STEMI diagnosis and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for STEMI diagnosis and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
STEMI diagnosis and management US Medical PG Question 1: A 28-year-old male presents with sharp, stabbing chest pain that worsens when lying flat and improves when sitting forward. He reports a recent viral upper respiratory infection 2 weeks ago. On examination, a friction rub is heard on auscultation. His vital signs are stable.
An ECG is most likely to show which of the following findings in this patient?
- A. Diffuse, concave ST-segment elevations (Correct Answer)
- B. Peaked T waves and ST-segment elevations in leads V1-V6
- C. Sawtooth-appearance of P waves
- D. S waves in lead I, Q waves in lead III, and inverted T waves in lead III
- E. Alternating high and low amplitude QRS complexes
STEMI diagnosis and management Explanation: ***Diffuse, concave ST-segment elevations***
- This is a hallmark ECG finding in **acute pericarditis**, along with **PR segment depression**, due to widespread inflammation of the epicardium.
- The chest pain described here (sharp, stabbing, worse when lying flat, improved by sitting forward) paired with a recent viral infection and a pericardial friction rub, is highly characteristic of **pericarditis**.
*Peaked T waves and ST-segment elevations in leads V1-V6*
- **Peaked T waves** are typically seen in early stages of hyperkalemia or myocardial ischemia, while **ST-segment elevations in specific leads (V1-V6)** are more indicative of an **ST-elevation myocardial infarction (STEMI)** involving the anterior wall.
- The diffuse nature of ST elevation in pericarditis, as opposed to regional changes, along with **PR depression**, differentiates it from STEMI.
*Sawtooth-appearance of P waves*
- A **sawtooth appearance of P waves** (often referred to as 'f waves') is characteristic of **atrial flutter**, a type of supraventricular tachycardia.
- This finding is unrelated to pericarditis, which primarily affects the pericardium and not the atrial electrical activity in this specific manner.
*S waves in lead I, Q waves in lead III, and inverted T waves in lead III*
- This pattern, known as the **S1Q3T3 pattern**, is a classic (though not always present) ECG finding suggestive of **acute pulmonary embolism**.
- While pulmonary embolism can cause chest pain, its presentation differs significantly from the positional relief and friction rub seen in pericarditis.
*Alternating high and low amplitude QRS complexes*
- This ECG finding, known as **electrical alternans**, is highly specific for a large **pericardial effusion** or **cardiac tamponade**, where the heart swings within the fluid-filled pericardial sac.
- Although pericarditis can lead to effusion, the presence of a friction rub and stable vital signs suggests acute pericarditis without significant tamponade at this stage, making diffuse ST elevation a more likely initial finding.
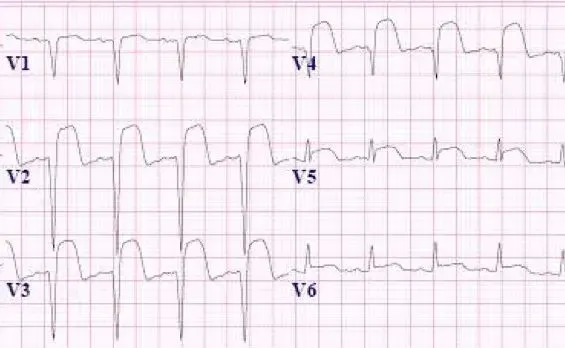
STEMI diagnosis and management US Medical PG Question 2: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
STEMI diagnosis and management Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
STEMI diagnosis and management US Medical PG Question 3: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
STEMI diagnosis and management Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
STEMI diagnosis and management US Medical PG Question 4: A 54-year-old man is brought to the emergency department 1 hour after the sudden onset of shortness of breath, severe chest pain, and sweating. He has hypertension and type 2 diabetes mellitus. He has smoked one pack and a half of cigarettes daily for 20 years. An ECG shows ST-segment elevations in leads II, III, and avF. The next hospital with a cardiac catheterization unit is more than 2 hours away. Reperfusion pharmacotherapy is initiated. Which of the following is the primary mechanism of action of this medication?
- A. Conversion of plasminogen to plasmin (Correct Answer)
- B. Inhibition of glutamic acid residue carboxylation
- C. Blocking of adenosine diphosphate receptors
- D. Direct inhibition of thrombin activity
- E. Prevention of thromboxane formation
STEMI diagnosis and management Explanation: ***Conversion of plasminogen to plasmin***
- **Fibrinolytic** (thrombolytic) drugs, like **tissue plasminogen activator (tPA)**, work by converting plasminogen to plasmin, which then degrades the **fibrin mesh** of a **blood clot**.
- This action helps to **restore blood flow** in cases of ST-segment elevation myocardial infarction (STEMI) where primary **percutaneous coronary intervention (PCI)** is not immediately available.
*Inhibition of glutamic acid residue carboxylation*
- This is the mechanism of action of **warfarin**, an anticoagulant that inhibits the synthesis of **vitamin K-dependent clotting factors** (II, VII, IX, X, protein C, and protein S).
- While important for long-term anticoagulation, it does not provide immediate reperfusion in an acute STEMI.
*Blocking of adenosine diphosphate receptors*
- This describes the mechanism of action of **P2Y12 inhibitors** such as **clopidogrel**, **prasugrel**, and **ticagrelor**.
- These drugs are **antiplatelet agents** that prevent platelet aggregation, but they do not directly dissolve an existing thrombus to restore blood flow in STEMI.
*Direct inhibition of thrombin activity*
- This is the mechanism of action of **direct thrombin inhibitors** like **dabigatran** and **bivalirudin**.
- These drugs primarily prevent clot formation or extension and are not used as primary reperfusion agents for acute STEMI due to an existing occlusive thrombus.
*Prevention of thromboxane formation*
- This is the primary mechanism of action of **aspirin**, which irreversibly inhibits **cyclooxygenase-1 (COX-1)**, thereby reducing the production of thromboxane A2.
- Aspirin is an important antiplatelet drug in STEMI management but does not provide reperfusion by dissolving the clot.
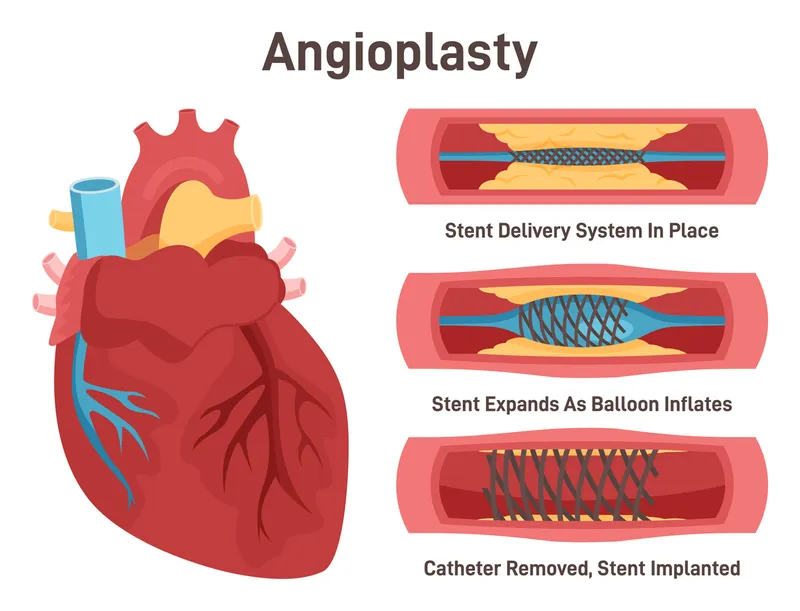
STEMI diagnosis and management US Medical PG Question 5: A 66-year-old female with hypertension and a recent history of acute ST-elevation myocardial infarction (STEMI) 6 days previous, treated with percutaneous transluminal angioplasty (PTA), presents with sudden onset chest pain, shortness of breath, diaphoresis, and syncope. Vitals are temperature 37°C (98.6°F), blood pressure 80/50 mm Hg, pulse 125/min, respirations 12/min, and oxygen saturation 92% on room air. On physical examination, the patient is pale and unresponsive. Cardiac exam reveals tachycardia and a pronounced holosystolic murmur loudest at the apex and radiates to the back. Lungs are clear to auscultation. Chest X-ray shows cardiomegaly with clear lung fields. ECG is significant for ST elevations in the precordial leads (V2-V4) and low-voltage QRS complexes. Emergency transthoracic echocardiography shows a left ventricular wall motion abnormality along with a significant pericardial effusion. The patient is intubated, and aggressive fluid resuscitation is initiated. What is the next best step in management?
- A. Immediate cardiac catheterization
- B. Immediate transfer to the operating room (Correct Answer)
- C. Emergency pericardiocentesis
- D. Intra-aortic balloon counterpulsation
- E. Administer dobutamine 5-10 mcg/kg/min IV
STEMI diagnosis and management Explanation: ***Immediate transfer to the operating room***
- The patient's presentation with sudden onset chest pain, shortness of breath, profound cardiogenic shock, and a new **holosystolic murmur at the apex radiating to the back** in the context of a recent **STEMI**, strongly suggests **acute papillary muscle rupture** causing severe mitral regurgitation. This is a surgical emergency requiring immediate intervention.
- The holosystolic murmur at the apex is pathognomonic for acute mitral regurgitation, distinguishing this from ventricular free wall rupture (which would present with tamponade physiology without a murmur).
- The patient requires urgent surgical repair (mitral valve replacement or repair) to address this mechanical complication of **myocardial infarction (MI)**, which is causing severe hemodynamic compromise.
*Immediate cardiac catheterization*
- While cardiac catheterization is essential for diagnosing coronary artery disease and revascularization, in this emergent situation with profound shock and a mechanical complication (papillary muscle rupture), the primary issue is structural cardiac damage requiring surgical repair, not ongoing ischemia alone.
- Delaying surgical intervention for catheterization in this hemodynamically unstable patient would be detrimental and potentially fatal.
*Emergency pericardiocentesis*
- Although there is a **pericardial effusion** on echocardiography, the patient's presentation with a new holosystolic murmur and profound shock after STEMI indicates **papillary muscle rupture with acute mitral regurgitation**, not cardiac tamponade.
- The presence of a loud murmur excludes ventricular free wall rupture as the primary cause. The effusion is likely reactive or incidental.
- Pericardiocentesis would not address the underlying mitral valve pathology causing the hemodynamic collapse.
*Intra-aortic balloon counterpulsation*
- **Intra-aortic balloon pump (IABP)** can improve cardiac output and reduce afterload, which may provide temporary hemodynamic support in cardiogenic shock.
- However, in cases of **papillary muscle rupture** with severe acute mitral regurgitation, IABP provides only temporary support and does not fix the underlying structural problem.
- It could be considered as a bridge to surgery, but the definitive treatment is surgical repair, which should be expedited without delay.
*Administer dobutamine 5-10 mcg/kg/min IV*
- **Dobutamine** is an inotrope that increases cardiac contractility. While it might improve cardiac output in some forms of cardiogenic shock, in the setting of **acute severe mitral regurgitation from papillary muscle rupture**, it cannot resolve the structural valvular incompetence.
- Increasing contractility may paradoxically worsen the regurgitant fraction and further compromise forward cardiac output.
- Medical management alone cannot resolve this mechanical complication, necessitating urgent surgical intervention.
STEMI diagnosis and management US Medical PG Question 6: A 52-year-old woman presents to the emergency room complaining of chest pain. She reports a 4-hour history of dull substernal pain radiating to her jaw. Her history is notable for hypertension, diabetes mellitus, and alcohol abuse. She has a 30 pack-year smoking history and takes lisinopril and metformin but has an allergy to aspirin. Her temperature is 99.1°F (37.3°C), blood pressure is 150/90 mmHg, pulse is 120/min, and respirations are 22/min. Physical examination reveals a diaphoretic and distressed woman. An electrocardiogram reveals ST elevations in leads I, aVL, and V5-6. She is admitted with plans for immediate transport to the catheterization lab for stent placement. What is the mechanism of the next medication that should be given to this patient?
- A. Cyclooxygenase activator
- B. ADP receptor inhibitor (Correct Answer)
- C. Phosphodiesterase activator
- D. Thrombin inhibitor
- E. Vitamin K epoxide reductase inhibitor
STEMI diagnosis and management Explanation: ***ADP receptor inhibitor***
- This patient is experiencing an **ST-elevation myocardial infarction (STEMI)** as evidenced by ST elevations in leads I, aVL, and V5-6 (lateral wall infarction)
- **Dual antiplatelet therapy** is the standard of care for STEMI, typically consisting of aspirin plus a P2Y12 inhibitor (ADP receptor inhibitor)
- Since this patient has an **aspirin allergy**, an ADP receptor inhibitor such as **clopidogrel, ticagrelor, or prasugrel** becomes the critical next antiplatelet medication
- These agents **irreversibly or reversibly block the P2Y12 receptor** on platelets, preventing ADP-mediated platelet activation and aggregation
- This is essential for preventing further thrombotic complications during and after percutaneous coronary intervention (PCI)
*Cyclooxygenase activator*
- No cyclooxygenase activator exists in clinical practice for cardiovascular disease
- Aspirin works as a **cyclooxygenase inhibitor**, blocking COX-1 to prevent thromboxane A2 synthesis, but the patient is allergic to aspirin
- "Activating" cyclooxygenase would promote platelet aggregation, which is counterproductive in acute MI
*Phosphodiesterase activator*
- Phosphodiesterase activation would decrease cAMP/cGMP levels, which is not therapeutically beneficial
- **Phosphodiesterase inhibitors** (such as cilostazol or dipyridamole) can have antiplatelet effects by increasing cAMP, but they are not first-line agents for acute STEMI
- An activator would have the opposite and undesirable effect
*Thrombin inhibitor*
- Thrombin inhibitors (e.g., **bivalirudin, heparin**) are anticoagulants that prevent conversion of fibrinogen to fibrin
- While **anticoagulation is important in STEMI management**, it is used as adjunctive therapy alongside antiplatelet agents
- Given the aspirin allergy, the immediate priority is **antiplatelet therapy with an ADP receptor inhibitor**
- Anticoagulation would typically be given concurrently but is not "the next" critical medication in this specific context
*Vitamin K epoxide reductase inhibitor*
- Warfarin is a vitamin K epoxide reductase inhibitor used for chronic anticoagulation
- It has a **slow onset of action** (days) and is inappropriate for acute STEMI management
- It is used for long-term anticoagulation in conditions like atrial fibrillation or mechanical heart valves, not for acute coronary syndromes requiring rapid platelet inhibition
STEMI diagnosis and management US Medical PG Question 7: A 71-year-old woman with a past medical history of type 2 diabetes, hypercholesterolemia, and hypertension was admitted to the hospital 8 hours ago with substernal chest pain for management of acute non-ST-elevated myocardial infarction (NSTEMI). The ECG findings noted by ST-depressions and T-wave inversions on anterolateral leads, which is also accompanied by elevated cardiac enzymes. Upon diagnosis, management with inhaled oxygen therapy, beta-blockers and aspirin, and low-molecular-weight heparin therapy were initiated, and she was placed on bed rest with continuous electrocardiographic monitoring. Since admission, she required 2 doses of sublingual nitroglycerin for recurrent angina, and the repeat troponin levels continued to rise. Given her risk factors, plans were made for early coronary angiography. The telemetry nurse calls the on-call physician because of her concern with the patient's mild confusion and increasing need for supplemental oxygen. At bedside evaluation, The vital signs include: heart rate 122/min, blood pressure 89/40 mm Hg, and the pulse oximetry is 91% on 6L of oxygen by nasal cannula. The telemetry and a repeat ECG show sinus tachycardia. She is breathing rapidly, appears confused, and complains of shortness of breath. On physical exam, the skin is cool and clammy and appears pale and dull. She has diffuse bilateral pulmonary crackles, and an S3 gallop is noted on chest auscultation with no new murmurs. She has jugular venous distention to the jaw-line, rapid and faint radial pulses, and 1+ dependent edema. She is immediately transferred to the intensive care unit for respiratory support and precautions for airway security. The bedside sonography shows abnormal hypodynamic anterior wall movement and an ejection fraction of 20%, but no evidence of mitral regurgitation or ventricular shunt. The chest X-ray demonstrates cephalization of pulmonary veins and pulmonary edema. What is the most appropriate next step in the stabilization of this patient?
- A. Obtain blood cultures and start preliminary broad-spectrum antibiotics
- B. Start intravenous fluids and epinephrine therapy
- C. Intubate the patient and perform an emergency cardiocentesis
- D. Initiate dopamine therapy and diuresis (Correct Answer)
- E. Insert two large-bore intravenous catheters and start rapid fluid resuscitation
STEMI diagnosis and management Explanation: ***Initiate dopamine therapy and diuresis***
- This patient is presenting with **cardiogenic shock** secondary to extensive NSTEMI, characterized by **hypotension**, signs of **end-organ hypoperfusion** (confusion, cool clammy skin), **pulmonary edema** (crackles, dyspnea, elevated jugular venous pressure), and **severely reduced ejection fraction**. Dopamine is a vasopressor that can increase cardiac output and blood pressure.
- **Diuresis** with loop diuretics such as furosemide is crucial to reduce the fluid overload contributing to the pulmonary edema and jugular venous distention.
*Obtain blood cultures and start preliminary broad-spectrum antibiotics*
- While infection is a concern in critically ill patients, there are **no signs of infection** in this clinical presentation. The patient's symptoms are clearly attributable to acute cardiac decompensation.
- A delay in treating cardiogenic shock to investigate for infection would be detrimental and potentially fatal.
*Start intravenous fluids and epinephrine therapy*
- Intravenous fluids would **worsen the existing pulmonary edema and fluid overload** in a patient with an ejection fraction of 20% and clinical signs of volume overload (crackles, JVD, S3 gallop).
- Epinephrine is a potent vasopressor but is generally reserved for more severe shock refractory to other inotropes, or in cases of **cardiac arrest**, not typically first-line for cardiogenic shock with significant pulmonary congestion.
*Intubate the patient and perform an emergency cardiocentesis*
- While the patient is confused and has respiratory distress, **intubation** should be considered after hemodynamic stabilization, if respiratory failure persists or worsens.
- **Cardiocentesis** is indicated for **cardiac tamponade**, which is not supported by the absence of an effusion on bedside sonography and the finding of hypodynamic anterior wall movement, which points to pump failure.
*Insert two large-bore intravenous catheters and start rapid fluid resuscitation*
- This patient is in **cardiogenic shock with clear evidence of fluid overload**, including pulmonary edema and elevated jugular venous pressure.
- **Rapid fluid resuscitation would exacerbate heart failure** and worsen respiratory compromise due to increased preload.
STEMI diagnosis and management US Medical PG Question 8: A 70-year-old man is brought to the emergency room with complaints of severe substernal chest pain for the last hour. The pain started suddenly, and the patient describes the pain as “going into the shoulder”. The patient took aspirin at home and has been given multiple doses of sublingual nitroglycerin, but the pain has not subsided. He has a blood pressure of 112/84 mm Hg, the pulse is 63/min, the respiratory rate is 18/min, and the temperature is 36.9°C (98.0°F). Cardiac auscultation reveals normal S1 and S2 sounds, however, an additional S4 sound is heard. The patient is sweating profusely, and the lungs are clear to auscultation. No jugular venous distension or pedal edema is observed. His initial ECG shows ST elevation in leads II, III, and aVF. Which of the following will likely have the most benefit in this patient?
- A. Antiarrhythmics
- B. Percutaneous coronary intervention (Correct Answer)
- C. Thrombolytics
- D. Beta blockers
- E. Clopidogrel
STEMI diagnosis and management Explanation: ***Percutaneous coronary intervention***
- This patient is experiencing a **ST-elevation myocardial infarction (STEMI)**, indicated by severe chest pain radiating to the shoulder, no relief with nitroglycerin, and ST elevation in leads II, III, and aVF.
- **Reperfusion therapy** is crucial for STEMI, and PCI is the preferred method when available within the recommended timeframe (typically <90-120 minutes from first medical contact) as it directly opens the occluded coronary artery.
*Antiarrhythmics*
- While **arrhythmias** can occur during an MI, there is no indication that the patient is currently experiencing a life-threatening arrhythmia requiring immediate antiarrhythmic drug administration.
- The primary goal in STEMI is **reperfusion**, not immediate arrhythmia suppression unless the arrhythmia is hemodynamically unstable.
*Thrombolytics*
- **Thrombolytics (fibrinolytics)** are an alternative reperfusion strategy for STEMI if PCI is not available or cannot be performed within the recommended timeframe.
- Given that the question asks for the "most benefit," and PCI is generally superior to thrombolytics in terms of complete reperfusion and clinical outcomes when available promptly, thrombolytics would not be the first choice.
*Beta blockers*
- **Beta blockers** are important for managing MI by reducing myocardial oxygen demand and preventing arrhythmias; however, they are often initiated after reperfusion and careful patient evaluation, especially in the acute phase of STEMI where immediate reperfusion is paramount.
- They should be used with caution if there are signs of **heart failure** or **cardiogenic shock**, which are not present here but still highlight that it's not the immediate, most beneficial intervention.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent that would be part of the medical management for STEMI, along with aspirin and anticoagulants, to prevent further clot formation.
- While important, it is an adjunctive therapy and does not directly address the need for **rapid reperfusion** to restore blood flow to the ischemic myocardium, which is the most critical intervention in STEMI.
STEMI diagnosis and management US Medical PG Question 9: A 70-year-old man presents to the emergency department with severe substernal chest pain of one hour’s duration. The patient was taking a morning walk when the onset of pain led him to seek care. His past medical history includes coronary artery disease, hyperlipidemia, and hypertension. Medications include aspirin, losartan, and atorvastatin. An electrocardiogram reveals ST elevations in the inferior leads II, III, and avF as well as in leads V5 and V6. The ST elevations found in leads V5-V6 are most indicative of pathology in which of the following areas of the heart?
- A. Lateral wall of left ventricle, left circumflex coronary artery (Correct Answer)
- B. Left atrium, left main coronary artery
- C. Inferior wall, right coronary artery
- D. Interventricular septum, left anterior descending coronary artery
- E. Right ventricle, right coronary artery
STEMI diagnosis and management Explanation: ***Lateral wall of left ventricle, left circumflex coronary artery***
- **ST elevations in leads V5 and V6** are characteristic findings for an **anterolateral or high lateral myocardial infarction**.
- These leads correspond to the **lateral wall of the left ventricle**, which is primarily supplied by the **left circumflex coronary artery**.
*Left atrium, left main coronary artery*
- The **left atrium** is involved in atrial arrhythmias or hypertrophy, but **ST segment changes** on an ECG primarily reflect **ventricular ischemia or infarction**.
- While the **left main coronary artery** supplies a large portion of the left ventricle, its occlusion typically presents with more widespread and severe **ST elevations**, potentially affecting multiple lead groups beyond just V5-V6, and often indicates extensive damage.
*Inferior wall, right coronary artery*
- **Inferior wall infarctions** are indicated by **ST elevations in leads II, III, and aVF** (which are also present in this patient), primarily supplied by the **right coronary artery**.
- Although there is an inferior MI, the question specifically asks about the V5-V6 changes, which point to a distinct region.
*Interventricular septum, left anterior descending coronary artery*
- **ST elevations in V1-V4** are typically associated with an **anterior myocardial infarction**, affecting the **interventricular septum** and anterior wall, often due to occlusion of the **left anterior descending coronary artery**.
- The given leads V5-V6 do not primarily represent the interventricular septum.
*Right ventricle, right coronary artery*
- **Right ventricular infarction** is indicated by **ST elevations in lead V4R** (a right-sided lead) and can accompany inferior infarctions; however, V5-V6 do not specifically represent the right ventricle.
- The **right ventricle** is primarily supplied by the **right coronary artery**, not branches of the left coronary system, and RV infarction would require right-sided ECG leads for diagnosis.
STEMI diagnosis and management US Medical PG Question 10: A 54-year-old woman is brought to the emergency department because of a 2-hour history of nausea and retrosternal chest pain. She has a 15-year history of type 2 diabetes mellitus. Her current medications include atorvastatin, metformin, and lisinopril. She is diaphoretic. Her serum troponin level is 3.0 ng/mL (N: < 0.04). She undergoes cardiac catheterization. A photograph of coronary angiography performed prior to percutaneous coronary intervention is shown. An acute infarct associated with the finding on angiography is most likely to manifest with ST elevations in which of the following leads on ECG?
- A. V3R–V6R
- B. I, aVR
- C. V1–V6 (Correct Answer)
- D. II, III, and aVF
- E. V7–V9
STEMI diagnosis and management Explanation: ***V1–V6***
- The angiography shows a significant occlusion in the **left anterior descending (LAD) artery**
- LAD occlusion causes **anterior wall myocardial infarction**
- Anterior MI manifests with **ST elevations in precordial leads V1–V6**
- This is the classic ECG pattern for LAD territory infarction
*V3R–V6R*
- These right-sided precordial leads indicate **right ventricular infarction**
- RV infarction is associated with **proximal right coronary artery (RCA) occlusion**
- Not consistent with the LAD occlusion shown in the angiography
*I, aVR*
- Lead **aVR ST elevation** (especially >1 mm or greater than V1) suggests **left main coronary artery occlusion** or severe multi-vessel disease
- This pattern typically shows widespread ST depression in other leads
- Does not specifically indicate isolated LAD occlusion
*II, III, and aVF*
- ST elevations in these inferior leads indicate **inferior wall myocardial infarction**
- Inferior MI is caused by **right coronary artery (RCA)** occlusion (80%) or left circumflex artery (20%)
- Not associated with LAD occlusion
*V7–V9*
- These posterior leads indicate **posterior wall myocardial infarction**
- Posterior MI results from **left circumflex artery** or dominant RCA occlusion
- Not the primary finding with LAD occlusion
More STEMI diagnosis and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.