Adult congenital heart disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adult congenital heart disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adult congenital heart disease US Medical PG Question 1: A 27-year-old woman, who recently immigrated from Bangladesh, presents to her primary care physician to discuss birth control. During a review of her past medical history, she reports that as a child she had a recurrent sore throat and fever followed by swollen and aching hip and knee joints. These symptoms returned every season and were never treated but went away on their own only to return with the next typhoon season. When asked about any current complaints, the patient says that she sometimes has shortness of breath and palpitations that do not last long. A physical exam is performed. In which of the auscultation sites will a murmur most likely be heard in this patient?
- A. Point 5 (Correct Answer)
- B. Point 4
- C. Point 2
- D. Point 3
- E. Point 1
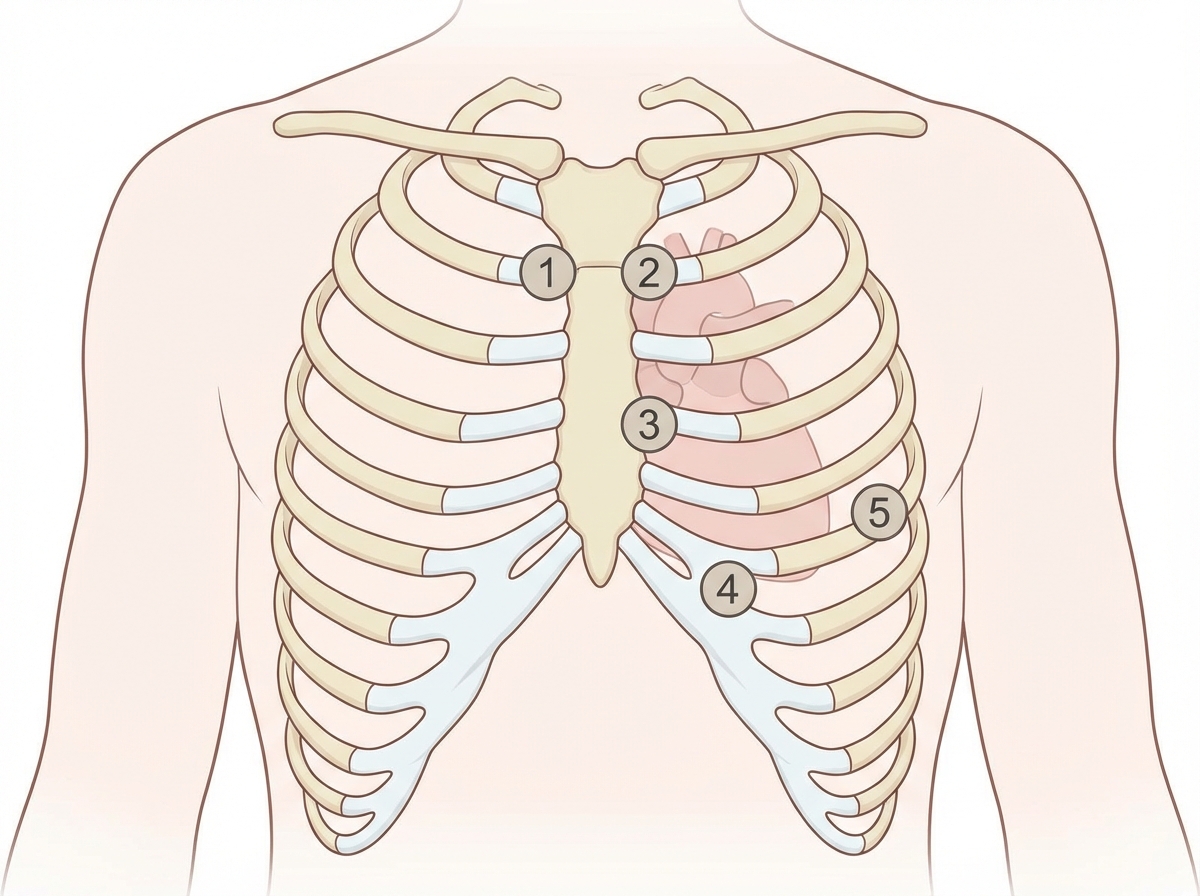
Adult congenital heart disease Explanation: ***Point 5***
- The patient's history of recurrent sore throat, fever, and migratory polyarthritis (swollen and aching hip and knee joints) followed by intermittent shortness of breath and palpitations is highly suggestive of **rheumatic fever** with subsequent **rheumatic heart disease**.
- This condition most commonly affects the **mitral valve**, leading to **mitral stenosis** or regurgitation, which would produce an apical murmur heard best at point 5 (the cardiac apex).
*Point 4*
- Point 4 corresponds to the **tricuspid area** (lower left sternal border). While rheumatic heart disease can affect the tricuspid valve, it is less common than mitral valve involvement and usually occurs in conjunction with severe mitral valve disease.
- An isolated murmur here would suggest tricuspid valve pathology, which is less likely as the primary presentation in rheumatic heart disease.
*Point 2*
- Point 2 is the **pulmonic area** (left upper sternal border, second intercostal space). Murmurs heard here typically indicate pulmonary valve disease or flow murmurs.
- While pulmonary hypertension can be a complication of severe left-sided heart disease, primary pulmonic valve involvement in rheumatic heart disease is rare.
*Point 3*
- Point 3 (Erb's point, third intercostal space, left sternal border) is often used to auscultate for murmurs of **aortic regurgitation** or to hear the splitting of S2.
- While aortic valve involvement can occur in rheumatic heart disease, **mitral valve disease** is significantly more prevalent and typically presents earlier and more severely.
*Point 1*
- Point 1 is the **aortic area** (right upper sternal border, second intercostal space). Murmurs heard here are typically associated with **aortic stenosis** or regurgitation.
- Although the aortic valve can be affected by rheumatic heart disease, the mitral valve is the most commonly involved valve, making an apical murmur (Point 5) more likely for the initial and most prominent finding.
Adult congenital heart disease US Medical PG Question 2: A 21-year-old Cambodian patient with a history of rheumatic heart disease presents to his primary care physician for a routine check-up. He reports being compliant with monthly penicillin G injections since being diagnosed with rheumatic fever at age 15. He denies any major side effects from the treatment, except for the inconvenience of organizing transportation to a physician's office every month. On exam, the patient is found to have a loud first heart sound and a mid-diastolic rumble that is best heard at the apex. Which of the following is the next best step?
- A. Switch to intramuscular cefotaxime, which has fewer side effects
- B. Continue intramuscular penicillin therapy (Correct Answer)
- C. Stop penicillin therapy
- D. Stop penicillin therapy in 4 years
- E. Decrease frequency of injections to bimonthly
Adult congenital heart disease Explanation: ***Continue intramuscular penicillin therapy***
- This patient has a history of **rheumatic heart disease** and is showing signs of **mitral stenosis** (loud S1, mid-diastolic rumble at the apex), indicating previous rheumatic fever and the effectiveness of current prophylaxis.
- Continuing prophylaxis is crucial to prevent further episodes of **rheumatic fever** and progression of cardiac damage, especially in regions with endemic rheumatic fever.
*Switch to intramuscular cefotaxime, which has fewer side effects*
- **Cefotaxime** is a third-generation cephalosporin and is not typically used for rheumatic fever prophylaxis, nor is it proven to have significantly fewer side effects in this context.
- **Penicillin G** is the gold standard for preventing recurrent rheumatic fever due to its proven efficacy and low cost.
*Stop penicillin therapy*
- Stopping prophylaxis would put the patient at high risk for **recurrent rheumatic fever** and worsening of their established **rheumatic heart disease**, which can lead to severe cardiac complications.
- The patient's current heart sounds suggest ongoing valvular disease, making continued prevention of exacerbations critical.
*Stop penicillin therapy in 4 years*
- The duration of **rheumatic fever prophylaxis** is determined by the patient's age and the presence of **rheumatic heart disease**. For patients with documented rheumatic heart disease, prophylaxis often continues for much longer periods, often until age 40 or even lifelong.
- Stopping at "4 years" from age 21 (i.e., at age 25) is too early for a patient with established rheumatic heart disease.
*Decrease frequency of injections to bimonthly*
- Monthly intramuscular **penicillin G** is the standard and most effective regimen for secondary prophylaxis of rheumatic fever.
- Decreasing the frequency would reduce the drug's therapeutic levels and significantly increase the risk of breakthrough streptococcal infections and subsequent episodes of **rheumatic fever**.
Adult congenital heart disease US Medical PG Question 3: A 4-year-old Caucasian male suffers from cyanosis and dyspnea relieved by squatting. Which of the following abnormalities is most likely present?
- A. Atrial septal defect
- B. Coarctation of the aorta
- C. Bicuspid aortic valve
- D. Ventricular septal defect
- E. Tetralogy of Fallot (Correct Answer)
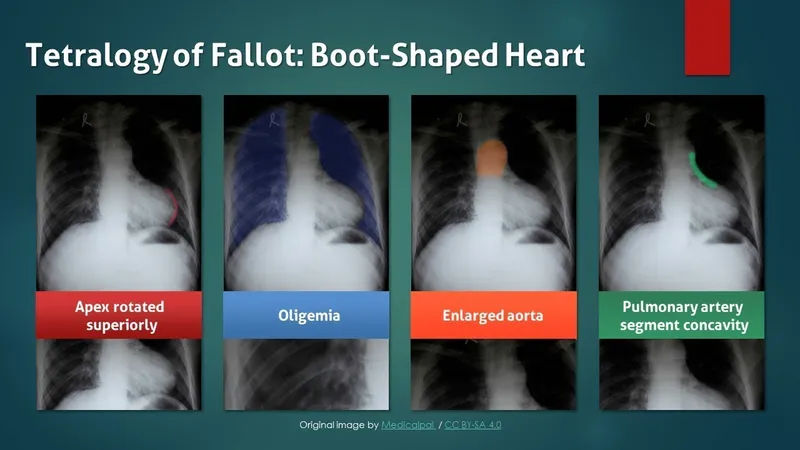
Adult congenital heart disease Explanation: ***Tetralogy of Fallot***
- **Cyanosis** and **dyspnea relieved by squatting** are the hallmark clinical features of **Tetralogy of Fallot**, making this the correct diagnosis.
- The condition consists of four anatomic abnormalities: **ventricular septal defect (VSD)**, **right ventricular outflow tract obstruction**, **right ventricular hypertrophy**, and **overriding aorta**.
- The right-to-left shunt across the VSD causes **deoxygenated blood** to enter systemic circulation, producing **cyanosis**.
- **Squatting increases systemic vascular resistance (SVR)**, which decreases the right-to-left shunt, improves pulmonary blood flow, and relieves cyanosis and dyspnea during **"tet spells"**.
*Atrial septal defect*
- ASDs typically cause **left-to-right shunts** and are **acyanotic lesions**.
- Patients may be asymptomatic or present with **exertional dyspnea** and **fatigue** in later childhood or adulthood.
- Cyanosis would only occur if **Eisenmenger syndrome** develops (reversal to right-to-left shunt due to pulmonary hypertension), which is rare at age 4 and does not improve with squatting.
*Coarctation of the aorta*
- This is an **acyanotic** lesion characterized by **narrowing of the descending aorta**.
- Classic findings include **upper extremity hypertension**, **diminished or delayed femoral pulses**, and **lower extremity hypotension**.
- Does not cause cyanosis or squatting relief.
*Bicuspid aortic valve*
- A common **acyanotic** congenital abnormality that may lead to **aortic stenosis** or **regurgitation** over time.
- Usually asymptomatic in childhood; may present with **murmur**, chest pain, or syncope in adulthood.
- Does not cause cyanosis or relief with squatting.
*Ventricular septal defect*
- Isolated VSDs typically cause **left-to-right shunts** and are **acyanotic**.
- May present with **heart failure symptoms** (tachypnea, poor feeding, failure to thrive) in infancy if the defect is large.
- Cyanosis occurs only if **Eisenmenger syndrome** develops (usually takes years to decades), and symptoms are not relieved by squatting.
Adult congenital heart disease US Medical PG Question 4: A 7-year-old boy is brought by his parents to his pediatrician due to progressive fatigue and shortness of breath while playing sports. He is otherwise healthy with no known medical disorders and no other symptoms. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. On physical examination, his temperature is 36.9ºC (98.4ºF), pulse rate is 90/min, blood pressure is 100/70 mm Hg, and respiratory rate is 18/min. Pulses in all four extremities are equal and normally palpated; there is no radio-femoral delay. The pediatrician suspects a congenital heart disease after auscultation of the heart. Which of the following congenital heart diseases is most likely to present with the clinical features listed above?
- A. Atrial septal defect (Correct Answer)
- B. Double-outlet right ventricle with subaortic ventricular septal defect
- C. Coarctation of the aorta
- D. Aortopulmonary window defect
- E. Complete atrioventricular septal defect
Adult congenital heart disease Explanation: ***Atrial septal defect***
- An **atrial septal defect (ASD)** typically presents in older children or adults with symptoms like **fatigue** and **shortness of breath on exertion (dyspnea)** due to increased pulmonary blood flow, after years of being asymptomatic.
- The absence of cyanosis and normal pulses are consistent with an ASD, as it's typically an **acyanotic heart defect** where shunting occurs from left to right.
*Double-outlet right ventricle with subaortic ventricular septal defect*
- This condition involves both great arteries originating from the **right ventricle**, often leading to **cyanosis** from birth or early infancy due to mixing of oxygenated and deoxygenated blood.
- Patients typically present much earlier with signs of **heart failure**, **cyanosis**, and **failure to thrive**, which are not reported in this 7-year-old boy.
*Coarctation of the aorta*
- **Coarctation of the aorta** is characterized by a **narrowing of the aorta**, leading to a classic finding of **radio-femoral delay** and **different blood pressures in the upper and lower extremities**, which are specifically stated to be absent in this patient.
- While it can cause shortness of breath and fatigue, the lack of radio-femoral delay makes this diagnosis unlikely.
*Aortopulmonary window defect*
- An **aortopulmonary window (APW)** is a rare defect involving a communication between the aorta and pulmonary artery, usually presenting in **infancy** with severe symptoms of **heart failure** and **pulmonary hypertension** due to a large left-to-right shunt.
- This patient's presentation at 7 years of age without early severe symptoms makes APW less likely.
*Complete atrioventricular septal defect*
- A **complete atrioventricular septal defect (AVSD)** involves a defect in both the atrial and ventricular septa and a common AV valve, usually causing **severe symptoms of heart failure** and **pulmonary hypertension in infancy**.
- It is also strongly associated with **Down syndrome**, which is not mentioned, and severe symptoms would have presented much earlier than age 7.
Adult congenital heart disease US Medical PG Question 5: A 3-year-old boy is brought to the physician because of recurrent nosebleeds and fatigue for the past 2 months. He also frequently complains his head hurts. The patient has met all motoric milestones for his age but does not like to run because his legs start to hurt if he does. He is at the 40th percentile for both height and weight. His temperature is 37.0°C (98.6°F), pulse is 125/min, respirations are 32/min, and blood pressure in the right arm is 130/85 mm Hg. A grade 2/6 systolic murmur is heard in the left paravertebral region. Further evaluation of this patient is most likely to show which of the following findings?
- A. Inferior rib notching
- B. Delayed pulse in lower extremities (Correct Answer)
- C. Interarm difference in tissue oxygenation
- D. Pulmonary valve stenosis
- E. Left-axis deviation on ECG
Adult congenital heart disease Explanation: ***Delayed pulse in lower extremities***
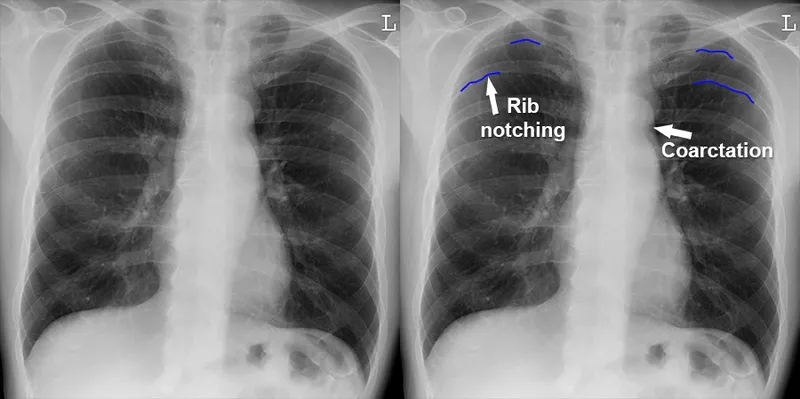
- The patient's symptoms, including **recurrent nosebleeds**, **headaches**, **leg pain with activity**, **hypertension** (especially in the right arm), and a **systolic murmur in the left paravertebral region**, are highly suggestive of **coarctation of the aorta**.
- A key physical finding in coarctation of the aorta is a **delayed and diminished femoral pulse** compared to the radial pulse due to obstruction of blood flow to the lower body.
*Inferior rib notching*
- This finding is characteristic of **collateral circulation** developing around a coarctation in older children and adults, as the **intercostal arteries** become enlarged to supply blood to the lower body.
- While associated with coarctation, it is typically seen on **chest X-rays** in older patients and is less likely to be present or pronounced in a 3-year-old.
*Interarm difference in tissue oxygenation*
- While coarctation can cause an **interarm blood pressure difference**, it typically does not directly cause a significant interarm difference in **tissue oxygenation** unless severe unilateral subclavian artery involvement is present, which is not the primary mechanism.
- The primary oxygenation concern in coarctation is usually related to overall cardiac output or systemic effects rather than a localized interarm difference.
*Pulmonary valve stenosis*
- **Pulmonary valve stenosis** would typically present with a **systolic ejection murmur** heard best at the left upper sternal border, often radiating to the back.
- It does not explain the specific constellation of symptoms such as **hypertension in the upper extremities**, **leg pain with activity**, or differential pulses characteristic of coarctation of the aorta.
*Left-axis deviation on ECG*
- **Left-axis deviation** on an ECG is often associated with conditions causing **left ventricular hypertrophy** or conduction defects.
- While severe coarctation can lead to left ventricular hypertrophy, left-axis deviation is not a specific or direct diagnostic finding for coarctation and is less characteristic than the described physical exam findings.
Adult congenital heart disease US Medical PG Question 6: A 36-year-old healthy man presents to his physician to discuss his concerns about developing heart disease. His father, grandfather, and older brother had heart problems, and he has become increasingly worried he might be at risk. He takes no medications and his past medical history is only significant for an appendectomy at 20 years ago. He is married happily with 2 young children and works as a hotel manager and exercises occasionally in the hotel gym. He drinks 3–5 alcoholic beverages per week but denies smoking and illicit drug use. Today his blood pressure is 146/96 mm Hg, pulse rate is 80/min, and respiratory rate is 16/min. He has a body mass index of 26.8 kg/m2. His physical examination is otherwise unremarkable. Laboratory tests show:
Laboratory test
Serum glucose (fasting) 88 mg/dL
Serum electrolytes
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 0.8 mg/dl
Blood urea nitrogen 10 mg/dl
Cholesterol, total 350 mg/dL
HDL-cholesterol 40 mg/dL
LDL-cholesterol 280 mg/dL
Triglycerides 130 mg/dL
Besides appropriate medications for his cholesterol and a follow-up for his hypertension, which of the following supplements is thought to provide a protective cardiovascular effect?
- A. Folic acid (Correct Answer)
- B. Thiamine
- C. Vitamin K
- D. Vitamin B12
- E. Vitamin E
Adult congenital heart disease Explanation: ***Folic acid***
- Folic acid (Vitamin B9) is involved in the metabolism of **homocysteine**, and elevated homocysteine levels are associated with increased cardiovascular risk.
- **Historically**, it was hypothesized that lowering homocysteine with folic acid would reduce cardiovascular events.
- However, **large randomized controlled trials (HOPE-2, NORVIT, VISP) have failed to demonstrate cardiovascular benefit** from folic acid supplementation despite successfully lowering homocysteine levels.
- Among the options listed, folic acid was the supplement most **historically thought** to provide cardiovascular protection, though current evidence does not support routine supplementation for this purpose.
- **Current guidelines do NOT recommend** folic acid supplementation for cardiovascular disease prevention in the general population.
*Thiamine*
- **Thiamine** (Vitamin B1) is crucial for carbohydrate metabolism and nerve function.
- Thiamine deficiency can lead to **beriberi** (including wet beriberi with cardiac manifestations), but supplementation in individuals without deficiency provides **no cardiovascular protection**.
*Vitamin K*
- **Vitamin K** is essential for blood clotting and bone metabolism, and may play a role in preventing vascular calcification.
- However, there is **insufficient evidence** to recommend vitamin K supplementation for cardiovascular protection in clinical practice.
*Vitamin B12*
- **Vitamin B12** is important for nerve function, red blood cell formation, and homocysteine metabolism.
- Like folic acid, B12 was studied for cardiovascular protection through homocysteine reduction, but **clinical trials failed to show benefit**.
- Routine B12 supplementation for cardiovascular protection in individuals with normal B12 levels is **not recommended**.
*Vitamin E*
- **Vitamin E** is an antioxidant that was extensively studied for cardiovascular protection in the 1990s-2000s.
- **Large clinical trials (HOPE, GISSI) conclusively showed NO cardiovascular benefit** from vitamin E supplementation, and some studies suggested potential harm at high doses.
- Vitamin E supplementation for cardiovascular disease prevention is **not recommended**.
Adult congenital heart disease US Medical PG Question 7: A 20-year-old man comes to the emergency room because of palpitations and mild dyspnea for the last 2 hours. He has had similar episodes in the past that resolved within 20 minutes, but they have been worsening since he started training for his first marathon 1 month ago. Ten years ago, he was treated for streptococcal pharyngitis with a 10-day course of penicillin. His maternal uncle passed away unexpectedly from a heart condition at age 40. He is 180 cm (5 ft 11 in) tall and weighs 85 kg (187 lb); BMI is 26.2 kg/m2. His temperature is 36.5°C (97.7°F), pulse is 70/min, respirations are 18/min, and blood pressure is 132/60 mm Hg. On examination, there is a decrescendo early diastolic murmur heard best along the left sternal border. His head slightly bobs about every second. The remainder of the examination shows no abnormalities. Which of the following is most likely to be present?
- A. Bicuspid aortic valve (Correct Answer)
- B. Antistreptolysin O antibodies
- C. Asymmetric septal hypertrophy
- D. Valve vegetation
- E. Myxomatous degeneration
Adult congenital heart disease Explanation: ***Bicuspid aortic valve***
- The patient presents with classic signs of **aortic regurgitation**, including a **decrescendo early diastolic murmur** and **De Musset's sign** (head bobbing). In a young individual, a **bicuspid aortic valve** is the most common congenital cause of aortic valve disease, often leading to regurgitation or stenosis over time.
- The patient's history of palpitations and dyspnea, worsening with exertion, suggests significant hemodynamic compromise related to chronic aortic insufficiency, which can develop secondary to a bicuspid valve.
*Antistreptolysin O antibodies*
- While the patient had a history of **streptococcal pharyngitis** 10 years ago, there are no other signs of **acute rheumatic fever** or **rheumatic heart disease**, such as migratory polyarthritis, chorea, or erythema marginatum.
- The murmur described is typical of aortic regurgitation without specific features pointing to rheumatic involvement, which typically affects the **mitral valve** first.
*Asymmetric septal hypertrophy*
- **Asymmetric septal hypertrophy** is characteristic of **hypertrophic cardiomyopathy**, which would typically present with a **systolic murmur** that increases with Valsalva maneuver, not an early diastolic murmur.
- While sudden cardiac death in a young relative might suggest hypertrophic cardiomyopathy, the physical exam findings here are inconsistent with that diagnosis.
*Valve vegetation*
- **Valve vegetations** are associated with **infective endocarditis** and would typically present with fever, new or worsening murmur, and signs of systemic infection, none of which are noted in this patient.
- The patient's symptoms are chronic and episodic, not acute, subacute, or associated with infectious signs.
*Myxomatous degeneration*
- **Myxomatous degeneration** primarily affects the **mitral valve**, leading to **mitral valve prolapse** and subsequent regurgitation, which would produce a **mid-systolic click** followed by a late systolic murmur.
- This condition is not typically associated with an early diastolic murmur characteristic of aortic regurgitation.
Adult congenital heart disease US Medical PG Question 8: A 68-year-old man is brought to the emergency department because of right-sided weakness for 2 hours. He has hypertension, dyslipidemia, and type 2 diabetes. Current medications include hydrochlorothiazide, metoprolol, amlodipine, pravastatin, and metformin. His pulse is 87/min and blood pressure is 164/98 mm Hg. Neurological examination shows right-sided weakness, facial droop, and hyperreflexia. Sensation is intact. Which of the following is the most likely cause of these findings?
- A. Lipohyalinosis of penetrating vessels (Correct Answer)
- B. Dissection of the vertebral artery
- C. Stenosis of the internal carotid artery
- D. Rupture of an intracranial aneurysm
- E. Embolism from the left atrium
Adult congenital heart disease Explanation: ***Lipohyalinosis of penetrating vessels***
- This patient presents with an acute onset of **hemiparesis**, **facial droop**, and hyperreflexia, without cortical signs like cortical sensory loss or aphasia, which is characteristic of a **lacunar stroke**.
- **Lipohyalinosis** is the most common cause of lacunar infarcts, resulting from chronic hypertension and diabetes affecting small penetrating arteries in the brain.
*Dissection of the vertebral artery*
- Vertebral artery dissection typically presents with **posterior circulation symptoms** such as vertigo, ataxia, brainstem dysfunction, and often includes severe headache or neck pain.
- The presented symptoms of pure motor hemiparesis are more indicative of an anterior circulation event involving deeper structures.
*Stenosis of the internal carotid artery*
- Significant **internal carotid artery stenosis** typically causes larger territorial infarcts by reducing blood flow or via artery-to-artery embolism to the middle cerebral artery territory.
- This would result in symptoms like **aphasia**, **cortical sensory deficits**, or **homonymous hemianopia**, which are not present here.
*Rupture of an intracranial aneurysm*
- A ruptured intracranial aneurysm usually causes a **subarachnoid hemorrhage**, leading to a sudden, severe headache ("thunderclap headache"), meningismus, and altered consciousness.
- While focal neurological deficits can occur, the primary presentation is distinct from the patient's symptoms of a gradual onset of pure motor deficit.
*Embolism from the left atrium*
- An embolism from the left atrium (e.g., due to atrial fibrillation) typically causes a **cortical infarct** involving a larger vascular territory, such as the middle cerebral artery.
- This would result in symptoms like **aphasia**, **neglect**, or **cortical sensory deficits**, which are absent in this presentation of pure motor hemiparesis.
Adult congenital heart disease US Medical PG Question 9: A 14-year-old boy is brought to the emergency department from school after falling in gym class. He was unable to stand after the accident and has a painful and swollen knee. On presentation he says that he has never had an incident like this before; however, he does suffer from hard to control nosebleeds and prolonged bleeding after minor cuts. Based on his presentation a panel of bleeding tests is obtained with the following results:
Bleeding time: Prolonged
Prothrombin time: Normal
Partial thromboplastin time: Prolonged
Which of the following describes the function of the component that is defective in the most likely cause of this patient's symptoms?
- A. Binds to a nucleotide derivative
- B. Binds to fibrinogen
- C. Binds to subendothelial collagen (Correct Answer)
- D. It is a cofactor for an epoxide reductase
- E. Catalyzes the conversion of factor X
Adult congenital heart disease Explanation: ***Binds to subendothelial collagen***
- The patient's history of **nosebleeds**, **prolonged bleeding**, and a knee injury suggests a **primary hemostasis** defect. The lab results (prolonged bleeding time, normal PT, prolonged PTT) point to **von Willebrand disease** (vWD).
- The most important function of **von Willebrand factor** (vWF), which is deficient or dysfunctional in vWD, is to mediate platelet adhesion to the **subendothelial collagen** at sites of vascular injury.
*Binds to a nucleotide derivative*
- This option refers to the function of **P2Y12 receptors** on platelets, which bind to ADP (a nucleotide derivative) to promote platelet aggregation.
- While important for platelet function, this is not the primary defect in von Willebrand disease, which is an issue with **platelet adhesion**.
*Binds to fibrinogen*
- **Glycoprotein IIb/IIIa receptors** on platelets bind to **fibrinogen** to mediate platelet aggregation and form a platelet plug.
- This is a secondary step in hemostasis, and while affected by vWF's indirect role in stabilizing FVIII, it's not the direct primary defect.
*It is a cofactor for an epoxide reductase*
- This describes the role of **Vitamin K** in the carboxylation of clotting factors; specifically, its role as a cofactor for **gamma-glutamyl carboxylase**, which is then reduced by **epoxide reductase**.
- Deficiencies in Vitamin K activity affect the **extrinsic** and **common pathways** (factors II, VII, IX, X), which would typically present with a **prolonged PT** in addition to PTT, unlike this patient.
*Catalyzes the conversion of factor X*
- This describes the function of **Factor IXa** (in complex with Factor VIIIa) and **Factor VIIa** (with Tissue Factor), which activate Factor X to Factor Xa.
- While vWF stabilizes **Factor VIII**, leading to prolonged PTT, the direct catalytic conversion of Factor X is not the primary function of vWF itself.
Adult congenital heart disease US Medical PG Question 10: An 80-year-old man presents to the emergency department because of gnawing substernal chest pain that started an hour ago and radiates to his neck and left jaw. A 12-lead ECG is obtained and shows ST-segment elevation with newly developing Q waves. He is admitted for treatment. 4 days after hospitalization he suddenly develops altered mental status, and his blood pressure falls from 115/75 mm Hg to 80/40 mm Hg. Physical examination shows jugular venous distention, pulsus paradoxus, and distant heart sounds. What is the most likely cause of this patient's condition?
- A. Pericardial inflammation
- B. Compression of heart chambers by blood in the pericardial space (Correct Answer)
- C. Arrhythmia caused by ventricular fibrillation
- D. Rupture of papillary muscle
- E. Acute pulmonary edema from left heart failure
Adult congenital heart disease Explanation: ***Compression of heart chambers by blood in the pericardial space***
- The patient's initial presentation with ST-elevation myocardial infarction (STEMI) and subsequent development of **hypotension**, **jugular venous distention**, **pulsus paradoxus**, and **distant heart sounds** (Beck's triad) is highly indicative of **cardiac tamponade.**
- In the context of a recent MI, this constellation of symptoms strongly suggests a **cardiac free wall rupture**, leading to blood accumulation in the pericardial sac and compression of the heart.
- Free wall rupture typically occurs **3-7 days post-MI** and is a life-threatening mechanical complication.
*Pericardial inflammation*
- While pericardial inflammation (pericarditis) can occur post-MI, it typically manifests with **pleuritic chest pain** that is relieved by leaning forward and is often associated with a **pericardial friction rub.**
- It does not typically lead to acute, severe hypotension, pulsus paradoxus, or sudden circulatory collapse in this manner without significant effusion and tamponade physiology.
*Arrhythmia caused by ventricular fibrillation*
- **Ventricular fibrillation** would cause immediate cardiac arrest and loss of consciousness, not a gradual development of hypotension, JVD, and pulsus paradoxus.
- While arrhythmias are common post-MI, the specific physical findings point away from isolated VFib as the primary cause of hemodynamic collapse.
*Acute pulmonary edema from left heart failure*
- **Acute pulmonary edema** is a manifestation of **left heart failure**, characterized by severe dyspnea, orthopnea, and crackles on lung auscultation.
- While left heart failure can cause hypotension in cardiogenic shock, it would not typically present with the classic signs of cardiac tamponade such as pulsus paradoxus, distant heart sounds, and prominent JVD without pulmonary congestion findings.
*Rupture of papillary muscle*
- **Papillary muscle rupture** leads to severe **acute mitral regurgitation**, causing acute pulmonary edema, a new holosystolic murmur, and often cardiogenic shock.
- While it can lead to hypotension, it doesn't typically present with the classic signs of cardiac tamponade such as pulsus paradoxus and distant heart sounds; instead, a loud murmur would be prominent.
More Adult congenital heart disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.