Reperfusion strategies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Reperfusion strategies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
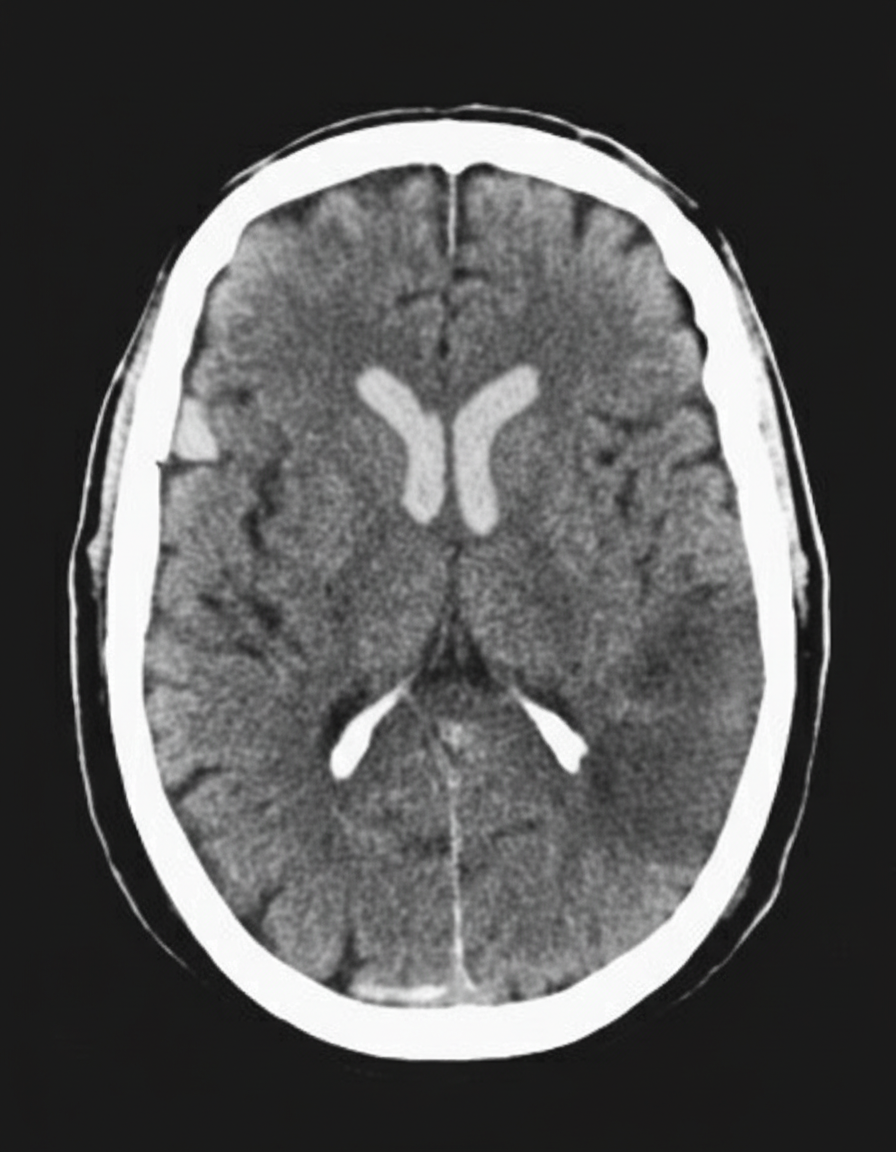
Reperfusion strategies US Medical PG Question 1: A 45-year-old man presents to the emergency department with complaints of right-sided weakness and slurring of speech for 1 hour. There is no history of head trauma, myocardial infarction, recent surgery, gastrointestinal or urinary bleeding. He has hypertension, chronic atrial fibrillation, and a 20 pack-year cigarette smoking history. The medication list includes valsartan and rivaroxaban. The vital signs include: blood pressure 180/92 mm Hg, pulse 144/min and irregular, and temperature 37.2°C (99.0°F). On physical examination, there is a facial asymmetry with a deviation of angle of mouth to the left side on smiling. Muscle strength is reduced in both upper and lower limbs on the right side while on the left side it’s normal. Random blood glucose is 104 mg/dL. A complete blood count is normal. A CT scan of the head is shown in the image. What is the most appropriate next step in the management of this patient?
- A. Heparin
- B. Amiodarone
- C. Metoprolol
- D. Tissue plasminogen activator
- E. Aspirin (Correct Answer)
Reperfusion strategies Explanation: ***Aspirin***
- The patient presents with acute onset **neurological deficits** (right-sided weakness, slurred speech) consistent with an **ischemic stroke** in the setting of **atrial fibrillation**.
- The CT scan shows no evidence of hemorrhage (hypodense or normal appearance), confirming **ischemic stroke**.
- While the patient is on **rivaroxaban**, the question addresses the **within-window acute management**. In the acute setting (within 1 hour of symptom onset), after ruling out hemorrhage on CT, **aspirin 325 mg** is considered as initial antiplatelet therapy for ischemic stroke.
- **Note:** Current guidelines suggest holding rivaroxaban temporarily and avoiding dual therapy (anticoagulation + antiplatelet) due to bleeding risk. However, aspirin remains the safest acute intervention among the choices provided for confirmed ischemic stroke.
*Tissue plasminogen activator (tPA)*
- **tPA** is the preferred thrombolytic for acute ischemic stroke **within 3-4.5 hours** of symptom onset.
- However, it is **absolutely contraindicated** in patients on **direct oral anticoagulants** (like rivaroxaban) due to **dramatically increased risk of intracranial hemorrhage** (up to 10-fold increase).
- Even with normal PT/INR, patients on DOACs cannot receive tPA safely without reversal agents.
*Heparin*
- **Heparin** provides additional anticoagulation on top of rivaroxaban, which would **significantly increase bleeding risk** (both intracranial and systemic).
- Not indicated in acute ischemic stroke management, especially when patient is already therapeutically anticoagulated.
- May be considered in specific scenarios (e.g., crescendo TIAs, arterial dissection) but not first-line here.
*Metoprolol*
- **Metoprolol** is a beta-blocker used for **rate control in atrial fibrillation** (patient has pulse 144/min - rapid ventricular response).
- While rate control is important, **acute blood pressure lowering in ischemic stroke can worsen cerebral perfusion** and extend the infarct.
- Current guidelines recommend **permissive hypertension** in acute stroke (allow BP up to 220/120 unless giving tPA).
- Rate control can be addressed after acute stroke management is initiated.
*Amiodarone*
- **Amiodarone** is an antiarrhythmic used for rhythm control in atrial fibrillation.
- Does **not treat the acute stroke** and is not indicated for emergency management of stroke.
- Rhythm control is not the priority in the acute stroke setting; the focus is on salvaging brain tissue and preventing further ischemia.
Reperfusion strategies US Medical PG Question 2: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Reperfusion strategies Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
Reperfusion strategies US Medical PG Question 3: A 54-year-old man is brought to the emergency department 1 hour after the sudden onset of shortness of breath, severe chest pain, and sweating. He has hypertension and type 2 diabetes mellitus. He has smoked one pack and a half of cigarettes daily for 20 years. An ECG shows ST-segment elevations in leads II, III, and avF. The next hospital with a cardiac catheterization unit is more than 2 hours away. Reperfusion pharmacotherapy is initiated. Which of the following is the primary mechanism of action of this medication?
- A. Conversion of plasminogen to plasmin (Correct Answer)
- B. Inhibition of glutamic acid residue carboxylation
- C. Blocking of adenosine diphosphate receptors
- D. Direct inhibition of thrombin activity
- E. Prevention of thromboxane formation
Reperfusion strategies Explanation: ***Conversion of plasminogen to plasmin***
- **Fibrinolytic** (thrombolytic) drugs, like **tissue plasminogen activator (tPA)**, work by converting plasminogen to plasmin, which then degrades the **fibrin mesh** of a **blood clot**.
- This action helps to **restore blood flow** in cases of ST-segment elevation myocardial infarction (STEMI) where primary **percutaneous coronary intervention (PCI)** is not immediately available.
*Inhibition of glutamic acid residue carboxylation*
- This is the mechanism of action of **warfarin**, an anticoagulant that inhibits the synthesis of **vitamin K-dependent clotting factors** (II, VII, IX, X, protein C, and protein S).
- While important for long-term anticoagulation, it does not provide immediate reperfusion in an acute STEMI.
*Blocking of adenosine diphosphate receptors*
- This describes the mechanism of action of **P2Y12 inhibitors** such as **clopidogrel**, **prasugrel**, and **ticagrelor**.
- These drugs are **antiplatelet agents** that prevent platelet aggregation, but they do not directly dissolve an existing thrombus to restore blood flow in STEMI.
*Direct inhibition of thrombin activity*
- This is the mechanism of action of **direct thrombin inhibitors** like **dabigatran** and **bivalirudin**.
- These drugs primarily prevent clot formation or extension and are not used as primary reperfusion agents for acute STEMI due to an existing occlusive thrombus.
*Prevention of thromboxane formation*
- This is the primary mechanism of action of **aspirin**, which irreversibly inhibits **cyclooxygenase-1 (COX-1)**, thereby reducing the production of thromboxane A2.
- Aspirin is an important antiplatelet drug in STEMI management but does not provide reperfusion by dissolving the clot.
Reperfusion strategies US Medical PG Question 4: A 67-year-old man presents to the emergency department for squeezing and substernal chest pain. He states that he was at home eating dinner when his symptoms began. The patient has a past medical history of diabetes, hypertension, and dyslipidemia. He is currently taking atorvastatin, lisinopril, insulin, metformin, metoprolol, and aspirin. Six days ago he underwent percutaneous coronary intervention. His temperature is 99.5°F (37.5°C), blood pressure is 197/118 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam reveals an uncomfortable elderly man who is sweating. An ECG is ordered. Which of the following is the best next step in management for this patient?
- A. Stress testing
- B. Angiography (Correct Answer)
- C. Cardiac troponins
- D. Creatine kinase-MB
- E. Myoglobin
Reperfusion strategies Explanation: ***Correct: Angiography***
- This patient presenting with **acute chest pain 6 days post-PCI** is at high risk for **stent thrombosis or acute in-stent restenosis**, which represents a life-threatening emergency.
- Given the **clinical instability** (severe hypertension 197/118, tachycardia 120/min, diaphoresis) and classic ACS symptoms in the immediate post-PCI period, **urgent coronary angiography** is the best next step in management.
- While ECG and troponins are important diagnostic tools, this patient requires **immediate intervention** to evaluate the recent PCI site and potentially perform emergent revascularization.
- In the setting of suspected **acute stent thrombosis**, time to reperfusion is critical, and angiography allows both diagnosis and treatment.
*Incorrect: Cardiac troponins*
- While troponins are essential biomarkers for myocardial injury and should be obtained, they are a **diagnostic test** rather than definitive management.
- Waiting for troponin results would delay definitive management in a patient with clear clinical evidence of ACS.
- In this high-risk post-PCI patient with active symptoms, management should not wait for biomarker confirmation.
*Incorrect: Stress testing*
- Stress testing is **absolutely contraindicated** in patients with active chest pain and suspected acute MI.
- It could precipitate further myocardial ischemia, arrhythmias, or cardiac arrest.
- Stress testing is reserved for risk stratification in stable patients or after ACS has been ruled out.
*Incorrect: Creatine kinase-MB*
- CK-MB is less sensitive and specific than troponins for myocardial injury, as it can be elevated in skeletal muscle conditions.
- It has a shorter elevation window and has largely been replaced by troponins in modern practice.
- Like troponins, it would not change the immediate management need in this clinically unstable patient.
*Incorrect: Myoglobin*
- Myoglobin lacks cardiac specificity (present in both cardiac and skeletal muscle) and has poor diagnostic accuracy for MI.
- Its rapid rise and fall make it unreliable, and it generates many false positives.
- It has no role in guiding management decisions in suspected ACS.
Reperfusion strategies US Medical PG Question 5: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Reperfusion strategies Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Reperfusion strategies US Medical PG Question 6: A 74-year-old man presents to the emergency department by paramedics for slurred speech and weakness in the left arm and leg for 1 hour. The patient was playing with his grandson when the symptoms started and his wife immediately called an ambulance. There is no history of head trauma or recent surgery. The patient takes captopril for hypertension. The vital signs include: pulse 110/min, respiratory rate 22/min, and blood pressure 200/105 mm Hg. The physical examination shows that the patient is alert and conscious, but speech is impaired. Muscle strength is 0/5 in the left arm and leg and 5/5 in the right arm and leg. A non-contrast CT of the head shows no evidence of intracranial bleeding. The lab results are as follows:
Serum glucose 90 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 1.3 mg/dL
Blood urea nitrogen 20 mg/dL
Cholesterol, total 240 mg/dL
HDL-cholesterol 38 mg/dL
LDL-cholesterol 100 mg/dL
Triglycerides 190 mg/dL
Hemoglobin (Hb%) 15.3 g/dL
Mean corpuscular volume (MCV) 83 fL
Reticulocyte count 0.8%
Erythrocyte count 5.3 million/mm3
Platelet count 130,000/mm3
Partial thromboplastin time (aPTT) 30 sec
Prothrombin time (PT) 12 sec
Although he is within the time frame for the standard therapy of the most likely condition, the treatment cannot be started because of which of the following contraindications?
- A. A platelet count of 130,000/mm3
- B. Age of 74 years
- C. Cholesterol level of 240 mg/dL
- D. Creatinine level of 1.3 mg/dL
- E. Systolic blood pressure of 200 mm Hg (Correct Answer)
Reperfusion strategies Explanation: ***Systolic blood pressure of 200 mm Hg***
- The patient presents with symptoms highly suggestive of an **acute ischemic stroke**, including **slurred speech** and **left-sided weakness**.
- For patients with acute ischemic stroke who are candidates for **thrombolytic therapy (e.g., alteplase)**, a **systolic blood pressure consistently >185 mm Hg or diastolic >110 mm Hg is a contraindication** due to increased risk of hemorrhagic transformation.
*A platelet count of 130,000/mm3*
- A platelet count of 130,000/mm³ is above the **contraindication threshold for thrombolytic therapy**, which is typically <100,000/mm³.
- Therefore, this platelet count would **not prevent** the initiation of tPA.
*Age of 74 years*
- While older age was once considered a relative contraindication, current guidelines **do not consider age alone (including 74 years old) as an absolute contraindication** for thrombolytic therapy in acute ischemic stroke.
- Eligibility is determined by a comprehensive risk-benefit assessment, not solely by age.
*Cholesterol level of 240 mg/dL*
- An elevated **cholesterol level** is a **risk factor for atherosclerosis** and ischemic stroke, but it is **not a contraindication for acute thrombolytic therapy**.
- It relates to the underlying cause of the stroke rather than the immediate treatment decision.
*Creatinine level of 1.3 mg/dL*
- A **creatinine level of 1.3 mg/dL** indicates **mild renal impairment**, but it is **not a contraindication for thrombolytic therapy**.
- Renal function more significantly impacts the use of certain anticoagulants, but not typically alteplase in the acute setting.
Reperfusion strategies US Medical PG Question 7: A 58-year-old woman is brought to the emergency department for shortness of breath and chest pain. Pulmonary angiography shows a large saddle embolus in the pulmonary arteries. Emergency drug therapy is administered and she is admitted to the hospital for observation. A follow-up CT scan of the chest shortly after admission shows that the thrombus has disappeared. Five hours later, the patient is found to be lethargic with slurred speech. Physical examination shows decreased consciousness, dysarthria, and optic disc swelling bilaterally. Which of the following is the most likely cause of her neurological symptoms?
- A. Acute metabolic encephalopathy
- B. Embolic cerebrovascular accident
- C. Idiopathic intracranial hypertension
- D. Intracerebral hemorrhage (Correct Answer)
- E. Drug-induced hypotension
Reperfusion strategies Explanation: ***Intracerebral hemorrhage***
- The patient was treated for a **saddle pulmonary embolism** with drug therapy (likely thrombolytics). This type of therapy carries a significant risk of **intracerebral hemorrhage**, especially in older patients or those with underlying risks. The sudden onset of neurological symptoms, including decreased consciousness, dysarthria, and **bilateral optic disc swelling** (indicating increased intracranial pressure), five hours after receiving thrombolytic therapy, is highly suspicious for a hemorrhagic stroke.
- The rapid dissolution of the pulmonary thrombus followed by new neurological deficits strongly suggests a side effect of aggressive anticoagulation or thrombolysis.
*Acute metabolic encephalopathy*
- While metabolic encephalopathy can cause decreased consciousness and lethargy, it typically does not present with focal neurological signs like **dysarthria** or **optic disc swelling** indicating increased intracranial pressure.
- The rapid onset immediately following thrombolytic treatment for a significant thromboembolic event points away from a primary metabolic cause.
*Embolic cerebrovascular accident*
- An embolic stroke could cause similar neurological symptoms, but the history of massive thrombolysis for a pulmonary embolism makes **hemorrhage** a more immediate concern given the treatment. Additionally, an embolic stroke would not typically cause **bilateral optic disc swelling** so rapidly.
- While theoretically possible if a paradoxical embolism occurred (e.g., via a patent foramen ovale), the administration of powerful anticoagulants/thrombolytics makes hemorrhage the more probable complication.
*Idiopathic intracranial hypertension*
- This condition is characterized by **increased intracranial pressure without an identifiable cause** and primarily affects young, obese women. It typically presents with chronic headaches and visual disturbances, but rarely acute neurological deterioration with decreased consciousness or dysarthria.
- The acute, post-treatment onset of symptoms is inconsistent with the chronic nature of idiopathic intracranial hypertension.
*Drug-induced hypotension*
- Severe hypotension could lead to global cerebral hypoperfusion and altered mental status, but it usually causes more generalized symptoms, and is less likely to produce focal neurological signs like **dysarthria** or **bilateral optic disc swelling** within such a short timeframe as the primary cause.
- While hypotension can be a side effect of some drugs, the specific constellation of symptoms, particularly the optic disc swelling, points more directly towards an acute intracranial event like hemorrhage.
Reperfusion strategies US Medical PG Question 8: A 55-year-old man comes to the emergency department because of left-sided chest pain and difficulty breathing for the past 30 minutes. His pulse is 88/min. He is pale and anxious. Serum studies show increased cardiac enzymes. An ECG shows ST-elevations in leads I, aVL, and V5-V6. A percutaneous coronary intervention is performed. In order to localize the site of the lesion, the catheter must pass through which of the following structures?
- A. Left coronary artery → left circumflex artery (Correct Answer)
- B. Right coronary artery → posterior descending artery
- C. Left coronary artery → left anterior descending artery
- D. Right coronary artery → right marginal artery
- E. Left coronary artery → posterior descending artery
Reperfusion strategies Explanation: ***Left coronary artery → left circumflex artery***
- **ST-elevations** in leads I, aVL, and V5-V6 are indicative of a **lateral myocardial infarction**.
- The **left circumflex artery** primarily supplies the lateral wall of the left ventricle.
*Right coronary artery → posterior descending artery*
- The **posterior descending artery** (PDA) typically supplies the inferior wall and posterior interventricular septum.
- An occlusion here would cause **ST-elevations** in leads II, III, and aVF, which is not seen in this case.
*Left coronary artery → left anterior descending artery*
- The **left anterior descending** (LAD) artery supplies the anterior wall and apex of the left ventricle.
- Occlusion of the LAD would typically cause **ST-elevations** in leads V1-V4, indicating an anterior MI.
*Right coronary artery → right marginal artery*
- The **right marginal artery** is a branch of the right coronary artery and supplies part of the right ventricle.
- Occlusion here would primarily affect the **right ventricle**, and is not typically associated with the given ECG changes.
*Left coronary artery → posterior descending artery*
- While the **posterior descending artery** can sometimes originate from the left circumflex artery (**left dominant circulation**), it primarily supplies the inferior wall.
- The observed ECG changes in leads I, aVL, and V5-V6 are characteristic of a **lateral wall infarct**, which is supplied by the left circumflex artery.
Reperfusion strategies US Medical PG Question 9: A 70-year-old man is brought to the emergency room with complaints of severe substernal chest pain for the last hour. The pain started suddenly, and the patient describes the pain as “going into the shoulder”. The patient took aspirin at home and has been given multiple doses of sublingual nitroglycerin, but the pain has not subsided. He has a blood pressure of 112/84 mm Hg, the pulse is 63/min, the respiratory rate is 18/min, and the temperature is 36.9°C (98.0°F). Cardiac auscultation reveals normal S1 and S2 sounds, however, an additional S4 sound is heard. The patient is sweating profusely, and the lungs are clear to auscultation. No jugular venous distension or pedal edema is observed. His initial ECG shows ST elevation in leads II, III, and aVF. Which of the following will likely have the most benefit in this patient?
- A. Antiarrhythmics
- B. Percutaneous coronary intervention (Correct Answer)
- C. Thrombolytics
- D. Beta blockers
- E. Clopidogrel
Reperfusion strategies Explanation: ***Percutaneous coronary intervention***
- This patient is experiencing a **ST-elevation myocardial infarction (STEMI)**, indicated by severe chest pain radiating to the shoulder, no relief with nitroglycerin, and ST elevation in leads II, III, and aVF.
- **Reperfusion therapy** is crucial for STEMI, and PCI is the preferred method when available within the recommended timeframe (typically <90-120 minutes from first medical contact) as it directly opens the occluded coronary artery.
*Antiarrhythmics*
- While **arrhythmias** can occur during an MI, there is no indication that the patient is currently experiencing a life-threatening arrhythmia requiring immediate antiarrhythmic drug administration.
- The primary goal in STEMI is **reperfusion**, not immediate arrhythmia suppression unless the arrhythmia is hemodynamically unstable.
*Thrombolytics*
- **Thrombolytics (fibrinolytics)** are an alternative reperfusion strategy for STEMI if PCI is not available or cannot be performed within the recommended timeframe.
- Given that the question asks for the "most benefit," and PCI is generally superior to thrombolytics in terms of complete reperfusion and clinical outcomes when available promptly, thrombolytics would not be the first choice.
*Beta blockers*
- **Beta blockers** are important for managing MI by reducing myocardial oxygen demand and preventing arrhythmias; however, they are often initiated after reperfusion and careful patient evaluation, especially in the acute phase of STEMI where immediate reperfusion is paramount.
- They should be used with caution if there are signs of **heart failure** or **cardiogenic shock**, which are not present here but still highlight that it's not the immediate, most beneficial intervention.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent that would be part of the medical management for STEMI, along with aspirin and anticoagulants, to prevent further clot formation.
- While important, it is an adjunctive therapy and does not directly address the need for **rapid reperfusion** to restore blood flow to the ischemic myocardium, which is the most critical intervention in STEMI.
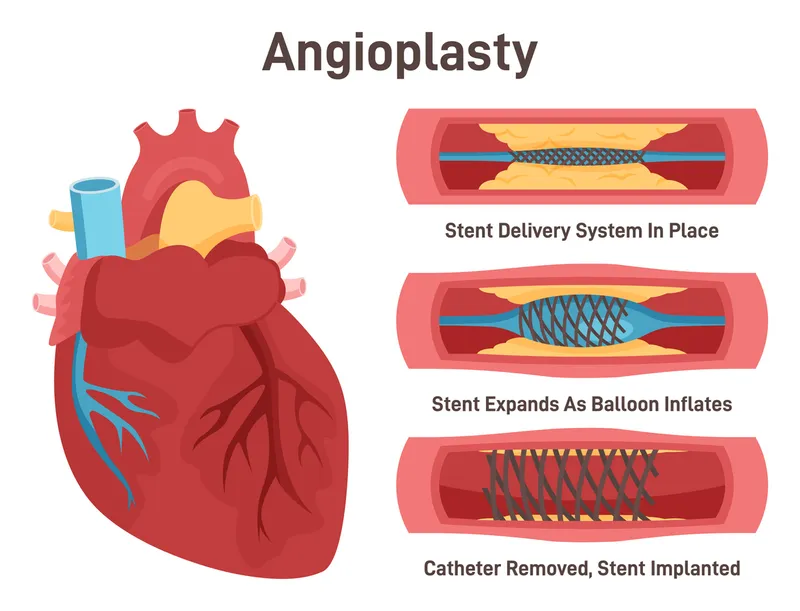
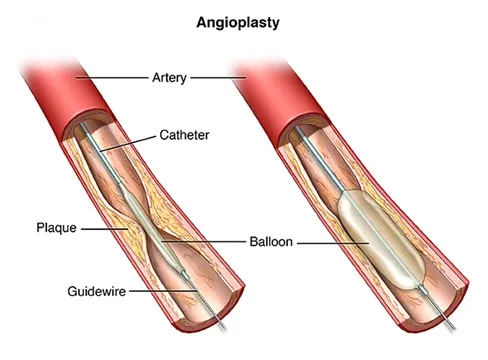
Reperfusion strategies US Medical PG Question 10: A 53-year-old man with a past medical history significant for hyperlipidemia, hypertension, and hyperhomocysteinemia presents to the emergency department complaining of 10/10 crushing, left-sided chest pain radiating down his left arm and up his neck into the left side of his jaw. His ECG shows ST-segment elevation in leads V2-V4. He is taken to the cardiac catheterization laboratory for successful balloon angioplasty and stenting of a complete blockage in his left anterior descending coronary artery. Echocardiogram the following day shows decreased left ventricular function and regional wall motion abnormalities. A follow-up echocardiogram 14 days later shows a normal ejection fraction and no regional wall motion abnormalities. This post-infarct course illustrates which of the following concepts?
- A. Coronary collateral circulation
- B. Ventricular remodeling
- C. Myocardial hibernation
- D. Myocardial stunning (Correct Answer)
- E. Reperfusion injury
Reperfusion strategies Explanation: ***Myocardial stunning***
- This refers to a temporary **post-ischemic contractile dysfunction** that persists even after blood flow has been restored following an acute ischemic event.
- The return to normal left ventricular function and absence of regional wall motion abnormalities after successful reperfusion indicates that the initial dysfunction was transient and not due to permanent myocardial damage.
- Classic timeframe: recovery occurs over **days to weeks** after reperfusion, as seen in this patient (14 days).
*Coronary collateral circulation*
- This involves the development of alternative pathways for blood supply to the myocardium when the primary coronary arteries are occluded.
- While it can mitigate the extent of myocardial injury, it generally doesn't explain the reversal of severe regional wall motion abnormalities and low ejection fraction to normal in such a short period after a complete blockage.
*Ventricular remodeling*
- This refers to changes in the **size, shape, and function of the ventricles** in response to myocardial injury or chronic pressure/volume overload, often leading to progressive heart failure.
- It typically involves *persistent* and *often detrimental* changes, which is contrary to the improvement seen in this patient's echocardiogram.
*Myocardial hibernation*
- This is a state of **persistently impaired myocardial function at rest** due to **chronic inadequate blood flow** that can improve with revascularization.
- Hibernation requires **pre-existing chronic ischemia** with baseline dysfunction prior to intervention, not an acute complete occlusion presenting as STEMI.
- This patient had an **acute presentation** with complete blockage and no history suggesting chronic stable ischemia, making stunning (not hibernation) the correct answer.
*Reperfusion injury*
- This is damage to the myocardial tissue that occurs **after blood flow is restored** to an ischemic area, often involving oxidative stress and inflammation.
- While it can worsen myocardial function, it is a complication of reperfusion that causes *additional damage*, not a phenomenon that explains the *recovery* of cardiac function after reperfusion.
More Reperfusion strategies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.