Atrial fibrillation and flutter US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Atrial fibrillation and flutter. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Atrial fibrillation and flutter US Medical PG Question 1: A 21-year-old woman presents with palpitations and anxiety. She had a recent outpatient ECG that was suggestive of supraventricular tachycardia, but her previous physician failed to find any underlying disease. No other significant past medical history. Her vital signs include blood pressure 102/65 mm Hg, pulse 120/min, respiratory rate 17/min, and temperature 36.5℃ (97.7℉). Electrophysiological studies reveal an atrioventricular nodal reentrant tachycardia. The patient refuses an ablation procedure so it is decided to perform synchronized cardioversion with consequent ongoing management with verapamil. Which of the following ECG features should be monitored in this patient during treatment?
- A. Amplitude and direction of the T wave
- B. Length of QRS complex
- C. Length of QT interval
- D. Length of PR interval (Correct Answer)
- E. QRS complex amplitude
Atrial fibrillation and flutter Explanation: ***Length of PR interval***
- Verapamil is a **non-dihydropyridine calcium channel blocker** that primarily acts on the **AV node** to slow conduction.
- Monitoring the **PR interval** is crucial because excessive slowing of AV nodal conduction can lead to **AV block**, which is indicated by a prolonged PR interval.
*Amplitude and direction of the T wave*
- Changes in T-wave amplitude and direction are often associated with **myocardial ischemia** or **electrolyte imbalances**, which are not the primary concerns with verapamil.
- While verapamil can affect repolarization, the most direct and common adverse effect related to its mechanism of action on the AV node is not primarily reflected in T-wave changes.
*Length of QRS complex*
- The QRS complex duration primarily reflects **ventricular depolarization** and is typically affected by medications that alter conduction through the His-Purkinje system or within the ventricles, such as antiarrhythmics like **flecainide** or **amiodarone**.
- Verapamil's main action is on the AV node, so it generally does not significantly prolong the QRS complex unless there is pre-existing conduction system disease.
*Length of QT interval*
- The QT interval represents **ventricular repolarization**, and its prolongation can lead to **Torsades de Pointes**, a life-threatening arrhythmia.
- While many antiarrhythmics can prolong the QT interval, **verapamil is not known to significantly prolong the QT interval** and is generally considered safe in this regard.
*QRS complex amplitude*
- Changes in QRS amplitude can indicate conditions like **pericardial effusion**, **cardiomyopathy**, or changes in ventricular mass.
- These are generally not direct or common side effects of verapamil therapy, which primarily focuses on AV nodal conduction.
Atrial fibrillation and flutter US Medical PG Question 2: A 75-year-old man presents to the emergency department after an episode of syncope while walking outside with his wife. His wife states that he suddenly appeared pale and collapsed to the ground. She says he remained unconscious for 1 minute. He says he noticed a fluttering in his chest and excessive sweating before the episode. He has type 2 diabetes mellitus, essential hypertension, and chronic stable angina. He has not started any new medications in the past few months. Vital signs reveal: temperature 37.0°C (98.6°F), blood pressure 135/72 mm Hg, and pulse 72/min. Physical examination is unremarkable. ECG shows an old bifascicular block. Echocardiogram and 24-hour Holter monitoring are normal. Which of the following is the best next step in the evaluation of this patient's condition?
- A. Cardiac enzymes
- B. Continuous loop recorder (Correct Answer)
- C. Valsalva maneuver
- D. Electroencephalography (EEG)
- E. Tilt-table test
Atrial fibrillation and flutter Explanation: ***Continuous loop recorder***
- This patient's syncope is preceded by **palpitations (fluttering in chest)** and **sweating**, suggesting a cardiac etiology, specifically a **transient arrhythmia** not captured on a standard ECG or 24-hour Holter.
- A continuous loop recorder provides prolonged monitoring (months to years), increasing the likelihood of detecting intermittent arrhythmias responsible for syncopal episodes.
*Cardiac enzymes*
- While cardiac enzymes (e.g., troponin) are crucial for evaluating **acute myocardial ischemia** or infarction, the patient presents with syncope and no new chest pain, and his stable angina suggests chronic disease rather than an acute event leading to syncope in this specific instance.
- An **ECG showing an old bifascicular block** and an **unremarkable physical exam** make an acute cardiac event less likely as the primary cause of syncope when an arrhythmia is suspected.
*Valsalva maneuver*
- The Valsalva maneuver is a diagnostic tool often used to differentiate between certain types of **tachyarrhythmias** or to evaluate for **autonomic dysfunction**, but it is not an evaluative step for a patient presenting with unexplained syncope where an arrhythmia has not yet been documented.
- It would not help in identifying the cause of intermittent syncope in a patient whose standard workup has been unremarkable, as it's a test for immediate physiological response, not prolonged cardiac rhythm monitoring.
*Electroencephalography (EEG)*
- EEG is indicated when **seizure disorder** is suspected as the cause of loss of consciousness, often characterized by tonic-clonic movements, post-ictal confusion, or focal neurologic signs, which are absent in this patient's presentation.
- The patient's pre-syncopal symptoms of **palpitations and sweating** point away from a seizure and towards a cardiac cause.
*Tilt-table test*
- A tilt-table test is used to evaluate for **vasovagal syncope** or **postural orthostatic tachycardia syndrome (POTS)**, often considered when other cardiac causes are ruled out or when syncope is typically triggered by prolonged standing.
- Given the patient's pre-syncopal **palpitations**, a **cardiac arrhythmia** remains a higher suspicion than vasovagal syncope at this stage, especially after normal echocardiogram and Holter monitoring, necessitating further arrhythmia investigation.
Atrial fibrillation and flutter US Medical PG Question 3: A 26-year-old nursing home staff presents to the emergency room with complaints of palpitations and chest pain for the past 2 days. She was working at the nursing home for the last year but has been trying to get into modeling for the last 6 months and trying hard to lose weight. She is a non-smoker and occasionally drinks alcohol on weekends with friends. On examination, she appears well nourished and is in no distress. The blood pressure is 150/84 mm Hg and the pulse is 118/min. An ECG shows absent P waves. All other physical findings are normal. What is the probable diagnosis?
- A. Anorexia nervosa
- B. Graves' disease
- C. Hashimoto thyroiditis
- D. Toxic nodular goiter
- E. Factitious thyrotoxicosis (Correct Answer)
Atrial fibrillation and flutter Explanation: ***Factitious thyrotoxicosis***
- The patient's profession as a nursing home staff member provides access to medications, and her attempts to lose weight for modeling suggest a motive for **self-administration of thyroid hormones**.
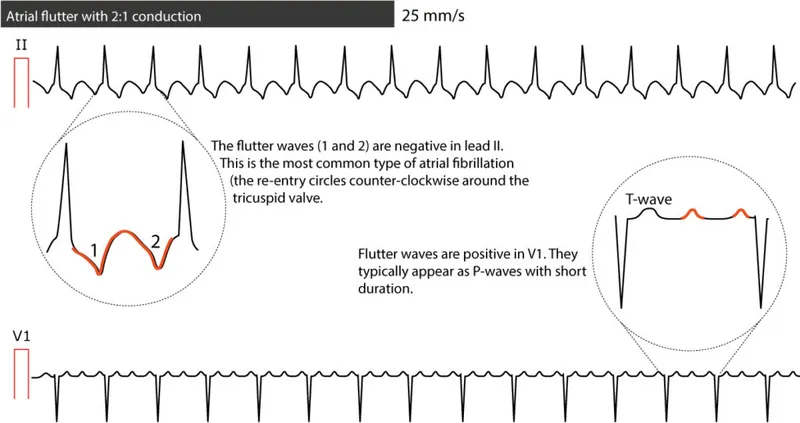
- **Absent P waves** on ECG along with **palpitations and tachycardia** are consistent with atrial arrhythmias often seen in thyrotoxicosis, but the overall presentation with a desire for weight loss points towards an exogenous source.
*Anorexia nervosa*
- While patients with anorexia nervosa do try to lose weight, their presentation is typically associated with **bradycardia**, not the tachycardia and elevated blood pressure seen here.
- ECG findings in anorexia nervosa would more likely show **QT prolongation** or other conduction abnormalities due to electrolyte imbalances, not specifically absent P waves caused by arrhythmia.
*Graves' disease*
- Graves' disease is an autoimmune condition causing hyperthyroidism, presenting with similar symptoms like **tachycardia and palpitations**. However, it is typically associated with other systemic findings such as **ophthalmopathy (exophthalmos)**, **pretibial myxedema**, or a palpable goiter, none of which are mentioned.
- Laboratory findings would show **high T3/T4** with **low TSH**, and often **positive TSH receptor antibodies**, differentiating it from factitious causes.
*Hashimoto thyroiditis*
- Hashimoto thyroiditis is an **autoimmune cause of hypothyroidism**, characterized by fatigue, weight gain, and bradycardia, which are opposite to the patient's symptoms of palpitations, tachycardia, and weight loss efforts.
- While it can initially present with transient hyperthyroidism (hashitoxicosis), the chronic state is hypothyroidism, and the ECG would not typically show absent P waves.
*Toxic nodular goiter*
- A toxic nodular goiter causes hyperthyroidism due to **autonomous thyroid nodules**, leading to symptoms similar to Graves' disease (palpitations, weight loss).
- However, the physical examination would usually reveal a **palpable nodular goiter**, which is not mentioned in this case, making it a less likely diagnosis compared to factitious thyrotoxicosis given the context.
Atrial fibrillation and flutter US Medical PG Question 4: A 29-year-old woman with Wolff-Parkinson-White syndrome presents to her cardiologist’s office for a follow-up visit. She collapsed at her job and made a trip to the emergency department 1 week ago. At that time, she received a diagnosis of atrial fibrillation with rapid ventricular response and hemodynamic instability. While in the emergency department, she underwent direct-current cardioversion to return her heart to sinus rhythm. Her current medications include procainamide. At the cardiologist’s office, her heart rate is 61/min, respiratory rate is 16/min, the temperature is 36.5°C (97.7°F), and blood pressure is 118/60 mm Hg. Her cardiac examination reveals a regular rhythm and a I/VI systolic ejection murmur best heard at the right upper sternal border. An ECG obtained in the clinic is shown. Which of the following is the most appropriate treatment to prevent further episodes of tachyarrhythmia?
- A. Begin anticoagulation with dabigatran
- B. Add verapamil to her medication regimen
- C. Begin anticoagulation with warfarin
- D. Refer her for electrophysiology (EP) study and ablation (Correct Answer)
- E. Refer her for right heart catheterization
Atrial fibrillation and flutter Explanation: ***Refer her for electrophysiology (EP) study and ablation***
- This patient has **Wolff-Parkinson-White (WPW) syndrome** and experienced a life-threatening episode of **atrial fibrillation with rapid ventricular response (AFib with RVR)** and **hemodynamic instability**, indicating a high-risk accessory pathway.
- **Catheter ablation** of the accessory pathway is the definitive treatment to eliminate the re-entrant circuit and prevent future tachyarrhythmia episodes and sudden cardiac death in symptomatic WPW patients.
*Begin anticoagulation with dabigatran*
- While anticoagulation is indicated for stroke prevention in AFib, this patient's primary risk is not stroke but rather recurrent, potentially fatal, **tachyarrhythmias due to WPW**.
- Current guidelines suggest that anticoagulation is not routinely needed for AFib in the setting of WPW unless other risk factors for stroke are present (e.g., high **CHA₂DS₂-VASc score** for non-valvular AFib), which are not mentioned here for a 29-year-old.
*Add verapamil to her medication regimen*
- **Calcium channel blockers** like verapamil are contraindicated in WPW syndrome with AFib.
- They can block the normal AV nodal conduction, shunting more impulses down the **accessory pathway** and potentially accelerating the ventricular rate, leading to **ventricular fibrillation**.
*Begin anticoagulation with warfarin*
- Similar to dabigatran, anticoagulation with warfarin is primarily for **stroke prevention in AFib**, not for preventing the tachyarrhythmia itself in WPW.
- The immediate and most critical concern for this patient is the risk of recurrent, life-threatening **re-entrant tachyarrhythmias** via the accessory pathway.
*Refer her for right heart catheterization*
- A **right heart catheterization** is used to measure pressures and oxygen saturations in the right side of the heart and pulmonary arteries, typically to evaluate for conditions like pulmonary hypertension or heart failure.
- It is not indicated for the diagnosis or treatment of **supraventricular tachycardias** or **accessory pathways** like in WPW syndrome.
Atrial fibrillation and flutter US Medical PG Question 5: A 24-year-old woman comes to the physician for a routine health maintenance examination. She feels well. On questioning, she has had occasional morning dizziness and palpitations during the past year. She is a graduate student. She does not smoke and drinks 1–2 glasses of wine on the weekends. Her vital signs are within normal limits. Physical examination shows an irregular pulse. On auscultation of the chest, S1 and S2 are normal and there are no murmurs. An ECG is shown. Which of the following is the most appropriate next step in management?
- A. Reassurance (Correct Answer)
- B. Event recorder implantation
- C. Administration of flecainide
- D. Administration of metoprolol
- E. Stress echocardiography
Atrial fibrillation and flutter Explanation: ***Reassurance***
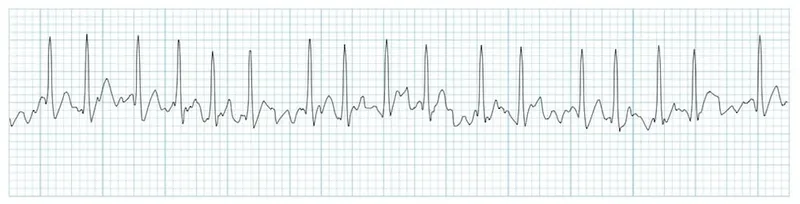
- This young, healthy patient has **occasional, mild symptoms** (morning dizziness and palpitations) with stable vital signs and a normal cardiac examination except for an irregular pulse.
- The ECG shown likely demonstrates **benign ectopy** such as premature atrial contractions (PACs) or premature ventricular contractions (PVCs), which are common in young adults and typically benign.
- In the absence of **red flags** (syncope, family history of sudden cardiac death, structural heart disease, hemodynamic instability), reassurance is appropriate for asymptomatic or minimally symptomatic patients with benign arrhythmias.
- No intervention is needed unless symptoms become more severe or frequent.
*Event recorder implantation*
- An event recorder would be considered if the patient had **significant symptoms** (syncope, presyncope) or if the routine ECG was **normal** and there was a need to capture intermittent arrhythmias.
- Since an ECG was obtained during the visit showing the irregular rhythm, further rhythm monitoring is not the next step unless the diagnosis remains unclear or symptoms worsen.
- This represents overinvestigation for likely benign ectopy in a young, healthy patient.
*Administration of flecainide*
- Flecainide is a **Class IC antiarrhythmic** used for specific arrhythmias like atrial fibrillation or supraventricular tachycardia.
- It should never be initiated without a clear diagnosis and is **contraindicated** in patients with structural heart disease due to proarrhythmic risk.
- Empiric antiarrhythmic therapy is not warranted for occasional, mild symptoms with likely benign ectopy.
*Administration of metoprolol*
- Metoprolol is a **beta-blocker** that can reduce the frequency of ectopic beats and control heart rate in certain arrhythmias.
- While it could be considered if symptoms were bothersome despite reassurance, it is not the first-line approach for a minimally symptomatic patient with benign ectopy.
- Medical therapy should be reserved for patients with significant symptoms affecting quality of life.
*Stress echocardiography*
- Stress echocardiography evaluates for **exercise-induced ischemia** or valvular abnormalities provoked by exertion.
- This patient has no symptoms of angina, dyspnea, or features suggesting structural heart disease on examination.
- There is no indication for stress testing in a young patient with isolated benign ectopy and no cardiovascular risk factors.
Atrial fibrillation and flutter US Medical PG Question 6: A 50-year-old man with a history of atrial fibrillation presents to his cardiologist’s office for a follow-up visit. He recently started treatment with an anti-arrhythmic drug to prevent future recurrences and reports that he has been feeling well and has no complaints. The physical examination shows that the arrhythmia appears to have resolved; however, there is now mild bradycardia. In addition, the electrocardiogram recording shows a slight prolongation of the PR and QT intervals. Which of the following drugs was most likely used to treat this patient?
- A. Metoprolol
- B. Sotalol (Correct Answer)
- C. Propranolol
- D. Verapamil
- E. Carvedilol
Atrial fibrillation and flutter Explanation: ***Sotalol***
- **Sotalol** is a **beta-blocker** and a **Class III antiarrhythmic** drug, meaning it blocks potassium channels.
- This dual action explains the **bradycardia** (beta-blockade) and the **prolongation of the PR and QT intervals** (potassium channel blockade), which are characteristic side effects.
*Metoprolol*
- **Metoprolol** is a **selective beta-1 blocker** (Class II antiarrhythmic) that would cause **bradycardia** and **PR prolongation**, but it does not typically prolong the **QT interval**.
- It primarily affects the heart rate and AV nodal conduction without significant potassium channel blocking properties.
*Propranolol*
- **Propranolol** is a **non-selective beta-blocker** (Class II antiarrhythmic) that would cause **bradycardia** and **PR prolongation**.
- Similar to metoprolol, it does not typically prolong the **QT interval**.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that causes **bradycardia** and **PR prolongation**.
- However, it does not prolong the **QT interval**; instead, it can sometimes shorten it.
*Carvedilol*
- **Carvedilol** is a **non-selective beta-blocker** with **alpha-1 blocking properties** (Class II antiarrhythmic), leading to **bradycardia** and **PR prolongation**.
- It does not have effects on potassium channels that would lead to **QT prolongation**.
Atrial fibrillation and flutter US Medical PG Question 7: A 70-year-old male presents for an annual exam. His past medical history is notable for shortness of breath when he sleeps, and upon exertion. Recently he has experienced dyspnea and lower extremity edema that seems to be worsening. Both of these symptoms have resolved since he was started on several medications and instructed to weigh himself daily. Which of the following is most likely a component of his medical management?
- A. Lidocaine
- B. Verapamil
- C. Carvedilol (Correct Answer)
- D. Aspirin
- E. Ibutilide
Atrial fibrillation and flutter Explanation: ***Carvedilol***
- The patient exhibits classic symptoms of **heart failure**, such as **dyspnea on exertion**, **orthopnea** (shortness of breath when he sleeps), and **lower extremity edema**.
- **Beta-blockers** like carvedilol are essential for managing **chronic heart failure** by reducing myocardial oxygen demand and improving cardiac function.
*Lidocaine*
- **Lidocaine** is primarily an **antiarrhythmic drug** used for acute treatment of **ventricular arrhythmias**, not for chronic heart failure management.
- It works by blocking sodium channels and has no direct benefit in addressing the underlying pathophysiology of heart failure.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** typically used for hypertension, angina, and supraventricular tachyarrhythmias.
- It can have **negative inotropic effects**, which are generally contraindicated or used with extreme caution in patients with **systolic heart failure** due to its potential to worsen cardiac function.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used for primary or secondary prevention of **atherosclerotic cardiovascular disease** (e.g., in patients with coronary artery disease).
- It does not directly manage the symptoms or pathophysiology of **heart failure** unless there is a coexisting ischemic etiology.
*Ibutilide*
- **Ibutilide** is an **antiarrhythmic drug** specifically used for the rapid conversion of **atrial flutter and atrial fibrillation** of recent onset to sinus rhythm.
- It is not a medication used for the long-term management of **heart failure** symptoms described in the patient.
Atrial fibrillation and flutter US Medical PG Question 8: A 65-year-old man with hypertension and paroxysmal atrial fibrillation presents to his cardiologist for follow-up after recently starting metoprolol for rate control. His EKG shows an atrial rate of 260/min with ventricular rate of 50/min on an irregular baseline. An echocardiogram from his previous visit revealed no evidence of hypokinesis or hypertrophy with functionally intact valves. The patient does not drink alcohol and had no evidence of liver dysfunction in prior studies. What is the best medication for rhythm control in this patient?
- A. Amiodarone
- B. Flecainide (Correct Answer)
- C. Procainamide
- D. Verapamil
- E. Mexiletine
Atrial fibrillation and flutter Explanation: ***Flecainide***
- **Flecainide** is a **Class IC antiarrhythmic** medication that is effective for rhythm control in patients with **paroxysmal atrial fibrillation** and no structural heart disease.
- The patient's echocardiogram showed no evidence of hypokinesis or hypertrophy, with functionally intact valves, indicating the **absence of structural heart disease**, which is a prerequisite for using Class IC agents like flecainide.
*Amiodarone*
- **Amiodarone** is a potent antiarrhythmic but is associated with numerous significant **extracardiac side effects**, including **pulmonary fibrosis**, **thyroid dysfunction**, and liver toxicity.
- It is generally reserved for patients with structural heart disease or those who have failed other antiarrhythmic therapies due to its extensive side effect profile.
*Procainamide*
- **Procainamide** is a **Class IA antiarrhythmic** that has a high incidence of side effects, including **drug-induced lupus**, and is typically used for acute management of arrhythmias, not long-term rhythm control in this setting.
- Its use is limited by its short half-life and significant proarrhythmic potential, especially in patients with structural heart disease or LV dysfunction.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** primarily used for **rate control** in atrial fibrillation, not rhythm control.
- The patient is already on metoprolol for rate control, and the question specifically asks for a medication for rhythm control.
*Mexiletine*
- **Mexiletine** is a **Class IB antiarrhythmic** agent primarily used for treating **ventricular arrhythmias**, particularly in the setting of myocardial infarction.
- It is not typically used for rhythm control in atrial fibrillation and has limited efficacy in this context.
Atrial fibrillation and flutter US Medical PG Question 9: A 44-year-old woman comes to the physician because of progressively worsening shortness of breath with exertion and intermittent palpitations over the last 2 months. She has had neither chest pain nor a cough. Her pulse is 124/min and irregular. Physical examination shows a grade 4/6 high-pitched holosystolic murmur that is best heard at the apex and radiates to the back. The murmur increases in intensity when she clenches her hands into fists. The lungs are clear to auscultation. Further evaluation of this patient is most likely to show which of the following findings?
- A. Obstruction of the right marginal artery on coronary angiogram
- B. Diffuse ST elevations on electrocardiogram
- C. Dilation of left atrium on echocardiogram (Correct Answer)
- D. Reversible area of myocardial ischemia on nuclear stress test
- E. Pulmonary artery thrombus on computed tomography scan
Atrial fibrillation and flutter Explanation: ***Dilation of left atrium on echocardiogram***
- The patient's symptoms of **shortness of breath**, **palpitations**, and an **irregular pulse** suggest a cardiac etiology, specifically a **valvular problem**. The **holosystolic murmur** best heard at the **apex** and radiating to the **back**, which increases with handgrip (a maneuver that increases afterload), is highly characteristic of **mitral regurgitation**.
- **Chronic mitral regurgitation** leads to **volume overload** in the left atrium, causing its **dilation** as it tries to accommodate the increased blood flow from both the pulmonary veins and the regurgitant jet from the left ventricle. This can also lead to **atrial fibrillation**, explaining the irregular pulse and palpitations.
*Obstruction of the right marginal artery on coronary angiogram*
- This finding would indicate **coronary artery disease** affecting the right coronary artery, typically presenting with **chest pain** or angina, which the patient explicitly denies.
- While coronary artery disease can cause shortness of breath, the distinctive **holosystolic murmur** and its radiation are not primary features of isolated coronary artery obstruction.
*Diffuse ST elevations on electrocardiogram*
- **Diffuse ST elevations** are typically seen in conditions like **pericarditis**, which often presents with pleuritic chest pain and a pericardial friction rub, none of which are described.
- It could also indicate an ST-elevation myocardial infarction (STEMI), but the 2-month history and the specific murmur point away from an acute coronary event.
*Reversible area of myocardial ischemia on nuclear stress test*
- This would suggest **ischemic heart disease**, again primarily indicated by **angina** or exertional chest discomfort, which is absent in this patient.
- While ischemia can cause shortness of breath and palpitations, it does not explain the characteristic **holosystolic murmur** and its specific radiation.
*Pulmonary artery thrombus on computed tomography scan*
- A **pulmonary artery thrombus** (pulmonary embolism) would typically cause **acute dyspnea**, pleuritic chest pain, and sometimes hemoptysis, which are not mentioned.
- While it can cause palpitations and an irregular pulse (due to right heart strain), it does not account for the **holosystolic murmur** heard at the apex and radiating to the back.
Atrial fibrillation and flutter US Medical PG Question 10: A 63-year-old woman presents to the primary care physician’s clinic complaining of fatigue, diarrhea, headaches, and a loss of appetite. She denies any personal history of blood clots in her past, but she says that her mother has also had to be treated for pulmonary embolism in the recent past. Her past medical history is significant for preeclampsia, hypertension, polycystic ovarian syndrome, and hypercholesterolemia. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and she currently denies any illicit drug use, although she has a remote past of injection drug use with heroin. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 111/min and irregular, and respiratory rate 17/min. On physical examination, her pulses are bounding and complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 91% on room air and electrocardiogram (ECG) showed atrial fibrillation. Upon further discussion with the patient, her physician discovers that she is having some cognitive difficulty. The laboratory results reveal: mean corpuscular volume (MCV) 111 fL; hemoglobin (Hgb) 9.3 g/dL; methylmalonic acid (MMA) and homocysteine are both elevated. Schilling test is positive. What is the next best step in the management of this patient?
- A. Lifelong Vitamin B12 supplementation (Correct Answer)
- B. Obtain a Coomb’s test
- C. Lifelong folic acid supplementation
- D. Give corticosteroids and iron supplementation
- E. Iron supplementation for 4–6 months
Atrial fibrillation and flutter Explanation: ***Lifelong Vitamin B12 supplementation***
- The patient's **macrocytic anemia** (MCV 111 fL, Hgb 9.3 g/dL), elevated methylmalonic acid (MMA) and homocysteine, and a positive Schilling test strongly indicate **pernicious anemia**, a form of **Vitamin B12 deficiency** due to inadequate intrinsic factor.
- **Pernicious anemia** requires lifelong Vitamin B12 supplementation, usually via intramuscular injections due to impaired absorption.
- The **elevated MMA** is particularly specific for B12 deficiency (as opposed to folate deficiency, which does not elevate MMA).
*Obtain a Coombs test*
- A **Coombs test** is used to detect antibodies that coat red blood cells, which is relevant in **autoimmune hemolytic anemia**.
- The patient's clinical picture, particularly the elevated MMA/homocysteine and positive Schilling test, points away from **hemolytic anemia** and towards **Vitamin B12 deficiency**.
*Lifelong folic acid supplementation*
- While **folic acid deficiency** can also cause **macrocytic anemia** and elevated homocysteine, it does **not** cause elevated MMA.
- Supplementing with **folic acid alone** in the presence of **Vitamin B12 deficiency** can mask the hematological symptoms while allowing neurological damage to progress.
*Give corticosteroids and iron supplementation*
- **Corticosteroids** are typically used in conditions like **autoimmune hemolytic anemia** or other autoimmune diseases, which are not suggested by the lab results.
- **Iron supplementation** is indicated for **iron-deficiency anemia**, which presents with **microcytic** or **normocytic anemia**, not the **macrocytic anemia** seen here.
*Iron supplementation for 4–6 months*
- This intervention is appropriate for **iron-deficiency anemia**, which is characterized by **microcytic anemia** and low ferritin/iron levels.
- The patient's **macrocytic anemia** and elevated MMA/homocysteine rule out **iron-deficiency anemia** as the primary issue.
More Atrial fibrillation and flutter US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.