Special populations (elderly, renal dysfunction) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Special populations (elderly, renal dysfunction). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Special populations (elderly, renal dysfunction) US Medical PG Question 1: A 50-year-old morbidly obese woman presents to a primary care clinic for the first time. She states that her father recently died due to kidney failure and wants to make sure she is healthy. She works as an accountant, is not married or sexually active, and drinks alcohol occasionally. She currently does not take any medications. She does not know if she snores at night but frequently feels fatigued. She denies any headaches but reports occasional visual difficulties driving at night. She further denies any blood in her urine or increased urinary frequency. She does not engage in any fitness program. She has her period every 2 months with heavy flows. Her initial vital signs reveal that her blood pressure is 180/100 mmHg and heart rate is 70/min. Her body weight is 150 kg (330 lb). On physical exam, the patient has droopy eyelids, a thick neck with a large tongue, no murmurs or clicks on cardiac auscultation, clear lungs, a soft nontender, albeit large abdomen, and palpable pulses in her distal extremities. She can walk without difficulty. A repeat measurement of her blood pressure shows 155/105 mmHg. Which among the following is part of the most appropriate next step in management?
- A. Renal artery doppler ultrasonography
- B. Polysomnography
- C. Urinalysis (Correct Answer)
- D. Thyroid-stimulating hormone
- E. Cortisol levels
Special populations (elderly, renal dysfunction) Explanation: ***Urinalysis***
- Given the patient's strong family history of **kidney failure**, current presentation with **hypertension (BP 180/100 mmHg, confirmed at 155/105 mmHg)**, and concern for her health, a urinalysis is a crucial initial step to look for signs of kidney damage or disease.
- Urinalysis can detect **proteinuria**, **hematuria**, or other abnormalities indicative of renal pathology, helping to assess her kidney health.
*Renal artery doppler ultrasonography*
- While **renal artery stenosis** can cause hypertension, it is usually considered after initial non-invasive tests and if there are specific signs of secondary hypertension like a **renal bruit** or **unexplained renal insufficiency**, which are not explicitly described here as a first step.
- This is a more advanced diagnostic test and not typically the *most appropriate next step* before basic screening like urinalysis.
*Polysomnography*
- The patient's **morbid obesity**, **fatigue**, and physical exam findings like a **thick neck with a large tongue** suggest **obstructive sleep apnea (OSA)**, for which polysomnography is the diagnostic test.
- However, while important, addressing the immediate concern of **hypertension** and assessing **kidney health** (given the family history) is a higher priority in the *initial* workup.
*Thyroid-stimulating hormone*
- Symptoms like **fatigue**, **heavy menstrual periods (menorrhagia)**, and features like a **thick tongue** could suggest **hypothyroidism**.
- However, **hypertension** and the urgent need to evaluate **kidney function** (due to family history and current high blood pressure) make urinalysis a more immediate and critical step before an extensive endocrine workup.
*Cortisol levels*
- Elevated blood pressure, obesity, and menstrual irregularities could, in some contexts, raise suspicion for **Cushing's syndrome**.
- However, there are no classic features like **buffalo hump**, **moon facies**, or **striae** mentioned, and assessing renal involvement given the family history and current hypertension is a more direct next step.
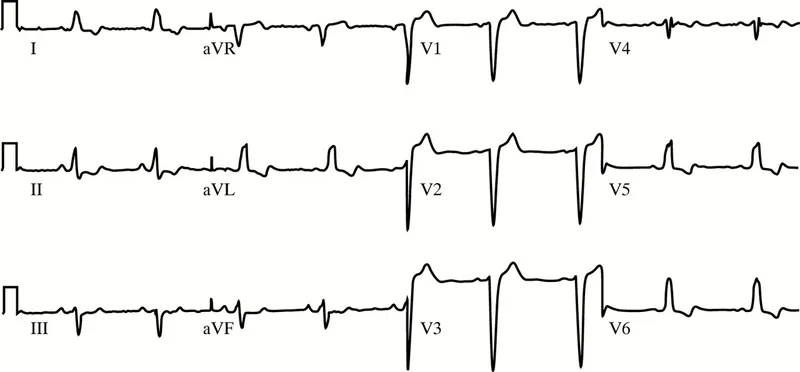
Special populations (elderly, renal dysfunction) US Medical PG Question 2: A 50-year-old man with a history of stage 4 kidney disease was admitted to the hospital for an elective hemicolectomy. His past medical history is significant for severe diverticulitis. After the procedure he becomes septic and was placed on broad spectrum antibiotics. On morning rounds, he appear weak and complains of fatigue and nausea. His words are soft and he has difficulty answering questions. His temperature is 38.9°C (102.1°F), heart rate is 110/min, respiratory rate is 15/min, blood pressure 90/65 mm Hg, and saturation is 89% on room air. On physical exam, his mental status appears altered. He has a bruise on his left arm that spontaneously appeared overnight. His cardiac exam is positive for a weak friction rub. Blood specimens are collected and sent for evaluation. An ECG is performed (see image). What therapy will this patient most likely receive next?
- A. Send the patient for hemodialysis (Correct Answer)
- B. Perform a STAT pericardiocentesis
- C. Prepare the patient for renal transplant
- D. Treat the patient with aspirin
- E. Treat the patient with cyclophosphamide and prednisone
Special populations (elderly, renal dysfunction) Explanation: ***Send the patient for hemodialysis***
- This patient presents with symptoms of **uremic encephalopathy** and **uremic pericarditis** in the context of **stage 4 kidney disease**. The altered mental status, weakness, fatigue, nausea, and the development of a bruise (which could indicate uremic coagulopathy) are suggestive of severe uremia. The ECG shows widespread **ST elevation and PR depression**, particularly noticeable in leads like II, V2-V6, which is a classic finding for pericarditis. The **weak friction rub** confirms this clinical suspicion. Hemodialysis is crucial to rapidly remove uremic toxins and resolve both uremic encephalopathy and pericarditis.
- The ECG findings, including diffuse **ST elevation** with **PR depression**, are characteristic of **pericarditis**. In a patient with end-stage renal disease, **uremia** is a common cause of pericarditis, which can be life-threatening if not promptly treated with dialysis.
*Perform a STAT pericardiocentesis*
- While the patient has pericarditis, there are no immediate signs of **cardiac tamponade**, such as muffled heart sounds, jugular venous distension, or pulsus paradoxus, that would necessitate an emergency pericardiocentesis.
- The primary treatment for **uremic pericarditis** is typically **hemodialysis** to resolve the underlying uremic state, not direct fluid removal unless tamponade is present.
*Prepare the patient for renal transplant*
- **Renal transplant** is a long-term solution for end-stage renal disease, but it is not an acute intervention for immediate life-threatening uremic complications like uremic pericarditis and encephalopathy.
- The patient needs urgent stabilization and treatment of his current acute medical issues before transplant consideration.
*Treat the patient with aspirin*
- While aspirin can be used for some forms of pericarditis, it is generally **contraindicated** in patients with **uremic pericarditis** due to the increased risk of **gastric bleeding** and potential exacerbation of uremic coagulopathy.
- The primary treatment for uremic pericarditis is **dialysis**, not anti-inflammatory medications, as the inflammation is driven by uremic toxins.
*Treat the patient with cyclophosphamide and prednisone*
- **Immunosuppressants** like cyclophosphamide and prednisone are used for autoimmune or inflammatory conditions causing pericarditis, such as systemic lupus erythematosus.
- This patient's pericarditis is clearly linked to **uremia** from kidney disease, not an autoimmune condition, making immunosuppressive therapy inappropriate and potentially harmful.
Special populations (elderly, renal dysfunction) US Medical PG Question 3: A 62-year-old man comes to the physician in May for a routine health maintenance examination. He feels well. He underwent a right inguinal hernia repair 6 months ago. He has hypertension and type 2 diabetes mellitus. There is no family history of serious illness. Current medications include metformin, sitagliptin, enalapril, and metoprolol. He received the zoster vaccine 1 year ago. He received the PPSV23 vaccine 4 years ago. His last colonoscopy was 7 years ago and was normal. He smoked a pack of cigarettes a day for 20 years but quit 17 years ago. He drinks two to three alcoholic beverages on weekends. He is allergic to amoxicillin. He is scheduled to visit Australia and New Zealand in 2 weeks to celebrate his 25th wedding anniversary. He appears healthy. Vital signs are within normal limits. An S4 is heard at the apex. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate recommendation at this time?
- A. Colonoscopy
- B. Influenza vaccine (Correct Answer)
- C. Pneumococcal conjugate vaccine 13
- D. Cardiac stress test
- E. Abdominal ultrasound
Special populations (elderly, renal dysfunction) Explanation: ***Influenza vaccine***
- Current guidelines recommend annual **influenza vaccination** for all adults, particularly those over 60 years old and those with chronic medical conditions like diabetes and hypertension.
- **Critical timing consideration**: The patient is traveling to Australia and New Zealand (Southern Hemisphere) in 2 weeks, where it will be **winter season** (May-September) with peak influenza activity.
- He is a **high-risk patient** (age >60, diabetes, hypertension, cardiovascular disease) who should receive influenza vaccine before travel to areas experiencing influenza season.
- This is the **most appropriate and time-sensitive recommendation** at this visit.
*Colonoscopy*
- The patient had a normal colonoscopy 7 years ago; current guidelines suggest a repeat colonoscopy every **10 years** for average-risk individuals.
- There are no new symptoms, family history, or risk factors that would necessitate an earlier repeat colonoscopy at this time.
*Pneumococcal conjugate vaccine 13*
- The patient received **PPSV23** four years ago at approximately age 58.
- Per **current CDC guidelines (2019+)**, PCV13 is **no longer routinely recommended** for immunocompetent adults ≥65 years old.
- PPSV23 alone is now the standard recommendation for adults ≥65, which this patient has already received.
- PCV13 may be considered through **shared decision-making** in specific circumstances, but is not a routine or urgent recommendation.
*Cardiac stress test*
- Although the patient has risk factors for cardiovascular disease (hypertension, diabetes, former smoker) and an **S4 heart sound** (indicating **left ventricular hypertrophy**), he is asymptomatic.
- Routine **screening stress tests** are not recommended for asymptomatic individuals without signs of active cardiac ischemia.
*Abdominal ultrasound*
- There are **no symptoms** or specific indications (e.g., abdominal aortic aneurysm screening criteria not met - would need age 65-75 with smoking history).
- The patient is 62 years old and quit smoking 17 years ago, so AAA screening criteria are not yet met.
- Routine screening abdominal ultrasounds are not indicated.
Special populations (elderly, renal dysfunction) US Medical PG Question 4: A primary care physician who focuses on treating elderly patients is researching recommendations for secondary prevention. She is particularly interested in recommendations regarding aspirin, as she has several patients who ask her if they should take it. Of the following, which patient should be started on lifelong aspirin as monotherapy for secondary prevention of atherosclerotic cardiovascular disease?
- A. An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits
- B. A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago
- C. A 67-year-old female who has diabetes mellitus and atrial fibrillation
- D. A 45-year-old female with no health problems
- E. A 63-year-old male with a history of a transient ischemic attack (Correct Answer)
Special populations (elderly, renal dysfunction) Explanation: **A 63-year-old male with a history of a transient ischemic attack**
- A patient with a history of **Transient Ischemic Attack (TIA)** has a high risk of subsequent stroke and should be on **lifelong aspirin monotherapy** for secondary prevention of **atherosclerotic cardiovascular disease (ASCVD)**.
- Aspirin helps prevent further thrombotic events by inhibiting platelet aggregation, making it a cornerstone for secondary prevention after TIA or ischemic stroke.
*An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits*
- Aspirin is generally **contraindicated** in patients with a history of **hemorrhagic stroke** due to the increased risk of recurrent bleeding.
- In such cases, the risks of aspirin therapy typically **outweigh the benefits** for cardiovascular prevention.
*A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago*
- A patient with a recently placed **drug-eluting stent (DES)** requires **dual antiplatelet therapy (DAPT)**, typically aspirin plus a P2Y12 inhibitor, for a specific duration (e.g., 6-12 months), not aspirin monotherapy.
- Monotherapy with aspirin alone would be **insufficient** to prevent stent thrombosis in the immediate post-stenting period.
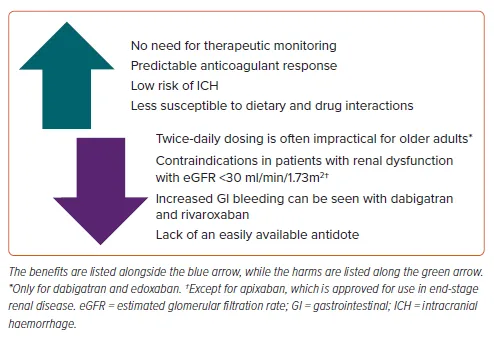
*A 67-year-old female who has diabetes mellitus and atrial fibrillation*
- This patient has two significant risk factors requiring specific management: **diabetes mellitus** for cardiovascular risk and **atrial fibrillation** for stroke risk.
- For atrial fibrillation, **anticoagulation with warfarin or a direct oral anticoagulant (DOAC)** is typically indicated, which makes aspirin monotherapy either unnecessary or potentially harmful if used alone.
*A 45-year-old female with no health problems*
- There is no indication for **aspirin primary prevention** in this patient, especially given the increased risk of bleeding without a clear cardiovascular benefit.
- Guidelines currently recommend against routine aspirin use for primary prevention in healthy individuals due to the **unfavorable risk-benefit ratio**.
Special populations (elderly, renal dysfunction) US Medical PG Question 5: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Special populations (elderly, renal dysfunction) Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
Special populations (elderly, renal dysfunction) US Medical PG Question 6: A 67-year-old man presents to the emergency department for squeezing and substernal chest pain. He states that he was at home eating dinner when his symptoms began. The patient has a past medical history of diabetes, hypertension, and dyslipidemia. He is currently taking atorvastatin, lisinopril, insulin, metformin, metoprolol, and aspirin. Six days ago he underwent percutaneous coronary intervention. His temperature is 99.5°F (37.5°C), blood pressure is 197/118 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals an uncomfortable elderly man who is sweating. An ECG is ordered. Which of the following is the best next step in management for this patient?
- A. Stress testing
- B. Angiography (Correct Answer)
- C. Cardiac troponins
- D. Creatine kinase-MB
- E. Myoglobin
Special populations (elderly, renal dysfunction) Explanation: ***Correct: Angiography***
- This patient presenting with **acute chest pain 6 days post-PCI** is at high risk for **stent thrombosis or acute in-stent restenosis**, which represents a life-threatening emergency.
- Given the **clinical instability** (severe hypertension 197/118, tachycardia 120/min, diaphoresis) and classic ACS symptoms in the immediate post-PCI period, **urgent coronary angiography** is the best next step in management.
- While ECG and troponins are important diagnostic tools, this patient requires **immediate intervention** to evaluate the recent PCI site and potentially perform emergent revascularization.
- In the setting of suspected **acute stent thrombosis**, time to reperfusion is critical, and angiography allows both diagnosis and treatment.
*Incorrect: Cardiac troponins*
- While troponins are essential biomarkers for myocardial injury and should be obtained, they are a **diagnostic test** rather than definitive management.
- Waiting for troponin results would delay definitive management in a patient with clear clinical evidence of ACS.
- In this high-risk post-PCI patient with active symptoms, management should not wait for biomarker confirmation.
*Incorrect: Stress testing*
- Stress testing is **absolutely contraindicated** in patients with active chest pain and suspected acute MI.
- It could precipitate further myocardial ischemia, arrhythmias, or cardiac arrest.
- Stress testing is reserved for risk stratification in stable patients or after ACS has been ruled out.
*Incorrect: Creatine kinase-MB*
- CK-MB is less sensitive and specific than troponins for myocardial injury, as it can be elevated in skeletal muscle conditions.
- It has a shorter elevation window and has largely been replaced by troponins in modern practice.
- Like troponins, it would not change the immediate management need in this clinically unstable patient.
*Incorrect: Myoglobin*
- Myoglobin lacks cardiac specificity (present in both cardiac and skeletal muscle) and has poor diagnostic accuracy for MI.
- Its rapid rise and fall make it unreliable, and it generates many false positives.
- It has no role in guiding management decisions in suspected ACS.
Special populations (elderly, renal dysfunction) US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Special populations (elderly, renal dysfunction) Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Special populations (elderly, renal dysfunction) US Medical PG Question 8: A 59-year-old man presents to his primary care physician for fatigue. In general, he has been in good health; however, he recently has experienced some weight loss, abdominal pain, and general fatigue. He has a past medical history of anxiety, diabetes, a fracture of his foot sustained when he tripped, and a recent cold that caused him to miss work for a week. His current medications include metformin, insulin, buspirone, vitamin D, calcium, and sodium docusate. His temperature is 99.5°F (37.5°C), blood pressure is 150/100 mmHg, pulse is 90/min, respirations are 18/min, and oxygen saturation is 98% on room air. Physical exam reveals a calm gentleman. A mild systolic murmur is heard in the left upper sternal region. The rest of the physical exam is within normal limits. Laboratory values are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 66,500/mm^3 with normal differential
Platelet count: 177,000/mm^3
Leukocyte alkaline phosphatase: elevated
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
BUN: 20 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.9 mEq/L
AST: 12 U/L
ALT: 10 U/L
Which of the following is the most likely diagnosis?
- A. Chronic myeloid leukemia
- B. Acute lymphoblastic leukemia
- C. Multiple myeloma
- D. Leukemoid reaction (Correct Answer)
- E. Chronic lymphocytic leukemia
Special populations (elderly, renal dysfunction) Explanation: ***Leukemoid reaction***
- The **highly elevated leukocyte count** (66,500/mm^3) with **normal differential** and **elevated leukocyte alkaline phosphatase (LAP)** are classic features of a leukemoid reaction.
- This condition is a reactive increase in white blood cells, often triggered by **severe infections, inflammation, or malignancy**, rather than a primary hematologic malignancy.
- The patient's **recent cold/infection** provides a clear trigger for this reactive process.
*Chronic myeloid leukemia*
- While CML also presents with marked leukocytosis, it is typically characterized by a **low or normal LAP score** and a left shift with immature myeloid forms (e.g., myelocytes, metamyelocytes).
- The patient's **normal differential** and **elevated LAP score** argue strongly against CML.
*Acute lymphoblastic leukemia*
- ALL is characterized by the presence of a large number of **lymphoblasts** (immature lymphocytes) in the blood and bone marrow, which is not suggested by the normal differential.
- It usually presents with symptoms of **bone marrow failure** (anemia, thrombocytopenia, infection) and often affects children, though it can occur in adults.
*Multiple myeloma*
- Multiple myeloma is a plasma cell malignancy characterized by **monoclonal gammopathy**, bone lesions, renal failure, and hypercalcemia; **marked leukocytosis is not a primary feature**.
- Although the patient has mildly elevated calcium, the absence of other myeloma features (renal dysfunction, anemia, bone pain) and the **very high WBC count with elevated LAP** make this diagnosis unlikely.
*Chronic lymphocytic leukemia*
- CLL is characterized by a **profound lymphocytosis** (elevated lymphocytes) with mature-appearing cells, which is not described by the "normal differential" of the leukocyte count.
- The elevated LAP would also be unusual in CLL, as CLL cells typically have low LAP activity.
Special populations (elderly, renal dysfunction) US Medical PG Question 9: Two days after undergoing an uncomplicated total thyroidectomy, a 63-year-old woman has acute, progressive chest pain. The pain is sharp and burning. She feels nauseated and short of breath. The patient has a history of hypertension, type 1 diabetes mellitus, medullary thyroid cancer, multiple endocrine neoplasia type 2A, anxiety, coronary artery disease, and gastroesophageal reflux disease. She smoked half a pack of cigarettes daily for 24 years but quit 18 years ago. Current medications include lisinopril, insulin glargine, insulin aspart, sertraline, aspirin, ranitidine, and levothyroxine. She appears anxious and diaphoretic. Her temperature is 37.4°C (99.3°F), pulse is 64/min, respirations are 17/min, and blood pressure is 148/77 mm Hg. The lungs are clear to auscultation. Examination shows a 3-cm linear incision over the anterior neck with 1 mm of surrounding erythema and mild serous discharge. The chest wall and abdomen are nontender. There is 5/5 strength in all extremities and decreased sensation to soft touch on the feet bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Obtain an ECG and troponin T levels (Correct Answer)
- B. Administer IV pantoprazole and schedule endoscopy
- C. Discontinue levothyroxine and obtain fT4 levels
- D. Administer IV levofloxacin and obtain chest radiograph
- E. Obtain urine and plasma metanephrine levels
Special populations (elderly, renal dysfunction) Explanation: **Obtain an ECG and troponin T levels**
- The patient presents with acute, progressive **chest pain that is sharp and burning**, along with nausea and shortness of breath, which are classic symptoms of an acute coronary syndrome, especially given her history of **coronary artery disease**, hypertension, diabetes, and prior smoking.
- An **ECG** and **troponin T levels** are crucial first steps to evaluate for myocardial ischemia or infarction in this high-risk patient.
*Administer IV pantoprazole and schedule endoscopy*
- While the patient has a history of gastroesophageal reflux disease (GERD) and her pain is described as "burning," the **acuteness, progression, and associated symptoms** (nausea, shortness of breath) in a patient with significant cardiac risk factors make a GI cause less likely as the primary concern.
- Empiric treatment for GERD without first ruling out a life-threatening cardiac event would be inappropriate and potentially dangerous.
*Discontinue levothyroxine and obtain fT4 levels*
- The patient is taking levothyroxine after a thyroidectomy for medullary thyroid cancer, but there is no immediate indication of thyroid hormone imbalance (e.g., hyperthyroidism causing chest pain) that would warrant discontinuing her medication or rushing fT4 levels as the first step in an acute chest pain presentation.
- Her pulse of 64/min is not suggestive of hyperthyroidism, which typically causes tachycardia.
*Administer IV levofloxacin and obtain chest radiograph*
- While shortness of breath can be a symptom of pneumonia, the **sharp, burning nature of the chest pain**, coupled with the absence of fever (temperature 37.4°C is mild), cough, or abnormal lung sounds (lungs clear to auscultation), makes an acute infection like pneumonia less probable as the primary diagnosis.
- Antibiotics and a chest radiograph would be considered after ruling out more immediate life-threatening conditions like acute coronary syndrome.
*Obtain urine and plasma metanephrine levels*
- The patient has a history of multiple endocrine neoplasia type 2A (MEN2A), which includes medullary thyroid cancer and can be associated with pheochromocytoma (adrenal tumor secreting catecholamines). However, her blood pressure (148/77 mm Hg) is not acutely elevated to crisis levels, and her symptoms are more consistent with cardiac ischemia than a pheochromocytoma crisis.
- While metanephrine levels would be important for long-term follow-up of MEN2A, they are not the immediate next step for acute chest pain in a patient with known coronary artery disease.
Special populations (elderly, renal dysfunction) US Medical PG Question 10: A 25-year-old man comes to the emergency department because of a 1-week-history of progressively worsening dyspnea and intermittent chest pain that increases on inspiration. He had an upper respiratory tract infection 2 weeks ago. His pulse is 115/min and blood pressure is 100/65 mm Hg. Examination shows inspiratory crackles bilaterally. His serum troponin I is 0.21 ng/mL (N < 0.1). An x-ray of the chest shows an enlarged cardiac silhouette and prominent vascular markings in both lung fields; costophrenic angles are blunted. A rhythm strip shows inverted T waves. Which of the following additional findings is most likely in this patient's condition?
- A. Opening snap with low-pitched diastolic rumble
- B. Elevated brain natriuretic peptide (Correct Answer)
- C. Sarcomere duplication
- D. Right ventricular dilation
- E. Electrical alternans
Special populations (elderly, renal dysfunction) Explanation: ***Elevated brain natriuretic peptide***
- This patient presents with symptoms of **dyspnea**, **chest pain**, **tachycardia**, elevated **troponin I**, an enlarged **cardiac silhouette** with prominent vascular markings, and **blunted costophrenic angles**, all consistent with **cardiomyopathy** and heart failure, likely post-viral **myocarditis**.
- **Brain natriuretic peptide (BNP)** is released by myocardial cells in response to ventricular stretch and volume overload, making it a strong indicator for **heart failure**.
*Opening snap with low-pitched diastolic rumble*
- An **opening snap** followed by a **low-pitched diastolic rumble** is characteristic of **mitral stenosis**, a valvular disorder not suggested by the patient's acute presentation and other findings.
- Mitral stenosis would typically be associated with a history of **rheumatic fever** and more specific echocardiographic findings of valve abnormalities.
*Sarcomere duplication*
- **Sarcomere duplication** and disarray are characteristic pathological findings in **hypertrophic cardiomyopathy (HCM)**, an inherited genetic disorder.
- While HCM can cause dyspnea and chest pain, this patient's acute presentation following a viral infection and evidence of fluid overload are more indicative of an **acquired cardiomyopathy** such as myocarditis.
*Right ventricular dilation*
- While the patient has signs of **heart failure**, the chest X-ray shows an **enlarged cardiac silhouette** and **prominent vascular markings in both lung fields** and **blunted costophrenic angles**, suggesting **left ventricular failure** with fluid redistribution and pleural effusions.
- Significant **right ventricular dilation** would typically be associated with signs of right-sided heart failure like **peripheral edema** and **jugular venous distension**, which are not explicitly mentioned as primary findings.
*Electrical alternans*
- **Electrical alternans** is a specific ECG finding characterized by beat-to-beat variation in the QRS amplitude or axis, most commonly associated with **pericardial effusion** leading to cardiac tamponade.
- Although the patient has an enlarged cardiac silhouette, which could indicate effusion, the primary findings point more broadly to **myocardial dysfunction** and **heart failure** rather than tamponade.
More Special populations (elderly, renal dysfunction) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.