ECG interpretation fundamentals US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for ECG interpretation fundamentals. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
ECG interpretation fundamentals US Medical PG Question 1: A 21-year-old woman presents with palpitations and anxiety. She had a recent outpatient ECG that was suggestive of supraventricular tachycardia, but her previous physician failed to find any underlying disease. No other significant past medical history. Her vital signs include blood pressure 102/65 mm Hg, pulse 120/min, respiratory rate 17/min, and temperature 36.5℃ (97.7℉). Electrophysiological studies reveal an atrioventricular nodal reentrant tachycardia. The patient refuses an ablation procedure so it is decided to perform synchronized cardioversion with consequent ongoing management with verapamil. Which of the following ECG features should be monitored in this patient during treatment?
- A. Amplitude and direction of the T wave
- B. Length of QRS complex
- C. Length of QT interval
- D. Length of PR interval (Correct Answer)
- E. QRS complex amplitude
ECG interpretation fundamentals Explanation: ***Length of PR interval***
- Verapamil is a **non-dihydropyridine calcium channel blocker** that primarily acts on the **AV node** to slow conduction.
- Monitoring the **PR interval** is crucial because excessive slowing of AV nodal conduction can lead to **AV block**, which is indicated by a prolonged PR interval.
*Amplitude and direction of the T wave*
- Changes in T-wave amplitude and direction are often associated with **myocardial ischemia** or **electrolyte imbalances**, which are not the primary concerns with verapamil.
- While verapamil can affect repolarization, the most direct and common adverse effect related to its mechanism of action on the AV node is not primarily reflected in T-wave changes.
*Length of QRS complex*
- The QRS complex duration primarily reflects **ventricular depolarization** and is typically affected by medications that alter conduction through the His-Purkinje system or within the ventricles, such as antiarrhythmics like **flecainide** or **amiodarone**.
- Verapamil's main action is on the AV node, so it generally does not significantly prolong the QRS complex unless there is pre-existing conduction system disease.
*Length of QT interval*
- The QT interval represents **ventricular repolarization**, and its prolongation can lead to **Torsades de Pointes**, a life-threatening arrhythmia.
- While many antiarrhythmics can prolong the QT interval, **verapamil is not known to significantly prolong the QT interval** and is generally considered safe in this regard.
*QRS complex amplitude*
- Changes in QRS amplitude can indicate conditions like **pericardial effusion**, **cardiomyopathy**, or changes in ventricular mass.
- These are generally not direct or common side effects of verapamil therapy, which primarily focuses on AV nodal conduction.
ECG interpretation fundamentals US Medical PG Question 2: A 75-year-old man presents to the emergency department after an episode of syncope while walking outside with his wife. His wife states that he suddenly appeared pale and collapsed to the ground. She says he remained unconscious for 1 minute. He says he noticed a fluttering in his chest and excessive sweating before the episode. He has type 2 diabetes mellitus, essential hypertension, and chronic stable angina. He has not started any new medications in the past few months. Vital signs reveal: temperature 37.0°C (98.6°F), blood pressure 135/72 mm Hg, and pulse 72/min. Physical examination is unremarkable. ECG shows an old bifascicular block. Echocardiogram and 24-hour Holter monitoring are normal. Which of the following is the best next step in the evaluation of this patient's condition?
- A. Cardiac enzymes
- B. Continuous loop recorder (Correct Answer)
- C. Valsalva maneuver
- D. Electroencephalography (EEG)
- E. Tilt-table test
ECG interpretation fundamentals Explanation: ***Continuous loop recorder***
- This patient's syncope is preceded by **palpitations (fluttering in chest)** and **sweating**, suggesting a cardiac etiology, specifically a **transient arrhythmia** not captured on a standard ECG or 24-hour Holter.
- A continuous loop recorder provides prolonged monitoring (months to years), increasing the likelihood of detecting intermittent arrhythmias responsible for syncopal episodes.
*Cardiac enzymes*
- While cardiac enzymes (e.g., troponin) are crucial for evaluating **acute myocardial ischemia** or infarction, the patient presents with syncope and no new chest pain, and his stable angina suggests chronic disease rather than an acute event leading to syncope in this specific instance.
- An **ECG showing an old bifascicular block** and an **unremarkable physical exam** make an acute cardiac event less likely as the primary cause of syncope when an arrhythmia is suspected.
*Valsalva maneuver*
- The Valsalva maneuver is a diagnostic tool often used to differentiate between certain types of **tachyarrhythmias** or to evaluate for **autonomic dysfunction**, but it is not an evaluative step for a patient presenting with unexplained syncope where an arrhythmia has not yet been documented.
- It would not help in identifying the cause of intermittent syncope in a patient whose standard workup has been unremarkable, as it's a test for immediate physiological response, not prolonged cardiac rhythm monitoring.
*Electroencephalography (EEG)*
- EEG is indicated when **seizure disorder** is suspected as the cause of loss of consciousness, often characterized by tonic-clonic movements, post-ictal confusion, or focal neurologic signs, which are absent in this patient's presentation.
- The patient's pre-syncopal symptoms of **palpitations and sweating** point away from a seizure and towards a cardiac cause.
*Tilt-table test*
- A tilt-table test is used to evaluate for **vasovagal syncope** or **postural orthostatic tachycardia syndrome (POTS)**, often considered when other cardiac causes are ruled out or when syncope is typically triggered by prolonged standing.
- Given the patient's pre-syncopal **palpitations**, a **cardiac arrhythmia** remains a higher suspicion than vasovagal syncope at this stage, especially after normal echocardiogram and Holter monitoring, necessitating further arrhythmia investigation.
ECG interpretation fundamentals US Medical PG Question 3: A 71-year-old man is brought to the emergency department by his wife because of increasing confusion, weakness, and vomiting for 1 day. He has had 5 episodes of vomiting and blurry vision; he told his wife that "everything appears in different colors." He has been unable to recall his wife's name or their address. His wife reports that his drug regimen was adjusted because of worsening tibial edema 1 week ago. He has congestive heart failure, atrial fibrillation, hypothyroidism, and osteoarthritis. Current medications include rivaroxaban, metoprolol, digoxin, levothyroxine, spironolactone, and furosemide. His temperature is 36.7°C (98°F), pulse is 56/min, and blood pressure is 98/68 mm Hg. He is confused and oriented only to person. Neurologic examination shows no focal findings. The abdomen is soft, and there is tenderness to palpation of both lower quadrants without guarding or rebound. There is 1+ pitting edema of both ankles. This patient is most likely to have which of the following ECG findings?
- A. Low QRS voltage
- B. Increased PR interval (Correct Answer)
- C. Mobitz type 2 atrioventricular block
- D. Prolonged QT interval
- E. Peaked T waves
ECG interpretation fundamentals Explanation: ***Increased PR interval***
- The patient's symptoms (confusion, weakness, vomiting, blurry vision with "everything appears in different colors," bradycardia) are classic signs of **digoxin toxicity**. Digoxin primarily affects the **AV node**, leading to slowed conduction and thus an **increased PR interval** on ECG.
- The recent adjustment of his diuretic regimen (spironolactone and furosemide) for worsening edema suggests possible **hypokalemia** or **renal impairment**, which can precipitate digoxin toxicity even at therapeutic levels.
*Low QRS voltage*
- **Low QRS voltage** is typically associated with conditions like **pericardial effusion**, severe hypothyroidism, or diffuse myocardial disease, which are not directly suggested by the patient's acute presentation.
- While the patient has hypothyroidism, acute digoxin toxicity does not primarily cause low QRS voltage.
*Mobitz type 2 atrioventricular block*
- While digoxin toxicity can cause various arrhythmias, **Mobitz type 2 AV block** (characterized by constant PR interval before a dropped beat) usually indicates issues deeper in the His-Purkinje system.
- **First-degree AV block** (increased PR interval) and **Wenckebach (Mobitz type 1) AV block** are more common manifestations of digoxin's direct inhibitory effect on the AV node.
*Prolonged QT interval*
- A **prolonged QT interval** is associated with an increased risk of **Torsades de Pointes** and can be caused by certain antiarrhythmics (e.g., amiodarone, sotalol) or electrolyte imbalances, but it is not a direct or typical ECG finding of digoxin toxicity.
- Digoxin toxicity is more commonly associated with a **shortened QT interval** or "scooping" of the ST segment.
*Peaked T waves*
- **Peaked T waves** are a hallmark of **hyperkalemia**, an electrolyte disturbance that can cause cardiac arrhythmias and muscle weakness.
- While electrolyte imbalances can contribute to digoxin toxicity, peaked T waves themselves are not a direct consequence of digoxin.
ECG interpretation fundamentals US Medical PG Question 4: A 72-year-old man comes to the physician because of a 2-month history of intermittent retrosternal chest pain and tightness on exertion. He has type 2 diabetes mellitus, osteoarthritis of the right hip, and hypertension. Current medications include insulin, ibuprofen, enalapril, and hydrochlorothiazide. Vital signs are within normal limits. His troponin level is within the reference range. An ECG at rest shows a right bundle branch block and infrequent premature ventricular contractions. The patient's symptoms are reproduced during adenosine stress testing. Repeat ECG during stress testing shows new ST depression of > 1 mm in leads V2, V3, and V4. Which of the following is the most important underlying mechanism of this patient's ECG changes?
- A. Diversion of blood flow from stenotic coronary arteries (Correct Answer)
- B. Transient atrioventricular nodal blockade
- C. Reduced left ventricular preload
- D. Ruptured cholesterol plaque within a coronary vessel
- E. Increased myocardial oxygen demand
ECG interpretation fundamentals Explanation: ***Diversion of blood flow from stenotic coronary arteries***
- The **adenosine stress test** induces **submaximal coronary vasodilation** in healthy vessels, diverting blood flow away from stenosed areas that are already maximally dilated, a phenomenon known as **coronary steal**.
- This **relative hypoperfusion** in areas supplied by stenotic arteries leads to myocardial ischemia, manifested as **new ST depression** on the ECG due to **subendocardial oxygen supply-demand mismatch**.
*Transient atrioventricular nodal blockade*
- While adenosine can cause transient AV nodal blockade, leading to AV blocks, this would manifest as specific changes in **PR interval** or **QRS drop-out**, not ST segment depression indicative of ischemia.
- The patient's symptoms and ECG changes point towards myocardial ischemia, not an AV conduction disturbance.
*Reduced left ventricular preload*
- Reduced preload can occur in certain cardiac conditions but is not the primary mechanism behind ST depression during an adenosine stress test.
- ECG changes due to reduced preload are usually nonspecific, such as **sinus tachycardia** or **low voltage**, and do not typically cause new ST depression in specific leads.
*Ruptured cholesterol plaque within a coronary vessel*
- A ruptured plaque with subsequent **thrombus formation** would lead to **acute coronary syndrome (ACS)**, characterized by persistent chest pain, **elevated troponins**, and potentially **ST elevation** or new **pathologic Q waves** if complete occlusion occurs.
- The patient's troponin level is normal, and his symptoms are intermittent and reproducible on stress testing, which is more consistent with **stable angina**.
*Increased myocardial oxygen demand*
- While increased myocardial oxygen demand is a component of angina pectoris, adenosine primarily causes **coronary vasodilation**, which can worsen ischemia in stenotic areas by diverting blood flow, rather than directly increasing myocardial oxygen demand itself.
- **Dobutamine stress testing** would be the test that primarily increases myocardial oxygen demand.
ECG interpretation fundamentals US Medical PG Question 5: A 41-year-old woman presents to the emergency room with chest pain. She has had progressive substernal chest pain accompanied by weakness and mild shortness of breath for the past 2 hours. Her past medical history is notable for poorly controlled systemic lupus erythematosus (SLE), Sjogren syndrome, and interstitial lung disease. She was hospitalized last year with pericarditis presumed to be from SLE. Her temperature is 98.6°F (37°C), blood pressure is 106/56 mmHg, pulse is 132/min, and respirations are 26/min. On exam, the skin overlying the internal jugular vein fills at 9 cm above the sternal angle and distant heart sounds are appreciated. There is no friction rub. She is given 1000cc of intravenous fluids with no appreciable change in her blood pressure. An electrocardiogram in this patient would most likely reveal which of the following findings?
- A. Polymorphic P waves
- B. ST elevations in leads II, III, and aVF
- C. Peaked T waves
- D. Wide QRS complexes with no P waves
- E. Electrical alternans (Correct Answer)
ECG interpretation fundamentals Explanation: ***Electrical alternans***
- The patient's symptoms (chest pain, shortness of breath, **hypotension**, **tachycardia**, **elevated JVP**, and **distant heart sounds**) in the context of a history of **pericarditis** and **SLE** are highly suggestive of **cardiac tamponade.**
- **Electrical alternans**, characterized by alternating QRS complex heights due to the swinging motion of the heart in a large pericardial effusion, is a classic EKG finding for cardiac tamponade.
- This finding reflects the mechanical swinging of the heart within the pericardial fluid, causing beat-to-beat variation in QRS amplitude.
*Polymorphic P waves*
- **Polymorphic P waves** (multifocal atrial tachycardia) occur when there are at least three different P wave morphologies on the EKG, indicating multiple ectopic atrial foci.
- This is typically seen in patients with severe lung disease or other conditions causing increased atrial stretch, but it is not a direct consequence or typical finding of cardiac tamponade.
*ST elevations in leads II, III, and aVF*
- **ST elevations in leads II, III, and aVF** indicate an **inferior myocardial infarction**, which is caused by coronary artery occlusion.
- While chest pain is present, the patient's other signs (elevated JVP, distant heart sounds, hypotension not responding to fluids, history of pericarditis/SLE) point away from an acute MI and strongly towards cardiac tamponade.
*Peaked T waves*
- **Peaked T waves** are characteristic of **hyperkalemia**, a condition of excessively high potassium levels in the blood.
- While hyperkalemia can cause cardiac symptoms, it does not typically present with the specific hemodynamic compromise and physical exam findings (elevated JVP, distant heart sounds) described, which are classic for cardiac tamponade.
*Wide QRS complexes with no P waves*
- **Wide QRS complexes with no P waves** are characteristic of a **ventricular arrhythmia**, such as ventricular tachycardia or idioventricular rhythm.
- While the patient is hypotensive and tachycardic, the presenting symptoms and physical exam findings are not directly indicative of a primary ventricular arrhythmia, but rather suggest an extracardiac compression of the heart due to tamponade.
ECG interpretation fundamentals US Medical PG Question 6: A 45-year-old man comes to the physician for a routine health maintenance examination. He feels well. He underwent appendectomy at the age of 25 years. He has a history of hypercholesterolemia that is well controlled with atorvastatin. He is an avid marathon runner and runs 8 miles per day four times a week. His father died of myocardial infarction at the age of 42 years. The patient does not smoke or drink alcohol. His vital signs are within normal limits. Cardiopulmonary examination shows no abnormalities. His abdomen is soft and nontender with a surgical scar in the right lower quadrant. Laboratory studies are within normal limits. An ECG is shown. Which of the following is the most likely diagnosis?
- A. Mobitz type II AV block
- B. First-degree AV block
- C. Mobitz type I AV block (Correct Answer)
- D. Third-degree AV block
- E. Atrial fibrillation
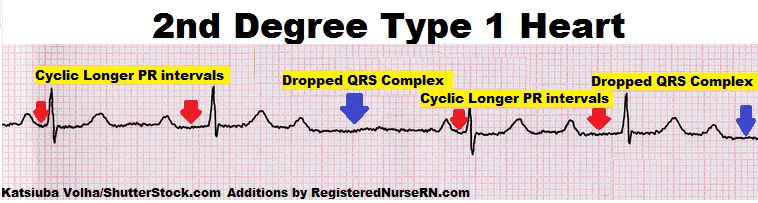
ECG interpretation fundamentals Explanation: ***Mobitz type I AV block***
- The ECG shows progressive prolongation of the **PR interval** followed by a dropped QRS complex, which is characteristic of a **Mobitz type I (Wenckebach) AV block**.
- This rhythm disturbance is often benign, especially in athletes with high **vagal tone**, and does not usually require treatment.
*Mobitz type II AV block*
- **Mobitz type II AV block** is characterized by a constant PR interval before the dropped QRS complex.
- This type of block is generally more serious and indicative of a conduction disturbance below the AV node, often requiring a **pacemaker**.
*First-degree AV block*
- A **first-degree AV block** presents with a consistently prolonged PR interval (greater than 0.20 seconds) on every beat, without any dropped beats.
- In this patient's ECG, there is a dropped QRS complex after progressive PR prolongation.
*Third-degree AV block*
- **Third-degree (complete) AV block** is characterized by complete dissociation between the P waves and QRS complexes.
- There is no relationship between atrial and ventricular activity, and the ventricular rate is typically very slow and escape rhythms are observed.
*Atrial fibrillation*
- **Atrial fibrillation** is an irregularly irregular rhythm with no discernible P waves and varying R-R intervals.
- The ECG provided shows clear P waves and a regular, albeit interrupted, rhythm pattern.
ECG interpretation fundamentals US Medical PG Question 7: A 23-year-old man comes to the emergency department because of palpitations, dizziness, and substernal chest pain for three hours. The day prior, he was at a friend’s wedding, where he consumed seven glasses of wine. The patient appears diaphoretic. His pulse is 220/min and blood pressure is 120/84 mm Hg. Based on the patient's findings on electrocardiography, the physician diagnoses atrial fibrillation with rapid ventricular response and administers verapamil for rate control. Ten minutes later, the patient is unresponsive and loses consciousness. Despite resuscitative efforts, the patient dies. Histopathologic examination of the heart at autopsy shows an accessory atrioventricular conduction pathway. Electrocardiography prior to the onset of this patient's symptoms would most likely have shown which of the following findings?
- A. Epsilon wave following the QRS complex
- B. Prolongation of the QT interval
- C. Cyclic alteration of the QRS axis
- D. Slurred upstroke of the QRS complex (Correct Answer)
- E. Positive Sokolow-Lyon index
ECG interpretation fundamentals Explanation: ***Slurred upstroke of the QRS complex***
- The patient's presentation with **atrial fibrillation with rapid ventricular response** and subsequent collapse after verapamil administration—a calcium channel blocker—is classic for a pre-excitation syndrome like **Wolff-Parkinson-White (WPW) syndrome**.
- In WPW, an accessory pathway (bundle of Kent) bypasses the AV node, leading to a **short PR interval** and a **delta wave** (slurred upstroke of the QRS complex) on ECG during normal sinus rhythm.
*Epsilon wave following the QRS complex*
- An **epsilon wave** is characteristic of **arrhythmogenic right ventricular cardiomyopathy (ARVC)**, representing delayed depolarization of the right ventricle.
- While ARVC can cause arrhythmias, it is distinctly different from the pre-excitation syndrome described, which involves an accessory pathway.
*Prolongation of the QT interval*
- **Prolonged QT interval** is associated with an increased risk of **torsades de pointes**, a polymorphic ventricular tachycardia.
- This finding is typical of **long QT syndrome** and does not directly relate to an accessory atrioventricular conduction pathway.
*Cyclic alteration of the QRS axis*
- **Cyclic alteration of the QRS axis** or electrical alternans is seen in conditions causing swings in cardiac position, most notably **pericardial effusion with tamponade**.
- This ECG finding is unrelated to accessory pathways or the mechanisms of pre-excitation syndromes.
*Positive Sokolow-Lyon index*
- A **positive Sokolow-Lyon index** signifies **left ventricular hypertrophy (LVH)**, characterized by large QRS voltages (e.g., SV1 + RV5/V6 ≥ 35 mm).
- While LVH can be associated with various cardiac conditions, it is not a direct ECG manifestation of an accessory atrioventricular conduction pathway.
ECG interpretation fundamentals US Medical PG Question 8: Two days after undergoing an uncomplicated total thyroidectomy, a 63-year-old woman has acute, progressive chest pain. The pain is sharp and burning. She feels nauseated and short of breath. The patient has a history of hypertension, type 1 diabetes mellitus, medullary thyroid cancer, multiple endocrine neoplasia type 2A, anxiety, coronary artery disease, and gastroesophageal reflux disease. She smoked half a pack of cigarettes daily for 24 years but quit 18 years ago. Current medications include lisinopril, insulin glargine, insulin aspart, sertraline, aspirin, ranitidine, and levothyroxine. She appears anxious and diaphoretic. Her temperature is 37.4°C (99.3°F), pulse is 64/min, respirations are 17/min, and blood pressure is 148/77 mm Hg. The lungs are clear to auscultation. Examination shows a 3-cm linear incision over the anterior neck with 1 mm of surrounding erythema and mild serous discharge. The chest wall and abdomen are nontender. There is 5/5 strength in all extremities and decreased sensation to soft touch on the feet bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Obtain an ECG and troponin T levels (Correct Answer)
- B. Administer IV pantoprazole and schedule endoscopy
- C. Discontinue levothyroxine and obtain fT4 levels
- D. Administer IV levofloxacin and obtain chest radiograph
- E. Obtain urine and plasma metanephrine levels
ECG interpretation fundamentals Explanation: **Obtain an ECG and troponin T levels**
- The patient presents with acute, progressive **chest pain that is sharp and burning**, along with nausea and shortness of breath, which are classic symptoms of an acute coronary syndrome, especially given her history of **coronary artery disease**, hypertension, diabetes, and prior smoking.
- An **ECG** and **troponin T levels** are crucial first steps to evaluate for myocardial ischemia or infarction in this high-risk patient.
*Administer IV pantoprazole and schedule endoscopy*
- While the patient has a history of gastroesophageal reflux disease (GERD) and her pain is described as "burning," the **acuteness, progression, and associated symptoms** (nausea, shortness of breath) in a patient with significant cardiac risk factors make a GI cause less likely as the primary concern.
- Empiric treatment for GERD without first ruling out a life-threatening cardiac event would be inappropriate and potentially dangerous.
*Discontinue levothyroxine and obtain fT4 levels*
- The patient is taking levothyroxine after a thyroidectomy for medullary thyroid cancer, but there is no immediate indication of thyroid hormone imbalance (e.g., hyperthyroidism causing chest pain) that would warrant discontinuing her medication or rushing fT4 levels as the first step in an acute chest pain presentation.
- Her pulse of 64/min is not suggestive of hyperthyroidism, which typically causes tachycardia.
*Administer IV levofloxacin and obtain chest radiograph*
- While shortness of breath can be a symptom of pneumonia, the **sharp, burning nature of the chest pain**, coupled with the absence of fever (temperature 37.4°C is mild), cough, or abnormal lung sounds (lungs clear to auscultation), makes an acute infection like pneumonia less probable as the primary diagnosis.
- Antibiotics and a chest radiograph would be considered after ruling out more immediate life-threatening conditions like acute coronary syndrome.
*Obtain urine and plasma metanephrine levels*
- The patient has a history of multiple endocrine neoplasia type 2A (MEN2A), which includes medullary thyroid cancer and can be associated with pheochromocytoma (adrenal tumor secreting catecholamines). However, her blood pressure (148/77 mm Hg) is not acutely elevated to crisis levels, and her symptoms are more consistent with cardiac ischemia than a pheochromocytoma crisis.
- While metanephrine levels would be important for long-term follow-up of MEN2A, they are not the immediate next step for acute chest pain in a patient with known coronary artery disease.
ECG interpretation fundamentals US Medical PG Question 9: A 30-year-old man is brought into the emergency room for complaints of acute onset chest pain and shortness of breath. He has a history of mental retardation and lives at home with his adoptive parents. His parents inform you that he has not seen a doctor since he was adopted as child and that he currently takes no medications. The patient's temperature is 99.1°F (37.3°C), pulse is 108/min, blood pressure is 125/70 mmHg, respirations are 25/min, and oxygen saturation is 92% on 2L nasal cannula. Physical exam is notable for a tall, thin individual with high-arched feet and mild pectus excavatum. There is mild asymmetry in the lower extremities with discomfort to dorsiflexion of the larger leg. Lung auscultation reveals no abnormalities. What is the most appropriate next step in management?
- A. Chest radiograph
- B. Serum blood test
- C. Genetic testing
- D. Angiogram
- E. Electrocardiogram (Correct Answer)
ECG interpretation fundamentals Explanation: ***Correct: Electrocardiogram***
- **Acute chest pain** mandates an immediate **ECG** as the first diagnostic test to rule out **ST-elevation myocardial infarction (STEMI)**, which requires emergent intervention (PCI or thrombolysis).
- While this patient's presentation is highly suspicious for **pulmonary embolism (PE)** given the **unilateral leg swelling with pain on dorsiflexion** (suggestive of DVT), **tachycardia**, **tachypnea**, and **hypoxemia**, the ECG remains the most appropriate initial step per ACLS protocols for chest pain.
- ECG can also show findings suggestive of PE (sinus tachycardia, S1Q3T3 pattern, right heart strain) and help differentiate cardiac from pulmonary etiologies.
- The **Marfanoid features** (tall, thin, pectus excavatum, high-arched feet) raise concern for **aortic dissection**, which ECG can help evaluate alongside clinical assessment.
*Incorrect: Chest radiograph*
- Chest X-ray is critical in the workup and would typically be ordered simultaneously with or immediately after ECG in this patient with suspected PE.
- CXR helps exclude pneumothorax, pneumonia, and can show classic PE findings (Westermark sign, Hampton's hump), though it is often normal in PE.
- In the context of Marfan syndrome, CXR can reveal a widened mediastinum suggesting aortic dissection.
- However, ECG takes precedence as the immediate first step for any acute chest pain presentation.
*Incorrect: Serum blood test*
- Laboratory tests including **cardiac troponins** (for MI), **D-dimer** (for PE), and **CBC** are important but take time to result.
- D-dimer would be useful in this moderate-to-high probability PE case, but imaging (CT pulmonary angiography) would be more appropriate given the high clinical suspicion.
- Blood tests do not provide the immediate actionable information needed as the first diagnostic step in acute chest pain.
*Incorrect: Genetic testing*
- While the patient's phenotype suggests **Marfan syndrome** or another connective tissue disorder, genetic testing is an outpatient diagnostic tool for long-term management.
- It provides no immediate utility in the acute management of chest pain and respiratory distress.
- Genetic counseling and testing would be appropriate after stabilization and initial workup.
*Incorrect: Angiogram*
- **CT pulmonary angiography** would be the definitive test for PE diagnosis after initial ECG and CXR, but is not the immediate first step.
- **Cardiac catheterization** would be indicated if ECG showed STEMI or if there was high suspicion for ACS after initial workup.
- **CT aortography** might be needed if aortic dissection is suspected based on initial findings.
- Angiography is an invasive or advanced imaging procedure performed after non-invasive screening tests guide the diagnosis.
ECG interpretation fundamentals US Medical PG Question 10: A 40-year-old woman comes to the physician for a 6-month history of recurrent episodes of chest pain, racing pulse, dizziness, and difficulty breathing. The episodes last up to several minutes. She also reports urinary urgency and two episodes of loss of consciousness followed by spontaneous recovery. There is no personal or family history of serious illness. She does not smoke or drink alcohol. Vitals signs are within normal limits. Cardiopulmonary examination shows no abnormalities. Holter monitoring is performed. ECG recordings during episodes of tachycardia show a QRS duration of 100 ms, regular RR-interval, and absent P waves. Which of the following is the most likely underlying cause of this patient's condition?
- A. AV node with slow and fast pathway (Correct Answer)
- B. Pre-excitation of the ventricles
- C. Mutations in genes that code for myocyte ion channels
- D. Macroreentrant rhythm in the right atria through cavotricuspid isthmus
- E. Fibrosis of the sinoatrial node and surrounding myocardium
ECG interpretation fundamentals Explanation: ***AV node with slow and fast pathway***
- This describes **AV nodal reentrant tachycardia (AVNRT)**, a common cause of **paroxysmal supraventricular tachycardia (PSVT)**. The ECG findings of **narrow QRS (100 ms)**, regular RR-interval, and **absent P waves** (often hidden within the QRS complex) are characteristic of AVNRT.
- The patient's symptoms of recurrent chest pain, racing pulse, dizziness, and spontaneous recovery from loss of consciousness fit the episodic nature of **AVNRT**. The presence of two pathways (slow and fast) within the AV node facilitates the reentrant circuit.
*Pre-excitation of the ventricles*
- **Pre-excitation syndromes** (e.g., Wolff-Parkinson-White syndrome) involve an accessory pathway that bypasses the AV node, leading to a **delta wave** and **short PR interval** on the baseline ECG.
- While they can cause SVT, the ECG during tachycardia would typically show a **wide QRS complex** if the accessory pathway is part of the reentrant circuit (antidromic), or a narrow QRS with a visible P wave if orthodromic and the accessory pathway is used for retrograde conduction, which doesn't fully align with the absent P waves and typically *normal* QRS during tachycardia as described.
*Mutations in genes that code for myocyte ion channels*
- This refers to **channelopathies** (e.g., long QT syndrome, Brugada syndrome), which predispose to **ventricular arrhythmias** like **polymorphic ventricular tachycardia** and **ventricular fibrillation**.
- These conditions typically cause **wide QRS tachycardias** and have distinct ECG patterns (e.g., prolonged QT interval, Brugada pattern) not described here. The narrow QRS and regular rhythm point away from primary ventricular channelopathies as the cause of this specific tachycardia.
*Macroreentrant rhythm in the right atria through cavotricuspid isthmus*
- This describes **atrial flutter**, which typically presents with characteristic **"sawtooth" F waves** on ECG, representing atrial activity.
- While atrial flutter can cause recurrent episodes of rapid heart rate, the ECG description of **absent P waves** and a **narrow QRS complex** without F waves makes atrial flutter less likely.
*Fibrosis of the sinoatrial node and surrounding myocardium*
- **Sinoatrial node dysfunction (sick sinus syndrome)** can lead to bradycardia, sinus pauses, or alternating bradycardia and tachycardia (tachy-brady syndrome).
- It does not primarily cause the described paroxysmal narrow-complex tachycardia with absent P waves. The patient's symptoms are more consistent with an abrupt-onset, regular supraventricular tachycardia.
More ECG interpretation fundamentals US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.