Ventricular arrhythmias US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ventricular arrhythmias. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ventricular arrhythmias US Medical PG Question 1: An ECG from an 8-year-old male with neurosensory deafness and a family history of sudden cardiac arrest demonstrates QT-interval prolongation. Which of the following is this patient most at risk of developing?
- A. Hypertrophic cardiac myopathy
- B. Cardiac tamponade
- C. Essential hypertension
- D. Torsades de pointes (Correct Answer)
- E. First degree atrioventricular block
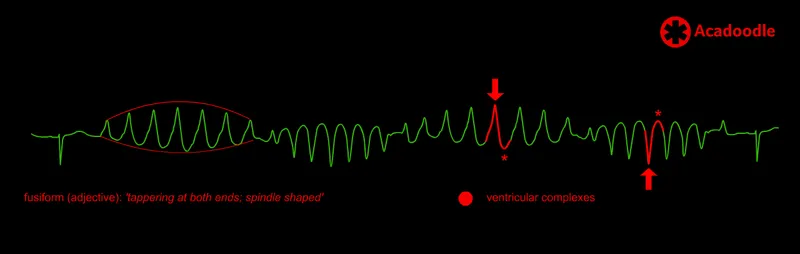
Ventricular arrhythmias Explanation: ***Torsades de pointes***
- The combination of **neurosensory deafness**, **QT-interval prolongation**, and a family history of **sudden cardiac arrest** is highly suggestive of **Jervell and Lange-Nielsen syndrome**, a form of **long QT syndrome**.
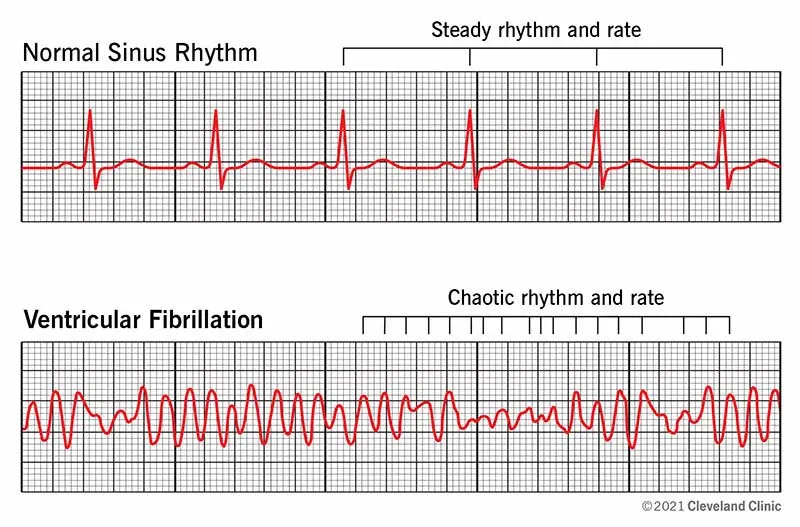
- Patients with long QT syndrome are at significant risk for developing **polymorphic ventricular tachycardia** known as **Torsades de pointes**, which can degenerate into **ventricular fibrillation** and cause sudden cardiac death.
*Hypertrophic cardiac myopathy*
- This condition involves thickening of the **ventricular walls** and is associated with outflow tract obstruction, not primarily with QT prolongation.
- While it can cause sudden cardiac arrest, it typically presents with symptoms like **dyspnea, chest pain**, or syncope during exertion, and its ECG findings usually include **left ventricular hypertrophy** and **deep Q waves**.
*Cardiac tamponade*
- **Cardiac tamponade** results from the accumulation of fluid in the **pericardial sac**, compressing the heart and impairing its filling.
- This condition is not related to **QT prolongation** or **sensorineural deafness** and would present with signs of **hemodynamic instability**, such as **pulsus paradoxus** and muffled heart sounds.
*Essential hypertension*
- **Essential hypertension** is chronic high blood pressure with no identifiable secondary cause, commonly affecting adults.
- It is not associated with **congenital neurosensory deafness** or significant **QT-interval prolongation** in childhood.
*First degree atrioventricular block*
- **First-degree AV block** is characterized by a prolonged **PR interval** on ECG, indicating delayed conduction through the AV node.
- While it's an electrical abnormality, it is distinct from **QT prolongation** and is not typically associated with **neurosensory deafness** or the same risk of sudden cardiac arrest as long QT syndrome.
Ventricular arrhythmias US Medical PG Question 2: A 62-year-old man is brought to the emergency department because of syncope. He reports sudden onset of palpitations followed by loss of consciousness while carrying his groceries to his car. He is unable to recall any further details and does not have any chest pain or dizziness. He has a history of hypertension, type 2 diabetes mellitus, gastroparesis, and osteoarthritis of the knees. Medications include lisinopril, metformin, and ondansetron as needed for nausea. He also takes methadone daily for chronic pain. Apart from an abrasion on his forehead, he appears well. His temperature is 37.2 °C (98.9 F), heart rate is 104/min and regular, and blood pressure is 135/70 mm Hg. While he is in the emergency department, he loses consciousness again. Telemetry shows polymorphic ventricular tachycardia with cyclic alteration of the QRS axis that spontaneously resolves after 30 seconds. Results of a complete blood count, serum electrolyte concentrations, and serum thyroid studies show no abnormalities. Cardiac enzymes are within normal limits. Which of the following is the most likely underlying cause of this patient's syncope?
- A. Prinzmetal angina
- B. Fast accessory conduction pathway
- C. Brugada syndrome
- D. Prolonged QT interval (Correct Answer)
- E. Hypomagnesemia
Ventricular arrhythmias Explanation: ***Prolonged QT interval***
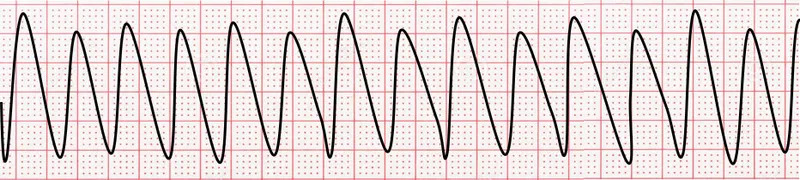
- The patient experienced **polymorphic ventricular tachycardia** with cyclic alteration of the **QRS axis** (Torsades de Pointes), which is characteristic of a prolonged QT interval.
- **Methadone is known to prolong the QT interval**, and the patient's history of syncope preceded by palpitations is consistent with this arrhythmia.
*Prinzmetal angina*
- Prinzmetal angina involves **coronary artery spasm**, leading to **transient myocardial ischemia**, typically causing chest pain, not primarily syncope from polymorphic VT.
- While it can cause arrhythmias, the characteristic EKG finding would be **ST-segment elevation during pain**, which is not described.
*Fast accessory conduction pathway*
- A fast accessory pathway (e.g., in Wolfe-Parkinson-White syndrome) can lead to **AV reentrant tachycardia** or **pre-excitation** with atrial fibrillation, but not typically polymorphic VT with cyclic QRS alteration.
- The EKG would show a **delta wave** and a short PR interval, which is not mentioned.
*Brugada syndrome*
- Brugada syndrome is an inherited channelopathy **characterized by specific EKG patterns** (e.g., coved-type ST elevation in V1-V3) and an increased risk of sudden cardiac death due to ventricular arrhythmias.
- The patient's EKG findings of polymorphic VT with cyclic QRS alteration are not typical of Brugada syndrome-induced arrhythmia.
*Hypomagnesemia*
- While **hypomagnesemia can prolong the QT interval** and lead to Torsades de Pointes, the patient's **serum electrolyte concentrations were normal**, ruling out this direct cause.
- Magnesium levels would need to be critically low for such an effect, and this is typically detected on blood tests.
Ventricular arrhythmias US Medical PG Question 3: A 29-year-old woman with Wolff-Parkinson-White syndrome presents to her cardiologist’s office for a follow-up visit. She collapsed at her job and made a trip to the emergency department 1 week ago. At that time, she received a diagnosis of atrial fibrillation with rapid ventricular response and hemodynamic instability. While in the emergency department, she underwent direct-current cardioversion to return her heart to sinus rhythm. Her current medications include procainamide. At the cardiologist’s office, her heart rate is 61/min, respiratory rate is 16/min, the temperature is 36.5°C (97.7°F), and blood pressure is 118/60 mm Hg. Her cardiac examination reveals a regular rhythm and a I/VI systolic ejection murmur best heard at the right upper sternal border. An ECG obtained in the clinic is shown. Which of the following is the most appropriate treatment to prevent further episodes of tachyarrhythmia?
- A. Begin anticoagulation with dabigatran
- B. Add verapamil to her medication regimen
- C. Begin anticoagulation with warfarin
- D. Refer her for electrophysiology (EP) study and ablation (Correct Answer)
- E. Refer her for right heart catheterization
Ventricular arrhythmias Explanation: ***Refer her for electrophysiology (EP) study and ablation***
- This patient has **Wolff-Parkinson-White (WPW) syndrome** and experienced a life-threatening episode of **atrial fibrillation with rapid ventricular response (AFib with RVR)** and **hemodynamic instability**, indicating a high-risk accessory pathway.
- **Catheter ablation** of the accessory pathway is the definitive treatment to eliminate the re-entrant circuit and prevent future tachyarrhythmia episodes and sudden cardiac death in symptomatic WPW patients.
*Begin anticoagulation with dabigatran*
- While anticoagulation is indicated for stroke prevention in AFib, this patient's primary risk is not stroke but rather recurrent, potentially fatal, **tachyarrhythmias due to WPW**.
- Current guidelines suggest that anticoagulation is not routinely needed for AFib in the setting of WPW unless other risk factors for stroke are present (e.g., high **CHA₂DS₂-VASc score** for non-valvular AFib), which are not mentioned here for a 29-year-old.
*Add verapamil to her medication regimen*
- **Calcium channel blockers** like verapamil are contraindicated in WPW syndrome with AFib.
- They can block the normal AV nodal conduction, shunting more impulses down the **accessory pathway** and potentially accelerating the ventricular rate, leading to **ventricular fibrillation**.
*Begin anticoagulation with warfarin*
- Similar to dabigatran, anticoagulation with warfarin is primarily for **stroke prevention in AFib**, not for preventing the tachyarrhythmia itself in WPW.
- The immediate and most critical concern for this patient is the risk of recurrent, life-threatening **re-entrant tachyarrhythmias** via the accessory pathway.
*Refer her for right heart catheterization*
- A **right heart catheterization** is used to measure pressures and oxygen saturations in the right side of the heart and pulmonary arteries, typically to evaluate for conditions like pulmonary hypertension or heart failure.
- It is not indicated for the diagnosis or treatment of **supraventricular tachycardias** or **accessory pathways** like in WPW syndrome.
Ventricular arrhythmias US Medical PG Question 4: A 25-year-old man presents to the emergency department complaining of palpitations, lightheadedness, and sweating. He just started working at an investment firm and has been working long hours to make a good impression. Today, he had a dozen cups of espresso to keep himself awake and working. He has never had such an episode before. His past medical history is unremarkable. His pulse is 150/min, blood pressure is 134/88 mm Hg, respirations are 12/min, and temperature is 36.7°C (98.0°F). ECG shows supraventricular tachycardia. Which of the following is the next best step in the management of this patient?
- A. Drinking coffee
- B. Synchronized cardioversion
- C. Valsalva maneuver (Correct Answer)
- D. Adenosine infusion
- E. Dipping his face in cold water
Ventricular arrhythmias Explanation: ***Valsalva maneuver***
- The Valsalva maneuver is a **first-line vagal maneuver** used to terminate **supraventricular tachycardia (SVT)** in a stable patient, as it increases vagal tone to slow heart rate.
- Given the patient's **hemodynamic stability** (BP 134/88 mmHg, no signs of shock), vagal maneuvers are the appropriate initial intervention.
*Drinking coffee*
- **Caffeine** is a stimulant that can *induce* or worsen tachycardia, making it an inappropriate and potentially harmful intervention in this situation.
- The patient's current symptoms are likely **caffeine-induced**, so more caffeine would exacerbate the problem.
*Synchronized cardioversion*
- **Synchronized cardioversion** is reserved for **unstable SVT** (e.g., hypotension, altered mental status, acute heart failure, ischemic chest pain), which is not present in this patient.
- It is an invasive procedure with risks and should only be used when less aggressive measures fail or the patient is in immediate danger.
*Adenosine infusion*
- **Adenosine** is an effective pharmacological agent for terminating SVT but is typically used if **vagal maneuvers fail** or are contraindicated.
- As this patient is stable, **vagal maneuvers** should be attempted first due to their non-invasive nature and rapid action.
*Dipping his face in cold water*
- While **diving reflex** (induced by cold water immersion) is a vagal maneuver that can terminate SVT, it is **less commonly used** and often less effective than the Valsalva maneuver.
- The Valsalva maneuver is generally the preferred and more practical initial vagal maneuver in an emergency setting.
Ventricular arrhythmias US Medical PG Question 5: An investigator is comparing the risk of adverse effects among various antiarrhythmic medications. One of the drugs being studied primarily acts by blocking the outward flow of K+ during myocyte repolarization. Further investigation shows that the use of this drug is associated with a lower rate of ventricular tachycardia, ventricular fibrillation, and torsades de pointes when compared to similar drugs. Which of the following drugs is most likely being studied?
- A. Verapamil
- B. Procainamide
- C. Esmolol
- D. Amiodarone (Correct Answer)
- E. Sotalol
Ventricular arrhythmias Explanation: ***Amiodarone***
- Amiodarone is a **Class III antiarrhythmic drug** that primarily blocks **potassium channels**, thereby prolonging repolarization and the effective refractory period in cardiac myocytes.
- While it has properties of all four Vaughn-Williams classes, its dominant action as a potassium channel blocker makes it highly effective in preventing and treating various arrhythmias, including **ventricular tachycardia (VT)** and **ventricular fibrillation (VF)**, and it has a relatively lower risk of **torsades de pointes (TdP)** compared to other Class III drugs due to its broader ion channel effects.
*Verapamil*
- Verapamil is a **Class IV antiarrhythmic drug (non-dihydropyridine calcium channel blocker)** that primarily blocks **L-type calcium channels**, slowing conduction through the AV node.
- It is mainly used for **supraventricular tachycardias** and rate control in atrial fibrillation, not typically for ventricular arrhythmias like VT/VF.
*Procainamide*
- Procainamide is a **Class IA antiarrhythmic drug** that blocks **sodium channels** and also prolongs repolarization by blocking some potassium channels, but its primary effect is on sodium channels.
- Class IA drugs are known to **increase the QT interval** and carry a significant risk of **torsades de pointes**, making them less favorable for preventing VT/VF with adverse effect concerns.
*Esmolol*
- Esmolol is a **Class II antiarrhythmic drug (beta-blocker)** that primarily acts by **blocking beta-adrenergic receptors**, thereby reducing heart rate, contractility, and AV nodal conduction.
- While useful in some arrhythmias, its main mechanism is not potassium channel blockade, and it is not typically preferred for the direct prevention of VT/VF in situations with concerns about TdP.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic drug** that primarily acts as a **potassium channel blocker**, prolonging the action potential duration and effective refractory period, and also has **beta-blocking properties**.
- While it blocks potassium channels, sotalol carries a **higher risk of torsades de pointes** compared to amiodarone, especially at higher doses and in patients with underlying heart conditions.
Ventricular arrhythmias US Medical PG Question 6: A 45-year-old man comes to the physician for a routine health maintenance examination. He feels well. He underwent appendectomy at the age of 25 years. He has a history of hypercholesterolemia that is well controlled with atorvastatin. He is an avid marathon runner and runs 8 miles per day four times a week. His father died of myocardial infarction at the age of 42 years. The patient does not smoke or drink alcohol. His vital signs are within normal limits. Cardiopulmonary examination shows no abnormalities. His abdomen is soft and nontender with a surgical scar in the right lower quadrant. Laboratory studies are within normal limits. An ECG is shown. Which of the following is the most likely diagnosis?
- A. Mobitz type II AV block
- B. First-degree AV block
- C. Mobitz type I AV block (Correct Answer)
- D. Third-degree AV block
- E. Atrial fibrillation
Ventricular arrhythmias Explanation: ***Mobitz type I AV block***
- The ECG shows progressive prolongation of the **PR interval** followed by a dropped QRS complex, which is characteristic of a **Mobitz type I (Wenckebach) AV block**.
- This rhythm disturbance is often benign, especially in athletes with high **vagal tone**, and does not usually require treatment.
*Mobitz type II AV block*
- **Mobitz type II AV block** is characterized by a constant PR interval before the dropped QRS complex.
- This type of block is generally more serious and indicative of a conduction disturbance below the AV node, often requiring a **pacemaker**.
*First-degree AV block*
- A **first-degree AV block** presents with a consistently prolonged PR interval (greater than 0.20 seconds) on every beat, without any dropped beats.
- In this patient's ECG, there is a dropped QRS complex after progressive PR prolongation.
*Third-degree AV block*
- **Third-degree (complete) AV block** is characterized by complete dissociation between the P waves and QRS complexes.
- There is no relationship between atrial and ventricular activity, and the ventricular rate is typically very slow and escape rhythms are observed.
*Atrial fibrillation*
- **Atrial fibrillation** is an irregularly irregular rhythm with no discernible P waves and varying R-R intervals.
- The ECG provided shows clear P waves and a regular, albeit interrupted, rhythm pattern.
Ventricular arrhythmias US Medical PG Question 7: A 55-year-old man with a past medical history of obesity and hyperlipidemia suddenly develops left-sided chest pain and shortness of breath while at work. He relays to coworkers that the pain is intense and has spread to his upper left arm over the past 10 minutes. He reports it feels a lot like the “heart attack” he had a year ago. He suddenly collapses and is unresponsive. Coworkers perform cardiopulmonary resuscitation for 18 minutes until emergency medical services arrives. Paramedics pronounce him dead at the scene. Which of the following is the most likely cause of death in this man?
- A. Pericarditis
- B. Aortic dissection
- C. Atrial fibrillation
- D. Ventricular tachycardia (Correct Answer)
- E. Free wall rupture
Ventricular arrhythmias Explanation: ***Ventricular tachycardia***
- The patient's history of MI **1 year ago** creates a substrate of **scarred myocardium** that predisposes to life-threatening ventricular arrhythmias.
- The current presentation of sudden chest pain radiating to the arm suggests **acute re-infarction**, which triggers electrical instability in already compromised myocardium.
- **Ventricular tachycardia (VT)** degenerating to **ventricular fibrillation (VF)** is the **most common cause of sudden cardiac death** in patients with prior MI, especially during acute ischemic events.
- The rapid collapse and death within minutes, despite CPR, is classic for fatal ventricular arrhythmia.
*Free wall rupture*
- Free wall rupture is a **mechanical complication** that occurs **3-14 days** (typically days 3-7) after an **acute MI**, not 1 year later.
- By 1 year post-MI, the ventricular wall has either healed with fibrous scar tissue or formed a chronic ventricular aneurysm.
- While this would cause sudden death via cardiac tamponade, the **timing makes this unlikely** in this scenario.
*Pericarditis*
- Pericarditis causes **pleuritic chest pain** that is sharp, positional, and typically relieved by leaning forward.
- It is **not an immediate cause of sudden cardiac death** and would not explain the rapid collapse and unresponsiveness.
- While post-MI (Dressler) pericarditis can occur weeks after MI, it doesn't cause this presentation.
*Aortic dissection*
- Aortic dissection presents with **sudden, severe, tearing chest pain** often radiating to the back.
- While potentially fatal, the patient's description of pain "a lot like the heart attack he had a year ago" and his cardiac risk factors make **recurrent MI with fatal arrhythmia more likely**.
- No mention of blood pressure differential or pulse deficits that would suggest dissection.
*Atrial fibrillation*
- Atrial fibrillation is a **supraventricular arrhythmia** that causes palpitations, dyspnea, and irregular pulse.
- It is **not typically immediately fatal** in isolation and does not cause sudden collapse and death within minutes.
- While AF can lead to stroke or heart failure over time, it doesn't explain this acute sudden cardiac death.
Ventricular arrhythmias US Medical PG Question 8: A 40-year-old woman comes to the physician for a 6-month history of recurrent episodes of chest pain, racing pulse, dizziness, and difficulty breathing. The episodes last up to several minutes. She also reports urinary urgency and two episodes of loss of consciousness followed by spontaneous recovery. There is no personal or family history of serious illness. She does not smoke or drink alcohol. Vitals signs are within normal limits. Cardiopulmonary examination shows no abnormalities. Holter monitoring is performed. ECG recordings during episodes of tachycardia show a QRS duration of 100 ms, regular RR-interval, and absent P waves. Which of the following is the most likely underlying cause of this patient's condition?
- A. AV node with slow and fast pathway (Correct Answer)
- B. Pre-excitation of the ventricles
- C. Mutations in genes that code for myocyte ion channels
- D. Macroreentrant rhythm in the right atria through cavotricuspid isthmus
- E. Fibrosis of the sinoatrial node and surrounding myocardium
Ventricular arrhythmias Explanation: ***AV node with slow and fast pathway***
- This describes **AV nodal reentrant tachycardia (AVNRT)**, a common cause of **paroxysmal supraventricular tachycardia (PSVT)**. The ECG findings of **narrow QRS (100 ms)**, regular RR-interval, and **absent P waves** (often hidden within the QRS complex) are characteristic of AVNRT.
- The patient's symptoms of recurrent chest pain, racing pulse, dizziness, and spontaneous recovery from loss of consciousness fit the episodic nature of **AVNRT**. The presence of two pathways (slow and fast) within the AV node facilitates the reentrant circuit.
*Pre-excitation of the ventricles*
- **Pre-excitation syndromes** (e.g., Wolff-Parkinson-White syndrome) involve an accessory pathway that bypasses the AV node, leading to a **delta wave** and **short PR interval** on the baseline ECG.
- While they can cause SVT, the ECG during tachycardia would typically show a **wide QRS complex** if the accessory pathway is part of the reentrant circuit (antidromic), or a narrow QRS with a visible P wave if orthodromic and the accessory pathway is used for retrograde conduction, which doesn't fully align with the absent P waves and typically *normal* QRS during tachycardia as described.
*Mutations in genes that code for myocyte ion channels*
- This refers to **channelopathies** (e.g., long QT syndrome, Brugada syndrome), which predispose to **ventricular arrhythmias** like **polymorphic ventricular tachycardia** and **ventricular fibrillation**.
- These conditions typically cause **wide QRS tachycardias** and have distinct ECG patterns (e.g., prolonged QT interval, Brugada pattern) not described here. The narrow QRS and regular rhythm point away from primary ventricular channelopathies as the cause of this specific tachycardia.
*Macroreentrant rhythm in the right atria through cavotricuspid isthmus*
- This describes **atrial flutter**, which typically presents with characteristic **"sawtooth" F waves** on ECG, representing atrial activity.
- While atrial flutter can cause recurrent episodes of rapid heart rate, the ECG description of **absent P waves** and a **narrow QRS complex** without F waves makes atrial flutter less likely.
*Fibrosis of the sinoatrial node and surrounding myocardium*
- **Sinoatrial node dysfunction (sick sinus syndrome)** can lead to bradycardia, sinus pauses, or alternating bradycardia and tachycardia (tachy-brady syndrome).
- It does not primarily cause the described paroxysmal narrow-complex tachycardia with absent P waves. The patient's symptoms are more consistent with an abrupt-onset, regular supraventricular tachycardia.
Ventricular arrhythmias US Medical PG Question 9: A 62-year-old woman presents to the emergency department complaining of fever, worsening fatigue, and muscle weakness for the previous 48 hours. The patient describes her muscle weakness as symmetric and worse in the upper limbs. Her past medical history is significant for long-standing diabetes type 2 complicated by stage 5 chronic kidney disease (CKD) on hemodialysis. She takes lisinopril, verapamil, metformin, and glargine. Today, the patient’s vital signs include: temperature 38.6°C (101.5°F), pulse 80/min, blood pressure 155/89 mm Hg, respirations 24/min, and 95% oxygen saturation on room air. The cardiac and pulmonary exams are unremarkable. The abdomen is soft and non-tender. Her strength is 3/5 in the upper extremities and 4/5 in the lower extremities and her sensation is intact. Deep tendon reflexes are absent in both the upper and lower limbs. A 12-lead electrocardiogram (ECG) is shown in the image below. Blood work is drawn and the patient is admitted and started on continuous cardiac monitoring. Based on the available information, what is the next best step in managing this patient?
- A. Order a stat serum potassium level
- B. Administer IV calcium gluconate (Correct Answer)
- C. Emergency dialysis
- D. Administer IV sodium bicarbonate
- E. Administer regular insulin and 50% dextrose in water
Ventricular arrhythmias Explanation: ***Administer IV calcium gluconate***
- The patient's presentation with **symmetrical muscle weakness** (worse in upper limbs), **absent deep tendon reflexes**, and characteristic ECG changes (peaked T waves, prolonged PR interval, wide QRS) in the context of **end-stage renal disease** and hemodialysis strongly suggests **severe hyperkalemia**.
- **Intravenous calcium gluconate** is the first-line treatment for clinically significant hyperkalemia with ECG changes, as it directly antagonizes the cardiac membrane effects of potassium and helps to stabilize the myocardium.
*Order a stat serum potassium level*
- While it is crucial to confirm hyperkalemia with a **stat serum potassium level**, the clinical picture (CKD, hemodialysis, muscle weakness, absent reflexes, and ECG changes) is emergent and highly suggestive of severe hyperkalemia.
- Waiting for laboratory confirmation before administering calcium gluconate can delay life-saving treatment and is not the "next best step" when ECG changes are evident.
*Emergency dialysis*
- **Emergency dialysis** is an effective way to remove potassium from the body and is often needed in severe hyperkalemia, especially in ESRD patients.
- However, **calcium gluconate** should be administered *immediately* to stabilize the cardiac membrane and prevent life-threatening arrhythmias, even before preparing for dialysis.
*Administer IV sodium bicarbonate*
- **Sodium bicarbonate** can shift potassium intracellularly, particularly in the setting of metabolic acidosis, but its effect is slower and less reliable than calcium in stabilizing cardiac membranes.
- It is often used as an adjunct but not as the initial, most critical intervention for immediate cardiac stabilization in severe hyperkalemia.
*Administer regular insulin and 50% dextrose in water*
- **Insulin and dextrose** shift potassium into cells, thereby lowering serum potassium levels. This is an important step in managing hyperkalemia.
- However, similar to sodium bicarbonate, its effect on serum potassium is not immediate enough to counteract the acute cardiotoxic effects, making **calcium gluconate** the priority for cardiac stabilization.
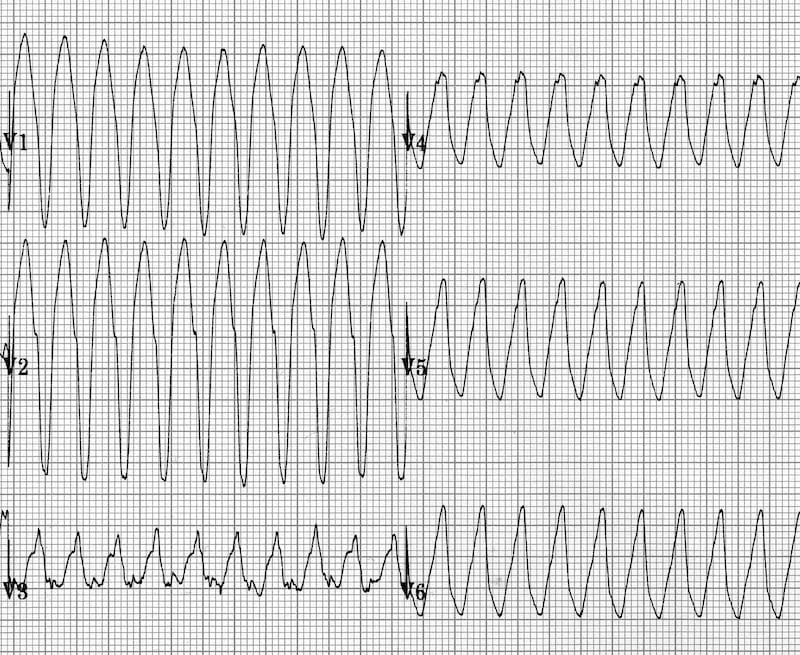
Ventricular arrhythmias US Medical PG Question 10: A 42-year-old man is brought to the emergency department 20 minutes after the sudden onset of severe chest pain, diaphoresis, shortness of breath, and palpitations. His symptoms occurred while he was at a party with friends. He has smoked one pack of cigarettes daily for 24 years. He uses cocaine occasionally. The last use was three hours ago. He appears pale. His pulse is 110/min, blood pressure is 178/106 mm Hg, and respirations are 24/min. His pupils are dilated and react sluggishly to light. The lungs are clear to auscultation. An ECG shows tachycardia and ST segment elevation in leads II, III, and aVF. While recording the ECG, the patient loses consciousness. A photo of the ECG at that point is shown. Which of the following is the most appropriate next step in management?
- A. Administer lidocaine
- B. Unsynchronized cardioversion (Correct Answer)
- C. Administer epinephrine
- D. Coronary angiography
- E. Synchronized cardioversion
Ventricular arrhythmias Explanation: ***Unsynchronized cardioversion***
- The ECG shows **ventricular fibrillation (VF)**, characterized by chaotic, irregular electrical activity without distinct QRS complexes, indicating a life-threatening arrhythmia.
- In a patient who has lost consciousness due to VF, immediate **defibrillation (unsynchronized cardioversion)** is crucial to restore normal sinus rhythm and prevent sudden cardiac death.
- Note: Unsynchronized cardioversion and defibrillation are **synonymous terms** for delivering an unsynchronized shock, with "defibrillation" being the preferred ACLS terminology for VF/pulseless VT.
*Administer lidocaine*
- While lidocaine is an **antiarrhythmic** used in some ventricular arrhythmias, it is typically administered after initial defibrillation attempts have failed or as an adjunct therapy.
- It is not the primary treatment for **unstable ventricular fibrillation**, which requires immediate electrical therapy.
*Administer epinephrine*
- Epinephrine is a **vasopressor** used during cardiac arrest to improve coronary and cerebral perfusion.
- It is administered during **cardiopulmonary resuscitation (CPR)** intervals, usually after initial defibrillation attempts, but not as the first line treatment for VF.
*Coronary angiography*
- Coronary angiography is an **invasive diagnostic procedure** to visualize coronary arteries and identify blockages, suggested by the patient's symptoms and ST elevation in the initial ECG leads.
- However, in the context of **cardiac arrest due to VF**, immediate life-saving interventions take precedence over diagnostic procedures.
*Synchronized cardioversion*
- **Synchronized cardioversion** delivers an electrical shock timed to the R-wave of the QRS complex to treat **tachyarrhythmias with a pulse** (e.g., ventricular tachycardia, atrial fibrillation with rapid ventricular response).
- It is **contraindicated in ventricular fibrillation** because there are no organized QRS complexes to synchronize with, and attempting synchronization can delay life-saving defibrillation.
More Ventricular arrhythmias US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.