Unstable angina US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Unstable angina. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
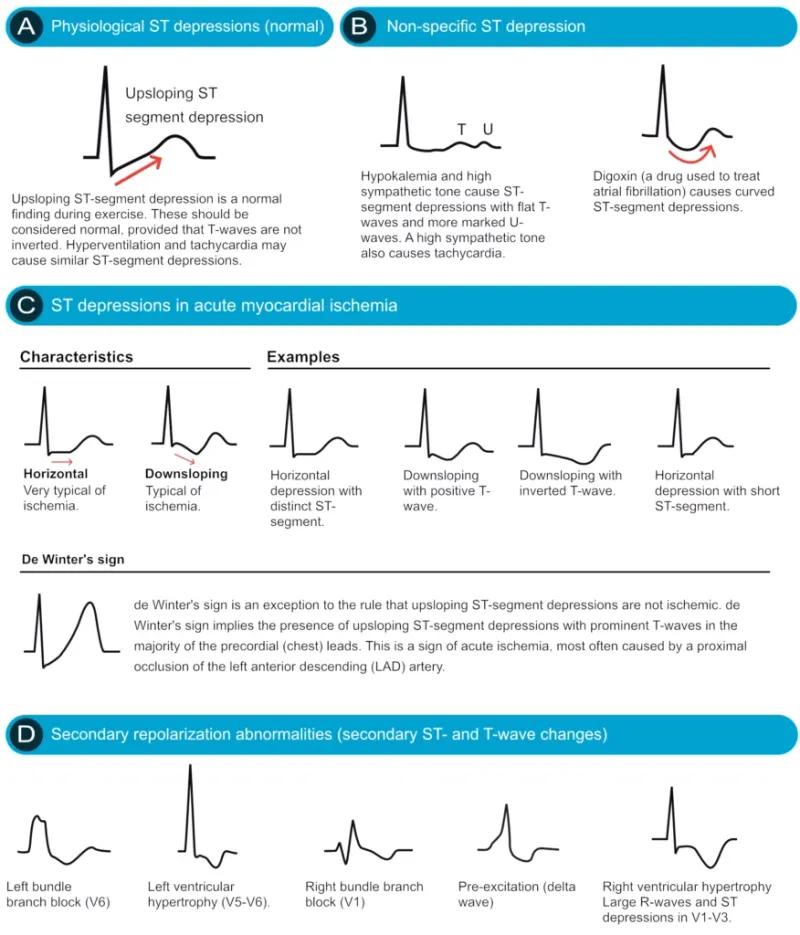
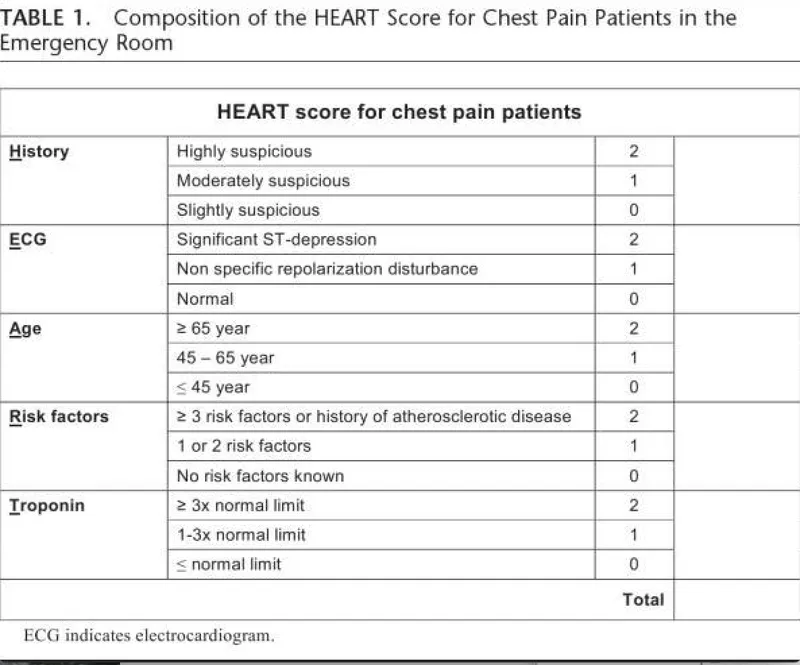
Unstable angina US Medical PG Question 1: A 60-year-old woman presents to the emergency room with chest pain that started 20 minutes ago while watching television at home. The pain is substernal and squeezing in nature. She rates the pain as 6/10 and admits to having similar pain in the past with exertion. Her past medical history is significant for diabetes mellitus that is controlled with metformin. The physical examination is unremarkable. An electrocardiogram (ECG) shows ST-segment depression in the lateral leads. She is started on aspirin, nitroglycerin, metoprolol, unfractionated heparin, and insulin. She is asked not to take metformin while at the hospital. Three sets of cardiac enzymes are negative.
Lab results are given below:
Serum glucose 88 mg/dL
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 1.2 mg/dL
Blood urea nitrogen 22 mg/dL
Cholesterol, total 170 mg/dL
HDL-cholesterol 40 mg/dL
LDL-cholesterol 80 mg/dL
Triglycerides 170 mg/dL
Hematocrit 38%
Hemoglobin 13 g/dL
Leucocyte count 7,500/mm3
Platelet count 185,000 /mm3
Activated partial thromboplastin time (aPTT) 30 seconds
Prothrombin time (PT) 12 seconds
Urinalysis
Glucose negative
Ketones negative
Leucocytes negative
Nitrites negative
Red blood cells (RBC) negative
Casts negative
An echocardiogram reveals left ventricular wall motion abnormalities. With the pain subsiding, she was admitted and the medications were continued. A coronary angiography is planned in 4 days. In addition to regular blood glucose testing, which of the following should be closely monitored in this patient?
- A. Activated partial thromboplastin time (aPTT) alone
- B. Prothrombin time alone
- C. aPTT and platelet count (Correct Answer)
- D. Platelet count alone
- E. Prothrombin time and platelet count
Unstable angina Explanation: ***aPTT and platelet count***
- The patient is receiving **unfractionated heparin**, which requires monitoring of **aPTT** to ensure therapeutic anticoagulation and prevent bleeding complications.
- Heparin can also induce **heparin-induced thrombocytopenia (HIT)**, necessitating close monitoring of the **platelet count**.
*Activated partial thromboplastin time (aPTT) alone*
- While **aPTT** monitoring is crucial for unfractionated heparin, it does not account for the risk of **heparin-induced thrombocytopenia (HIT)**.
- Monitoring platelet count is equally important alongside aPTT in patients receiving heparin.
*Prothrombin time alone*
- **Prothrombin time (PT)** is used to monitor **warfarin** therapy, not unfractionated heparin.
- Monitoring PT in this context would be inappropriate and would not provide information about the efficacy or safety of the prescribed heparin.
*Platelet count alone*
- Monitoring **platelet count** is important for detecting **heparin-induced thrombocytopenia (HIT)**, but it does not assess the therapeutic effect of heparin.
- **aPTT** monitoring is essential to ensure adequate anticoagulation and prevent thrombotic events.
*Prothrombin time and platelet count*
- **Prothrombin time (PT)** is irrelevant for unfractionated heparin monitoring, as it measures the extrinsic pathway and is used for warfarin.
- Although **platelet count** monitoring is important, relying on PT is incorrect for unfractionated heparin management.
Unstable angina US Medical PG Question 2: A 59-year-old man with angina pectoris comes to the physician because of a 6-month history of shortness of breath on exertion that improves with rest. He has hypertension and hyperlipidemia. Current medications include aspirin, metoprolol, and nitroglycerine. Echocardiography shows left ventricular septal and apical hypokinesis. Cardiac catheterization shows 96% occlusion of the left anterior descending artery. The patient undergoes angioplasty and placement of a stent. The patient's shortness of breath subsequently resolves and follow-up echocardiography one week later shows normal regional contractile function. Which of the following is the most accurate explanation for the changes in echocardiography?
- A. Myocardial scarring
- B. Unstable angina pectoris
- C. Stress cardiomyopathy
- D. Hibernating myocardium (Correct Answer)
- E. Cardiac remodeling
Unstable angina Explanation: ***Hibernating myocardium***
- This refers to chronically **ischemic but viable myocardium** that shows reduced contractility at rest due to persistent hypoperfusion, which improves or normalizes after revascularization.
- The resolution of symptoms and normalization of regional contractile function after stent placement in this patient with chronic angina and a highly occluded LAD artery is highly consistent with this phenomenon.
*Myocardial scarring*
- **Myocardial scarring** represents irreversible damage and fibrosis, typically resulting from a myocardial infarction (heart attack).
- Scarred tissue does not regain contractile function even after revascularization; the observed improvement in contractility rules out this explanation.
*Unstable angina pectoris*
- **Unstable angina** is characterized by new-onset angina, crescendo angina, or angina at rest, indicating an acute coronary syndrome.
- While the patient had angina, the prompt and complete resolution of contractile dysfunction post-revascularization points to a chronic ischemic state rather than an acute, potentially irreversible event or a transient episode of unstable angina that would not cause such persistent functional changes.
*Stress cardiomyopathy*
- Also known as **Takotsubo cardiomyopathy**, this condition involves transient left ventricular dysfunction, often triggered by severe emotional or physical stress, mimicking a myocardial infarction.
- It typically resolves spontaneously over weeks or months and is not caused by fixed coronary artery occlusion that improves with revascularization via stenting.
*Cardiac remodeling*
- **Cardiac remodeling** refers to changes in the size, shape, and function of the heart in response to chronic stress, such as hypertension or chronic ischemia.
- While the patient's long-standing hypertension and hyperlipidemia could lead to some remodeling, the rapid and complete improvement in regional contractility specifically after LAD revascularization best explains the phenomenon as hibernating myocardium, a specific type of physiological adaptation, rather than general remodeling.
Unstable angina US Medical PG Question 3: A 70-year-old woman presents with substernal chest pain. She says that the symptoms began 2 hours ago and have not improved. She describes the pain as severe, episodic, and worse with exertion. She reports that she has had multiple similar episodes that have worsened and increased in frequency over the previous 4 months. Past medical history is significant for diabetes and hypertension, both managed medically. The vital signs include temperature 37.0°C (98.6°F), blood pressure 150/100 mm Hg, pulse 80/min, and respiratory rate 15/min. Her serum total cholesterol is 280 mg/dL and high-density lipoprotein (HDL) is 30 mg/dL. The electrocardiogram (ECG) shows ST-segment depression on multiple chest leads. Coronary angiography reveals 75% narrowing of her left main coronary artery. In which of the following anatomical locations is a mural thrombus most likely to form in this patient?
- A. Left ventricle (Correct Answer)
- B. Left atrium
- C. Aorta
- D. Right atrium
- E. Right ventricle
Unstable angina Explanation: ***Left ventricle***
- The patient presents with symptoms and ECG findings consistent with **unstable angina** or **non-ST elevation myocardial infarction (NSTEMI)**, indicating myocardial ischemia.
- With **75% left main coronary artery stenosis**, there is high risk of progression to **transmural myocardial infarction (STEMI)**, particularly affecting the anterior wall and septum.
- Mural thrombi in the left ventricle typically form **3-7 days post-infarction** in areas of **dyskinetic or akinetic myocardium** due to blood stasis, endocardial injury, and hypercoagulability (Virchow's triad).
- Left main disease affecting such a large territory makes the **left ventricle the most likely site** for mural thrombus formation.
*Left atrium*
- Mural thrombi in the left atrium are most commonly associated with **atrial fibrillation** due to blood stasis in the **left atrial appendage**.
- This patient's symptoms are characteristic of coronary artery disease affecting the left ventricle, not an atrial arrhythmia.
*Aorta*
- While thrombi can form in the aorta (e.g., in the setting of **atherosclerosis** or **aneurysms**), they are typically mural thrombi associated with specific vascular pathologies.
- The symptoms of **chest pain, ST depression**, and **coronary artery narrowing** point toward a myocardial event, making the left ventricle the most likely site for mural thrombus in this clinical context.
*Right atrium*
- Thrombi in the right atrium are usually associated with conditions leading to **venous stasis, such as deep vein thrombosis**, **central venous catheters**, or **right-sided heart failure**.
- The patient's presentation with exertional chest pain and left main coronary artery narrowing is unrelated to right atrial thrombosis.
*Right ventricle*
- The right ventricle is **much less commonly** affected by ischemic events leading to mural thrombi compared to the left ventricle, due to its **lower oxygen demand** and **different blood supply** (right coronary artery).
- While right ventricular infarction can occur (usually with inferior MI), the **left main coronary artery** supplies the left ventricle, making it the primary concern for mural thrombus formation in this patient.
Unstable angina US Medical PG Question 4: A 47-year-old man presents as a new patient at an outpatient clinic. He has never seen a physician before, but was motivated by his 40-year-old brother's recent heart attack and seeks to optimize his health. In particular, he read that uncontrolled atherosclerosis can lead to a heart attack. Which molecule is downregulated in response to the advent of atherosclerosis?
- A. Tumor necrosis factor
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Interleukin 1
- E. Thromboxane A2
Unstable angina Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is a potent **vasodilator** and **anti-inflammatory** molecule produced by endothelial cells. In atherosclerosis, endothelial dysfunction leads to reduced NO bioavailability.
- Decreased NO production contributes to vasoconstriction, increased platelet aggregation, and enhanced smooth muscle cell proliferation, all of which promote **atherosclerotic plaque formation** and progression.
*Tumor necrosis factor*
- **Tumor necrosis factor-alpha (TNF-α)** is a **pro-inflammatory cytokine** that plays a significant role in the pathogenesis of atherosclerosis.
- It is **upregulated** in response to atherosclerotic plaque formation, contributing to endothelial activation, leukocyte recruitment, and smooth muscle cell proliferation.
*Serotonin*
- **Serotonin (5-hydroxytryptamine)** is primarily known for its role as a neurotransmitter but also acts as a **vasoconstrictor** and promotes platelet aggregation.
- While it can be released from activated platelets in the context of vascular injury, it is not consistently **downregulated** in atherosclerosis; rather, its effects can contribute to disease progression.
*Interleukin 1*
- **Interleukin-1 (IL-1)**, particularly IL-1β, is a major **pro-inflammatory cytokine** critically involved in the immune response in atherosclerosis.
- It is **upregulated** in atherosclerotic plaques, contributing to systemic inflammation, endothelial dysfunction, and vascular smooth muscle cell activation.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is a potent **vasoconstrictor** and **platelet aggregator** produced by activated platelets.
- Its levels are **increased** in atherosclerosis, contributing to hypercoagulability and increased risk of thrombotic events like myocardial infarction.
Unstable angina US Medical PG Question 5: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
Unstable angina Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
Unstable angina US Medical PG Question 6: A 73-year-old man presents to the outpatient clinic complaining of chest pain with exertion. He states that resting for a few minutes usually resolves the chest pain. Currently, he takes 81 mg of aspirin daily. He has a blood pressure of 127/85 mm Hg and heart rate of 75/min. Physical examination reveals regular heart sounds and clear lung sounds bilateral. Which medication regimen below should be added?
- A. Metoprolol and a statin daily. Sublingual nitroglycerin as needed. (Correct Answer)
- B. Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.
- C. Amlodipine and a statin daily. Sublingual nitroglycerin as needed.
- D. Amlodipine daily. Sublingual nitroglycerin as needed.
- E. Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.
Unstable angina Explanation: ***Metoprolol and a statin daily. Sublingual nitroglycerin as needed.***
- This patient presents with symptoms consistent with **stable angina** (**chest pain with exertion, relieved by rest**). The recommended medical therapy includes **antiplatelet agents** (aspirin, already prescribed), **beta-blockers** (metoprolol) for symptom control and improved survival post-MI, and **high-intensity statins** for lipid management and plaque stabilization. **Sublingual nitroglycerin** is crucial for acute symptom relief.
- Beta-blockers like metoprolol decrease myocardial **oxygen demand** by reducing heart rate and contractility, effectively treating angina. Statins are essential for **atherosclerosis management**.
*Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.*
- While clopidogrel is an **antiplatelet agent**, aspirin is typically the first-line choice for stable angina unless there's an intolerance or compelling reason for dual antiplatelet therapy (e.g., recent stent placement), which is not indicated here.
- Amlodipine, a **calcium channel blocker**, can be used for angina but is usually a second-line agent if beta-blockers are contraindicated or insufficient; it doesn't offer the mortality benefit seen with beta-blockers post-MI.
*Amlodipine and a statin daily. Sublingual nitroglycerin as needed.*
- This regimen includes a **statin** and sublingual nitroglycerin, which are appropriate. However, it uses amlodipine instead of a beta-blocker, which is generally the preferred initial therapy for angina due to its benefits in reducing myocardial oxygen demand and improving outcomes, especially in patients with a history of MI or heart failure.
- Beta-blockers provide superior **mortality reduction benefits** in patients with coronary artery disease compared to calcium channel blockers.
*Amlodipine daily. Sublingual nitroglycerin as needed.*
- This option misses two critical components of comprehensive treatment for stable angina: a **statin** for lipid management and plaque stabilization, and a **beta-blocker** for primary symptom control and long-term cardiac protection.
- Relying solely on amlodipine and sublingual nitroglycerin would leave the patient incompletely treated for their underlying **coronary artery disease**.
*Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.*
- This option lacks a **statin**, which is a cornerstone of therapy for stable angina to manage atherosclerosis.
- While metoprolol is appropriate and ranolazine can be used as an add-on therapy for refractory angina, it's not typically a first-line agent and doesn't replace the need for a statin.
Unstable angina US Medical PG Question 7: A 58-year-old man presents to the emergency department with severe chest pain and uneasiness. He says that symptoms onset acutely half an hour ago while he was watching television. He describes the pain as being 8/10 in intensity, sharp in character, localized to the center of the chest and retrosternal, and radiating to the back and shoulders. The patient denies any associated change in the pain with breathing or body position. He says he has associated nausea but denies any vomiting. He denies any recent history of fever, chills, or chronic cough. His past medical history is significant for hypertension, hyperlipidemia, and diabetes mellitus for which he takes lisinopril, hydrochlorothiazide, simvastatin, and metformin. He reports a 30-pack-year smoking history and has 1–2 alcoholic drinks during the weekend. Family history is significant for hypertension, hyperlipidemia, and an ST elevation myocardial infarction in his father and paternal uncle. His blood pressure is 220/110 mm Hg in the right arm and 180/100 mm Hg in the left arm. On physical examination, the patient is diaphoretic. Cardiac exam reveals a grade 2/6 diastolic decrescendo murmur loudest over the left sternal border. Remainder of the physical examination is normal. The chest radiograph shows a widened mediastinum. The electrocardiogram (ECG) reveals non-specific ST segment and T wave changes. Intravenous morphine and beta-blockers are started. Which of the following is the most likely diagnosis in this patient?
- A. Pulmonary embolism
- B. Acute myocardial infarction
- C. Myocarditis
- D. Aortic regurgitation
- E. Aortic dissection (Correct Answer)
Unstable angina Explanation: ***Aortic dissection***
- The patient's **sudden onset, sharp tearing chest pain radiating to the back** is the classic presentation of aortic dissection.
- The **blood pressure differential between arms** (220/110 mm Hg right vs 180/100 mm Hg left) is a highly specific finding indicating involvement of the brachiocephalic or subclavian arteries.
- The **diastolic decrescendo murmur** represents acute aortic regurgitation secondary to the dissection involving the aortic root.
- The **widened mediastinum on chest X-ray** is a key radiographic finding strongly suggestive of aortic dissection.
- Major risk factors present: **uncontrolled hypertension, smoking history, age, and atherosclerotic disease** (hyperlipidemia, diabetes).
*Pulmonary embolism*
- While PE can cause acute chest pain and dyspnea, the pain is typically **pleuritic in nature** (worsens with breathing or coughing).
- PE does not cause **blood pressure differentials between arms** or a **widened mediastinum**.
- The sharp, tearing quality radiating to the back is not characteristic of PE.
*Acute myocardial infarction*
- MI typically presents with **pressure-like or crushing chest pain**, often radiating to the left arm, jaw, or epigastrium rather than the back.
- While the patient has significant MI risk factors, the **unequal blood pressures between arms** and **diastolic murmur** are not explained by isolated MI.
- The **widened mediastinum** is not a feature of uncomplicated MI.
*Myocarditis*
- Myocarditis typically presents with **chest pain following a viral prodrome** (fever, URI symptoms), which this patient denies.
- It does not cause **blood pressure differentials**, **widened mediastinum**, or the acute tearing pain radiating to the back.
- Myocarditis pain is usually more constant and pressure-like, not sharp and tearing.
*Aortic regurgitation*
- While the **diastolic decrescendo murmur** indicates aortic regurgitation, this is a **finding rather than the primary diagnosis**.
- In this acute presentation, the AR is **secondary to aortic dissection** involving the aortic root.
- Chronic AR is typically asymptomatic until heart failure develops; acute severe AR (as in dissection) causes acute decompensation.
- The constellation of findings (acute pain, BP differential, widened mediastinum) indicates **aortic dissection as the primary catastrophic event** causing secondary AR.
Unstable angina US Medical PG Question 8: A 60-year-old man presents to the emergency department with progressive dyspnea for the last 3 weeks. He complains of shortness of breath while lying flat and reports nighttime awakenings due to shortness of breath for the same duration. The patient has been a smoker for the last 30 years. Past medical history is significant for myocardial infarction 7 months ago. Current medications include metoprolol, aspirin, and rosuvastatin, but the patient is noncompliant with his medications. His temperature is 37.2°C (98.9°F), the blood pressure is 150/115 mm Hg, the pulse is 110/min, and the respiratory rate is 24/min. Oxygen saturation on room air is 88%. Chest auscultation reveals bilateral crackles and an S3 gallop. On physical examination, the cardiac apex is palpated in left 6th intercostal space. Bilateral pitting edema is present, and the patient is in moderate distress. Which of the following is the best next step in the management of the patient?
- A. Intravenous beta blockers
- B. Intravenous diuretics (Correct Answer)
- C. Echocardiography
- D. Cardiac stress testing
- E. Intravenous inotropes
Unstable angina Explanation: ***Intravenous diuretics***
- The patient presents with classic signs and symptoms of **acute decompensated heart failure**, such as progressive dyspnea, orthopnea, paroxysmal nocturnal dyspnea, bilateral crackles, S3 gallop, pitting edema, and elevated blood pressure with elevated heart rate due to fluid overload.
- **Intravenous loop diuretics** (e.g., furosemide) are the most appropriate initial therapy to reduce preload, alleviate pulmonary and systemic congestion, and improve oxygenation.
*Intravenous beta blockers*
- While beta-blockers are a cornerstone of chronic heart failure management, **starting or acutely increasing beta-blocker dosage in acute decompensated heart failure** can worsen cardiac output and lead to symptomatic hypotension or cardiogenic shock.
- Beta-blockers should generally be withheld or reduced during acute exacerbations and reinstituted once the patient is stable.
*Echocardiography*
- While an **echocardiogram** is essential for diagnosing the underlying cause and assessing cardiac function in heart failure, it is not the *best next step* in a patient presenting with acute, severe symptoms requiring immediate stabilization.
- The patient's acute respiratory distress and hypoxemia necessitate immediate medical intervention to reduce fluid overload before detailed diagnostic imaging.
*Cardiac stress testing*
- **Cardiac stress testing** is used to evaluate for inducible ischemia in stable patients and is not appropriate in the setting of acute decompensated heart failure.
- Performing a stress test on a patient with signs of fluid overload and respiratory distress would be dangerous and could exacerbate their condition.
*Intravenous inotropes*
- **Intravenous inotropes** (e.g., dobutamine, milrinone) are typically reserved for patients with evidence of **cardiogenic shock** or severe heart failure with persistent hypoperfusion despite optimal fluid management and diuretic therapy.
- This patient, while acutely ill, primarily exhibits signs of fluid overload without clear evidence of severe hypoperfusion compromising end-organ function.
Unstable angina US Medical PG Question 9: A 72-year-old female presents to the emergency department following a syncopal episode while walking down several flights of stairs. The patient has not seen a doctor in several years and does not take any medications. Your work-up demonstrates that she has symptoms of angina and congestive heart failure. Temperature is 36.8 degrees Celsius, blood pressure is 160/80 mmHg, heart rate is 81/min, and respiratory rate is 20/min. Physical examination is notable for a 3/6 crescendo-decrescendo systolic murmur present at the right upper sternal border with radiation to the carotid arteries. Random blood glucose is 205 mg/dL. Which of the following portends the worst prognosis in this patient?
- A. Hypertension
- B. Angina
- C. Diabetes
- D. Syncope
- E. Congestive heart failure (CHF) (Correct Answer)
Unstable angina Explanation: ***Congestive heart failure (CHF)***
- Once **congestive heart failure** symptoms develop in severe aortic stenosis, the prognosis is very poor, with an average survival of 1.5-2 years if untreated.
- This indicates significant myocardial dysfunction and increased risk of sudden cardiac death.
*Syncope*
- **Syncope** in aortic stenosis, while serious and indicating reduced cerebral perfusion, has a slightly better prognosis than CHF, with an average survival of 2-3 years untreated.
- It often reflects a critical reduction in cardiac output, but the heart muscle itself may still have some compensatory capacity.
*Angina*
- **Angina** is a common symptom of aortic stenosis, reflecting increased myocardial oxygen demand or reduced coronary perfusion.
- Untreated, patients with angina in aortic stenosis have an average survival of 3-5 years, which is better than syncope or CHF.
*Hypertension*
- While **hypertension** is a risk factor for aortic stenosis and can exacerbate symptoms, it is not a direct symptom of severe aortic stenosis itself but rather a co-morbidity.
- Its presence doesn't inherently portend a worse prognosis for aortic stenosis than the severe symptomatic manifestations like syncope or CHF.
*Diabetes*
- **Diabetes** is a systemic disease that can accelerate atherosclerosis and increase cardiovascular risk, but it is a chronic condition rather than an acute symptom of severe aortic stenosis.
- While it complicates management and overall prognosis, its impact is not as immediate or as severe as the development of CHF directly attributable to the aortic stenosis itself.
Unstable angina US Medical PG Question 10: A 57-year-old man presents to his primary care provider because of chest pain for the past 3 weeks. The chest pain occurs after climbing more than 2 flight of stairs or walking for more than 10 minutes and resolves with rest. He is obese, has a history of type 2 diabetes mellitus, and has smoked 15-20 cigarettes a day for the past 25 years. His father died from a myocardial infarction at 52 years of age. Vital signs reveal a temperature of 36.7 °C (98.06°F), a blood pressure of 145/93 mm Hg, and a heart rate of 85/min. The physical examination is unremarkable. Which of the following best represents the most likely etiology of the patient’s condition?
- A. Hypertrophy of the interventricular septum
- B. Multivessel atherosclerotic disease with or without a nonocclusive thrombus
- C. Intermittent coronary vasospasm with or without coronary atherosclerosis
- D. Fixed, atherosclerotic coronary stenosis (> 70%) (Correct Answer)
- E. Sudden disruption of an atheromatous plaque, with a resulting occlusive thrombus
Unstable angina Explanation: ***Fixed, atherosclerotic coronary stenosis (> 70%)***
- The patient's presentation with **exertional chest pain** that resolves with rest (stable angina), along with multiple **cardiovascular risk factors** (obesity, type 2 diabetes mellitus, smoking, family history of early MI, hypertension), strongly points towards **stable ischemic heart disease**.
- This clinical picture is typically caused by a **fixed, hemodynamically significant stenosis** in one or more coronary arteries, usually greater than 70%, that limits blood flow during increased demand.
*Multivessel atherosclerotic disease with or without a nonocclusive thrombus*
- While the patient likely has **multivessel atherosclerosis**, the phrase "with or without a nonocclusive thrombus" leans towards **unstable angina** or NSTEMI, which typically involves a sudden change in symptoms or rest angina.
- The patient's symptoms are **stable and reproducible** with exertion, resolving with rest, which is characteristic of stable angina rather than a thrombotic event.
*Sudden disruption of an atheromatous plaque, with a resulting occlusive thrombus*
- This mechanism describes an **acute coronary syndrome (ACS)**, such as an **ST-elevation myocardial infarction (STEMI)** or **non-ST-elevation myocardial infarction (NSTEMI)**.
- ACS typically presents with new-onset, worsening, or rest angina, which is different from the stable, exertional pattern described in the patient.
*Intermittent coronary vasospasm with or without coronary atherosclerosis*
- **Coronary vasospasm** (e.g., Prinzmetal angina) typically causes chest pain that occurs **at rest**, often at night or in the early morning, and is not necessarily related to exertion.
- While the patient could have underlying atherosclerosis, the **predictable exertional nature** of his symptoms makes vasospasm less likely as the primary etiology.
*Hypertrophy of the interventricular septum*
- **Interventricular septal hypertrophy** is characteristic of **hypertrophic cardiomyopathy (HCM)**, which can cause exertional chest pain due to outflow tract obstruction or myocardial ischemia.
- However, HCM is less likely to be the primary etiology in a 57-year-old with multiple classic **atherosclerotic risk factors** and no mention of a heart murmur or family history of HCM.
More Unstable angina US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.