Secondary prevention US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Secondary prevention. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Secondary prevention US Medical PG Question 1: A 48-year-old male accountant presents to the family practice clinic for his first health check-up in years. He has no complaints, and as far as he is concerned, he is well. He does not have any known medical conditions. His blood pressure is 140/89 mm Hg and his heart rate is 89/min. Physical examination is otherwise unremarkable. What is the single best initial management for this patient?
- A. Treat the patient with beta-blockers.
- B. Try angiotensin-converting enzyme inhibitor.
- C. Start trial of calcium channel blockers.
- D. Return to the clinic for a repeat blood pressure reading and counseling on the importance of aerobic exercise. (Correct Answer)
- E. The patient does not require any treatment.
Secondary prevention Explanation: ***Return to the clinic for a repeat blood pressure reading and counseling on the importance of aerobic exercise.***
- The patient's blood pressure of **140/89 mm Hg** is considered **Stage 1 hypertension**. It is crucial to confirm sustained hypertension with **repeat measurements** over several weeks to avoid misdiagnosis and unnecessary medication.
- Initial management for Stage 1 hypertension without other compelling indications typically involves **lifestyle modifications**, such as regular aerobic exercise, dietary changes, and weight management, before initiating pharmacotherapy.
*Treat the patient with beta-blockers.*
- **Beta-blockers** are generally not first-line agents for isolated hypertension unless there are specific indications such as **concomitant heart failure**, **post-myocardial infarction**, or **migraines**.
- Without confirmed sustained hypertension and prior lifestyle interventions, initiating beta-blockers would be **premature**.
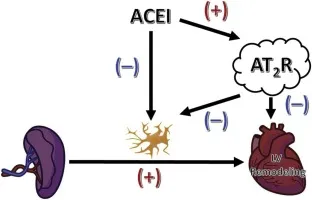
*Try angiotensin-converting enzyme inhibitor.*
- **ACE inhibitors** are effective first-line agents for hypertension, but only after proper diagnosis confirmation and a trial of **lifestyle modifications**.
- Rushing to medication without confirming sustained hypertension and exploring non-pharmacological approaches is **not the recommended initial step**.
*Start trial of calcium channel blockers.*
- **Calcium channel blockers** are also effective antihypertensive agents, especially in older adults or those with **isolated systolic hypertension**.
- However, similar to other pharmaceutical interventions, they should be considered **after confirming sustained hypertension** and attempting lifestyle changes.
*The patient does not require any treatment.*
- A blood pressure reading of **140/89 mm Hg** is elevated and indicates **Stage 1 hypertension**, which requires management.
- While immediate medication might not be necessary, **monitoring and lifestyle interventions** are crucial to prevent progression to more severe hypertension and cardiovascular complications.
Secondary prevention US Medical PG Question 2: A 47-year-old man comes to the physician for a routine health maintenance examination. He has no complaints and has no history of serious illness. He works as a forklift operator in a factory. His brother died of malignant melanoma. He smokes occasionally and drinks a glass of wine once a week. His pulse is 79/min and blood pressure is 129/84 mm Hg. Which of the following causes of death is this patient most at risk for over the next 15 years?
- A. Industrial accident
- B. Coronary artery disease (Correct Answer)
- C. Prostate cancer
- D. Malignant melanoma
- E. Lung cancer
Secondary prevention Explanation: ***Coronary artery disease***
- **Coronary artery disease (CAD)** is the **leading cause of death** in middle-aged men in the United States, making it the statistically most likely cause of death for this patient over the next 15 years.
- This patient has multiple modifiable risk factors including male sex, smoking (even occasional), and blood pressure of 129/84 mm Hg (elevated blood pressure/stage 1 hypertension by current guidelines).
- Even with relatively modest risk factors, the cumulative 15-year risk of cardiovascular mortality substantially exceeds other causes of death in this demographic group.
*Industrial accident*
- While working as a forklift operator carries some occupational risk, **industrial accidents** account for a very small proportion of deaths compared to chronic diseases in this age group.
- There is no indication of high-risk working conditions or safety concerns that would elevate this above cardiovascular disease as a cause of death.
*Prostate cancer*
- At age 47, the patient is relatively young for **prostate cancer** mortality. Most prostate cancer deaths occur in men over 65.
- While prostate cancer is common in older men, it typically has a long natural history, and mortality within 15 years would be less likely than cardiovascular disease in this age group.
- No specific high-risk features (family history, African-American ethnicity) are mentioned.
*Malignant melanoma*
- Although his brother died of **malignant melanoma**, family history alone does not make this the most likely cause of death over cardiovascular disease.
- The patient has no described personal risk factors (numerous nevi, history of severe sunburns, fair skin) or current lesions of concern.
- Melanoma mortality rates are substantially lower than cardiovascular disease mortality in middle-aged men.
*Lung cancer*
- The patient smokes **occasionally**, which confers some increased risk, but this is not described as heavy or chronic smoking.
- **Lung cancer** typically requires more substantial cumulative tobacco exposure (pack-years) to become a leading cause of mortality.
- Even in smokers, cardiovascular disease often causes death before lung cancer in this age group, particularly with modest smoking history.
Secondary prevention US Medical PG Question 3: A 70-year-old male presents for an annual exam. His past medical history is notable for shortness of breath when he sleeps, and upon exertion. Recently he has experienced dyspnea and lower extremity edema that seems to be worsening. Both of these symptoms have resolved since he was started on several medications and instructed to weigh himself daily. Which of the following is most likely a component of his medical management?
- A. Lidocaine
- B. Verapamil
- C. Carvedilol (Correct Answer)
- D. Aspirin
- E. Ibutilide
Secondary prevention Explanation: ***Carvedilol***
- The patient exhibits classic symptoms of **heart failure**, such as **dyspnea on exertion**, **orthopnea** (shortness of breath when he sleeps), and **lower extremity edema**.
- **Beta-blockers** like carvedilol are essential for managing **chronic heart failure** by reducing myocardial oxygen demand and improving cardiac function.
*Lidocaine*
- **Lidocaine** is primarily an **antiarrhythmic drug** used for acute treatment of **ventricular arrhythmias**, not for chronic heart failure management.
- It works by blocking sodium channels and has no direct benefit in addressing the underlying pathophysiology of heart failure.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** typically used for hypertension, angina, and supraventricular tachyarrhythmias.
- It can have **negative inotropic effects**, which are generally contraindicated or used with extreme caution in patients with **systolic heart failure** due to its potential to worsen cardiac function.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used for primary or secondary prevention of **atherosclerotic cardiovascular disease** (e.g., in patients with coronary artery disease).
- It does not directly manage the symptoms or pathophysiology of **heart failure** unless there is a coexisting ischemic etiology.
*Ibutilide*
- **Ibutilide** is an **antiarrhythmic drug** specifically used for the rapid conversion of **atrial flutter and atrial fibrillation** of recent onset to sinus rhythm.
- It is not a medication used for the long-term management of **heart failure** symptoms described in the patient.
Secondary prevention US Medical PG Question 4: Serum studies show a troponin T concentration of 6.73 ng/mL (N < 0.01), and fingerstick blood glucose concentration of 145 mg/dL. The cardiac catheterization team is activated. Treatment with unfractionated heparin, aspirin, ticagrelor, and sublingual nitroglycerin is begun, and the patient's pain subsides. His temperature is 37.3°C (99.1°F), pulse is 65/min, respirations are 23/min, and blood pressure is 91/60 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Which of the following is the most appropriate additional pharmacotherapy?
- A. Intravenous morphine
- B. Intravenous furosemide
- C. Intravenous insulin
- D. Oral atorvastatin (Correct Answer)
- E. Intravenous nitroglycerin
Secondary prevention Explanation: ***Oral atorvastatin***
- All patients with **acute coronary syndrome (ACS)** should receive high-intensity statin therapy, such as **atorvastatin 80 mg daily**, as early as possible.
- Statins stabilize plaques, reduce inflammation, and improve endothelial function, which are crucial in the acute setting of a myocardial infarction.
*Intravenous morphine*
- Morphine can be used for persistent chest pain refractory to nitroglycerin, but its routine use is now questioned due to potential adverse effects like hypotension and delayed antiplatelet absorption.
- The patient's pain has already subsided with initial treatment, and his blood pressure is already low (91/60 mm Hg), making morphine less appropriate.
*Intravenous furosemide*
- Furosemide is a loop diuretic primarily used for treating **fluid overload** and **pulmonary edema**, which are not indicated by the patient's current presentation (oxygen saturation 96%, no mention of crackles or dyspnea).
- Its use in a patient with **borderline hypotension** could worsen hemodynamic stability.
*Intravenous insulin*
- While the patient has elevated fingerstick glucose (145 mg/dL), this level does not immediately require intravenous insulin unless there is evidence of **diabetic ketoacidosis** or **hyperosmolar hyperglycemic state**, or persistent severe hyperglycemia.
- More moderate hyperglycemia can often be managed with subcutaneous insulin or diet in the acute phase, and focuses remain on cardiac stabilization.
*Intravenous nitroglycerin*
- Intravenous nitroglycerin is indicated for ongoing ischemic chest pain or uncontrolled hypertension in ACS, but the patient's pain has subsided and he is **hypotensive** (91/60 mm Hg).
- Administering more nitroglycerin would likely worsen his hypotension and could compromise coronary perfusion.
Secondary prevention US Medical PG Question 5: A 56-year-old woman comes to the physician for follow-up after a measurement of elevated blood pressure at her last visit three months ago. She works as a high school teacher at a local school. She says that she mostly eats cafeteria food and take-out. She denies any regular physical activity. She does not smoke or use any recreational drugs. She drinks 2 to 3 glasses of wine per day. She has hypercholesterolemia for which she takes atorvastatin. Her height is 165 cm (5 ft 5 in), weight is 82 kg (181 lb), and BMI is 30.1 kg/m2. Her pulse is 67/min, respirations are 18/min, and blood pressure is 152/87 mm Hg on the right arm and 155/92 mm Hg on the left arm. She would like to try lifestyle modifications to improve her blood pressure before considering pharmacologic therapy. Which of the following lifestyle modifications is most likely to result in the greatest reduction of this patient's systolic blood pressure?
- A. Walking for 30 minutes, 5 days per week
- B. Reducing sodium intake to less than 2.4 g per day
- C. Losing 15 kg (33 lb) of body weight (Correct Answer)
- D. Adopting a DASH diet
- E. Decreasing alcohol consumption to maximum of one drink per day
Secondary prevention Explanation: ***Losing 15 kg (33 lb) of body weight***
- **Weight reduction** is the most effective lifestyle modification for lowering blood pressure, correlating directly with the amount of weight lost.
- A loss of 15 kg (33 lb) in this patient, who is **obese (BMI 30.1)**, could significantly reduce her systolic blood pressure, potentially by 5-20 mmHg per 10 kg weight loss.
*Walking for 30 minutes, 5 days per week*
- Regular **aerobic physical activity** is beneficial for blood pressure reduction, typically resulting in a 4-9 mmHg decrease in systolic pressure.
- While helpful, the magnitude of reduction from exercise alone is generally less than that achieved with significant weight loss in an obese individual.
*Reducing sodium intake to less than 2.4 g per day*
- **Sodium restriction** is an effective strategy, often leading to a 2-8 mmHg reduction in systolic blood pressure.
- Given the patient's diet of cafeteria and take-out food, high sodium intake is likely, making this a relevant intervention, but typically less impactful than substantial weight loss.
*Adopting a DASH diet*
- The **Dietary Approaches to Stop Hypertension (DASH) diet** emphasizes fruits, vegetables, and low-fat dairy, and can significantly lower blood pressure, by 8-14 mmHg.
- This diet is highly effective, but for an obese individual, the blood pressure reduction from achieving a healthy weight is often greater.
*Decreasing alcohol consumption to maximum of one drink per day*
- Reducing **excessive alcohol intake** can decrease systolic blood pressure by 2-4 mmHg, as the patient reports 2-3 glasses of wine daily.
- While beneficial, this reduction is likely to be less substantial compared to major weight loss or other dietary changes.
Secondary prevention US Medical PG Question 6: A 69-year-old man is brought by his son to the emergency department with weakness in his right arm and leg. The man insists that he is fine and blames his son for "creating panic". Four hours ago the patient was having tea with his wife when he suddenly dropped his teacup. He has had difficulty moving his right arm since then and cannot walk because his right leg feels stuck. He has a history of hypertension and dyslipidemia, for which he currently takes lisinopril and atorvastatin, respectively. He is allergic to aspirin and peanuts. A computerized tomography (CT) scan shows evidence of an ischemic stroke. Which medication would most likely prevent such attacks in this patient in the future?
- A. Celecoxib
- B. Abciximab
- C. Urokinase
- D. Clopidogrel (Correct Answer)
- E. Alteplase
Secondary prevention Explanation: ***Clopidogrel***
- This patient has suffered an **ischemic stroke** and has a **contraindication to aspirin** due to allergy. **Clopidogrel**, an **alternative antiplatelet agent**, is the most appropriate long-term secondary prevention medication to reduce the risk of future thrombotic events.
- As a **P2Y12 inhibitor**, clopidogrel prevents platelet aggregation, thereby reducing the likelihood of clot formation in patients at high risk for cardiovascular events.
*Celecoxib*
- **Celecoxib** is a **COX-2 selective NSAID** primarily used for pain and inflammation. It has no role in the prevention of ischemic stroke.
- While NSAIDs can have antiplatelet effects through COX-1 inhibition, **COX-2 selective inhibitors like celecoxib generally have a prothrombotic effect** and are not indicated for stroke prevention.
*Abciximab*
- **Abciximab** is a **glycoprotein IIb/IIIa inhibitor** that potently prevents platelet aggregation. It is typically used in acute settings, such as during percutaneous coronary intervention (PCI), and not for long-term stroke prevention.
- Its potent antiplatelet effect and **risk of bleeding** make it unsuitable for chronic outpatient management.
*Urokinase*
- **Urokinase** is a **thrombolytic agent** used to dissolve existing blood clots in acute conditions like pulmonary embolism or acute myocardial infarction. It is not indicated for the prevention of future ischemic strokes.
- Thrombolytics carry a **significant risk of hemorrhage** and are solely for acute clot lysis, not chronic prevention.
*Alteplase*
- **Alteplase** is a **tissue plasminogen activator (tPA)**, a thrombolytic used in the **acute treatment of ischemic stroke** within a specific time window to dissolve clots and restore blood flow.
- It is an **acute rescue therapy** and is not used for long-term secondary prevention of stroke due to its high bleeding risk and short duration of action.
Secondary prevention US Medical PG Question 7: A 73-year-old man presents to the outpatient clinic complaining of chest pain with exertion. He states that resting for a few minutes usually resolves the chest pain. Currently, he takes 81 mg of aspirin daily. He has a blood pressure of 127/85 mm Hg and heart rate of 75/min. Physical examination reveals regular heart sounds and clear lung sounds bilateral. Which medication regimen below should be added?
- A. Metoprolol and a statin daily. Sublingual nitroglycerin as needed. (Correct Answer)
- B. Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.
- C. Amlodipine and a statin daily. Sublingual nitroglycerin as needed.
- D. Amlodipine daily. Sublingual nitroglycerin as needed.
- E. Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.
Secondary prevention Explanation: ***Metoprolol and a statin daily. Sublingual nitroglycerin as needed.***
- This patient presents with symptoms consistent with **stable angina** (**chest pain with exertion, relieved by rest**). The recommended medical therapy includes **antiplatelet agents** (aspirin, already prescribed), **beta-blockers** (metoprolol) for symptom control and improved survival post-MI, and **high-intensity statins** for lipid management and plaque stabilization. **Sublingual nitroglycerin** is crucial for acute symptom relief.
- Beta-blockers like metoprolol decrease myocardial **oxygen demand** by reducing heart rate and contractility, effectively treating angina. Statins are essential for **atherosclerosis management**.
*Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.*
- While clopidogrel is an **antiplatelet agent**, aspirin is typically the first-line choice for stable angina unless there's an intolerance or compelling reason for dual antiplatelet therapy (e.g., recent stent placement), which is not indicated here.
- Amlodipine, a **calcium channel blocker**, can be used for angina but is usually a second-line agent if beta-blockers are contraindicated or insufficient; it doesn't offer the mortality benefit seen with beta-blockers post-MI.
*Amlodipine and a statin daily. Sublingual nitroglycerin as needed.*
- This regimen includes a **statin** and sublingual nitroglycerin, which are appropriate. However, it uses amlodipine instead of a beta-blocker, which is generally the preferred initial therapy for angina due to its benefits in reducing myocardial oxygen demand and improving outcomes, especially in patients with a history of MI or heart failure.
- Beta-blockers provide superior **mortality reduction benefits** in patients with coronary artery disease compared to calcium channel blockers.
*Amlodipine daily. Sublingual nitroglycerin as needed.*
- This option misses two critical components of comprehensive treatment for stable angina: a **statin** for lipid management and plaque stabilization, and a **beta-blocker** for primary symptom control and long-term cardiac protection.
- Relying solely on amlodipine and sublingual nitroglycerin would leave the patient incompletely treated for their underlying **coronary artery disease**.
*Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.*
- This option lacks a **statin**, which is a cornerstone of therapy for stable angina to manage atherosclerosis.
- While metoprolol is appropriate and ranolazine can be used as an add-on therapy for refractory angina, it's not typically a first-line agent and doesn't replace the need for a statin.
Secondary prevention US Medical PG Question 8: A 60-year-old man presents to the emergency department with progressive dyspnea for the last 3 weeks. He complains of shortness of breath while lying flat and reports nighttime awakenings due to shortness of breath for the same duration. The patient has been a smoker for the last 30 years. Past medical history is significant for myocardial infarction 7 months ago. Current medications include metoprolol, aspirin, and rosuvastatin, but the patient is noncompliant with his medications. His temperature is 37.2°C (98.9°F), the blood pressure is 150/115 mm Hg, the pulse is 110/min, and the respiratory rate is 24/min. Oxygen saturation on room air is 88%. Chest auscultation reveals bilateral crackles and an S3 gallop. On physical examination, the cardiac apex is palpated in left 6th intercostal space. Bilateral pitting edema is present, and the patient is in moderate distress. Which of the following is the best next step in the management of the patient?
- A. Intravenous beta blockers
- B. Intravenous diuretics (Correct Answer)
- C. Echocardiography
- D. Cardiac stress testing
- E. Intravenous inotropes
Secondary prevention Explanation: ***Intravenous diuretics***
- The patient presents with classic signs and symptoms of **acute decompensated heart failure**, such as progressive dyspnea, orthopnea, paroxysmal nocturnal dyspnea, bilateral crackles, S3 gallop, pitting edema, and elevated blood pressure with elevated heart rate due to fluid overload.
- **Intravenous loop diuretics** (e.g., furosemide) are the most appropriate initial therapy to reduce preload, alleviate pulmonary and systemic congestion, and improve oxygenation.
*Intravenous beta blockers*
- While beta-blockers are a cornerstone of chronic heart failure management, **starting or acutely increasing beta-blocker dosage in acute decompensated heart failure** can worsen cardiac output and lead to symptomatic hypotension or cardiogenic shock.
- Beta-blockers should generally be withheld or reduced during acute exacerbations and reinstituted once the patient is stable.
*Echocardiography*
- While an **echocardiogram** is essential for diagnosing the underlying cause and assessing cardiac function in heart failure, it is not the *best next step* in a patient presenting with acute, severe symptoms requiring immediate stabilization.
- The patient's acute respiratory distress and hypoxemia necessitate immediate medical intervention to reduce fluid overload before detailed diagnostic imaging.
*Cardiac stress testing*
- **Cardiac stress testing** is used to evaluate for inducible ischemia in stable patients and is not appropriate in the setting of acute decompensated heart failure.
- Performing a stress test on a patient with signs of fluid overload and respiratory distress would be dangerous and could exacerbate their condition.
*Intravenous inotropes*
- **Intravenous inotropes** (e.g., dobutamine, milrinone) are typically reserved for patients with evidence of **cardiogenic shock** or severe heart failure with persistent hypoperfusion despite optimal fluid management and diuretic therapy.
- This patient, while acutely ill, primarily exhibits signs of fluid overload without clear evidence of severe hypoperfusion compromising end-organ function.
Secondary prevention US Medical PG Question 9: A 54-year-old man with alcoholism comes to the emergency department because of vomiting blood for 6 hours. He has had 3–4 episodes in which he has vomited dark red blood during this period. He has had no epigastric pain or tarry stools. On arrival, his temperature is 37.3°C (99.1°F), pulse is 134/min, and blood pressure is 80/50 mm Hg. He is resuscitated with 0.9% saline and undergoes an emergency upper endoscopy, which shows actively bleeding varices. Band ligation of the varices is done and hemostasis is achieved. He is diagnosed with Child class B cirrhosis. He is concerned about the possibility of recurrence of such an episode. He is asked to abstain from alcohol, to which he readily agrees. In addition to non-selective beta-blocker therapy, which of the following is the most appropriate recommendation to prevent future morbidity and mortality from this condition?
- A. Terlipressin
- B. Transjugular intrahepatic portosystemic shunt
- C. Variceal sclerotherapy
- D. Variceal ligation (Correct Answer)
- E. Octreotide therapy
Secondary prevention Explanation: ***Variceal ligation***
- **Endoscopic variceal ligation (EVL) is the gold standard for secondary prophylaxis** (preventing re-bleeding) in patients who have already experienced a variceal hemorrhage.
- It involves placing elastic bands on varices to occlude them, leading to fibrosis and eradication of the varices.
*Terlipressin*
- **Terlipressin is a vasoconstrictor primarily used to control acute variceal bleeding**, not for long-term secondary prevention.
- It reduces portal pressure by causing splanchnic vasoconstriction but is not suitable for chronic management.
*Transjugular intrahepatic portosystemic shunt*
- **TIPS is typically reserved for patients who fail endoscopic and pharmacological therapies** or have refractory ascites.
- While effective in reducing portal pressure, it carries risks such as **hepatic encephalopathy** and is not the first-line secondary prevention strategy.
*Variceal sclerotherapy*
- **Variceal sclerotherapy involves injecting a sclerosant solution into or adjacent to varices to induce thrombosis and fibrosis.**
- It is an alternative to band ligation but is generally **less preferred for secondary prophylaxis due to a higher rate of complications** like esophageal ulceration and re-bleeding.
*Octreotide therapy*
- **Octreotide, a somatostatin analog, is used to reduce splanchnic blood flow and portal pressure during acute variceal bleeding episodes.**
- It is **not recommended for long-term secondary prophylaxis** and is typically used in conjunction with endoscopic therapy for acute management.
Secondary prevention US Medical PG Question 10: A 68-year-old man presents to your office concerned about the frequency with which he wakes up in the middle night feeling out of breath. He has been required to use 3 more pillows in order to reduce the shortness of breath. In addition to this, he has noticed that he tires easily with minor tasks such as walking 1 block, and more recently when he is dressing up in the mornings. Physical examination reveals a blood pressure of 120/85 mm Hg, heart rate of 82/min, respiratory rate of 20/min, and body temperature of 36.0°C (98.0°F). Cardiopulmonary examination reveals regular and rhythmic heart sounds with S4 gallop, a laterally displaced point of maximum impulse (PMI), and rales in both lung bases. He also presents with prominent hepatojugular reflux, orthopnea, and severe lower limb edema. Which of the following changes would be seen in this patient’s heart?
- A. Decreased expression of metalloproteinases
- B. Decreased collagen synthesis
- C. Increased production of brain natriuretic peptide (Correct Answer)
- D. Cardiomyocyte hyperplasia
- E. Increased nitric oxide bioactivity
Secondary prevention Explanation: ***Increased production of brain natriuretic peptide***
- The patient's symptoms (orthopnea, dyspnea on exertion, S4 gallop, rales, edema, hepatojugular reflux) are classic for **congestive heart failure**.
- In heart failure, the **ventricular cardiomyocytes** are stretched due to increased volume and pressure, leading to the compensatory release of **BNP** to promote vasodilation and diuresis.
*Decreased expression of metalloproteinases*
- **Matrix metalloproteinases (MMPs)** are often **upregulated** in heart failure, contributing to adverse cardiac remodeling, not decreased expression.
- Their increased activity promotes degradation of the extracellular matrix, further impairing cardiac function.
*Decreased collagen synthesis*
- In heart failure, there is often an **initial compensatory increase in collagen synthesis** and deposition, leading to **fibrosis** and increased myocardial stiffness.
- While chronic heart failure can lead to complex remodeling, a primary decrease in collagen synthesis is not the typical response.
*Cardiomyocyte hyperplasia*
- **Cardiomyocytes** are terminally differentiated cells with very limited proliferative capacity in adults; therefore, **hyperplasia** (increase in cell number) is not a significant mechanism of response to increased workload in heart failure.
- Instead, the heart typically responds through **cardiomyocyte hypertrophy** (increase in cell size) and fibrosis.
*Increased nitric oxide bioactivity*
- In heart failure, **endothelial dysfunction** is common, leading to **reduced nitric oxide (NO) bioavailability** rather than increased bioactivity.
- Reduced NO bioactivity contributes to increased vascular resistance and impaired vasodilation, exacerbating heart failure.
More Secondary prevention US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.