Sudden cardiac death US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sudden cardiac death. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sudden cardiac death US Medical PG Question 1: A previously healthy 19-year-old man is brought to the emergency department by his girlfriend after briefly losing consciousness. He passed out while moving furniture into her apartment. She said that he was unresponsive for a minute but regained consciousness and was not confused. The patient did not have any chest pain, palpitations, or difficulty breathing before or after the episode. He has had episodes of dizziness when exercising at the gym. His blood pressure is 125/75 mm Hg while supine and 120/70 mm Hg while standing. Pulse is 70/min while supine and 75/min while standing. On examination, there is a grade 3/6 systolic murmur at the left lower sternal border and a systolic murmur at the apex, both of which disappear with passive leg elevation. Which of the following is the most likely cause?
- A. Prolonged QT interval
- B. Hypertrophic cardiomyopathy (Correct Answer)
- C. Mitral valve stenosis
- D. Mitral valve prolapse
- E. Bicuspid aortic valve
Sudden cardiac death Explanation: ***Hypertrophic cardiomyopathy***
- This patient's **syncope associated with exertion** (moving furniture) and episodes of **dizziness during exercise** are highly suggestive of hypertrophic cardiomyopathy (HCM).
- The presence of a **systolic murmur at the left sternal border and apex** that **decreases/disappears with passive leg elevation** indicates a dynamic left ventricular outflow tract (LVOT) obstruction that is sensitive to preload changes, a hallmark of HCM.
- Passive leg elevation **increases preload** → **increases LV volume** → **decreases LVOT obstruction** → **decreases murmur intensity**.
*Prolonged QT interval*
- While it can cause syncope, especially exertional, a prolonged QT interval generally **does not present with dynamic murmurs** that change with preload.
- ECG findings (not mentioned here) would be the primary diagnostic clue, not physical exam findings related to murmurs.
*Mitral valve stenosis*
- Mitral stenosis would typically present with a **diastolic murmur** (not systolic) and symptoms like dyspnea, fatigue, and possibly hemoptysis due to elevated left atrial pressure.
- The murmur of mitral stenosis would not characteristically change with passive leg elevation in the manner described.
*Mitral valve prolapse*
- Mitral valve prolapse often presents with a **mid-systolic click** followed by a systolic murmur, which typically **intensifies with standing** or maneuvers that decrease left ventricular volume.
- The murmur described here decreases with leg elevation (increased preload), which is the opposite behavior of a mitral prolapse murmur.
*Bicuspid aortic valve*
- A bicuspid aortic valve can cause an **aortic stenosis murmur** (a systolic ejection murmur heard best at the right upper sternal border) or regurgitation, but it generally **does not cause a dynamic murmur that changes with preload** in this characteristic fashion.
- Symptoms related to bicuspid aortic valve disease (like syncope) would more commonly be associated with significant stenosis, not with a murmur that is acutely sensitive to preload changes.
Sudden cardiac death US Medical PG Question 2: A 16-year-old male presents to the cardiologist after passing out during a basketball practice. An echocardiogram confirmed the diagnosis of hypertrophic cardiomyopathy. The cardiologist advises that a pacemaker must be implanted to prevent any further complications and states the player cannot play basketball anymore. Unfortunately, the coach objects to sidelining the player since a big game against their rivals is next week. The coach asks if the pacemaker can be implanted after the game, which of the following steps should the physician take?
- A. Postpone the procedure so the patient can play
- B. Allow the patient to play and schedule a follow up after the game
- C. Recommend to the legal guardian that the player stop playing and have the procedure performed (Correct Answer)
- D. Perform the procedure immediately so that both the physician and coach's wishes may be fulfilled
- E. Allow the patient to make the decision regarding his health
Sudden cardiac death Explanation: ***Recommend to the legal guardian that the player stop playing and have the procedure performed***
- The physician's primary ethical duty is **beneficence** and **non-maleficence**, meaning acting in the patient's best interest and preventing harm.
- Playing basketball with **hypertrophic cardiomyopathy** carries a significant risk of sudden cardiac death, making it medically unsafe regardless of the coach's objections.
*Postpone the procedure so the patient can play*
- This option disregards the **immediate and severe risks** associated with hypertrophic cardiomyopathy during strenuous physical activity.
- Postponing the procedure for a game prioritizes a non-medical event over the patient's life-saving treatment, violating the principle of **patient safety**.
*Allow the patient to play and schedule a follow up after the game*
- This is medically irresponsible, as it exposes the patient to a high risk of **sudden cardiac arrest** during the game.
- Delaying urgent intervention for a non-medical reason fails to uphold the physician's obligation to protect the patient from **foreseeable harm**.
*Perform the procedure immediately so that both the physician and coach's wishes may be fulfilled*
- While performing the procedure immediately is medically sound, stating that the coach's wishes can be fulfilled is inaccurate if the player is being sidelined.
- The physician's advice to stop playing basketball stems from medical necessity, which directly conflicts with the coach's desire for the player to participate, thus **not fulfilling both wishes**.
*Allow the patient to make the decision regarding his health*
- While patient autonomy is important, a **16-year-old** is typically considered a minor and cannot make high-risk medical decisions without the consent of a **legal guardian**.
- In situations of significant risk to life, the physician has a responsibility to guide the patient and their guardians towards the safest medical option, rather than simply deferring to the patient's potentially uninformed decision.
Sudden cardiac death US Medical PG Question 3: A previously healthy 20-year-old man is brought to the emergency department 15 minutes after collapsing while playing basketball. He has no history of serious illness. On arrival, there is no palpable pulse or respiratory effort observed. He is declared dead. The family agrees to an autopsy. Cardiac workup prior to this patient's death would most likely have shown which of the following findings?
- A. Systolic anterior motion of the mitral valve (Correct Answer)
- B. Narrowing of the left main coronary artery
- C. Bicuspid aortic valve
- D. Asymmetric septal hypertrophy
- E. Ventricular septal defect
Sudden cardiac death Explanation: ***Systolic anterior motion of the mitral valve***
- This finding is characteristic of **hypertrophic cardiomyopathy (HCM)**, the most common cause of sudden cardiac death in young athletes.
- **Systolic anterior motion (SAM)** of the mitral valve leads to **left ventricular outflow tract (LVOT) obstruction**, which can precipitate fatal arrhythmias during exertion.
- While asymmetric septal hypertrophy is the underlying anatomical abnormality in HCM, **SAM is the dynamic functional finding** on echocardiography that directly explains the mechanism of sudden death during exercise due to LVOT obstruction.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** is a congenital heart defect that typically presents with a **murmur** and may lead to heart failure or pulmonary hypertension if large.
- While VSDs can cause complications, they are not typically associated with sudden cardiac death in a previously healthy young adult collapsing during exertion without prior symptoms.
*Narrowing of the left main coronary artery*
- Significant **coronary artery disease (CAD)**, especially of the left main, is a common cause of sudden cardiac death but is rare in a **20-year-old** without significant risk factors.
- When coronary anomalies occur in young individuals causing sudden death, it's typically due to **anomalous coronary artery origin** rather than atherosclerotic narrowing.
*Bicuspid aortic valve*
- A **bicuspid aortic valve** is a congenital malformation that can lead to **aortic stenosis** or **regurgitation**, or an increased risk of aortic dissection.
- While it can be associated with sudden cardiac events, it is less commonly implicated in sudden cardiac death in an otherwise healthy young athlete during exertion compared to HCM.
*Asymmetric septal hypertrophy*
- This describes the **morphological hallmark** of **hypertrophic cardiomyopathy (HCM)** where the **interventricular septum** is disproportionately thickened (≥15 mm or septal-to-free wall ratio ≥1.3).
- While this is the diagnostic anatomical finding for HCM, **systolic anterior motion (SAM) of the mitral valve** is the specific *dynamic functional abnormality* seen on cardiac workup that directly causes LVOT obstruction and explains the mechanism of sudden death during exercise in this clinical scenario.
Sudden cardiac death US Medical PG Question 4: A 19-year-old woman is brought to the emergency department by ambulance 30 minutes after her neighbor found her unconscious on a running trail. Her neighbor reports that she has been training for a marathon since the beginning of the summer. She is alert and oriented but becomes irritable when realizing that she is at a hospital and refuses to answer questions. She appears tired. She is 174 cm (5 ft 7 in) tall and weighs 51 kg (112 lb). Her temperature is 35.5°C (96°F), pulse is 44/min, respirations are 20/min, and blood pressure is 84/48 mm Hg. Examination shows dry, scaly skin and dry mucous membranes. Cardiopulmonary examination shows a high-frequency, mid-to-late systolic murmur that is heard best at the apex. Her hemoglobin concentration is 11.9 g/dL. Which of the following is the most likely diagnosis?
- A. Heat exhaustion
- B. Hypertrophic obstructive cardiomyopathy
- C. Hypothyroidism
- D. Amphetamine use
- E. Anorexia nervosa (Correct Answer)
Sudden cardiac death Explanation: ***Anorexia nervosa***
- The patient's **low BMI** (16.9 kg/m^2), **bradycardia**, **hypotension**, **hypothermia**, and **dry, scaly skin** are classic signs of anorexia nervosa, exacerbated by intense exercise (marathon training).
- The **mid-to-late systolic murmur** heard best at the apex is likely due to **mitral valve prolapse**, a common cardiac finding in patients with severe anorexia nervosa due to decreased ventricular size and structural changes.
*Heat exhaustion*
- Although the patient was exercising, her **temperature is low (96°F)**, which contradicts the expected elevated temperature in heat exhaustion.
- Heat exhaustion typically presents with profuse sweating, not **dry mucous membranes** or **dry, scaly skin**.
*Hypertrophic obstructive cardiomyopathy*
- While it can cause a **systolic murmur** and exercise-induced syncope, it usually presents with a **loud S4**, and the patient's other symptoms like **hypothermia**, **bradycardia**, and severe **cachexia** are not typical.
- It would not explain the **low body weight**, **dry skin**, or **hypotension** as primary symptoms.
*Hypothyroidism*
- Hypothyroidism can cause **fatigue**, **bradycardia**, **hypothermia**, and **dry skin**, but it does not typically lead to such extreme **weight loss** or **hypotension** in a young, active individual.
- It doesn't explain the specific cardiac murmur described or the history of intense marathon training contributing to the presentation.
*Amphetamine use*
- Amphetamine use typically causes **tachycardia**, **hypertension**, **dilation of pupils**, and **hyperthermia**, which are opposite to this patient's presentation of bradycardia, hypotension, and hypothermia.
- The patient's **cachectic appearance** could be associated with stimulant use, but the vital signs and overall clinical picture strongly contradict it.
Sudden cardiac death US Medical PG Question 5: You are the team physician for an NBA basketball team. On the morning of an important playoff game, an EKG of a star player, Mr. P, shows findings suspicious for hypertrophic cardiomyopathy (HCM). Mr. P is an otherwise healthy, fit, professional athlete.
The playoff game that night is the most important of Mr. P's career. When you inform the coach that you are thinking of restricting Mr. P's participation, he threatens to fire you. Later that day you receive a phone call from the owner of the team threatening a lawsuit should you restrict Mr. P's ability to play. Mr. P states that he will be playing in the game "if it's the last thing I do."
Which of the following is the most appropriate next step?
- A. Allow Mr. P to play against medical advice
- B. Consult with a psychiatrist to have Mr. P committed
- C. Call the police and have Mr. P arrested
- D. Schedule a repeat EKG for the following morning
- E. Educate Mr. P about the risks of HCM and restrict him from playing pending cardiology evaluation (Correct Answer)
Sudden cardiac death Explanation: ***Educate Mr. P about the risks of HCM and restrict him from playing pending cardiology evaluation***
- The physician's primary ethical duty is to **protect the patient's well-being** (beneficence and non-maleficence), especially when there is a significant risk of sudden cardiac death associated with **hypertrophic cardiomyopathy (HCM)** during strenuous activity.
- While navigating external pressures, the physician must uphold professional standards by **educating the patient** about the risks and **restricting high-risk activities** until a definitive diagnosis and management plan from a cardiologist can be established.
*Allow Mr. P to play against medical advice*
- Allowing Mr. P to play against medical advice would be a **breach of the physician's ethical duty** to prevent harm, especially given the high risk of **sudden cardiac death** associated with HCM in athletes.
- This action could also expose the physician to **legal liability** should Mr. P suffer an adverse cardiac event during the game.
*Consult with a psychiatrist to have Mr. P committed*
- There is no indication that Mr. P is a danger to himself or others due to a **mental health crisis** requiring commitment; his desire to play is driven by external pressures and personal ambition, not a psychiatric condition.
- Committing Mr. P against his will would be an **unwarranted and extreme measure**, infringing on his autonomy without appropriate medical justification.
*Call the police and have Mr. P arrested*
- Calling the police to arrest Mr. P is an **inappropriate and disproportionate response** to a medical disagreement, as it does not address the medical issue or the ethical obligations of the physician.
- This action would severely damage the **physician-patient relationship** and would not be a valid legal or ethical approach to managing the situation.
*Schedule a repeat EKG for the following morning*
- Delaying further diagnostic evaluation until the following morning keeps Mr. P’s participation in the immediate playoff game an option, despite the **urgent suspicion of HCM**, which carries a high risk of **sudden cardiac death during exertion**.
- A repeat EKG alone is insufficient; **immediate cardiac evaluation** (e.g., echocardiogram) is necessary to confirm or rule out HCM before allowing him to play.
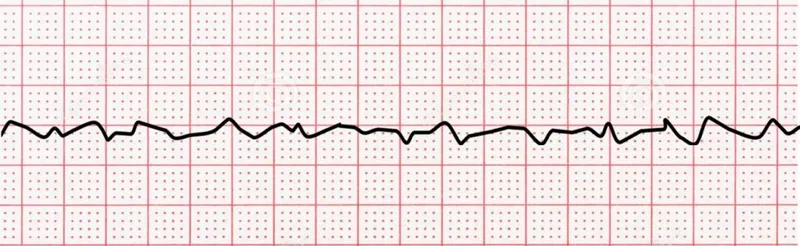
Sudden cardiac death US Medical PG Question 6: A 72-year-old man is taken to the emergency room after losing consciousness. According to his wife, he suddenly complained of fluttering in his chest, lightheadedness, and profuse sweating while walking to the grocery store. He then turned gray, lost consciousness, and collapsed onto the ground. His medical history is significant for a prior anterior wall myocardial infarction 2 years ago that was complicated by severe left ventricular systolic dysfunction. His blood pressure is 80/50 mm Hg, the temperature is 36.7°C (98.0°F), and the carotid pulse is not palpable. An ECG was obtained and the results are shown in the picture. Cardiopulmonary resuscitation is initiated and the patient is cardioverted to sinus rhythm with an external defibrillator. The patient regains consciousness and states there was no antecedent chest discomfort. Cardiac enzymes are negative and serum electrolytes are normal. Which of the following is the best next step for this patient?
- A. Intravenous magnesium sulphate
- B. Intravenous adenosine
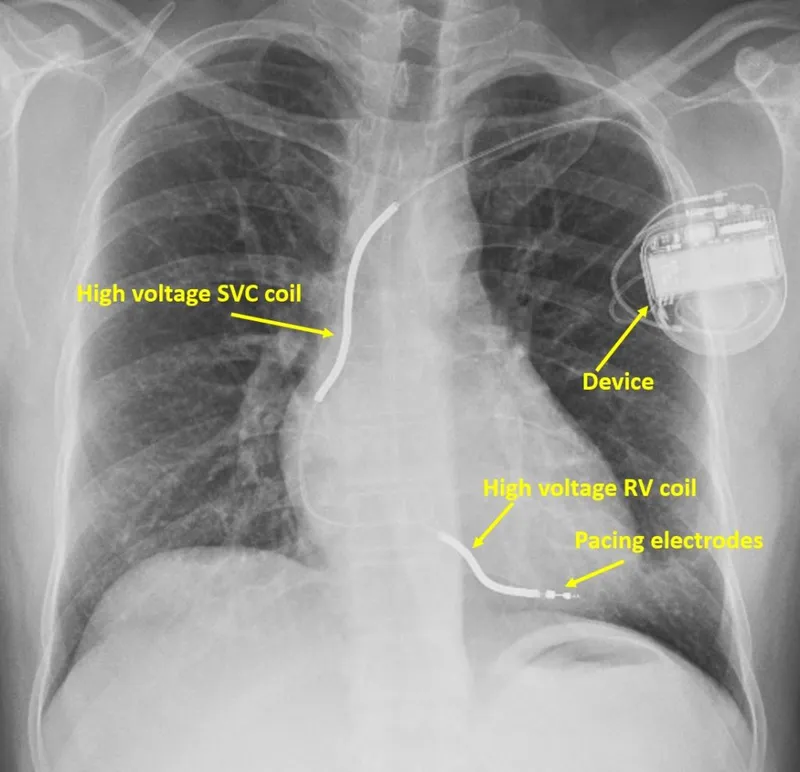
- C. Implantable cardioverter-defibrillator (Correct Answer)
- D. Intravenous metoprolol
- E. Temporary or permanent cardiac pacing
Sudden cardiac death Explanation: ***Implantable cardioverter-defibrillator***
- The patient experienced **sudden cardiac arrest (SCA)** due to a **lethal ventricular arrhythmia (ventricular tachycardia progressing to ventricular fibrillation)**, suggested by the syncopal episode, unrecordable pulse, and successful defibrillation.
- Given the history of severe **left ventricular systolic dysfunction** (LVEF <35-40%) post-MI, he is at high risk for recurrence, making an **ICD** the most appropriate intervention for secondary prevention of SCA.
*Intravenous magnesium sulphate*
- **Magnesium sulfate** is primarily used for the treatment of **Torsades de Pointes**, a polymorphic VT often associated with a prolonged QT interval.
- The provided ECG (though not visible here, the clinical context implies a monomorphic VT or VF) and history do not specifically suggest Torsades de Pointes.
*Intravenous adenosine*
- **Adenosine** is the drug of choice for terminating **supraventricular tachycardias (SVTs)** by transiently blocking the AV node.
- It is **contraindicated** in wide-complex tachycardias of uncertain origin, especially in patients with structural heart disease, as it can worsen ventricular arrhythmias.
*Intravenous metoprolol*
- **Beta-blockers** like metoprolol are used to slow heart rate, reduce myocardial oxygen demand, and can be helpful in some forms of VT, but they are not the definitive treatment for **hemodynamically unstable** VT or for preventing future SCA in a patient with severe LV dysfunction.
- Administering a beta-blocker during an acute, unstable event could worsen hypotension.
*Temporary or permanent cardiac pacing*
- **Cardiac pacing** is indicated for **bradyarrhythmias** or some forms of **tachycardia** (e.g., overdrive pacing for recurrent VT), but it is not the primary treatment for preventing SCA from ventricular fibrillation in a patient with severe LV dysfunction like this.
- The patient's presentation was due to a fast, lethal arrhythmia, not a slow rhythm.
Sudden cardiac death US Medical PG Question 7: A 22-year-old woman presents to the emergency department feeling lightheaded and states that her heart is racing. She does not have a history of any chronic medical conditions. She is a college sophomore and plays club volleyball. Although she feels stressed about her upcoming final exams next week, she limits her caffeine intake to 3 cups of coffee per day to get a good night sleep. She notes that her brother takes medication for some type of heart condition, but she does not know the name of it. Both her parents are alive and well. She denies recent illness, injuries, or use of cigarettes, alcohol, or recreational drugs. The pertinent negatives from the review of systems include an absence of fever, nausea, vomiting, sweating, fatigue, or change in bowel habits. The vital signs include: temperature 36.8°C (98.2°F), heart rate 125/min, respiratory rate 15/min, blood pressure 90/75 mm Hg, and oxygen saturation of 100% on room air. The laboratory results are within normal limits. The ECG is significant for a shortened PR interval and widened QRS. Which of the following medications should the patient avoid in this scenario?
- A. Amlodipine
- B. Procainamide
- C. Diltiazem
- D. Verapamil (Correct Answer)
- E. Metoprolol
Sudden cardiac death Explanation: ***Verapamil***
- The ECG findings of a **shortened PR interval** and **widened QRS** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, an accessory pathway that can bypass the AV node.
- Verapamil is a **non-dihydropyridine calcium channel blocker** that blocks the AV node and can paradoxically increase conduction down the accessory pathway in WPW, potentially leading to **ventricular fibrillation** if an atrial tachyarrhythmia is present.
- **Verapamil is the most classically contraindicated medication in WPW syndrome** and is the prototype drug to avoid in this condition.
*Amlodipine*
- Amlodipine is a **dihydropyridine calcium channel blocker** primarily used for hypertension and angina.
- It has minimal effect on the AV node and does not carry the same risk as non-dihydropyridine calcium channel blockers in WPW syndrome.
*Procainamide*
- **Procainamide is a Class Ia antiarrhythmic** that can be used to treat tachyarrhythmias related to WPW syndrome, as it prolongs the refractory period of the accessory pathway.
- It would be a potential **treatment option**, not a medication to avoid, especially for antidromic atrioventricular reentrant tachycardia (AVRT) in WPW.
*Diltiazem*
- Similar to verapamil, diltiazem is a **non-dihydropyridine calcium channel blocker** that blocks the AV node.
- While it carries similar risks to verapamil in WPW syndrome, **verapamil is more classically emphasized** as the prototypical contraindicated medication in medical education and board examinations.
*Metoprolol*
- Metoprolol is a **beta-blocker** that slows conduction through the AV node.
- While beta-blockers are also generally **avoided in WPW syndrome with atrial fibrillation**, **AV nodal blocking calcium channel blockers (especially verapamil) are considered the primary contraindication** due to more pronounced effects on accessory pathway conduction.
Sudden cardiac death US Medical PG Question 8: A previously healthy 21-year-old man is brought to the emergency department for the evaluation of an episode of unconsciousness that suddenly happened while playing football 30 minutes ago. He was not shaking and regained consciousness after about 30 seconds. Over the past three months, the patient has had several episodes of shortness of breath while exercising as well as sensations of a racing heart. He does not smoke or drink alcohol. He takes no medications. His vital signs are within normal limits. On mental status examination, he is oriented to person, place, and time. Cardiac examination shows a systolic ejection murmur that increases with valsalva maneuver and standing and an S4 gallop. The remainder of the examination shows no abnormalities. An ECG shows a deep S wave in lead V1 and tall R waves in leads V5 and V6. Echocardiography is most likely to show which of the following findings?
- A. Mitral valve leaflet thickening ≥ 5 mm
- B. Ventricular septum defect
- C. Abnormal movement of the mitral valve (Correct Answer)
- D. Reduced left ventricular ejection fraction
- E. Symmetric left ventricular wall thickening
Sudden cardiac death Explanation: ***Abnormal movement of the mitral valve***
- This patient's presentation with exercise-induced syncope, shortness of breath, palpitations, a systolic ejection murmur that increases with **Valsalva maneuver** and **standing**, and ECG findings of **left ventricular hypertrophy** (deep S in V1, tall R in V5-V6) is highly suggestive of **hypertrophic cardiomyopathy (HCM)**.
- In HCM, the **hypertrophied septum** obstructs outflow, leading to **systolic anterior motion (SAM) of the mitral valve**, which an echocardiogram would reveal as abnormal movement.
*Mitral valve leaflet thickening ≥ 5 mm*
- Marked **mitral valve leaflet thickening** is typically associated with **rheumatic heart disease** or significant valvular degeneration.
- While HCM can affect mitral valve function, significant structural thickening to this extent is not its primary or diagnostic echocardiographic feature.
*Ventricular septum defect*
- A **ventricular septum defect (VSD)** is a congenital heart defect characterized by a hole in the septum separating the ventricles.
- While VSDs can cause murmurs, the characteristic murmur variations with Valsalva and standing, and the ECG findings in this case, are not typical of an isolated VSD.
*Reduced left ventricular ejection fraction*
- **Hypertrophic cardiomyopathy** is usually characterized by a **preserved or even hyperdynamic left ventricular ejection fraction** in the early stages, despite impaired diastolic function.
- **Reduced LVEF** is seen in **dilated cardiomyopathy** or advanced stages of other heart diseases.
*Symmetric left ventricular wall thickening*
- While there is **left ventricular wall thickening** in HCM, it is characteristically **asymmetric**, primarily affecting the **interventricular septum**.
- **Symmetric wall thickening** is more indicative of conditions like **hypertensive heart disease** or **athlete's heart**, rather than HCM.
Sudden cardiac death US Medical PG Question 9: A 55-year-old man with a past medical history of obesity and hyperlipidemia suddenly develops left-sided chest pain and shortness of breath while at work. He relays to coworkers that the pain is intense and has spread to his upper left arm over the past 10 minutes. He reports it feels a lot like the “heart attack” he had a year ago. He suddenly collapses and is unresponsive. Coworkers perform cardiopulmonary resuscitation for 18 minutes until emergency medical services arrives. Paramedics pronounce him dead at the scene. Which of the following is the most likely cause of death in this man?
- A. Pericarditis
- B. Aortic dissection
- C. Atrial fibrillation
- D. Ventricular tachycardia (Correct Answer)
- E. Free wall rupture
Sudden cardiac death Explanation: ***Ventricular tachycardia***
- The patient's history of MI **1 year ago** creates a substrate of **scarred myocardium** that predisposes to life-threatening ventricular arrhythmias.
- The current presentation of sudden chest pain radiating to the arm suggests **acute re-infarction**, which triggers electrical instability in already compromised myocardium.
- **Ventricular tachycardia (VT)** degenerating to **ventricular fibrillation (VF)** is the **most common cause of sudden cardiac death** in patients with prior MI, especially during acute ischemic events.
- The rapid collapse and death within minutes, despite CPR, is classic for fatal ventricular arrhythmia.
*Free wall rupture*
- Free wall rupture is a **mechanical complication** that occurs **3-14 days** (typically days 3-7) after an **acute MI**, not 1 year later.
- By 1 year post-MI, the ventricular wall has either healed with fibrous scar tissue or formed a chronic ventricular aneurysm.
- While this would cause sudden death via cardiac tamponade, the **timing makes this unlikely** in this scenario.
*Pericarditis*
- Pericarditis causes **pleuritic chest pain** that is sharp, positional, and typically relieved by leaning forward.
- It is **not an immediate cause of sudden cardiac death** and would not explain the rapid collapse and unresponsiveness.
- While post-MI (Dressler) pericarditis can occur weeks after MI, it doesn't cause this presentation.
*Aortic dissection*
- Aortic dissection presents with **sudden, severe, tearing chest pain** often radiating to the back.
- While potentially fatal, the patient's description of pain "a lot like the heart attack he had a year ago" and his cardiac risk factors make **recurrent MI with fatal arrhythmia more likely**.
- No mention of blood pressure differential or pulse deficits that would suggest dissection.
*Atrial fibrillation*
- Atrial fibrillation is a **supraventricular arrhythmia** that causes palpitations, dyspnea, and irregular pulse.
- It is **not typically immediately fatal** in isolation and does not cause sudden collapse and death within minutes.
- While AF can lead to stroke or heart failure over time, it doesn't explain this acute sudden cardiac death.
Sudden cardiac death US Medical PG Question 10: A 22-year-old medical student presents to a community health center due to an episode of loss of consciousness 3 days ago. She also has a history of multiple episodes of dizziness in the last year. These episodes almost always occur when she is observing surgery in the operating room. She describes her dizziness as a feeling of lightheadedness, warmth, excessive sweating, and palpitations. She feels that she will fall down if she stood longer and usually sits on the floor or leaves the room until the feeling subsides. Three days ago, she collapsed while observing an open cholecystectomy but regained consciousness after a few seconds. Once she regained consciousness, she was pale and sweating excessively. Her medical history is significant for migraines, but she is not on prophylactic therapy. Her younger brother has cerebral palsy, and her uncle had a sudden death at the age of 25. Her blood pressure is 120/80 mm Hg when lying down and 118/80 mm Hg when in a standing position. The rest of the physical examination is within normal limits. What is the next best step in the management of this patient?
- A. Electroencephalogram (EEG)
- B. MRI of the brain
- C. Psychiatric evaluation for anxiety
- D. Echocardiogram
- E. Electrocardiogram (ECG) (Correct Answer)
Sudden cardiac death Explanation: ***Electrocardiogram (ECG)***
- This patient presents with recurrent episodes of near-syncope and a recent syncopal episode, triggered by a stressful situation (observing surgery), along with a family history of **sudden death at a young age** (uncle at 25). These red flags suggest a possible **cardiac etiology** for her syncope, such as a **long QT syndrome** or other channelopathies, making an ECG the most crucial initial investigation.
- An ECG is a **non-invasive, inexpensive, and readily available** test that can detect structural or electrical abnormalities of the heart that could predispose to arrhythmias and syncope.
*Electroencephalogram (EEG)*
- While loss of consciousness occurred, the clinical description of lightheadedness, warmth, sweating, and palpitations followed by syncope and quick recovery with post-recovery pallor and sweating is more consistent with **vasovagal syncope** or a cardiac cause, rather than a seizure.
- The absence of typical seizure features such as **tonic-clonic movements**, post-ictal confusion, or tongue biting makes epilepsy less likely.
*MRI of the brain*
- **Brain imaging** is generally not indicated for the initial workup of syncope unless there are focal neurological deficits, head trauma, or other symptoms suggestive of a central nervous system pathology.
- The patient's symptoms are classic for syncope and do not point to a **structural brain lesion** as the cause of her loss of consciousness.
*Psychiatric evaluation for anxiety*
- While anxiety can trigger vasovagal responses, the primary concern in this case, given the **recurrent nature of syncope** and the concerning **family history of sudden death**, is to rule out a potentially life-threatening cardiac cause before attributing it solely to psychological factors.
- Attributing syncope to anxiety without a thorough cardiac workup could delay diagnosis of a serious underlying condition.
*Echocardiogram*
- An echocardiogram assesses the **heart's structure and function**, which is important in the workup of syncope. However, it is typically performed *after* an ECG, especially if the ECG reveals abnormalities suggesting a structural or electrical problem.
- While it could be a subsequent step if the ECG is abnormal, the **ECG is the most immediate and informative initial step** for ruling out electrical cardiac issues.
More Sudden cardiac death US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.