Cardioversion and defibrillation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardioversion and defibrillation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardioversion and defibrillation US Medical PG Question 1: A 55-year-old man presents to his physician with a complaint of recurrent episodes of palpitations over the past 2 weeks. He also mentions that he tends to tire easily. He denies chest pain, breathlessness, dizziness, or syncope, but has a history of ischemic heart disease. He smokes 1 pack of cigarettes every day and drinks alcohol occasionally. The physical examination revealed a temperature of 36.9°C (98.4°F), a pulse of 124/min (irregular), a blood pressure of 142/86 mm Hg, and a respiratory rate of 16/min. Auscultation of his chest is normal with an absence of rales overall lung fields. An ECG was significant for fibrillatory waves and an irregular RR interval. Thus, the physician concludes that the symptoms are due to atrial fibrillation. The patient is prescribed oral diltiazem. Which of the following side effects should the physician warn the patient about?
- A. Stevens-Johnson syndrome
- B. Bloody diarrhea
- C. Hypoglycemia
- D. Bilateral pedal edema (Correct Answer)
- E. Multifocal atrial tachycardia
Cardioversion and defibrillation Explanation: ***Bilateral pedal edema***
- **Diltiazem**, a **calcium channel blocker**, can cause **peripheral vasodilation**, leading to fluid extravasation and **bilateral pedal edema**.
- This is a common and dose-dependent side effect, typically managed by dose reduction or switching to another agent if bothersome.
*Stevens-Johnson syndrome*
- This is a severe, life-threatening **cutaneous adverse drug reaction** characterized by widespread blistering and epidermal detachment, commonly associated with drugs like **antibiotics (sulfonamides)** or **anticonvulsants**.
- It is **not a typical side effect of diltiazem**, although rare idiosyncratic reactions to nearly any drug are possible.
*Bloody diarrhea*
- **Bloody diarrhea** is typically associated with **gastrointestinal infections** (e.g., *E. coli* O157:H7, *Shigella* spp.) or inflammatory bowel disease.
- It is **not a known side effect of diltiazem**; diltiazem may cause constipation, not diarrhea.
*Hypoglycemia*
- **Hypoglycemia** is a common side effect of **insulin** or **sulfonylurea medications** used to treat diabetes.
- Diltiazem does **not directly affect blood glucose levels** or cause hypoglycemia.
*Multifocal atrial tachycardia*
- **Multifocal atrial tachycardia (MAT)** is an **arrhythmia** characterized by at least three distinct P wave morphologies and an irregular rhythm.
- **Diltiazem** is used to **treat arrhythmias** like atrial fibrillation and would not typically cause a new, distinct arrhythmia such as MAT.
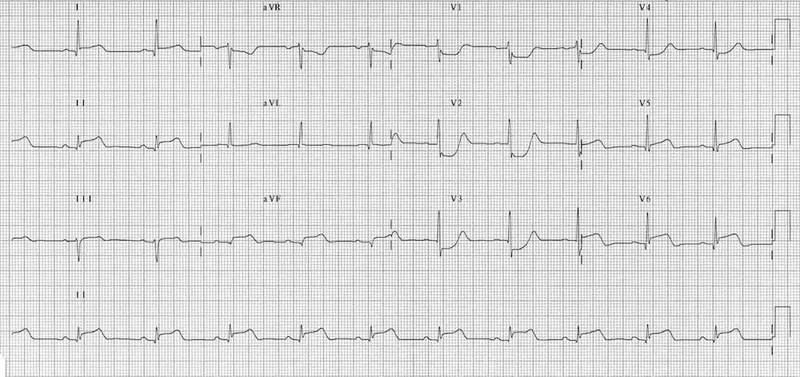
Cardioversion and defibrillation US Medical PG Question 2: A 42-year-old man is brought to the emergency department 20 minutes after the sudden onset of severe chest pain, diaphoresis, shortness of breath, and palpitations. His symptoms occurred while he was at a party with friends. He has smoked one pack of cigarettes daily for 24 years. He uses cocaine occasionally. The last use was three hours ago. He appears pale. His pulse is 110/min, blood pressure is 178/106 mm Hg, and respirations are 24/min. His pupils are dilated and react sluggishly to light. The lungs are clear to auscultation. An ECG shows tachycardia and ST segment elevation in leads II, III, and aVF. While recording the ECG, the patient loses consciousness. A photo of the ECG at that point is shown. Which of the following is the most appropriate next step in management?
- A. Administer lidocaine
- B. Unsynchronized cardioversion (Correct Answer)
- C. Administer epinephrine
- D. Coronary angiography
- E. Synchronized cardioversion
Cardioversion and defibrillation Explanation: ***Unsynchronized cardioversion***
- The ECG shows **ventricular fibrillation (VF)**, characterized by chaotic, irregular electrical activity without distinct QRS complexes, indicating a life-threatening arrhythmia.
- In a patient who has lost consciousness due to VF, immediate **defibrillation (unsynchronized cardioversion)** is crucial to restore normal sinus rhythm and prevent sudden cardiac death.
- Note: Unsynchronized cardioversion and defibrillation are **synonymous terms** for delivering an unsynchronized shock, with "defibrillation" being the preferred ACLS terminology for VF/pulseless VT.
*Administer lidocaine*
- While lidocaine is an **antiarrhythmic** used in some ventricular arrhythmias, it is typically administered after initial defibrillation attempts have failed or as an adjunct therapy.
- It is not the primary treatment for **unstable ventricular fibrillation**, which requires immediate electrical therapy.
*Administer epinephrine*
- Epinephrine is a **vasopressor** used during cardiac arrest to improve coronary and cerebral perfusion.
- It is administered during **cardiopulmonary resuscitation (CPR)** intervals, usually after initial defibrillation attempts, but not as the first line treatment for VF.
*Coronary angiography*
- Coronary angiography is an **invasive diagnostic procedure** to visualize coronary arteries and identify blockages, suggested by the patient's symptoms and ST elevation in the initial ECG leads.
- However, in the context of **cardiac arrest due to VF**, immediate life-saving interventions take precedence over diagnostic procedures.
*Synchronized cardioversion*
- **Synchronized cardioversion** delivers an electrical shock timed to the R-wave of the QRS complex to treat **tachyarrhythmias with a pulse** (e.g., ventricular tachycardia, atrial fibrillation with rapid ventricular response).
- It is **contraindicated in ventricular fibrillation** because there are no organized QRS complexes to synchronize with, and attempting synchronization can delay life-saving defibrillation.
Cardioversion and defibrillation US Medical PG Question 3: A 29-year-old woman with Wolff-Parkinson-White syndrome presents to her cardiologist’s office for a follow-up visit. She collapsed at her job and made a trip to the emergency department 1 week ago. At that time, she received a diagnosis of atrial fibrillation with rapid ventricular response and hemodynamic instability. While in the emergency department, she underwent direct-current cardioversion to return her heart to sinus rhythm. Her current medications include procainamide. At the cardiologist’s office, her heart rate is 61/min, respiratory rate is 16/min, the temperature is 36.5°C (97.7°F), and blood pressure is 118/60 mm Hg. Her cardiac examination reveals a regular rhythm and a I/VI systolic ejection murmur best heard at the right upper sternal border. An ECG obtained in the clinic is shown. Which of the following is the most appropriate treatment to prevent further episodes of tachyarrhythmia?
- A. Begin anticoagulation with dabigatran
- B. Add verapamil to her medication regimen
- C. Begin anticoagulation with warfarin
- D. Refer her for electrophysiology (EP) study and ablation (Correct Answer)
- E. Refer her for right heart catheterization
Cardioversion and defibrillation Explanation: ***Refer her for electrophysiology (EP) study and ablation***
- This patient has **Wolff-Parkinson-White (WPW) syndrome** and experienced a life-threatening episode of **atrial fibrillation with rapid ventricular response (AFib with RVR)** and **hemodynamic instability**, indicating a high-risk accessory pathway.
- **Catheter ablation** of the accessory pathway is the definitive treatment to eliminate the re-entrant circuit and prevent future tachyarrhythmia episodes and sudden cardiac death in symptomatic WPW patients.
*Begin anticoagulation with dabigatran*
- While anticoagulation is indicated for stroke prevention in AFib, this patient's primary risk is not stroke but rather recurrent, potentially fatal, **tachyarrhythmias due to WPW**.
- Current guidelines suggest that anticoagulation is not routinely needed for AFib in the setting of WPW unless other risk factors for stroke are present (e.g., high **CHA₂DS₂-VASc score** for non-valvular AFib), which are not mentioned here for a 29-year-old.
*Add verapamil to her medication regimen*
- **Calcium channel blockers** like verapamil are contraindicated in WPW syndrome with AFib.
- They can block the normal AV nodal conduction, shunting more impulses down the **accessory pathway** and potentially accelerating the ventricular rate, leading to **ventricular fibrillation**.
*Begin anticoagulation with warfarin*
- Similar to dabigatran, anticoagulation with warfarin is primarily for **stroke prevention in AFib**, not for preventing the tachyarrhythmia itself in WPW.
- The immediate and most critical concern for this patient is the risk of recurrent, life-threatening **re-entrant tachyarrhythmias** via the accessory pathway.
*Refer her for right heart catheterization*
- A **right heart catheterization** is used to measure pressures and oxygen saturations in the right side of the heart and pulmonary arteries, typically to evaluate for conditions like pulmonary hypertension or heart failure.
- It is not indicated for the diagnosis or treatment of **supraventricular tachycardias** or **accessory pathways** like in WPW syndrome.
Cardioversion and defibrillation US Medical PG Question 4: A 22-year-old woman presents to the emergency department feeling lightheaded and states that her heart is racing. She does not have a history of any chronic medical conditions. She is a college sophomore and plays club volleyball. Although she feels stressed about her upcoming final exams next week, she limits her caffeine intake to 3 cups of coffee per day to get a good night sleep. She notes that her brother takes medication for some type of heart condition, but she does not know the name of it. Both her parents are alive and well. She denies recent illness, injuries, or use of cigarettes, alcohol, or recreational drugs. The pertinent negatives from the review of systems include an absence of fever, nausea, vomiting, sweating, fatigue, or change in bowel habits. The vital signs include: temperature 36.8°C (98.2°F), heart rate 125/min, respiratory rate 15/min, blood pressure 90/75 mm Hg, and oxygen saturation of 100% on room air. The laboratory results are within normal limits. The ECG is significant for a shortened PR interval and widened QRS. Which of the following medications should the patient avoid in this scenario?
- A. Amlodipine
- B. Procainamide
- C. Diltiazem
- D. Verapamil (Correct Answer)
- E. Metoprolol
Cardioversion and defibrillation Explanation: ***Verapamil***
- The ECG findings of a **shortened PR interval** and **widened QRS** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, an accessory pathway that can bypass the AV node.
- Verapamil is a **non-dihydropyridine calcium channel blocker** that blocks the AV node and can paradoxically increase conduction down the accessory pathway in WPW, potentially leading to **ventricular fibrillation** if an atrial tachyarrhythmia is present.
- **Verapamil is the most classically contraindicated medication in WPW syndrome** and is the prototype drug to avoid in this condition.
*Amlodipine*
- Amlodipine is a **dihydropyridine calcium channel blocker** primarily used for hypertension and angina.
- It has minimal effect on the AV node and does not carry the same risk as non-dihydropyridine calcium channel blockers in WPW syndrome.
*Procainamide*
- **Procainamide is a Class Ia antiarrhythmic** that can be used to treat tachyarrhythmias related to WPW syndrome, as it prolongs the refractory period of the accessory pathway.
- It would be a potential **treatment option**, not a medication to avoid, especially for antidromic atrioventricular reentrant tachycardia (AVRT) in WPW.
*Diltiazem*
- Similar to verapamil, diltiazem is a **non-dihydropyridine calcium channel blocker** that blocks the AV node.
- While it carries similar risks to verapamil in WPW syndrome, **verapamil is more classically emphasized** as the prototypical contraindicated medication in medical education and board examinations.
*Metoprolol*
- Metoprolol is a **beta-blocker** that slows conduction through the AV node.
- While beta-blockers are also generally **avoided in WPW syndrome with atrial fibrillation**, **AV nodal blocking calcium channel blockers (especially verapamil) are considered the primary contraindication** due to more pronounced effects on accessory pathway conduction.
Cardioversion and defibrillation US Medical PG Question 5: A previously healthy 33-year-old woman comes to the emergency department because she could feel her heart racing intermittently for the last 2 hours. Each episode lasts about 10 minutes. She does not have any chest pain. Her mother died of a heart attack and her father had an angioplasty 3 years ago. She has smoked a half pack of cigarettes daily for 14 years. She drinks one to two beers daily. She appears anxious. Her temperature is 37.6°C (98.1°F), pulse is 160/min, and blood pressure is 104/76 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. An ECG is shown. Which of the following is the most appropriate initial step in management?
- A. Intravenous adenosine
- B. Aspirin
- C. Intravenous procainamide
- D. Vagal maneuvers (Correct Answer)
- E. Coronary angioplasty
Cardioversion and defibrillation Explanation: ***Vagal maneuvers***
- The ECG shows a **narrow complex tachycardia** at a rate of 160/min. Given the patient's stable hemodynamics (BP 104/76 mm Hg), **vagal maneuvers** are the most appropriate initial step to attempt to terminate the re-entrant rhythm, such as Valsalva maneuver or carotid sinus massage.
- Vagal maneuvers increase **parasympathetic tone** to the heart, which can slow conduction through the AV node and potentially break the re-entrant circuit causing the supraventricular tachycardia (SVT).
*Intravenous adenosine*
- **Adenosine** is a treatment for **narrow complex tachycardia** if vagal maneuvers fail, but it is not the *initial* step in a hemodynamically stable patient.
- It works by transiently blocking the **AV node**, interrupting re-entrant pathways.
*Intravenous procainamide*
- **Procainamide** is an antiarrhythmic typically used for **wide complex tachycardia** or for narrow complex tachycardias that are refractory to vagal maneuvers and adenosine, or when there is evidence of pre-excitation.
- It is not the first-line treatment for a stable **narrow complex tachycardia**.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used in the management of acute coronary syndromes or for cardiovascular disease prevention.
- It has no role in the immediate termination of a **tachyarrhythmia** like the one presented.
*Coronary angioplasty*
- **Coronary angioplasty** is a procedure used to open blocked or narrowed coronary arteries, usually for **acute coronary syndromes** or chronic stable angina.
- The patient presents with a **tachyarrhythmia** and no signs of acute ischemia (no chest pain, although risk factors are present), making angioplasty an inappropriate initial management step.
Cardioversion and defibrillation US Medical PG Question 6: Two days after admission for myocardial infarction and subsequent coronary angioplasty, a 65-year-old man becomes distressed and diaphoretic in the cardiac intensive care unit. Suddenly he is no longer responsive. Pulse oximetry does not show a tracing. He has a history of hypertension and depression. Prior to his admission, his medication included ramipril and aripiprazole. Examination shows no carotid pulse. An ECG is shown. After beginning chest compressions, which of the following is the most appropriate step in management of the patient?
- A. Intravenous procainamide
- B. Cardiac catheterization
- C. Intravenous amiodarone
- D. Intravenous magnesium sulfate
- E. Defibrillation (Correct Answer)
Cardioversion and defibrillation Explanation: ***Defibrillation***
- The ECG shows a **wide complex tachycardia** consistent with either **ventricular fibrillation (VF)** or **pulseless ventricular tachycardia (VT)**.
- In a patient who is **unresponsive and pulseless**, both VF and pulseless VT are treated identically with **immediate unsynchronized defibrillation** after initiating CPR, according to **ACLS guidelines**.
- **Defibrillation** is the definitive treatment to restore a perfusing rhythm and is the priority intervention after chest compressions have begun.
*Intravenous procainamide*
- **Procainamide** is an antiarrhythmic drug used for certain types of **stable ventricular tachycardia** or wide-complex tachycardia of uncertain type when the patient has a pulse.
- It is **contraindicated** in pulseless arrhythmias like VF or pulseless VT, where electrical therapy (defibrillation) is paramount.
- Administration would cause dangerous delay in definitive treatment.
*Cardiac catheterization*
- **Cardiac catheterization** is an invasive diagnostic and interventional procedure typically performed to evaluate and treat coronary artery disease.
- It is **not an immediate life-saving intervention** for a patient in **cardiac arrest**, which requires immediate electrical therapy.
- Catheterization may be considered after return of spontaneous circulation (ROSC) to address underlying ischemia.
*Intravenous amiodarone*
- **Amiodarone** is an antiarrhythmic agent used in **VF/pulseless VT that is refractory to initial defibrillation attempts** and after epinephrine administration.
- It is administered **after initial defibrillation attempts have failed**, not as the primary or first-line treatment.
- The ACLS algorithm recommends amiodarone after the third shock if VF/pulseless VT persists.
*Intravenous magnesium sulfate*
- **Magnesium sulfate** is the treatment of choice for **Torsades de Pointes**, a polymorphic ventricular tachycardia often associated with **prolonged QT interval**.
- The clinical presentation and ECG do not suggest Torsades de Pointes, and magnesium is not indicated as the initial treatment for VF or monomorphic VT.
- Magnesium may also be considered for refractory VF/VT with suspected hypomagnesemia.
Cardioversion and defibrillation US Medical PG Question 7: One hour after being admitted to the hospital for sharp, acute chest pain and diaphoresis, a 55-year-old woman with type 2 diabetes mellitus loses consciousness in the emergency department. There are no palpable pulses. Chest compressions are started. The patient has a history of breast cancer that was surgically treated 4 years ago. Prior to admission, the patient was on a long bus ride to visit her sister. Her medications include tamoxifen, atorvastatin, metoprolol, metformin, and insulin. Serum troponin levels are elevated. The cardiac rhythm is shown. Which of the following is the most appropriate next step in management?
- A. Defibrillation (Correct Answer)
- B. Coronary angiography
- C. Intravenous dextrose therapy
- D. Intravenous epinephrine therapy
- E. Intravenous glucagon therapy
Cardioversion and defibrillation Explanation: ***Defibrillation***
- The ECG shows **ventricular fibrillation (VF)**, characterized by chaotic, disorganized electrical activity with no identifiable QRS complexes and no palpable pulse. VF is a **shockable rhythm**.
- According to ACLS guidelines, the immediate management for VF is **unsynchronized defibrillation** along with high-quality chest compressions.
- Defibrillation depolarizes the myocardium simultaneously, allowing the sinoatrial node to potentially resume normal electrical activity and restore organized cardiac rhythm.
- For refractory VF after initial shocks, epinephrine and antiarrhythmics (amiodarone or lidocaine) are added.
*Intravenous epinephrine therapy*
- Epinephrine is a vasopressor used in cardiac arrest to increase coronary and cerebral perfusion pressure.
- While epinephrine is given during VF arrest, it is administered **after** the initial defibrillation attempts, not as the immediate first step.
- Epinephrine is the primary drug for **non-shockable rhythms** (PEA and asystole), but defibrillation takes priority in shockable rhythms like VF.
*Intravenous glucagon therapy*
- Glucagon is used for severe **hypoglycemia** or **beta-blocker/calcium channel blocker overdose**.
- While the patient takes metoprolol (a beta-blocker), the clinical presentation with elevated troponin, chest pain, and VF rhythm clearly indicates an acute cardiac event, not beta-blocker toxicity.
- Glucagon has no role in the immediate management of cardiac arrest from VF.
*Coronary angiography*
- Coronary angiography is indicated for **post-cardiac arrest care** after return of spontaneous circulation (ROSC), especially in patients with suspected acute coronary syndrome.
- The patient has elevated troponin suggesting acute MI, making early angiography important **after** successful resuscitation.
- However, angiography cannot be performed during active cardiac arrest; immediate defibrillation and CPR are required first.
*Intravenous dextrose therapy*
- Dextrose is used to treat **hypoglycemia**.
- While the patient has diabetes and takes insulin (hypoglycemia risk), the presentation with chest pain, elevated troponin, and VF rhythm indicates acute coronary syndrome with cardiac arrest.
- Hypoglycemia does not cause VF; the rhythm is consistent with ischemic cardiac arrest requiring immediate defibrillation.
Cardioversion and defibrillation US Medical PG Question 8: Two days after coronary artery stent placement for a posterior myocardial infarction, a 70-year-old woman complains of difficulty breathing and retrosternal chest pain. She has a history of atrial fibrillation, for which she takes verapamil. Following stent placement, the patient was started on aspirin and clopidogrel. She appears to be in acute distress and is disoriented. Respirations are 22/min. Pulse oximetry on room air shows an oxygen saturation of 80%. Diffuse crackles are heard on auscultation of the chest. The patient is intubated and mechanical ventilation is started. Shortly afterwards, she becomes unresponsive. Heart sounds are inaudible and her carotid pulses are not palpable. The cardiac monitor shows normal sinus rhythm with T-wave inversion. Which of the following is the most appropriate next step in management?
- A. Synchronized cardioversion
- B. Coronary angiography
- C. Unsynchronized cardioversion
- D. Intravenous epinephrine therapy
- E. Chest compressions (Correct Answer)
Cardioversion and defibrillation Explanation: ***Chest compressions***
- The patient presents with **pulselessness** despite a **normal sinus rhythm on the monitor** (pulseless electrical activity or PEA). In PEA, the immediate intervention is **high-quality chest compressions** as per ACLS guidelines.
- The preceding events (difficulty breathing, chest pain, disorientation, hypoxemia, diffuse crackles, and sudden unresponsiveness with unpalpable pulses) point towards acute cardiovascular collapse likely due to **cardiac tamponade** or other cause of obstructive shock, but the immediate response to pulselessness is compressions.
*Synchronized cardioversion*
- This is indicated for patients who are **unstable with a perfusing tachyarrhythmia**, such as unstable atrial fibrillation with rapid ventricular response or ventricular tachycardia with a pulse.
- The patient has no palpable pulses and exhibits **pulseless electrical activity (PEA)**, not a perfusing tachyarrhythmia, making synchronized cardioversion inappropriate.
*Coronary angiography*
- This is a diagnostic and interventional procedure used to assess and treat **coronary artery disease** or stent thrombosis.
- While post-stent complications are a concern, the patient is in **cardiac arrest (PEA)**, making immediate diagnostic angiography unfeasible and not the priority life-saving intervention.
*Unsynchronized cardioversion*
- Also known as **defibrillation**, this is indicated for **ventricular fibrillation (VF)** or **pulseless ventricular tachycardia (pVT)**.
- The cardiac monitor shows a **normal sinus rhythm**, not VF or pVT, therefore unsynchronized cardioversion is not indicated.
*Intravenous epinephrine therapy*
- Epinephrine is a **vasopressor** used during cardiac arrest to improve coronary and cerebral perfusion.
- While epinephrine is part of the **ACLS algorithm for PEA**, it is given *after* initiating chest compressions, not as the very first step in a pulseless patient.
Cardioversion and defibrillation US Medical PG Question 9: Match the following
A. Atrial fibrillation
B. Atrial flutter
C. PSVT
D. Ventricular tachycardia
- A. A-1, B-2, C-3, D-4
- B. A-2, B-1, C-3, D-4 (Correct Answer)
- C. A-1, B-2, C-4, D-3
- D. A-4, B-3, C-2, D-1
- E. A-2, B-1, C-4, D-3
Cardioversion and defibrillation Explanation: ***A-2, B-1, C-3, D-4***
- Image 2 shows irregularly irregular QRS complexes with no discernible P waves, which is characteristic of **atrial fibrillation**.
- Image 1 shows a "sawtooth" pattern of atrial activity, indicative of **atrial flutter**.
- Image 3 displays a narrow complex tachycardia with a very regular rhythm, consistent with **PSVT**.
- Image 4 demonstrates wide, regular QRS complexes without clear P waves, which is the hallmark of **ventricular tachycardia**.
*A-1, B-2, C-3, D-4*
- This option incorrectly matches atrial fibrillation with the "sawtooth" pattern (image 1) and atrial flutter with the irregularly irregular rhythm (image 2).
- Atrial fibrillation is characterized by the absence of discrete P waves and irregular ventricular response (image 2), while atrial flutter shows organized atrial activity with a "sawtooth" pattern (image 1).
*A-1, B-2, C-4, D-3*
- This option misidentifies image 1 as atrial fibrillation and image 2 as atrial flutter, which are reversed.
- It also incorrectly matches PSVT with image 4 (ventricular tachycardia) and ventricular tachycardia with image 3 (PSVT).
*A-2, B-1, C-4, D-3*
- This option correctly identifies atrial fibrillation (A-2) and atrial flutter (B-1), but incorrectly swaps the ventricular and supraventricular tachycardias.
- Image 3 shows narrow complex tachycardia (PSVT), not the wide complex pattern of ventricular tachycardia seen in image 4.
*A-4, B-3, C-2, D-1*
- This option incorrectly matches all the rhythms to the wrong images, demonstrating a fundamental misunderstanding of their characteristic ECG features.
- For example, it matches atrial fibrillation to image 4 (ventricular tachycardia) and ventricular tachycardia to image 1 (atrial flutter).
Cardioversion and defibrillation US Medical PG Question 10: A patient with a history of hypertension presents with atrial fibrillation, shortness of breath, and bilateral basal crackles on auscultation. Which of the following would be the least important in the management of this patient?
- A. Start on anticoagulants
- B. Start β-blocker
- C. Cardioversion to correct rhythm if hemodynamically remains unstable even after medical management
- D. IV Digoxin for control rate (Correct Answer)
- E. Administer diuretics for fluid overload
Cardioversion and defibrillation Explanation: ***IV Digoxin for control rate***
- While **Digoxin** can be used for **rate control in atrial fibrillation**, its role is limited, especially in patients with **congestive heart failure** due to its delayed onset of action and narrow therapeutic window.
- In a patient with **shortness of breath** and **bilateral basal crackles** (suggesting acute decompensated heart failure), rapid rate control with a **β-blocker** or **calcium channel blocker** is usually preferred for immediate symptom relief.
- Digoxin is not first-line therapy in this acute setting and is therefore the **least important** among the management options listed.
*Start on anticoagulants*
- **Anticoagulation** is crucial for patients with **atrial fibrillation** to prevent **thromboembolic events**, particularly strokes.
- Given the patient's history of **hypertension** and presence of **atrial fibrillation**, their **CHA2DS2-VASc score** is likely elevated, necessitating anticoagulation.
*Start β-blocker*
- **Beta-blockers** are first-line agents for **rate control in atrial fibrillation**, especially in patients with **hypertension** and signs of **heart failure**.
- They effectively reduce ventricular response rate, improve diastolic filling, and can alleviate symptoms like **shortness of breath**.
*Cardioversion to correct rhythm if hemodynamically remains unstable even after medical management*
- If a patient with **atrial fibrillation** and signs of **heart failure** remains **hemodynamically unstable** despite initial medical management (e.g., rate control, diuretics), **cardioversion** (electrical or pharmacological) is an essential intervention to restore sinus rhythm.
- This can acutely improve cardiac output and resolve symptoms of **decompensated heart failure**.
*Administer diuretics for fluid overload*
- **Diuretics** (e.g., furosemide) are essential for managing the **volume overload** in this patient, as evidenced by **bilateral basal crackles** and **shortness of breath**.
- Reducing preload helps improve **pulmonary congestion** and alleviates acute heart failure symptoms.
- Loop diuretics are a cornerstone of acute decompensated heart failure management.
More Cardioversion and defibrillation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.