rate of 96 mm/h. A CT scan of the chest shows thickening and narrowing of the aortic arch. Microscopic examination of the aortic arch is most likely to show which of the following findings?
- A. Fibrinoid necrosis of the intima and media
- B. Calcification of the media
- C. Granulomatous inflammation of the media (Correct Answer)
- D. Subendothelial hyaline deposition
- E. Subendothelial immune complex deposition
Aortic diseases Explanation: ***Granulomatous inflammation of the media***
- The clinical presentation, including **night sweats, malaise, weight loss, weak brachial and radial pulses** (pulseless disease), and **thickening and narrowing of the aortic arch**, is highly suggestive of **Takayasu arteritis**.
- **Takayasu arteritis** is a **large-vessel vasculitis** characterized pathologically by **granulomatous inflammation** primarily affecting the **tunica media** of the aorta and its major branches.
*Fibrinoid necrosis of the intima and media*
- **Fibrinoid necrosis** is typically seen in **small-to-medium vessel vasculitides** (e.g., polyarteritis nodosa) or in severe **hypertensive vasculopathy**.
- It involves the deposition of **fibrin-like material** in the vessel wall, which is not the primary histological feature of Takayasu arteritis.
*Calcification of the media*
- **Medial calcification** (Mönckeberg arteriosclerosis) primarily affects **muscular arteries** and is typically seen in older individuals, often incidentally.
- It does not cause significant luminal narrowing, inflammation, or the systemic symptoms described in this patient.
*Subendothelial hyaline deposition*
- **Hyaline deposition** in the subendothelium is characteristic of **hyaline arteriolosclerosis**, commonly seen in **benign hypertension** or **diabetes mellitus**, affecting small arteries and arterioles.
- This finding is not consistent with the specific large-vessel inflammatory process seen in Takayasu arteritis.
*Subendothelial immune complex deposition*
- **Immune complex deposition** in the subendothelium is typical of **Type III hypersensitivity reactions**, such as those seen in **lupus nephritis** or **Type II cryoglobulinemia**, often affecting glomeruli or small vessels.
- While Takayasu arteritis is immune-mediated, its hallmark is **granulomatous inflammation**, not primary immune complex deposition in the vessel wall.
Aortic diseases US Medical PG Question 5: A 65-year-old man with hypertension and type 2 diabetes mellitus is brought to the emergency department 20 minutes after the onset of severe anterior chest pain and shortness of breath. He has smoked one pack of cigarettes daily for 30 years. He appears distressed. His pulse is 116/min, respirations are 22/min, and blood pressure is 156/88 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. A grade 3/6, high-pitched, blowing, diastolic murmur is heard over the right upper sternal border. Which of the following is the most likely cause of this patient's symptoms?
- A. Rupture of a bulla in the lung
- B. Perforation of the esophageal wall
- C. Obstruction of the pulmonary arteries
- D. Fibrofatty plaque in the aortic wall
- E. Tear in the tunica intima (Correct Answer)
Aortic diseases Explanation: ***Tear in the tunica intima***
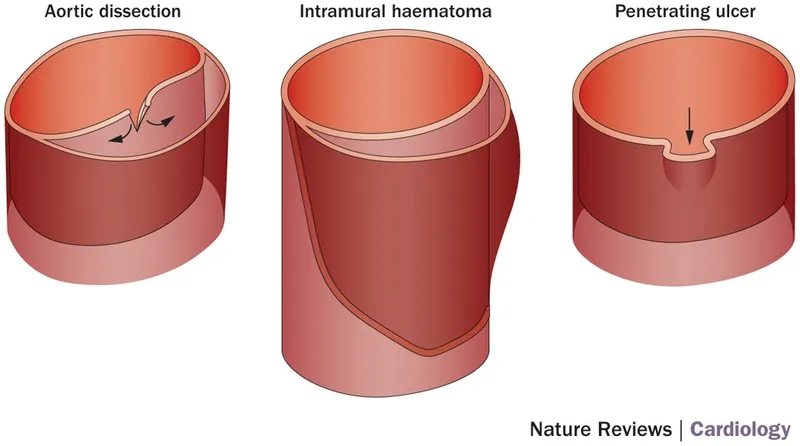
- The sudden onset of **severe anterior chest pain**, hypertension, and a **diastolic murmur** consistent with **aortic insufficiency** points strongly to an **aortic dissection**, which begins with a tear in the tunica intima.
- Risk factors like **hypertension**, **smoking**, and **advanced age** increase the likelihood of aortic dissection.
*Rupture of a bulla in the lung*
- This would typically cause **pneumothorax**, leading to **sharp, pleuritic chest pain** and **dyspnea**, often with diminished breath sounds on the affected side.
- A **cardiac murmur** and severe distress in the context of vascular risk factors are not characteristic of a ruptured bulla.
*Perforation of the esophageal wall*
- Esophageal perforation (Boerhaave syndrome) presents with **severe chest pain**, **vomiting**, and often **subcutaneous emphysema** or **pleural effusion**.
- While it causes severe chest pain, the described **diastolic murmur** and absence of vomiting or other specific signs make this less likely.
*Obstruction of the pulmonary arteries*
- **Pulmonary embolism** (obstruction of pulmonary arteries) typically causes **sudden onset dyspnea**, **pleuritic chest pain**, **tachycardia**, and **hypoxia**, often without a significant cardiac murmur of this nature.
- The oxygen saturation of 98% makes a large pulmonary embolism less probable.
*Fibrofatty plaque in the aortic wall*
- While common in patients with hypertension and smoking history, an **atherosclerotic plaque** in the aortic wall itself rarely causes acute, severe chest pain and a new diastolic murmur unless it leads to an **aortic dissection** or **rupture**.
- This option describes a precursor to diseases like aortic dissection but not the acute event itself.
Aortic diseases US Medical PG Question 6: A previously healthy 32-year-old man comes to the physician because of a 1-week history of upper back pain, dyspnea, and a sensation of pressure in his chest. He has had no shortness of breath, palpitations, fevers, or chills. He emigrated from Ecuador when he was 5 years old. He does not smoke or drink alcohol. He takes no medications. He is 194 cm (6 ft 4 in) tall and weighs 70.3 kg (155 lb); BMI is 19 kg/m2. His temperature is 37.2°C (99.0°F), pulse is 73/min, respirations are 15/min, and blood pressure is 152/86 mm Hg in the right arm and 130/72 mm Hg in the left arm. Pulmonary examination shows faint inspiratory wheezing bilaterally. A CT scan of the chest with contrast is shown. Which of the following is the most likely underlying cause of this patient's condition?
- A. Atherosclerotic plaque formation
- B. Large-vessel vasculitis
- C. Cystic medial necrosis (Correct Answer)
- D. Congenital narrowing of the aortic arch
- E. Infection with Trypanosoma cruzi
Aortic diseases Explanation: ***Cystic medial necrosis***
- The patient's tall stature, Marfanoid habitus (BMI 19 kg/m2), and differential blood pressures are highly suggestive of **Marfan syndrome**, which is primarily caused by **cystic medial necrosis** of the aorta.
- **Cystic medial necrosis** is a degenerative process in the aortic wall leading to loss of smooth muscle cells and elastic fibers, predisposing to **aortic dissection** or aneurysm, explaining the chest and back pain.
*Atherosclerotic plaque formation*
- This patient is young, has no traditional risk factors for atherosclerosis (e.g., smoking, obesity, diabetes), and **atherosclerosis** typically does not cause **aortic dissection** at this age in the absence of other risk factors.
- While atherosclerosis can cause aortic aneurysms, it is less likely to present with the acute pain and differential blood pressures seen here in a young, otherwise healthy individual.
*Large-vessel vasculitis*
- **Large-vessel vasculitis** (e.g., Takayasu arteritis) can cause differential blood pressures and aortic involvement, but it is less likely given the patient's presentation with acute pain and the strong clinical features of **Marfan syndrome**.
- Vasculitis would typically present with more systemic inflammatory signs and symptoms, which are absent in this case.
*Congenital narrowing of the aortic arch*
- **Coarctation of the aorta** is a congenital narrowing that can cause differential blood pressures and hypertension, but it would typically present earlier in life, often with signs of left ventricular hypertrophy, and is less likely to lead to acute aortic dissection or the Marfanoid habitus.
- The CT scan would show a distinct localized narrowing rather than the more diffuse aortic changes associated with connective tissue disorders.
*Infection with Trypanosoma cruzi*
- **Chagas disease** (caused by *Trypanosoma cruzi*) can cause **cardiomyopathy** and **megaesophagus/megacolon**, but it does not typically lead to acute aortic dissection or the specific connective tissue abnormalities seen in Marfan syndrome.
- While the patient emigrated from Ecuador, the clinical picture strongly points away from Chagasic aortopathy as the primary cause of his acute aortic symptoms.
Aortic diseases US Medical PG Question 7: A 58-year-old man presents to the emergency department with severe chest pain and uneasiness. He says that symptoms onset acutely half an hour ago while he was watching television. He describes the pain as being 8/10 in intensity, sharp in character, localized to the center of the chest and retrosternal, and radiating to the back and shoulders. The patient denies any associated change in the pain with breathing or body position. He says he has associated nausea but denies any vomiting. He denies any recent history of fever, chills, or chronic cough. His past medical history is significant for hypertension, hyperlipidemia, and diabetes mellitus for which he takes lisinopril, hydrochlorothiazide, simvastatin, and metformin. He reports a 30-pack-year smoking history and has 1–2 alcoholic drinks during the weekend. Family history is significant for hypertension, hyperlipidemia, and an ST elevation myocardial infarction in his father and paternal uncle. His blood pressure is 220/110 mm Hg in the right arm and 180/100 mm Hg in the left arm. On physical examination, the patient is diaphoretic. Cardiac exam reveals a grade 2/6 diastolic decrescendo murmur loudest over the left sternal border. Remainder of the physical examination is normal. The chest radiograph shows a widened mediastinum. The electrocardiogram (ECG) reveals non-specific ST segment and T wave changes. Intravenous morphine and beta-blockers are started. Which of the following is the most likely diagnosis in this patient?
- A. Pulmonary embolism
- B. Acute myocardial infarction
- C. Myocarditis
- D. Aortic regurgitation
- E. Aortic dissection (Correct Answer)
Aortic diseases Explanation: ***Aortic dissection***
- The patient's **sudden onset, sharp tearing chest pain radiating to the back** is the classic presentation of aortic dissection.
- The **blood pressure differential between arms** (220/110 mm Hg right vs 180/100 mm Hg left) is a highly specific finding indicating involvement of the brachiocephalic or subclavian arteries.
- The **diastolic decrescendo murmur** represents acute aortic regurgitation secondary to the dissection involving the aortic root.
- The **widened mediastinum on chest X-ray** is a key radiographic finding strongly suggestive of aortic dissection.
- Major risk factors present: **uncontrolled hypertension, smoking history, age, and atherosclerotic disease** (hyperlipidemia, diabetes).
*Pulmonary embolism*
- While PE can cause acute chest pain and dyspnea, the pain is typically **pleuritic in nature** (worsens with breathing or coughing).
- PE does not cause **blood pressure differentials between arms** or a **widened mediastinum**.
- The sharp, tearing quality radiating to the back is not characteristic of PE.
*Acute myocardial infarction*
- MI typically presents with **pressure-like or crushing chest pain**, often radiating to the left arm, jaw, or epigastrium rather than the back.
- While the patient has significant MI risk factors, the **unequal blood pressures between arms** and **diastolic murmur** are not explained by isolated MI.
- The **widened mediastinum** is not a feature of uncomplicated MI.
*Myocarditis*
- Myocarditis typically presents with **chest pain following a viral prodrome** (fever, URI symptoms), which this patient denies.
- It does not cause **blood pressure differentials**, **widened mediastinum**, or the acute tearing pain radiating to the back.
- Myocarditis pain is usually more constant and pressure-like, not sharp and tearing.
*Aortic regurgitation*
- While the **diastolic decrescendo murmur** indicates aortic regurgitation, this is a **finding rather than the primary diagnosis**.
- In this acute presentation, the AR is **secondary to aortic dissection** involving the aortic root.
- Chronic AR is typically asymptomatic until heart failure develops; acute severe AR (as in dissection) causes acute decompensation.
- The constellation of findings (acute pain, BP differential, widened mediastinum) indicates **aortic dissection as the primary catastrophic event** causing secondary AR.
Aortic diseases US Medical PG Question 8: A 55-year-old man presents to the emergency department for chest pain. He states that the pain started last night and has persisted until this morning. He describes the pain as in his chest and radiating into his back between his scapulae. The patient has a past medical history of alcohol abuse and cocaine abuse. He recently returned from vacation on a transatlantic flight. The patient has smoked 1 pack of cigarettes per day for the past 20 years. His temperature is 99.5°F (37.5°C), blood pressure is 167/118 mmHg, pulse is 120/min, and respirations are 22/min. Physical exam reveals tachycardia and clear air movement bilaterally on cardiopulmonary exam. Which of the following is also likely to be found in this patient?
- A. Pulmonary artery thrombus
- B. Coronary artery thrombus
- C. Elevated lipase
- D. Asymmetric blood pressures in the upper extremities (Correct Answer)
- E. Coronary artery vasospasm
Aortic diseases Explanation: ***Asymmetric blood pressures in the upper extremities***
- The patient's presentation with **sudden-onset, severe, tearing chest pain radiating to the back**, combined with **hypertension** and **tachycardia**, is highly suggestive of an **aortic dissection**. Asymmetric blood pressures are a classic sign.
- Aortic dissection involves a tear in the intima of the aorta, leading to a false lumen that can compress branch arteries, causing **pulse deficits** or **limb ischemia**, resulting in pressure differences.
*Pulmonary artery thrombus*
- While a **transatlantic flight** is a risk factor for **pulmonary embolism (PE)**, the described chest pain is typically pleuritic and not usually severe or radiating to the back in this manner.
- PE often presents with **dyspnea** and **hypoxia**, which are not prominent features described here.
*Coronary artery thrombus*
- **Cocaine abuse**, **smoking**, and **hypertension** are risk factors for **myocardial infarction (MI)** due to **coronary artery thrombosis**. However, MI pain is typically crushing or constricting, and radiation to the back between the scapulae is less common than in dissection.
- The description of **tearing pain** is more characteristic of aortic dissection than MI.
*Elevated lipase*
- The patient's history of **alcohol abuse** and **cocaine abuse** are risk factors for **pancreatitis**, which presents with elevated lipase. However, pancreatitis pain is typically **epigastric** and radiates to the back, but it's usually steady, severe, and often associated with nausea/vomiting, not the tearing quality described.
- The acute, severe, radiating chest pain pattern is not typical for an initial presentation of pancreatitis.
*Coronary artery vasospasm*
- **Cocaine abuse** is a known trigger for **coronary artery vasospasm**, leading to angina or MI, and can cause chest pain.
- However, the pain from vasospasm is usually anginal in quality, often responsive to nitrates, and less likely to present with the severe, tearing, interscapular back pain and hemodynamic instability suggestive of aortic dissection.
Aortic diseases US Medical PG Question 9: A 71-year old man is brought to the emergency department because of progressively worsening shortness of breath and fatigue for 3 days. During the last month, he has also noticed dark colored urine. He had an upper respiratory infection 6 weeks ago. He underwent a cholecystectomy at the age of 30 years. He has hypertension, hyperlipidemia, and type 2 diabetes mellitus. He immigrated to the US from Italy 50 years ago. Current medications include simvastatin, lisinopril, and metformin. He appears pale. His temperature is 37.1°C (98.8°F), pulse is 96/min, respirations are 21/min, and blood pressure is 150/80 mm Hg. Auscultation of the heart shows a grade 4/6 systolic murmur over the right second intercostal space that radiates to the carotids. Laboratory studies show:
Leukocyte count 9,000/mm3
Hemoglobin 8.3 g/dL
Hematocrit 24%
Platelet count 180,000/mm3
LDH 212 U/L
Haptoglobin 15 mg/dL (N=41–165)
Serum
Na+ 138 mEq/L
K+ 4.5 mEq/L
CL- 102 mEq/L
HCO3- 24 mEq/L
Urea nitrogen 20 mg/dL
Creatinine 1.2 mg/dL
Total bilirubin 1.8 mg/dL
Stool testing for occult blood is negative. Direct Coombs test is negative. Echocardiography shows an aortic jet velocity of 4.2 m/s and a mean pressure gradient of 46 mm Hg. Which of the following is the most appropriate next step in management to treat this patient's anemia?
- A. Aortic valve replacement (Correct Answer)
- B. Administration of corticosteroids
- C. Discontinuation of medication
- D. Administration of hydroxyurea
- E. Supplementation with iron
Aortic diseases Explanation: ***Aortic valve replacement***
- The patient's **severe aortic stenosis** (aortic jet velocity >4.0 m/s and mean pressure gradient >40 mmHg) is causing **shear stress** on red blood cells, leading to **microangiopathic hemolytic anemia**. This is characterized by low hemoglobin, high LDH, low haptoglobin, and negative Coombs test.
- **Aortic valve replacement** is the definitive treatment to reduce the shear stress, resolve the hemolysis, and improve the patient's symptoms of anemia and heart failure.
*Administration of corticosteroids*
- Corticosteroids are primarily used in **autoimmune hemolytic anemia** (positive Coombs test), which is not the case here as the direct Coombs test is negative.
- They would not address the underlying **mechanical destruction of red blood cells** due to aortic stenosis.
*Discontinuation of medication*
- The patient's current medications (simvastatin, lisinopril, metformin) are for managing his chronic conditions and are **not associated with hemolytic anemia**. Discontinuing them would be inappropriate and potentially harmful.
- There is no evidence to suggest a **drug-induced hemolytic anemia** in this case.
*Administration of hydroxyurea*
- Hydroxyurea is used in conditions like **sickle cell anemia** or **polycythemia vera** to modify red blood cell production or reduce cell counts, respectively.
- It has no role in treating **mechanical hemolytic anemia** caused by valvular heart disease.
*Supplementation with iron*
- While the patient has anemia, it is a **hemolytic anemia**, not an iron deficiency anemia, as indicated by the low haptoglobin and elevated LDH.
- Iron supplementation would **not stop the destruction of red blood cells** caused by the turbulent flow across the aortic valve.
Aortic diseases US Medical PG Question 10: A 69-year-old man is brought to the emergency room by his wife 30 minutes after losing consciousness while they were working in their garden together. The patient says that time seemed to slow down, his vision went dark, and he had a sensation of falling. After 3–5 seconds, he awoke slightly disoriented but quickly regained his baseline mental status. The patient says he has had a few similar episodes that occurred 1–2 months ago for which he did not seek any medical treatment. He says overall he has been more tired than usual and feeling out of breath on his morning walks. He denies any chest pain or palpitations. Past medical history is significant for type 1 diabetes mellitus. Current medications are atorvastatin and insulin. His family history is significant for his father who died of myocardial infarction in his 70’s. His blood pressure is 110/85 mm Hg and pulse is 82/min. On physical examination, there is a 3/6 systolic murmur best heard over the right sternal border with radiation to the carotids. S1 is normal but there is a soft unsplit S2. The lungs are clear to auscultation bilaterally. The remainder of the exam is unremarkable. Which of the following physical exam findings would also most likely be present in this patient?
- A. A decrease in systolic blood pressure ≥ 10 mmHg during inspiration
- B. A carotid biphasic pulse
- C. Increased capillary pulsations of the fingertips
- D. Distant heart sounds
- E. A slow-rising and delayed upstroke of the carotid pulse (Correct Answer)
Aortic diseases Explanation: ***A slow-rising and delayed upstroke of the carotid pulse***
- The patient's symptoms (syncope, dyspnea, fatigue) coupled with the **systolic murmur radiating to the carotids**, **soft unsplit S2**, and **type 1 diabetes mellitus** (a risk factor) are highly suggestive of **aortic stenosis**.
- **Pulsus parvus et tardus** (small, slow-rising, and delayed carotid pulse) is a classic physical exam finding in severe **aortic stenosis** due to the obstruction of left ventricular outflow.
*A decrease in systolic blood pressure ≥ 10 mmHg during inspiration*
- This finding, known as **pulsus paradoxus**, is characteristic of **cardiac tamponade** or severe **obstructive lung disease**.
- The patient's presentation of exertional syncope and a significant systolic ejection murmur does not align with these conditions.
*A carotid biphasic pulse*
- A **bisferiens pulse** (biphasic pulse) is typically observed in conditions that cause a rapid ejection followed by a second, smaller pulse, such as **aortic regurgitation** with or without **aortic stenosis**, or **hypertrophic obstructive cardiomyopathy**.
- While there is a systolic murmur, the overall clinical picture, particularly the unsplit S2, is more consistent with isolated **aortic stenosis**.
*Increased capillary pulsations of the fingertips*
- **Quincke's sign**, or capillary pulsations in the nail beds, is a characteristic finding of **severe aortic regurgitation** due to the wide pulse pressure.
- The patient’s symptoms and the murmur are more indicative of **aortic stenosis**, which is an outflow obstruction, rather than regurgitation.
*Distant heart sounds*
- **Distant heart sounds** are typically associated with conditions that create a barrier between the heart and the stethoscope, such as **pericardial effusion**, obesity, or emphysema.
- While common in a range of pathologies, it is not a specific or classic finding for **aortic stenosis**, and the other findings strongly point towards valvular disease rather than pericardial issues.
More Aortic diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.