Antiarrhythmic medications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antiarrhythmic medications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antiarrhythmic medications US Medical PG Question 1: A 54-year-old man comes to the emergency department because of episodic palpitations for the past 12 hours. He has no chest pain. He has coronary artery disease and type 2 diabetes mellitus. His current medications include aspirin, insulin, and atorvastatin. His pulse is 155/min and blood pressure is 116/77 mm Hg. Physical examination shows no abnormalities. An ECG shows monomorphic ventricular tachycardia. An amiodarone bolus and infusion is given, and the ventricular tachycardia converts to normal sinus rhythm. He is discharged home with oral amiodarone. Which of the following is the most likely adverse effect associated with long-term use of this medication?
- A. Angle-closure glaucoma
- B. Hepatic adenoma
- C. Shortened QT interval on ECG
- D. Progressive multifocal leukoencephalopathy
- E. Chronic interstitial pneumonitis (Correct Answer)
Antiarrhythmic medications Explanation: ***Chronic interstitial pneumonitis***
- **Amiodarone** is known to cause several dose-dependent adverse effects, including **pulmonary toxicity** in the form of **interstitial pneumonitis** or fibrosis.
- This adverse effect can manifest as progressive dyspnea, cough, and infiltrates on chest imaging, requiring careful monitoring during long-term use.
*Angle-closure glaucoma*
- While some medications can cause **angle-closure glaucoma**, it is **not a classic or common adverse effect of amiodarone**.
- **Topiramate** and **sulfonamides** are more commonly associated with acute angle-closure glaucoma.
*Hepatic adenoma*
- **Hepatic adenomas** are typically associated with **oral contraceptive use** and sometimes **anabolic steroid use**, not amiodarone.
- Amiodarone can cause **hepatic toxicity** (elevated transaminases, hepatitis), but not specifically hepatic adenoma.
*Shortened QT interval on ECG*
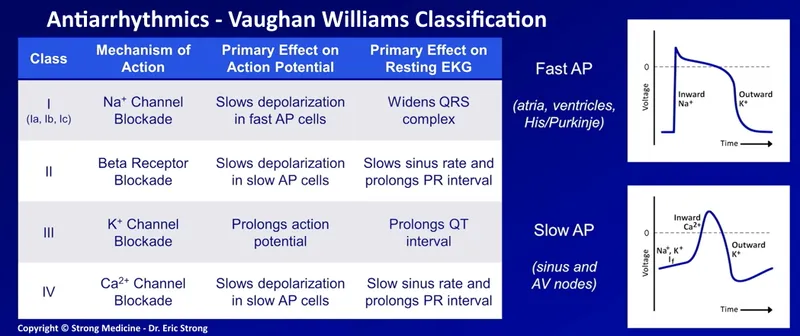
- **Amiodarone** is a Class III antiarrhythmic drug that **prolongs the QT interval** by blocking potassium channels, which is its mechanism of action for suppressing arrhythmias.
- Therefore, a shortened QT interval is the **opposite of what would be expected with amiodarone use**.
*Progressive multifocal leukoencephalopathy*
- **Progressive multifocal leukoencephalopathy (PML)** is a rare, severe opportunistic infection of the brain caused by the **JC virus**, typically seen in immunocompromised individuals.
- It is **not an adverse effect of amiodarone**; drugs like natalizumab or rituximab, which affect the immune system, are associated with PML.
Antiarrhythmic medications US Medical PG Question 2: A 53-year-old man with obesity and heart disease presents to your outpatient clinic with complaints of orthopnea, significant dyspnea on minimal exertion, nausea, vomiting, and diarrhea. He says that his old doctor gave him "some pills" that he takes in varying amounts every morning. Physical exam is significant for a severely displaced point of maximal impulse, bilateral rales in the lower lung fields, an S3 gallop, and hepatomegaly. You decide to perform an EKG (shown in figure A). Suddenly, his rhythm changes to ventricular tachycardia followed by ventricular fibrillation, and he syncopizes and expires despite resuscitative efforts. High levels of which medication are most likely responsible?
- A. Propranolol
- B. Amiodarone
- C. Lidocaine
- D. Verapamil
- E. Digoxin (Correct Answer)
Antiarrhythmic medications Explanation: ***Digoxin***
- The patient's presentation with **heart failure** symptoms (dyspnea, orthopnea, rales, S3 gallop, hepatomegaly) and erratic self-dosing of "some pills" strongly suggests **digoxin toxicity**.
- **Gastrointestinal symptoms** (nausea, vomiting, diarrhea) are common initial signs of digoxin toxicity, and the progression to **ventricular tachycardia** and **ventricular fibrillation** is consistent with severe digitalis-induced arrhythmia.
*Propranolol*
- This is a **beta-blocker** primarily used for hypertension, angina, and arrhythmias.
- While overdose can cause bradycardia, hypotension, and heart block, it typically does not lead to **ventricular tachycardia or fibrillation** as seen in this case.
*Amiodarone*
- This is a **Class III antiarrhythmic** medication with a long half-life, used for various tachyarrhythmias.
- Though it can cause many side effects, including proarrhythmia, it is less likely to present with the classic **GI symptoms** and rapid progression to fatal ventricular arrhythmias seen here, especially in the context of erratic self-dosing and underlying heart failure.
*Lidocaine*
- This is a **Class IB antiarrhythmic** primarily used for ventricular arrhythmias, especially post-myocardial infarction.
- Toxicity typically manifests as **neurological symptoms** (drowsiness, confusion, seizures) and sometimes hypotension or bradycardia, not the wide range of GI and lethal cardiac arrhythmias described.
*Verapamil*
- This is a **calcium channel blocker** used for hypertension, angina, and supraventricular tachycardias.
- Overdose primarily causes **bradycardia, hypotension, and atrioventricular block**, but it is generally not associated with the pronounced GI symptoms or directly triggering ventricular tachycardia/fibrillation like digoxin toxicity.
Antiarrhythmic medications US Medical PG Question 3: A 63-year-old man with a history of hypertension and atrial fibrillation is brought into the emergency room and found to have a ventricular tachyarrhythmia. Ibutilide is discontinued and the patient is switched to another drug that also prolongs the QT interval but is associated with a decreased risk of torsades de pointes. Which drug was most likely administered in this patient?
- A. Esmolol
- B. Digoxin
- C. Sotalol
- D. Amiodarone (Correct Answer)
- E. Quinidine
Antiarrhythmic medications Explanation: ***Amiodarone***
- **Amiodarone** prolongs the **QT interval** but has a lower risk of **torsades de pointes** compared to other **Class III antiarrhythmics** due to its mixed ion channel blocking properties and consistent action potential prolongation.
- It's a broad-spectrum **antiarrhythmic drug** effective for both **atrial** and **ventricular arrhythmias**, making it a good choice for someone with a history of **atrial fibrillation** presenting with **ventricular tachyarrhythmia**.
*Esmolol*
- **Esmolol** is a **beta-blocker** that does not prolong the **QT interval**; it is used to slow heart rate and can be used for rhythm control but not by **QT prolongation**.
- Its primary action is on **beta-1 receptors**, reducing **myocardial contractility** and **heart rate**, primarily used for acute control of **tachyarrhythmias** or **hypertensive emergencies**.
*Digoxin*
- **Digoxin** is a **cardiac glycoside** that does not prolong the **QT interval**; it primarily works by inhibiting the **Na+/K+-ATPase pump** and increasing **vagal tone**.
- It is used to control **ventricular rate** in **atrial fibrillation** and to manage **heart failure**, but it is not an **antiarrhythmic** in the sense of directly terminating **ventricular tachyarrhythmias** by affecting **QT prolongation**.
*Sotalol*
- **Sotalol** is a **beta-blocker** with **Class III antiarrhythmic properties** that prolongs the **QT interval** and has a significant **dose-related risk of torsades de pointes**, particularly at higher doses.
- While it's effective for both **ventricular** and **supraventricular arrhythmias**, its risk of **TdP** is a major concern, making **amiodarone** a safer alternative when **TdP risk** is to be minimized.
*Quinidine*
- **Quinidine** is a **Class IA antiarrhythmic** that significantly prolongs the **QT interval** and is known for a high risk of causing **torsades de pointes**.
- It primarily blocks **fast sodium channels** and also **potassium channels**, contributing to its **proarrhythmic effects** and making it a less favored option when **TdP risk** needs to be decreased.
Antiarrhythmic medications US Medical PG Question 4: A 65-year-old man with hypertension and paroxysmal atrial fibrillation presents to his cardiologist for follow-up after recently starting metoprolol for rate control. His EKG shows an atrial rate of 260/min with ventricular rate of 50/min on an irregular baseline. An echocardiogram from his previous visit revealed no evidence of hypokinesis or hypertrophy with functionally intact valves. The patient does not drink alcohol and had no evidence of liver dysfunction in prior studies. What is the best medication for rhythm control in this patient?
- A. Amiodarone
- B. Flecainide (Correct Answer)
- C. Procainamide
- D. Verapamil
- E. Mexiletine
Antiarrhythmic medications Explanation: ***Flecainide***
- **Flecainide** is a **Class IC antiarrhythmic** medication that is effective for rhythm control in patients with **paroxysmal atrial fibrillation** and no structural heart disease.
- The patient's echocardiogram showed no evidence of hypokinesis or hypertrophy, with functionally intact valves, indicating the **absence of structural heart disease**, which is a prerequisite for using Class IC agents like flecainide.
*Amiodarone*
- **Amiodarone** is a potent antiarrhythmic but is associated with numerous significant **extracardiac side effects**, including **pulmonary fibrosis**, **thyroid dysfunction**, and liver toxicity.
- It is generally reserved for patients with structural heart disease or those who have failed other antiarrhythmic therapies due to its extensive side effect profile.
*Procainamide*
- **Procainamide** is a **Class IA antiarrhythmic** that has a high incidence of side effects, including **drug-induced lupus**, and is typically used for acute management of arrhythmias, not long-term rhythm control in this setting.
- Its use is limited by its short half-life and significant proarrhythmic potential, especially in patients with structural heart disease or LV dysfunction.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** primarily used for **rate control** in atrial fibrillation, not rhythm control.
- The patient is already on metoprolol for rate control, and the question specifically asks for a medication for rhythm control.
*Mexiletine*
- **Mexiletine** is a **Class IB antiarrhythmic** agent primarily used for treating **ventricular arrhythmias**, particularly in the setting of myocardial infarction.
- It is not typically used for rhythm control in atrial fibrillation and has limited efficacy in this context.
Antiarrhythmic medications US Medical PG Question 5: A 62-year-old man is brought to the emergency department because of syncope. He reports sudden onset of palpitations followed by loss of consciousness while carrying his groceries to his car. He is unable to recall any further details and does not have any chest pain or dizziness. He has a history of hypertension, type 2 diabetes mellitus, gastroparesis, and osteoarthritis of the knees. Medications include lisinopril, metformin, and ondansetron as needed for nausea. He also takes methadone daily for chronic pain. Apart from an abrasion on his forehead, he appears well. His temperature is 37.2 °C (98.9 F), heart rate is 104/min and regular, and blood pressure is 135/70 mm Hg. While he is in the emergency department, he loses consciousness again. Telemetry shows polymorphic ventricular tachycardia with cyclic alteration of the QRS axis that spontaneously resolves after 30 seconds. Results of a complete blood count, serum electrolyte concentrations, and serum thyroid studies show no abnormalities. Cardiac enzymes are within normal limits. Which of the following is the most likely underlying cause of this patient's syncope?
- A. Prinzmetal angina
- B. Fast accessory conduction pathway
- C. Brugada syndrome
- D. Prolonged QT interval (Correct Answer)
- E. Hypomagnesemia
Antiarrhythmic medications Explanation: ***Prolonged QT interval***
- The patient experienced **polymorphic ventricular tachycardia** with cyclic alteration of the **QRS axis** (Torsades de Pointes), which is characteristic of a prolonged QT interval.
- **Methadone is known to prolong the QT interval**, and the patient's history of syncope preceded by palpitations is consistent with this arrhythmia.
*Prinzmetal angina*
- Prinzmetal angina involves **coronary artery spasm**, leading to **transient myocardial ischemia**, typically causing chest pain, not primarily syncope from polymorphic VT.
- While it can cause arrhythmias, the characteristic EKG finding would be **ST-segment elevation during pain**, which is not described.
*Fast accessory conduction pathway*
- A fast accessory pathway (e.g., in Wolfe-Parkinson-White syndrome) can lead to **AV reentrant tachycardia** or **pre-excitation** with atrial fibrillation, but not typically polymorphic VT with cyclic QRS alteration.
- The EKG would show a **delta wave** and a short PR interval, which is not mentioned.
*Brugada syndrome*
- Brugada syndrome is an inherited channelopathy **characterized by specific EKG patterns** (e.g., coved-type ST elevation in V1-V3) and an increased risk of sudden cardiac death due to ventricular arrhythmias.
- The patient's EKG findings of polymorphic VT with cyclic QRS alteration are not typical of Brugada syndrome-induced arrhythmia.
*Hypomagnesemia*
- While **hypomagnesemia can prolong the QT interval** and lead to Torsades de Pointes, the patient's **serum electrolyte concentrations were normal**, ruling out this direct cause.
- Magnesium levels would need to be critically low for such an effect, and this is typically detected on blood tests.
Antiarrhythmic medications US Medical PG Question 6: A 21-year-old woman presents with palpitations and anxiety. She had a recent outpatient ECG that was suggestive of supraventricular tachycardia, but her previous physician failed to find any underlying disease. No other significant past medical history. Her vital signs include blood pressure 102/65 mm Hg, pulse 120/min, respiratory rate 17/min, and temperature 36.5℃ (97.7℉). Electrophysiological studies reveal an atrioventricular nodal reentrant tachycardia. The patient refuses an ablation procedure so it is decided to perform synchronized cardioversion with consequent ongoing management with verapamil. Which of the following ECG features should be monitored in this patient during treatment?
- A. Amplitude and direction of the T wave
- B. Length of QRS complex
- C. Length of QT interval
- D. Length of PR interval (Correct Answer)
- E. QRS complex amplitude
Antiarrhythmic medications Explanation: ***Length of PR interval***
- Verapamil is a **non-dihydropyridine calcium channel blocker** that primarily acts on the **AV node** to slow conduction.
- Monitoring the **PR interval** is crucial because excessive slowing of AV nodal conduction can lead to **AV block**, which is indicated by a prolonged PR interval.
*Amplitude and direction of the T wave*
- Changes in T-wave amplitude and direction are often associated with **myocardial ischemia** or **electrolyte imbalances**, which are not the primary concerns with verapamil.
- While verapamil can affect repolarization, the most direct and common adverse effect related to its mechanism of action on the AV node is not primarily reflected in T-wave changes.
*Length of QRS complex*
- The QRS complex duration primarily reflects **ventricular depolarization** and is typically affected by medications that alter conduction through the His-Purkinje system or within the ventricles, such as antiarrhythmics like **flecainide** or **amiodarone**.
- Verapamil's main action is on the AV node, so it generally does not significantly prolong the QRS complex unless there is pre-existing conduction system disease.
*Length of QT interval*
- The QT interval represents **ventricular repolarization**, and its prolongation can lead to **Torsades de Pointes**, a life-threatening arrhythmia.
- While many antiarrhythmics can prolong the QT interval, **verapamil is not known to significantly prolong the QT interval** and is generally considered safe in this regard.
*QRS complex amplitude*
- Changes in QRS amplitude can indicate conditions like **pericardial effusion**, **cardiomyopathy**, or changes in ventricular mass.
- These are generally not direct or common side effects of verapamil therapy, which primarily focuses on AV nodal conduction.
Antiarrhythmic medications US Medical PG Question 7: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Antiarrhythmic medications Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
Antiarrhythmic medications US Medical PG Question 8: A 70-year-old man presents to the emergency department with severe substernal chest pain of one hour’s duration. The patient was taking a morning walk when the onset of pain led him to seek care. His past medical history includes coronary artery disease, hyperlipidemia, and hypertension. Medications include aspirin, losartan, and atorvastatin. An electrocardiogram reveals ST elevations in the inferior leads II, III, and avF as well as in leads V5 and V6. The ST elevations found in leads V5-V6 are most indicative of pathology in which of the following areas of the heart?
- A. Lateral wall of left ventricle, left circumflex coronary artery (Correct Answer)
- B. Left atrium, left main coronary artery
- C. Inferior wall, right coronary artery
- D. Interventricular septum, left anterior descending coronary artery
- E. Right ventricle, right coronary artery
Antiarrhythmic medications Explanation: ***Lateral wall of left ventricle, left circumflex coronary artery***
- **ST elevations in leads V5 and V6** are characteristic findings for an **anterolateral or high lateral myocardial infarction**.
- These leads correspond to the **lateral wall of the left ventricle**, which is primarily supplied by the **left circumflex coronary artery**.
*Left atrium, left main coronary artery*
- The **left atrium** is involved in atrial arrhythmias or hypertrophy, but **ST segment changes** on an ECG primarily reflect **ventricular ischemia or infarction**.
- While the **left main coronary artery** supplies a large portion of the left ventricle, its occlusion typically presents with more widespread and severe **ST elevations**, potentially affecting multiple lead groups beyond just V5-V6, and often indicates extensive damage.
*Inferior wall, right coronary artery*
- **Inferior wall infarctions** are indicated by **ST elevations in leads II, III, and aVF** (which are also present in this patient), primarily supplied by the **right coronary artery**.
- Although there is an inferior MI, the question specifically asks about the V5-V6 changes, which point to a distinct region.
*Interventricular septum, left anterior descending coronary artery*
- **ST elevations in V1-V4** are typically associated with an **anterior myocardial infarction**, affecting the **interventricular septum** and anterior wall, often due to occlusion of the **left anterior descending coronary artery**.
- The given leads V5-V6 do not primarily represent the interventricular septum.
*Right ventricle, right coronary artery*
- **Right ventricular infarction** is indicated by **ST elevations in lead V4R** (a right-sided lead) and can accompany inferior infarctions; however, V5-V6 do not specifically represent the right ventricle.
- The **right ventricle** is primarily supplied by the **right coronary artery**, not branches of the left coronary system, and RV infarction would require right-sided ECG leads for diagnosis.
Antiarrhythmic medications US Medical PG Question 9: A 48-year-old man presents to his primary care physician with diarrhea and weight loss. He states he has had diarrhea for the past several months that has been worsening steadily. The patient recently went on a camping trip and drank unfiltered stream water. Otherwise, the patient endorses a warm and flushed feeling in his face that occurs sporadically. His temperature is 97.2°F (36.2°C), blood pressure is 137/68 mmHg, pulse is 110/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for a murmur heard best over the left lower sternal border and bilateral wheezing on pulmonary exam. Which of the following is the best initial step in management?
- A. Pulmonary function tests
- B. Plasma free metanephrine levels
- C. Urinary 5-hydroxyindoleacetic acid level (Correct Answer)
- D. Echocardiography
- E. Stool culture and ova and parasite analysis
Antiarrhythmic medications Explanation: ***Urinary 5-hydroxyindoleacetic acid level***
- The combination of **diarrhea**, **weight loss**, episodic **flushing**, **wheezing**, and a **cardiac murmur** (suggesting right-sided valve involvement) is highly suggestive of **carcinoid syndrome**. The **urinary 5-HIAA** level is the most reliable initial biochemical test to diagnose this condition.
- Carcinoid tumors secrete **serotonin**, which is metabolized to 5-HIAA and excreted in the urine. Elevated levels confirm the diagnosis.
*Pulmonary function tests*
- While the patient has **wheezing**, which could be due to **bronchospasm** as part of carcinoid syndrome, pulmonary function tests are not the best initial diagnostic step.
- They would characterize the lung involvement but not identify the underlying cause of the systemic symptoms.
*Plasma free metanephrine levels*
- This test is used to diagnose **pheochromocytoma**, a condition that can also cause episodic flushing and palpitations.
- However, pheochromocytoma does not typically cause chronic diarrhea, weight loss, or the characteristic right-sided cardiac involvement seen in this patient.
*Echocardiography*
- An **echocardiogram** would be useful to evaluate the cardiac murmur and assess for **right-sided valvular heart disease**, which is a common manifestation of **carcinoid heart disease**.
- However, it is a follow-up imaging study to characterize complications, not the initial diagnostic test to confirm the biochemical syndrome.
*Stool culture and ova and parasite analysis*
- Given the history of drinking unfiltered stream water, **gastrointestinal infections** are a possibility for the diarrhea.
- However, the combination of **flushing**, **wheezing**, and a **cardiac murmur** points away from an infectious etiology as the primary cause of all symptoms.
Antiarrhythmic medications US Medical PG Question 10: A 74-year-old woman comes to the physician for a follow-up examination. Eight months ago, she underwent an emergency cardiac catheterization with stenting for myocardial infarction. At the time of discharge, her heart configuration was normal, end-diastolic volume was 300 mL and ejection fraction was 51%. For the past 8 weeks she has noticed increasing shortness of breath while playing with her 2-year-old grandson. She feels otherwise well. She has arterial hypertension, coronary artery disease, and hypercholesterolemia. She admits to rarely taking her medication as she usually feels well and has no symptoms. Her temperature is 37.3°C (99.1°F), pulse is 93/min, and blood pressure is 142/93 mm Hg. Examination shows no abnormalities. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. ECG shows broad, deep Q waves and T-wave inversion. Echocardiography shows left ventricular dilation and an end-diastolic volume of 370 mL; Ejection fraction is 40%. Which of the following is most likely to have prevented this patient's worsening of ventricular function?
- A. Nifedipine
- B. Atorvastatin
- C. Enalapril (Correct Answer)
- D. Diltiazem
- E. Digoxin
Antiarrhythmic medications Explanation: ***Enalapril***
- Enalapril, an **ACE inhibitor**, would prevent ventricular remodeling and worsening heart failure by blocking the **renin-angiotensin-aldosterone system (RAAS)**.
- RAAS activation after an MI leads to **ventricular hypertrophy** and dilation, which ACE inhibitors effectively counteract.
*Nifedipine*
- **Nifedipine is a dihydropyridine calcium channel blocker** primarily used for hypertension and angina.
- It does not have the same proven benefits in preventing ventricular remodeling or improving outcomes in **heart failure** as ACE inhibitors.
*Atorvastatin*
- **Atorvastatin is a HMG-CoA reductase inhibitor** that lowers cholesterol and stabilizes plaques.
- While essential for **secondary prevention of cardiovascular events**, it does not directly prevent ventricular remodeling or improve ejection fraction in the setting of heart failure.
*Diltiazem*
- **Diltiazem is a non-dihydropyridine calcium channel blocker** that reduces heart rate and contractility.
- It is generally **contraindicated** in patients with **reduced ejection fraction heart failure** as it can worsen cardiac function.
*Digoxin*
- **Digoxin is a positive inotrope** that can improve symptoms in heart failure but does not prevent ventricular remodeling or improve survival.
- It has a **narrow therapeutic window** and is primarily used for symptom control in advanced heart failure or for rate control in atrial fibrillation.
More Antiarrhythmic medications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.