Inherited arrhythmia syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Inherited arrhythmia syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Inherited arrhythmia syndromes US Medical PG Question 1: A 43-year-old woman presents to her primary care provider with shortness of breath. She reports a 4-month history of progressively worsening difficulty breathing with associated occasional chest pain. She is a long-distance runner but has had trouble running recently due to her breathing difficulties. Her past medical history is notable for well-controlled hypertension for which she takes hydrochlorothiazide. She had a tibial osteosarcoma lesion with pulmonary metastases as a child and successfully underwent chemotherapy and surgical resection. She has a 10 pack-year smoking history but quit 15 years ago. She drinks a glass of wine 3 times per week. Her temperature is 98.6°F (37°C), blood pressure is 140/85 mmHg, pulse is 82/min, and respirations are 18/min. On exam, she has increased work of breathing with a normal S1 and loud P2. An echocardiogram in this patient would most likely reveal which of the following?
- A. Biventricular dilatation with a decreased ejection fraction
- B. Left ventricular dilatation with an incompetent aortic valve
- C. Left atrial dilatation with mitral valve stenosis
- D. Right ventricular hypertrophy with a dilated pulmonary artery (Correct Answer)
- E. Left ventricular hypertrophy with a bicuspid aortic valve
Inherited arrhythmia syndromes Explanation: The patient's history of **pulmonary metastases** (even successfully treated) and a **loud P2 heart sound** suggest **pulmonary hypertension**, which leads to increased afterload on the right ventricle. [1] **Pulmonary hypertension** causes the **right ventricle to hypertrophy** to overcome the elevated pulmonary arterial pressure, and the **pulmonary artery itself often dilates** due to the sustained high pressure. [1] [2] This describes **dilated cardiomyopathy**, which typically presents with **symptoms of heart failure** but doesn't specifically explain the **loud P2**, which points to pulmonary hypertension. [2]
Inherited arrhythmia syndromes US Medical PG Question 2: An ECG from an 8-year-old male with neurosensory deafness and a family history of sudden cardiac arrest demonstrates QT-interval prolongation. Which of the following is this patient most at risk of developing?
- A. Hypertrophic cardiac myopathy
- B. Cardiac tamponade
- C. Essential hypertension
- D. Torsades de pointes (Correct Answer)
- E. First degree atrioventricular block
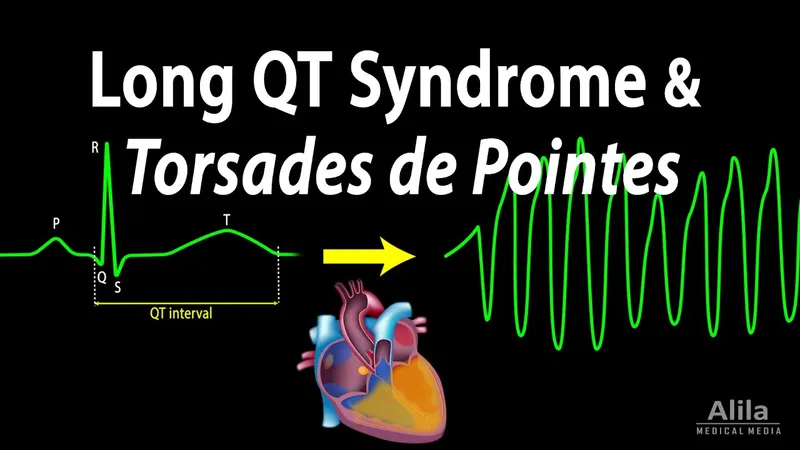
Inherited arrhythmia syndromes Explanation: ***Torsades de pointes***
- The combination of **neurosensory deafness**, **QT-interval prolongation**, and a family history of **sudden cardiac arrest** is highly suggestive of **Jervell and Lange-Nielsen syndrome**, a form of **long QT syndrome**.
- Patients with long QT syndrome are at significant risk for developing **polymorphic ventricular tachycardia** known as **Torsades de pointes**, which can degenerate into **ventricular fibrillation** and cause sudden cardiac death.
*Hypertrophic cardiac myopathy*
- This condition involves thickening of the **ventricular walls** and is associated with outflow tract obstruction, not primarily with QT prolongation.
- While it can cause sudden cardiac arrest, it typically presents with symptoms like **dyspnea, chest pain**, or syncope during exertion, and its ECG findings usually include **left ventricular hypertrophy** and **deep Q waves**.
*Cardiac tamponade*
- **Cardiac tamponade** results from the accumulation of fluid in the **pericardial sac**, compressing the heart and impairing its filling.
- This condition is not related to **QT prolongation** or **sensorineural deafness** and would present with signs of **hemodynamic instability**, such as **pulsus paradoxus** and muffled heart sounds.
*Essential hypertension*
- **Essential hypertension** is chronic high blood pressure with no identifiable secondary cause, commonly affecting adults.
- It is not associated with **congenital neurosensory deafness** or significant **QT-interval prolongation** in childhood.
*First degree atrioventricular block*
- **First-degree AV block** is characterized by a prolonged **PR interval** on ECG, indicating delayed conduction through the AV node.
- While it's an electrical abnormality, it is distinct from **QT prolongation** and is not typically associated with **neurosensory deafness** or the same risk of sudden cardiac arrest as long QT syndrome.
Inherited arrhythmia syndromes US Medical PG Question 3: An 8-year-old girl is brought to the physician by her parents for the evaluation of an episode of unconsciousness while at the playground that morning. She was unconscious for about 15 seconds and did not shake, bite her tongue, or lose bowel or bladder control. Her grandfather died suddenly at the age of 29 of an unknown heart condition; her parents are both healthy. An ECG shows sinus rhythm and a QT interval corrected for heart rate (QTc) of 470 milliseconds. Laboratory studies are within normal limits. Which of the following is the most likely additional finding in this patient?
- A. Oblique palpebral fissures
- B. Subvalvular ventricular outflow obstruction murmur
- C. Sensorineural hearing loss (Correct Answer)
- D. Brachial-femoral pulse delay
- E. Skin folds between the mastoid process and acromion
Inherited arrhythmia syndromes Explanation: ***Sensorineural hearing loss***
- This patient presents with an episode of syncope, a **prolonged QTc interval** (470 ms; normal <450 ms in prepubertal females, diagnostic threshold >460 ms), and a family history of **sudden cardiac death**, highly suggestive of **Long QT syndrome (LQTS)**.
- **Jervell and Lange-Nielsen syndrome** is a specific form of LQTS (autosomal recessive) characterized by both **prolonged QT interval** and **congenital sensorineural hearing loss**, making this the most likely additional finding.
*Oblique palpebral fissures*
- **Oblique palpebral fissures**, along with epicanthal folds and a flat facial profile, are characteristic features of **Down syndrome (Trisomy 21)**.
- These features are not typically associated with cardiac arrhythmias or Long QT syndrome, and there is no other information to suggest a chromosomal abnormality.
*Subvalvular ventricular outflow obstruction murmur*
- A **subvalvular ventricular outflow obstruction murmur** is indicative of conditions like **hypertrophic obstructive cardiomyopathy (HOCM)**.
- While HOCM can cause syncope and sudden cardiac death, the primary finding in this patient is a **prolonged QTc interval**, which is characteristic of LQTS, not HOCM.
*Brachial-femoral pulse delay*
- A **brachial-femoral pulse delay** is the classic physical exam finding for **coarctation of the aorta**, a congenital narrowing of the aorta.
- There is no clinical information to suggest coarctation, and it does not explain the prolonged QTc interval and family history of sudden cardiac death.
*Skin folds between the mastoid process and acromion*
- **Skin folds between the mastoid process and acromion** (webbed neck or pterygium colli) are a classic sign of **Turner syndrome (XO)** or **Noonan syndrome**.
- These conditions are not primarily associated with a prolonged QTc interval and exert their cardiac effects through structural defects like coarctation or pulmonary stenosis, not typically primary arrhythmias.
Inherited arrhythmia syndromes US Medical PG Question 4: A 40-year-old woman comes to the physician for a 6-month history of recurrent episodes of chest pain, racing pulse, dizziness, and difficulty breathing. The episodes last up to several minutes. She also reports urinary urgency and two episodes of loss of consciousness followed by spontaneous recovery. There is no personal or family history of serious illness. She does not smoke or drink alcohol. Vitals signs are within normal limits. Cardiopulmonary examination shows no abnormalities. Holter monitoring is performed. ECG recordings during episodes of tachycardia show a QRS duration of 100 ms, regular RR-interval, and absent P waves. Which of the following is the most likely underlying cause of this patient's condition?
- A. AV node with slow and fast pathway (Correct Answer)
- B. Pre-excitation of the ventricles
- C. Mutations in genes that code for myocyte ion channels
- D. Macroreentrant rhythm in the right atria through cavotricuspid isthmus
- E. Fibrosis of the sinoatrial node and surrounding myocardium
Inherited arrhythmia syndromes Explanation: ***AV node with slow and fast pathway***
- This describes **AV nodal reentrant tachycardia (AVNRT)**, a common cause of **paroxysmal supraventricular tachycardia (PSVT)**. The ECG findings of **narrow QRS (100 ms)**, regular RR-interval, and **absent P waves** (often hidden within the QRS complex) are characteristic of AVNRT.
- The patient's symptoms of recurrent chest pain, racing pulse, dizziness, and spontaneous recovery from loss of consciousness fit the episodic nature of **AVNRT**. The presence of two pathways (slow and fast) within the AV node facilitates the reentrant circuit.
*Pre-excitation of the ventricles*
- **Pre-excitation syndromes** (e.g., Wolff-Parkinson-White syndrome) involve an accessory pathway that bypasses the AV node, leading to a **delta wave** and **short PR interval** on the baseline ECG.
- While they can cause SVT, the ECG during tachycardia would typically show a **wide QRS complex** if the accessory pathway is part of the reentrant circuit (antidromic), or a narrow QRS with a visible P wave if orthodromic and the accessory pathway is used for retrograde conduction, which doesn't fully align with the absent P waves and typically *normal* QRS during tachycardia as described.
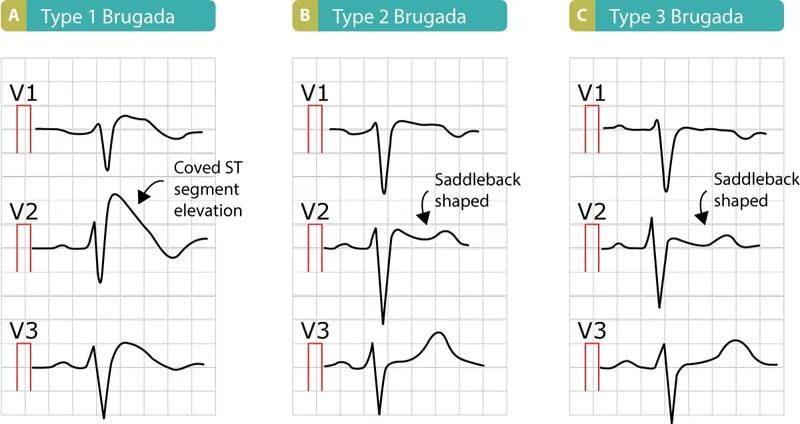
*Mutations in genes that code for myocyte ion channels*
- This refers to **channelopathies** (e.g., long QT syndrome, Brugada syndrome), which predispose to **ventricular arrhythmias** like **polymorphic ventricular tachycardia** and **ventricular fibrillation**.
- These conditions typically cause **wide QRS tachycardias** and have distinct ECG patterns (e.g., prolonged QT interval, Brugada pattern) not described here. The narrow QRS and regular rhythm point away from primary ventricular channelopathies as the cause of this specific tachycardia.
*Macroreentrant rhythm in the right atria through cavotricuspid isthmus*
- This describes **atrial flutter**, which typically presents with characteristic **"sawtooth" F waves** on ECG, representing atrial activity.
- While atrial flutter can cause recurrent episodes of rapid heart rate, the ECG description of **absent P waves** and a **narrow QRS complex** without F waves makes atrial flutter less likely.
*Fibrosis of the sinoatrial node and surrounding myocardium*
- **Sinoatrial node dysfunction (sick sinus syndrome)** can lead to bradycardia, sinus pauses, or alternating bradycardia and tachycardia (tachy-brady syndrome).
- It does not primarily cause the described paroxysmal narrow-complex tachycardia with absent P waves. The patient's symptoms are more consistent with an abrupt-onset, regular supraventricular tachycardia.
Inherited arrhythmia syndromes US Medical PG Question 5: A 55-year-old man with a past medical history of obesity and hyperlipidemia suddenly develops left-sided chest pain and shortness of breath while at work. He relays to coworkers that the pain is intense and has spread to his upper left arm over the past 10 minutes. He reports it feels a lot like the “heart attack” he had a year ago. He suddenly collapses and is unresponsive. Coworkers perform cardiopulmonary resuscitation for 18 minutes until emergency medical services arrives. Paramedics pronounce him dead at the scene. Which of the following is the most likely cause of death in this man?
- A. Pericarditis
- B. Aortic dissection
- C. Atrial fibrillation
- D. Ventricular tachycardia (Correct Answer)
- E. Free wall rupture
Inherited arrhythmia syndromes Explanation: ***Ventricular tachycardia***
- The patient's history of MI **1 year ago** creates a substrate of **scarred myocardium** that predisposes to life-threatening ventricular arrhythmias.
- The current presentation of sudden chest pain radiating to the arm suggests **acute re-infarction**, which triggers electrical instability in already compromised myocardium.
- **Ventricular tachycardia (VT)** degenerating to **ventricular fibrillation (VF)** is the **most common cause of sudden cardiac death** in patients with prior MI, especially during acute ischemic events.
- The rapid collapse and death within minutes, despite CPR, is classic for fatal ventricular arrhythmia.
*Free wall rupture*
- Free wall rupture is a **mechanical complication** that occurs **3-14 days** (typically days 3-7) after an **acute MI**, not 1 year later.
- By 1 year post-MI, the ventricular wall has either healed with fibrous scar tissue or formed a chronic ventricular aneurysm.
- While this would cause sudden death via cardiac tamponade, the **timing makes this unlikely** in this scenario.
*Pericarditis*
- Pericarditis causes **pleuritic chest pain** that is sharp, positional, and typically relieved by leaning forward.
- It is **not an immediate cause of sudden cardiac death** and would not explain the rapid collapse and unresponsiveness.
- While post-MI (Dressler) pericarditis can occur weeks after MI, it doesn't cause this presentation.
*Aortic dissection*
- Aortic dissection presents with **sudden, severe, tearing chest pain** often radiating to the back.
- While potentially fatal, the patient's description of pain "a lot like the heart attack he had a year ago" and his cardiac risk factors make **recurrent MI with fatal arrhythmia more likely**.
- No mention of blood pressure differential or pulse deficits that would suggest dissection.
*Atrial fibrillation*
- Atrial fibrillation is a **supraventricular arrhythmia** that causes palpitations, dyspnea, and irregular pulse.
- It is **not typically immediately fatal** in isolation and does not cause sudden collapse and death within minutes.
- While AF can lead to stroke or heart failure over time, it doesn't explain this acute sudden cardiac death.
Inherited arrhythmia syndromes US Medical PG Question 6: A 62-year-old woman presents to the emergency department complaining of fever, worsening fatigue, and muscle weakness for the previous 48 hours. The patient describes her muscle weakness as symmetric and worse in the upper limbs. Her past medical history is significant for long-standing diabetes type 2 complicated by stage 5 chronic kidney disease (CKD) on hemodialysis. She takes lisinopril, verapamil, metformin, and glargine. Today, the patient’s vital signs include: temperature 38.6°C (101.5°F), pulse 80/min, blood pressure 155/89 mm Hg, respirations 24/min, and 95% oxygen saturation on room air. The cardiac and pulmonary exams are unremarkable. The abdomen is soft and non-tender. Her strength is 3/5 in the upper extremities and 4/5 in the lower extremities and her sensation is intact. Deep tendon reflexes are absent in both the upper and lower limbs. A 12-lead electrocardiogram (ECG) is shown in the image below. Blood work is drawn and the patient is admitted and started on continuous cardiac monitoring. Based on the available information, what is the next best step in managing this patient?
- A. Order a stat serum potassium level
- B. Administer IV calcium gluconate (Correct Answer)
- C. Emergency dialysis
- D. Administer IV sodium bicarbonate
- E. Administer regular insulin and 50% dextrose in water
Inherited arrhythmia syndromes Explanation: ***Administer IV calcium gluconate***
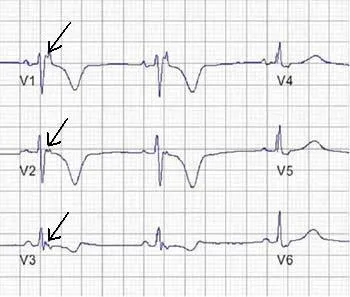
- The patient's presentation with **symmetrical muscle weakness** (worse in upper limbs), **absent deep tendon reflexes**, and characteristic ECG changes (peaked T waves, prolonged PR interval, wide QRS) in the context of **end-stage renal disease** and hemodialysis strongly suggests **severe hyperkalemia**.
- **Intravenous calcium gluconate** is the first-line treatment for clinically significant hyperkalemia with ECG changes, as it directly antagonizes the cardiac membrane effects of potassium and helps to stabilize the myocardium.
*Order a stat serum potassium level*
- While it is crucial to confirm hyperkalemia with a **stat serum potassium level**, the clinical picture (CKD, hemodialysis, muscle weakness, absent reflexes, and ECG changes) is emergent and highly suggestive of severe hyperkalemia.
- Waiting for laboratory confirmation before administering calcium gluconate can delay life-saving treatment and is not the "next best step" when ECG changes are evident.
*Emergency dialysis*
- **Emergency dialysis** is an effective way to remove potassium from the body and is often needed in severe hyperkalemia, especially in ESRD patients.
- However, **calcium gluconate** should be administered *immediately* to stabilize the cardiac membrane and prevent life-threatening arrhythmias, even before preparing for dialysis.
*Administer IV sodium bicarbonate*
- **Sodium bicarbonate** can shift potassium intracellularly, particularly in the setting of metabolic acidosis, but its effect is slower and less reliable than calcium in stabilizing cardiac membranes.
- It is often used as an adjunct but not as the initial, most critical intervention for immediate cardiac stabilization in severe hyperkalemia.
*Administer regular insulin and 50% dextrose in water*
- **Insulin and dextrose** shift potassium into cells, thereby lowering serum potassium levels. This is an important step in managing hyperkalemia.
- However, similar to sodium bicarbonate, its effect on serum potassium is not immediate enough to counteract the acute cardiotoxic effects, making **calcium gluconate** the priority for cardiac stabilization.
Inherited arrhythmia syndromes US Medical PG Question 7: A 22-year-old woman presents to the emergency department feeling lightheaded and states that her heart is racing. She does not have a history of any chronic medical conditions. She is a college sophomore and plays club volleyball. Although she feels stressed about her upcoming final exams next week, she limits her caffeine intake to 3 cups of coffee per day to get a good night sleep. She notes that her brother takes medication for some type of heart condition, but she does not know the name of it. Both her parents are alive and well. She denies recent illness, injuries, or use of cigarettes, alcohol, or recreational drugs. The pertinent negatives from the review of systems include an absence of fever, nausea, vomiting, sweating, fatigue, or change in bowel habits. The vital signs include: temperature 36.8°C (98.2°F), heart rate 125/min, respiratory rate 15/min, blood pressure 90/75 mm Hg, and oxygen saturation of 100% on room air. The laboratory results are within normal limits. The ECG is significant for a shortened PR interval and widened QRS. Which of the following medications should the patient avoid in this scenario?
- A. Amlodipine
- B. Procainamide
- C. Diltiazem
- D. Verapamil (Correct Answer)
- E. Metoprolol
Inherited arrhythmia syndromes Explanation: ***Verapamil***
- The ECG findings of a **shortened PR interval** and **widened QRS** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, an accessory pathway that can bypass the AV node.
- Verapamil is a **non-dihydropyridine calcium channel blocker** that blocks the AV node and can paradoxically increase conduction down the accessory pathway in WPW, potentially leading to **ventricular fibrillation** if an atrial tachyarrhythmia is present.
- **Verapamil is the most classically contraindicated medication in WPW syndrome** and is the prototype drug to avoid in this condition.
*Amlodipine*
- Amlodipine is a **dihydropyridine calcium channel blocker** primarily used for hypertension and angina.
- It has minimal effect on the AV node and does not carry the same risk as non-dihydropyridine calcium channel blockers in WPW syndrome.
*Procainamide*
- **Procainamide is a Class Ia antiarrhythmic** that can be used to treat tachyarrhythmias related to WPW syndrome, as it prolongs the refractory period of the accessory pathway.
- It would be a potential **treatment option**, not a medication to avoid, especially for antidromic atrioventricular reentrant tachycardia (AVRT) in WPW.
*Diltiazem*
- Similar to verapamil, diltiazem is a **non-dihydropyridine calcium channel blocker** that blocks the AV node.
- While it carries similar risks to verapamil in WPW syndrome, **verapamil is more classically emphasized** as the prototypical contraindicated medication in medical education and board examinations.
*Metoprolol*
- Metoprolol is a **beta-blocker** that slows conduction through the AV node.
- While beta-blockers are also generally **avoided in WPW syndrome with atrial fibrillation**, **AV nodal blocking calcium channel blockers (especially verapamil) are considered the primary contraindication** due to more pronounced effects on accessory pathway conduction.
Inherited arrhythmia syndromes US Medical PG Question 8: A 45-year-old man comes to the physician for a routine health maintenance examination. He feels well. He underwent appendectomy at the age of 25 years. He has a history of hypercholesterolemia that is well controlled with atorvastatin. He is an avid marathon runner and runs 8 miles per day four times a week. His father died of myocardial infarction at the age of 42 years. The patient does not smoke or drink alcohol. His vital signs are within normal limits. Cardiopulmonary examination shows no abnormalities. His abdomen is soft and nontender with a surgical scar in the right lower quadrant. Laboratory studies are within normal limits. An ECG is shown. Which of the following is the most likely diagnosis?
- A. Mobitz type II AV block
- B. First-degree AV block
- C. Mobitz type I AV block (Correct Answer)
- D. Third-degree AV block
- E. Atrial fibrillation
Inherited arrhythmia syndromes Explanation: ***Mobitz type I AV block***
- The ECG shows progressive prolongation of the **PR interval** followed by a dropped QRS complex, which is characteristic of a **Mobitz type I (Wenckebach) AV block**.
- This rhythm disturbance is often benign, especially in athletes with high **vagal tone**, and does not usually require treatment.
*Mobitz type II AV block*
- **Mobitz type II AV block** is characterized by a constant PR interval before the dropped QRS complex.
- This type of block is generally more serious and indicative of a conduction disturbance below the AV node, often requiring a **pacemaker**.
*First-degree AV block*
- A **first-degree AV block** presents with a consistently prolonged PR interval (greater than 0.20 seconds) on every beat, without any dropped beats.
- In this patient's ECG, there is a dropped QRS complex after progressive PR prolongation.
*Third-degree AV block*
- **Third-degree (complete) AV block** is characterized by complete dissociation between the P waves and QRS complexes.
- There is no relationship between atrial and ventricular activity, and the ventricular rate is typically very slow and escape rhythms are observed.
*Atrial fibrillation*
- **Atrial fibrillation** is an irregularly irregular rhythm with no discernible P waves and varying R-R intervals.
- The ECG provided shows clear P waves and a regular, albeit interrupted, rhythm pattern.
Inherited arrhythmia syndromes US Medical PG Question 9: A 6-year-old boy is brought to the pediatrician by his mother after he reported having red urine. He has never experienced this before and did not eat anything unusual before the episode. His past medical history is notable for sensorineural deafness requiring hearing aids. He is otherwise healthy and enjoys being in the 1st grade. His birth history was unremarkable. His temperature is 98.8°F (37.1°C), blood pressure is 145/85 mmHg, pulse is 86/min, and respirations are 18/min. On examination, he is a well-appearing boy in no acute distress. Cardiac, respiratory, and abdominal exams are normal. A urinalysis is notable for microscopic hematuria and mild proteinuria. This patient’s condition is most commonly caused by which of the following inheritance patterns?
- A. X-linked dominant
- B. Autosomal recessive
- C. Autosomal dominant
- D. X-linked recessive (Correct Answer)
- E. Mitochondrial inheritance
Inherited arrhythmia syndromes Explanation: ***X-linked recessive***
- This is the **most common inheritance pattern** for **Alport syndrome**, accounting for approximately **80-85% of all cases**.
- This inheritance pattern is characteristic of **Alport syndrome**, which classically presents with **hematuria**, **sensorineural hearing loss**, and ocular abnormalities.
- The patient's presentation with **red urine (hematuria)** and a history of **sensorineural deafness** strongly points to **Alport syndrome**, which is primarily caused by **X-linked recessive** inheritance due to mutations in the *COL4A5* gene encoding the alpha-5 chain of type IV collagen.
- Males with the mutation are typically more severely affected, while female carriers may have variable manifestations.
*X-linked dominant*
- While Alport syndrome can manifest in females with an X-linked dominant-like pattern (due to mosaicism or severely affected carrier females), the **classic and most common inheritance** for severe forms in males is **X-linked recessive**.
- Conditions like **Fragile X syndrome** or **Vitamin D-resistant rickets** are examples of X-linked dominant conditions, but they do not typically present with the specific triad observed here.
*Autosomal recessive*
- An autosomal recessive form of **Alport syndrome** exists, but it accounts for only approximately **10-15% of cases** compared to the X-linked recessive form.
- While other conditions with **renal and auditory involvement** can be autosomal recessive (e.g., specific forms of branchio-oto-renal syndrome), the **combination of hematuria and sensorineural deafness with significant renal progression risk** in a male points most strongly to the X-linked form.
*Autosomal dominant*
- Alport syndrome also has an **autosomal dominant** form, which is typically due to mutations in *COL4A3* or *COL4A4* genes, but it accounts for only approximately **5% of cases** and is **less common** than the X-linked recessive form.
- The autosomal dominant form often presents with a **later onset** and a **more variable phenotype** with milder disease progression.
- While some forms of **polycystic kidney disease** are autosomal dominant and can cause hematuria, they typically involve cyst formation, which is not suggested by the clinical picture here.
*Mitochondrial inheritance*
- This inheritance pattern is associated with disorders affecting **energy production**, commonly involving multiple organ systems, including muscle, brain, and eye.
- While some mitochondrial disorders can affect the kidneys or cause hearing impairment, the **specific combination of hematuria and sensorineural deafness** as the primary presentation in this context is not characteristic of mitochondrial inheritance.
Inherited arrhythmia syndromes US Medical PG Question 10: A 54-year-old woman is brought to the emergency department because of a 2-hour history of nausea and retrosternal chest pain. She has a 15-year history of type 2 diabetes mellitus. Her current medications include atorvastatin, metformin, and lisinopril. She is diaphoretic. Her serum troponin level is 3.0 ng/mL (N: < 0.04). She undergoes cardiac catheterization. A photograph of coronary angiography performed prior to percutaneous coronary intervention is shown. An acute infarct associated with the finding on angiography is most likely to manifest with ST elevations in which of the following leads on ECG?
- A. V3R–V6R
- B. I, aVR
- C. V1–V6 (Correct Answer)
- D. II, III, and aVF
- E. V7–V9
Inherited arrhythmia syndromes Explanation: ***V1–V6***
- The angiography shows a significant occlusion in the **left anterior descending (LAD) artery**
- LAD occlusion causes **anterior wall myocardial infarction**
- Anterior MI manifests with **ST elevations in precordial leads V1–V6**
- This is the classic ECG pattern for LAD territory infarction
*V3R–V6R*
- These right-sided precordial leads indicate **right ventricular infarction**
- RV infarction is associated with **proximal right coronary artery (RCA) occlusion**
- Not consistent with the LAD occlusion shown in the angiography
*I, aVR*
- Lead **aVR ST elevation** (especially >1 mm or greater than V1) suggests **left main coronary artery occlusion** or severe multi-vessel disease
- This pattern typically shows widespread ST depression in other leads
- Does not specifically indicate isolated LAD occlusion
*II, III, and aVF*
- ST elevations in these inferior leads indicate **inferior wall myocardial infarction**
- Inferior MI is caused by **right coronary artery (RCA)** occlusion (80%) or left circumflex artery (20%)
- Not associated with LAD occlusion
*V7–V9*
- These posterior leads indicate **posterior wall myocardial infarction**
- Posterior MI results from **left circumflex artery** or dominant RCA occlusion
- Not the primary finding with LAD occlusion
More Inherited arrhythmia syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.