Risk stratification in ACS US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Risk stratification in ACS. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Risk stratification in ACS US Medical PG Question 1: A 28-year-old male presents with sharp, stabbing chest pain that worsens when lying flat and improves when sitting forward. He reports a recent viral upper respiratory infection 2 weeks ago. On examination, a friction rub is heard on auscultation. His vital signs are stable.
An ECG is most likely to show which of the following findings in this patient?
- A. Diffuse, concave ST-segment elevations (Correct Answer)
- B. Peaked T waves and ST-segment elevations in leads V1-V6
- C. Sawtooth-appearance of P waves
- D. S waves in lead I, Q waves in lead III, and inverted T waves in lead III
- E. Alternating high and low amplitude QRS complexes
Risk stratification in ACS Explanation: ***Diffuse, concave ST-segment elevations***
- This is a hallmark ECG finding in **acute pericarditis**, along with **PR segment depression**, due to widespread inflammation of the epicardium.
- The chest pain described here (sharp, stabbing, worse when lying flat, improved by sitting forward) paired with a recent viral infection and a pericardial friction rub, is highly characteristic of **pericarditis**.
*Peaked T waves and ST-segment elevations in leads V1-V6*
- **Peaked T waves** are typically seen in early stages of hyperkalemia or myocardial ischemia, while **ST-segment elevations in specific leads (V1-V6)** are more indicative of an **ST-elevation myocardial infarction (STEMI)** involving the anterior wall.
- The diffuse nature of ST elevation in pericarditis, as opposed to regional changes, along with **PR depression**, differentiates it from STEMI.
*Sawtooth-appearance of P waves*
- A **sawtooth appearance of P waves** (often referred to as 'f waves') is characteristic of **atrial flutter**, a type of supraventricular tachycardia.
- This finding is unrelated to pericarditis, which primarily affects the pericardium and not the atrial electrical activity in this specific manner.
*S waves in lead I, Q waves in lead III, and inverted T waves in lead III*
- This pattern, known as the **S1Q3T3 pattern**, is a classic (though not always present) ECG finding suggestive of **acute pulmonary embolism**.
- While pulmonary embolism can cause chest pain, its presentation differs significantly from the positional relief and friction rub seen in pericarditis.
*Alternating high and low amplitude QRS complexes*
- This ECG finding, known as **electrical alternans**, is highly specific for a large **pericardial effusion** or **cardiac tamponade**, where the heart swings within the fluid-filled pericardial sac.
- Although pericarditis can lead to effusion, the presence of a friction rub and stable vital signs suggests acute pericarditis without significant tamponade at this stage, making diffuse ST elevation a more likely initial finding.
Risk stratification in ACS US Medical PG Question 2: Group of 100 medical students took an end of the year exam. The mean score on the exam was 70%, with a standard deviation of 25%. The professor states that a student's score must be within the 95% confidence interval of the mean to pass the exam. Which of the following is the minimum score a student can have to pass the exam?
- A. 45%
- B. 63.75%
- C. 67.5%
- D. 20%
- E. 65% (Correct Answer)
Risk stratification in ACS Explanation: ***65%***
- To find the **95% confidence interval (CI) of the mean**, we use the formula: Mean ± (Z-score × Standard Error). For a 95% CI, the Z-score is approximately **1.96**.
- The **Standard Error (SE)** is calculated as SD/√n, where n is the sample size (100 students). So, SE = 25%/√100 = 25%/10 = **2.5%**.
- The 95% CI is 70% ± (1.96 × 2.5%) = 70% ± 4.9%. The lower bound is 70% - 4.9% = **65.1%**, which rounds to **65%** as the minimum passing score.
*45%*
- This value is significantly lower than the calculated lower bound of the 95% confidence interval (approximately 65.1%).
- It would represent a score far outside the defined passing range.
*63.75%*
- This value falls below the calculated lower bound of the 95% confidence interval (approximately 65.1%).
- While close, this score would not meet the professor's criterion for passing.
*67.5%*
- This value is within the 95% confidence interval (65.1% to 74.9%) but is **not the minimum score**.
- Lower scores within the interval would still qualify as passing.
*20%*
- This score is extremely low and falls significantly outside the 95% confidence interval for a mean of 70%.
- It would indicate performance far below the defined passing threshold.
Risk stratification in ACS US Medical PG Question 3: Researchers are studying the relationship between heart disease and alcohol consumption. They review the electronic medical records of 500 patients at a local hospital during the study period and identify the presence or absence of acute coronary syndrome (ACS) and the number of alcoholic drinks consumed on the day of presentation. They find that there is a lower prevalence of acute coronary syndrome in patients who reported no alcohol consumption or 1 drink daily compared with those who reported 2 or more drinks. Which of the following is the most accurate description of this study type?
- A. Cross-sectional study
- B. Prospective study
- C. Randomized controlled trial
- D. Case-control study
- E. Retrospective study (Correct Answer)
Risk stratification in ACS Explanation: ***Retrospective study***
- This study **reviews electronic medical records** that were created in the past, making it retrospective by definition.
- Researchers looked **backward in time** during the study period to identify both the exposure (alcohol consumption) and outcome (ACS) from existing records.
- The key feature is that **data collection relies on pre-existing documentation** rather than prospectively following patients or collecting data at a single point in time.
- This is specifically a **retrospective cohort design** where researchers identified a population and assessed both exposure and outcome from historical records.
*Cross-sectional study*
- Cross-sectional studies collect data from participants at a **single point in time** through surveys, interviews, or direct assessment—not by reviewing past medical records.
- While this study assessed variables "at presentation," the **method of data collection** (reviewing electronic records retrospectively) makes it retrospective, not cross-sectional.
- Cross-sectional studies typically involve **active data collection** from living participants, not record review.
*Prospective study*
- A prospective study follows participants **forward in time** from exposure to outcome, recruiting them before outcomes develop.
- This study did not follow patients forward; it reviewed **records of events that already occurred**.
*Randomized controlled trial*
- An RCT involves **intervention and randomization** of participants to different treatment groups.
- This is an observational study with no intervention or randomization.
*Case-control study*
- A case-control study first identifies **cases (with disease)** and **controls (without disease)**, then looks backward to compare exposures.
- This study did not select participants based on disease status first; it reviewed a general hospital population and assessed both variables simultaneously from records.
Risk stratification in ACS US Medical PG Question 4: A 60-year-old woman presents to the emergency room with chest pain that started 20 minutes ago while watching television at home. The pain is substernal and squeezing in nature. She rates the pain as 6/10 and admits to having similar pain in the past with exertion. Her past medical history is significant for diabetes mellitus that is controlled with metformin. The physical examination is unremarkable. An electrocardiogram (ECG) shows ST-segment depression in the lateral leads. She is started on aspirin, nitroglycerin, metoprolol, unfractionated heparin, and insulin. She is asked not to take metformin while at the hospital. Three sets of cardiac enzymes are negative.
Lab results are given below:
Serum glucose 88 mg/dL
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 1.2 mg/dL
Blood urea nitrogen 22 mg/dL
Cholesterol, total 170 mg/dL
HDL-cholesterol 40 mg/dL
LDL-cholesterol 80 mg/dL
Triglycerides 170 mg/dL
Hematocrit 38%
Hemoglobin 13 g/dL
Leucocyte count 7,500/mm3
Platelet count 185,000 /mm3
Activated partial thromboplastin time (aPTT) 30 seconds
Prothrombin time (PT) 12 seconds
Urinalysis
Glucose negative
Ketones negative
Leucocytes negative
Nitrites negative
Red blood cells (RBC) negative
Casts negative
An echocardiogram reveals left ventricular wall motion abnormalities. With the pain subsiding, she was admitted and the medications were continued. A coronary angiography is planned in 4 days. In addition to regular blood glucose testing, which of the following should be closely monitored in this patient?
- A. Activated partial thromboplastin time (aPTT) alone
- B. Prothrombin time alone
- C. aPTT and platelet count (Correct Answer)
- D. Platelet count alone
- E. Prothrombin time and platelet count
Risk stratification in ACS Explanation: ***aPTT and platelet count***
- The patient is receiving **unfractionated heparin**, which requires monitoring of **aPTT** to ensure therapeutic anticoagulation and prevent bleeding complications.
- Heparin can also induce **heparin-induced thrombocytopenia (HIT)**, necessitating close monitoring of the **platelet count**.
*Activated partial thromboplastin time (aPTT) alone*
- While **aPTT** monitoring is crucial for unfractionated heparin, it does not account for the risk of **heparin-induced thrombocytopenia (HIT)**.
- Monitoring platelet count is equally important alongside aPTT in patients receiving heparin.
*Prothrombin time alone*
- **Prothrombin time (PT)** is used to monitor **warfarin** therapy, not unfractionated heparin.
- Monitoring PT in this context would be inappropriate and would not provide information about the efficacy or safety of the prescribed heparin.
*Platelet count alone*
- Monitoring **platelet count** is important for detecting **heparin-induced thrombocytopenia (HIT)**, but it does not assess the therapeutic effect of heparin.
- **aPTT** monitoring is essential to ensure adequate anticoagulation and prevent thrombotic events.
*Prothrombin time and platelet count*
- **Prothrombin time (PT)** is irrelevant for unfractionated heparin monitoring, as it measures the extrinsic pathway and is used for warfarin.
- Although **platelet count** monitoring is important, relying on PT is incorrect for unfractionated heparin management.
Risk stratification in ACS US Medical PG Question 5: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Risk stratification in ACS Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
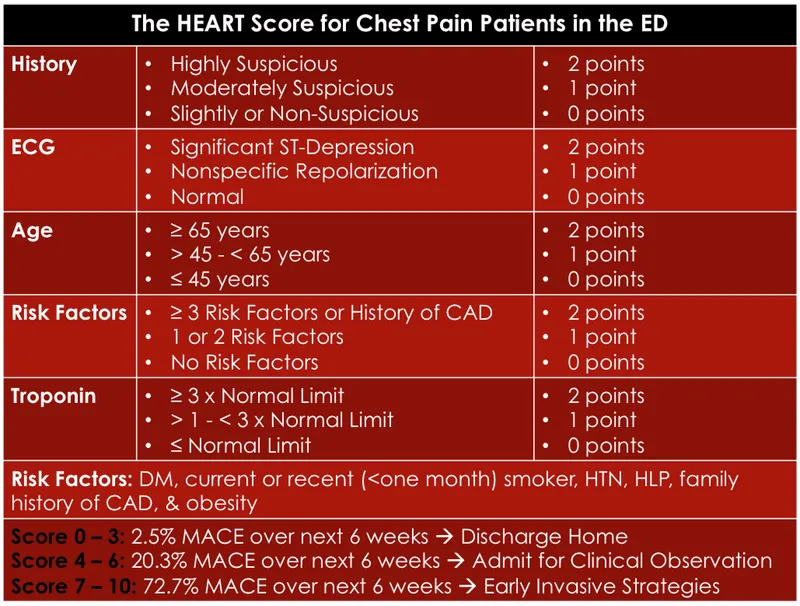
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
Risk stratification in ACS US Medical PG Question 6: A 56-year-old man presents to the emergency room with severe substernal chest pain associated with a 2-hour history of breathlessness and sweating. An electrocardiogram shows an ST-segment elevation myocardial infarction. Cardiac enzyme levels confirm a diagnosis of acute myocardial infarction. The patient is rushed to the catheter lab for angioplasty with stenting. The patient complains of recurrent chest pain in the ICU 56 hours post-angioplasty. Which of the following enzymes facilitates the patient’s diagnosis based on his current symptoms?
- A. Creatine kinase (CK)-MB (Correct Answer)
- B. Creatine kinase – MM
- C. Troponin T
- D. Troponin I
- E. Lactate dehydrogenase (LDH)
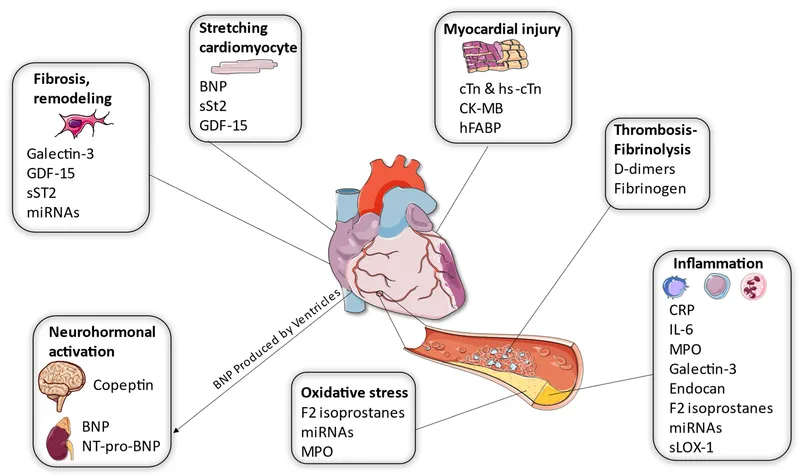
Risk stratification in ACS Explanation: ***Creatine kinase (CK)-MB***
- **CK-MB** is elevated in myocardial infarction, rising within 4-6 hours, peaking at 24 hours, and **returning to baseline within 48-72 hours** after the initial event.
- At **56 hours post-angioplasty**, CK-MB levels should have normalized from the initial MI, making a **new elevation highly specific** for reinfarction or new myocardial injury.
- This makes CK-MB particularly useful for detecting **early reinfarction** when the timing allows it to have cleared from the initial event.
- **Clinical pearl**: This represents classical teaching about cardiac enzyme kinetics, though modern practice increasingly uses serial troponin measurements with delta criteria.
*Creatine kinase – MM*
- **CK-MM** is the predominant isoform of creatine kinase found in **skeletal muscle**, not cardiac muscle.
- While total CK (which includes CK-MM) increases in MI, CK-MM elevation is **not specific to cardiac injury** and can be elevated from skeletal muscle damage or other causes.
- Its lack of cardiac specificity makes it a **poor indicator for myocardial reinfarction**.
*Troponin T*
- **Troponin T** is highly sensitive and specific for myocardial injury, but levels remain **elevated for 7-10 days** following an acute MI.
- At 56 hours post-angioplasty, troponin T would **still be elevated from the initial MI**, making it difficult to distinguish baseline elevation from a new acute event.
- While a **significant rise (>20%) from the previous value** can indicate reinfarction, the persistently elevated baseline makes interpretation more complex compared to CK-MB which should have normalized.
*Troponin I*
- **Troponin I** remains elevated for **5-7 days** following an acute MI, similar to troponin T.
- At 56 hours post-initial MI, troponin I levels would **still be elevated**, making it challenging to clearly identify a new ischemic event without comparing to prior values.
- Though troponins are the **gold standard for MI diagnosis**, their prolonged elevation window makes CK-MB more straightforward for detecting reinfarction at this specific timepoint (when CK-MB should have returned to baseline).
*Lactate dehydrogenase (LDH)*
- **LDH** elevation occurs later in MI (24-48 hours after onset) and remains elevated for **10-14 days**.
- Due to its **delayed rise and prolonged elevation**, LDH is not useful for diagnosing acute reinfarction in the early post-MI period.
- LDH lacks the rapid kinetics and cardiac specificity needed for timely diagnosis of new myocardial injury.
Risk stratification in ACS US Medical PG Question 7: A 69-year-old man is scheduled to undergo radical retropubic prostatectomy for prostate cancer in 2 weeks. He had a myocardial infarction at the age of 54 years. He has a history of GERD, unstable angina, hyperlipidemia, and severe osteoarthritis in the left hip. He is unable to climb up stairs or walk fast because of pain in his left hip. He had smoked one pack of cigarettes daily for 30 years but quit 25 years ago. He drinks one glass of wine daily. Current medications include aspirin, metoprolol, lisinopril, rosuvastatin, omeprazole, and ibuprofen as needed. His temperature is 36.4°C (97.5°F), pulse is 90/min, and blood pressure is 136/88 mm Hg. Physical examination shows no abnormalities. A 12-lead ECG shows Q waves and inverted T waves in leads II, III, and aVF. His B-type natriuretic protein is 84 pg/mL (N < 125). Which of the following is the most appropriate next step in management to assess this patient's perioperative cardiac risk?
- A. No further testing
- B. 24-hour ambulatory ECG monitoring
- C. Radionuclide myocardial perfusion imaging (Correct Answer)
- D. Treadmill stress test
- E. Resting echocardiography
Risk stratification in ACS Explanation: ***Radionuclide myocardial perfusion imaging***
- This patient requires **perioperative cardiac risk assessment** before intermediate-risk surgery (radical prostatectomy).
- Key factors include: history of **myocardial infarction**, current cardiac risk factors, and **inability to exercise** due to severe osteoarthritis.
- Since he cannot perform exercise stress testing, **pharmacologic stress testing** with radionuclide myocardial perfusion imaging (using agents like adenosine, dipyridamole, or regadenoson) is the most appropriate test to assess for **inducible myocardial ischemia**.
- This provides functional assessment of coronary perfusion under pharmacologic stress, helping guide perioperative risk stratification and management.
- *Note: The presence of unstable angina would typically require cardiac stabilization first; this question focuses on selecting the appropriate stress test modality for a patient unable to exercise.*
*No further testing*
- This patient has significant cardiac risk factors including **prior MI**, ongoing cardiac medications, and ECG changes suggesting old infarction.
- Proceeding directly to surgery without functional cardiac assessment would be **inappropriate** given his risk profile and the intermediate-risk nature of the planned surgery.
*24-hour ambulatory ECG monitoring*
- Holter monitoring detects arrhythmias and silent ischemic episodes but does not provide **functional capacity assessment** or evaluation of inducible ischemia under stress conditions.
- It is not the primary tool for **perioperative cardiac risk stratification** before major surgery.
*Treadmill stress test*
- The patient's **severe osteoarthritis** prevents him from climbing stairs or walking fast, making him unable to achieve adequate exercise workload for a treadmill stress test.
- This functional limitation makes **exercise stress testing contraindicated**; pharmacologic stress testing is required instead.
*Resting echocardiography*
- Resting echocardiography assesses **baseline left ventricular function**, wall motion abnormalities from prior infarction, and valvular disease.
- While useful for structural assessment, it does **not evaluate for exercise-induced or stress-induced ischemia**, which is critical for perioperative risk assessment in patients with coronary artery disease.
- His normal BNP (84 pg/mL) suggests adequate baseline ventricular function, making functional ischemia assessment more relevant than structural evaluation alone.
Risk stratification in ACS US Medical PG Question 8: Two days after undergoing an uncomplicated total thyroidectomy, a 63-year-old woman has acute, progressive chest pain. The pain is sharp and burning. She feels nauseated and short of breath. The patient has a history of hypertension, type 1 diabetes mellitus, medullary thyroid cancer, multiple endocrine neoplasia type 2A, anxiety, coronary artery disease, and gastroesophageal reflux disease. She smoked half a pack of cigarettes daily for 24 years but quit 18 years ago. Current medications include lisinopril, insulin glargine, insulin aspart, sertraline, aspirin, ranitidine, and levothyroxine. She appears anxious and diaphoretic. Her temperature is 37.4°C (99.3°F), pulse is 64/min, respirations are 17/min, and blood pressure is 148/77 mm Hg. The lungs are clear to auscultation. Examination shows a 3-cm linear incision over the anterior neck with 1 mm of surrounding erythema and mild serous discharge. The chest wall and abdomen are nontender. There is 5/5 strength in all extremities and decreased sensation to soft touch on the feet bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Obtain an ECG and troponin T levels (Correct Answer)
- B. Administer IV pantoprazole and schedule endoscopy
- C. Discontinue levothyroxine and obtain fT4 levels
- D. Administer IV levofloxacin and obtain chest radiograph
- E. Obtain urine and plasma metanephrine levels
Risk stratification in ACS Explanation: **Obtain an ECG and troponin T levels**
- The patient presents with acute, progressive **chest pain that is sharp and burning**, along with nausea and shortness of breath, which are classic symptoms of an acute coronary syndrome, especially given her history of **coronary artery disease**, hypertension, diabetes, and prior smoking.
- An **ECG** and **troponin T levels** are crucial first steps to evaluate for myocardial ischemia or infarction in this high-risk patient.
*Administer IV pantoprazole and schedule endoscopy*
- While the patient has a history of gastroesophageal reflux disease (GERD) and her pain is described as "burning," the **acuteness, progression, and associated symptoms** (nausea, shortness of breath) in a patient with significant cardiac risk factors make a GI cause less likely as the primary concern.
- Empiric treatment for GERD without first ruling out a life-threatening cardiac event would be inappropriate and potentially dangerous.
*Discontinue levothyroxine and obtain fT4 levels*
- The patient is taking levothyroxine after a thyroidectomy for medullary thyroid cancer, but there is no immediate indication of thyroid hormone imbalance (e.g., hyperthyroidism causing chest pain) that would warrant discontinuing her medication or rushing fT4 levels as the first step in an acute chest pain presentation.
- Her pulse of 64/min is not suggestive of hyperthyroidism, which typically causes tachycardia.
*Administer IV levofloxacin and obtain chest radiograph*
- While shortness of breath can be a symptom of pneumonia, the **sharp, burning nature of the chest pain**, coupled with the absence of fever (temperature 37.4°C is mild), cough, or abnormal lung sounds (lungs clear to auscultation), makes an acute infection like pneumonia less probable as the primary diagnosis.
- Antibiotics and a chest radiograph would be considered after ruling out more immediate life-threatening conditions like acute coronary syndrome.
*Obtain urine and plasma metanephrine levels*
- The patient has a history of multiple endocrine neoplasia type 2A (MEN2A), which includes medullary thyroid cancer and can be associated with pheochromocytoma (adrenal tumor secreting catecholamines). However, her blood pressure (148/77 mm Hg) is not acutely elevated to crisis levels, and her symptoms are more consistent with cardiac ischemia than a pheochromocytoma crisis.
- While metanephrine levels would be important for long-term follow-up of MEN2A, they are not the immediate next step for acute chest pain in a patient with known coronary artery disease.
Risk stratification in ACS US Medical PG Question 9: A 67-year-old man presents to the emergency department for squeezing and substernal chest pain. He states that he was at home eating dinner when his symptoms began. The patient has a past medical history of diabetes, hypertension, and dyslipidemia. He is currently taking atorvastatin, lisinopril, insulin, metformin, metoprolol, and aspirin. Six days ago he underwent percutaneous coronary intervention. His temperature is 99.5°F (37.5°C), blood pressure is 197/118 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals an uncomfortable elderly man who is sweating. An ECG is ordered. Which of the following is the best next step in management for this patient?
- A. Stress testing
- B. Angiography (Correct Answer)
- C. Cardiac troponins
- D. Creatine kinase-MB
- E. Myoglobin
Risk stratification in ACS Explanation: ***Correct: Angiography***
- This patient presenting with **acute chest pain 6 days post-PCI** is at high risk for **stent thrombosis or acute in-stent restenosis**, which represents a life-threatening emergency.
- Given the **clinical instability** (severe hypertension 197/118, tachycardia 120/min, diaphoresis) and classic ACS symptoms in the immediate post-PCI period, **urgent coronary angiography** is the best next step in management.
- While ECG and troponins are important diagnostic tools, this patient requires **immediate intervention** to evaluate the recent PCI site and potentially perform emergent revascularization.
- In the setting of suspected **acute stent thrombosis**, time to reperfusion is critical, and angiography allows both diagnosis and treatment.
*Incorrect: Cardiac troponins*
- While troponins are essential biomarkers for myocardial injury and should be obtained, they are a **diagnostic test** rather than definitive management.
- Waiting for troponin results would delay definitive management in a patient with clear clinical evidence of ACS.
- In this high-risk post-PCI patient with active symptoms, management should not wait for biomarker confirmation.
*Incorrect: Stress testing*
- Stress testing is **absolutely contraindicated** in patients with active chest pain and suspected acute MI.
- It could precipitate further myocardial ischemia, arrhythmias, or cardiac arrest.
- Stress testing is reserved for risk stratification in stable patients or after ACS has been ruled out.
*Incorrect: Creatine kinase-MB*
- CK-MB is less sensitive and specific than troponins for myocardial injury, as it can be elevated in skeletal muscle conditions.
- It has a shorter elevation window and has largely been replaced by troponins in modern practice.
- Like troponins, it would not change the immediate management need in this clinically unstable patient.
*Incorrect: Myoglobin*
- Myoglobin lacks cardiac specificity (present in both cardiac and skeletal muscle) and has poor diagnostic accuracy for MI.
- Its rapid rise and fall make it unreliable, and it generates many false positives.
- It has no role in guiding management decisions in suspected ACS.
Risk stratification in ACS US Medical PG Question 10: A 25-year-old man comes to the emergency department because of a 1-week-history of progressively worsening dyspnea and intermittent chest pain that increases on inspiration. He had an upper respiratory tract infection 2 weeks ago. His pulse is 115/min and blood pressure is 100/65 mm Hg. Examination shows inspiratory crackles bilaterally. His serum troponin I is 0.21 ng/mL (N < 0.1). An x-ray of the chest shows an enlarged cardiac silhouette and prominent vascular markings in both lung fields; costophrenic angles are blunted. A rhythm strip shows inverted T waves. Which of the following additional findings is most likely in this patient's condition?
- A. Opening snap with low-pitched diastolic rumble
- B. Elevated brain natriuretic peptide (Correct Answer)
- C. Sarcomere duplication
- D. Right ventricular dilation
- E. Electrical alternans
Risk stratification in ACS Explanation: ***Elevated brain natriuretic peptide***
- This patient presents with symptoms of **dyspnea**, **chest pain**, **tachycardia**, elevated **troponin I**, an enlarged **cardiac silhouette** with prominent vascular markings, and **blunted costophrenic angles**, all consistent with **cardiomyopathy** and heart failure, likely post-viral **myocarditis**.
- **Brain natriuretic peptide (BNP)** is released by myocardial cells in response to ventricular stretch and volume overload, making it a strong indicator for **heart failure**.
*Opening snap with low-pitched diastolic rumble*
- An **opening snap** followed by a **low-pitched diastolic rumble** is characteristic of **mitral stenosis**, a valvular disorder not suggested by the patient's acute presentation and other findings.
- Mitral stenosis would typically be associated with a history of **rheumatic fever** and more specific echocardiographic findings of valve abnormalities.
*Sarcomere duplication*
- **Sarcomere duplication** and disarray are characteristic pathological findings in **hypertrophic cardiomyopathy (HCM)**, an inherited genetic disorder.
- While HCM can cause dyspnea and chest pain, this patient's acute presentation following a viral infection and evidence of fluid overload are more indicative of an **acquired cardiomyopathy** such as myocarditis.
*Right ventricular dilation*
- While the patient has signs of **heart failure**, the chest X-ray shows an **enlarged cardiac silhouette** and **prominent vascular markings in both lung fields** and **blunted costophrenic angles**, suggesting **left ventricular failure** with fluid redistribution and pleural effusions.
- Significant **right ventricular dilation** would typically be associated with signs of right-sided heart failure like **peripheral edema** and **jugular venous distension**, which are not explicitly mentioned as primary findings.
*Electrical alternans*
- **Electrical alternans** is a specific ECG finding characterized by beat-to-beat variation in the QRS amplitude or axis, most commonly associated with **pericardial effusion** leading to cardiac tamponade.
- Although the patient has an enlarged cardiac silhouette, which could indicate effusion, the primary findings point more broadly to **myocardial dysfunction** and **heart failure** rather than tamponade.
More Risk stratification in ACS US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.