Complications of MI US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Complications of MI. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Complications of MI US Medical PG Question 1: A 28-year-old male presents with sharp, stabbing chest pain that worsens when lying flat and improves when sitting forward. He reports a recent viral upper respiratory infection 2 weeks ago. On examination, a friction rub is heard on auscultation. His vital signs are stable.
An ECG is most likely to show which of the following findings in this patient?
- A. Diffuse, concave ST-segment elevations (Correct Answer)
- B. Peaked T waves and ST-segment elevations in leads V1-V6
- C. Sawtooth-appearance of P waves
- D. S waves in lead I, Q waves in lead III, and inverted T waves in lead III
- E. Alternating high and low amplitude QRS complexes
Complications of MI Explanation: ***Diffuse, concave ST-segment elevations***
- This is a hallmark ECG finding in **acute pericarditis**, along with **PR segment depression**, due to widespread inflammation of the epicardium.
- The chest pain described here (sharp, stabbing, worse when lying flat, improved by sitting forward) paired with a recent viral infection and a pericardial friction rub, is highly characteristic of **pericarditis**.
*Peaked T waves and ST-segment elevations in leads V1-V6*
- **Peaked T waves** are typically seen in early stages of hyperkalemia or myocardial ischemia, while **ST-segment elevations in specific leads (V1-V6)** are more indicative of an **ST-elevation myocardial infarction (STEMI)** involving the anterior wall.
- The diffuse nature of ST elevation in pericarditis, as opposed to regional changes, along with **PR depression**, differentiates it from STEMI.
*Sawtooth-appearance of P waves*
- A **sawtooth appearance of P waves** (often referred to as 'f waves') is characteristic of **atrial flutter**, a type of supraventricular tachycardia.
- This finding is unrelated to pericarditis, which primarily affects the pericardium and not the atrial electrical activity in this specific manner.
*S waves in lead I, Q waves in lead III, and inverted T waves in lead III*
- This pattern, known as the **S1Q3T3 pattern**, is a classic (though not always present) ECG finding suggestive of **acute pulmonary embolism**.
- While pulmonary embolism can cause chest pain, its presentation differs significantly from the positional relief and friction rub seen in pericarditis.
*Alternating high and low amplitude QRS complexes*
- This ECG finding, known as **electrical alternans**, is highly specific for a large **pericardial effusion** or **cardiac tamponade**, where the heart swings within the fluid-filled pericardial sac.
- Although pericarditis can lead to effusion, the presence of a friction rub and stable vital signs suggests acute pericarditis without significant tamponade at this stage, making diffuse ST elevation a more likely initial finding.
Complications of MI US Medical PG Question 2: A 55-year-old man with a past medical history of obesity and hyperlipidemia suddenly develops left-sided chest pain and shortness of breath while at work. He relays to coworkers that the pain is intense and has spread to his upper left arm over the past 10 minutes. He reports it feels a lot like the “heart attack” he had a year ago. He suddenly collapses and is unresponsive. Coworkers perform cardiopulmonary resuscitation for 18 minutes until emergency medical services arrives. Paramedics pronounce him dead at the scene. Which of the following is the most likely cause of death in this man?
- A. Pericarditis
- B. Aortic dissection
- C. Atrial fibrillation
- D. Ventricular tachycardia (Correct Answer)
- E. Free wall rupture
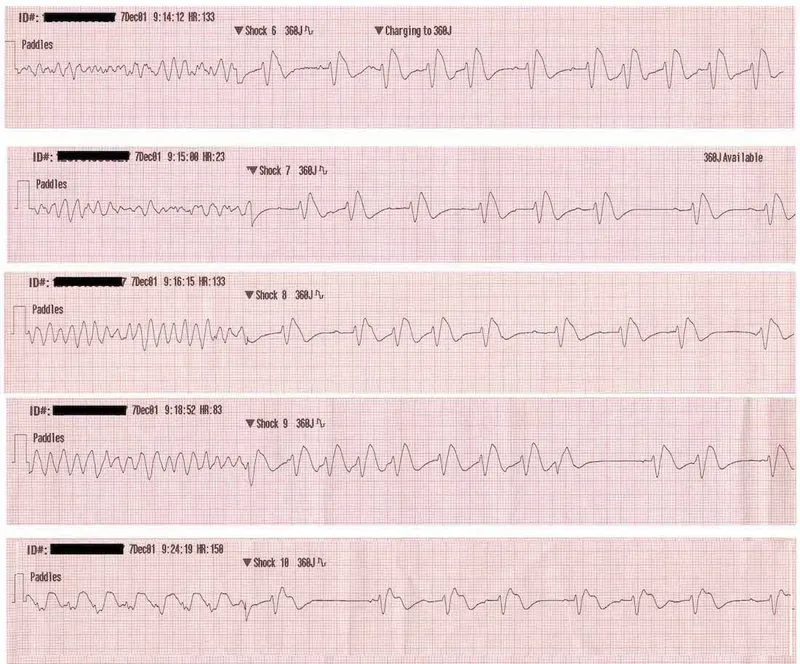
Complications of MI Explanation: ***Ventricular tachycardia***
- The patient's history of MI **1 year ago** creates a substrate of **scarred myocardium** that predisposes to life-threatening ventricular arrhythmias.
- The current presentation of sudden chest pain radiating to the arm suggests **acute re-infarction**, which triggers electrical instability in already compromised myocardium.
- **Ventricular tachycardia (VT)** degenerating to **ventricular fibrillation (VF)** is the **most common cause of sudden cardiac death** in patients with prior MI, especially during acute ischemic events.
- The rapid collapse and death within minutes, despite CPR, is classic for fatal ventricular arrhythmia.
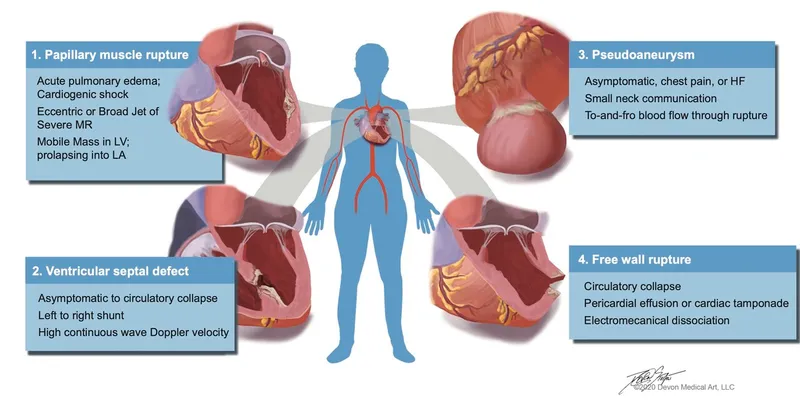
*Free wall rupture*
- Free wall rupture is a **mechanical complication** that occurs **3-14 days** (typically days 3-7) after an **acute MI**, not 1 year later.
- By 1 year post-MI, the ventricular wall has either healed with fibrous scar tissue or formed a chronic ventricular aneurysm.
- While this would cause sudden death via cardiac tamponade, the **timing makes this unlikely** in this scenario.
*Pericarditis*
- Pericarditis causes **pleuritic chest pain** that is sharp, positional, and typically relieved by leaning forward.
- It is **not an immediate cause of sudden cardiac death** and would not explain the rapid collapse and unresponsiveness.
- While post-MI (Dressler) pericarditis can occur weeks after MI, it doesn't cause this presentation.
*Aortic dissection*
- Aortic dissection presents with **sudden, severe, tearing chest pain** often radiating to the back.
- While potentially fatal, the patient's description of pain "a lot like the heart attack he had a year ago" and his cardiac risk factors make **recurrent MI with fatal arrhythmia more likely**.
- No mention of blood pressure differential or pulse deficits that would suggest dissection.
*Atrial fibrillation*
- Atrial fibrillation is a **supraventricular arrhythmia** that causes palpitations, dyspnea, and irregular pulse.
- It is **not typically immediately fatal** in isolation and does not cause sudden collapse and death within minutes.
- While AF can lead to stroke or heart failure over time, it doesn't explain this acute sudden cardiac death.
Complications of MI US Medical PG Question 3: A 53-year-old man with a past medical history significant for hyperlipidemia, hypertension, and hyperhomocysteinemia presents to the emergency department complaining of 10/10 crushing, left-sided chest pain radiating down his left arm and up his neck into the left side of his jaw. His ECG shows ST-segment elevation in leads V2-V4. He is taken to the cardiac catheterization laboratory for successful balloon angioplasty and stenting of a complete blockage in his left anterior descending coronary artery. Echocardiogram the following day shows decreased left ventricular function and regional wall motion abnormalities. A follow-up echocardiogram 14 days later shows a normal ejection fraction and no regional wall motion abnormalities. This post-infarct course illustrates which of the following concepts?
- A. Coronary collateral circulation
- B. Ventricular remodeling
- C. Myocardial hibernation
- D. Myocardial stunning (Correct Answer)
- E. Reperfusion injury
Complications of MI Explanation: ***Myocardial stunning***
- This refers to a temporary **post-ischemic contractile dysfunction** that persists even after blood flow has been restored following an acute ischemic event.
- The return to normal left ventricular function and absence of regional wall motion abnormalities after successful reperfusion indicates that the initial dysfunction was transient and not due to permanent myocardial damage.
- Classic timeframe: recovery occurs over **days to weeks** after reperfusion, as seen in this patient (14 days).
*Coronary collateral circulation*
- This involves the development of alternative pathways for blood supply to the myocardium when the primary coronary arteries are occluded.
- While it can mitigate the extent of myocardial injury, it generally doesn't explain the reversal of severe regional wall motion abnormalities and low ejection fraction to normal in such a short period after a complete blockage.
*Ventricular remodeling*
- This refers to changes in the **size, shape, and function of the ventricles** in response to myocardial injury or chronic pressure/volume overload, often leading to progressive heart failure.
- It typically involves *persistent* and *often detrimental* changes, which is contrary to the improvement seen in this patient's echocardiogram.
*Myocardial hibernation*
- This is a state of **persistently impaired myocardial function at rest** due to **chronic inadequate blood flow** that can improve with revascularization.
- Hibernation requires **pre-existing chronic ischemia** with baseline dysfunction prior to intervention, not an acute complete occlusion presenting as STEMI.
- This patient had an **acute presentation** with complete blockage and no history suggesting chronic stable ischemia, making stunning (not hibernation) the correct answer.
*Reperfusion injury*
- This is damage to the myocardial tissue that occurs **after blood flow is restored** to an ischemic area, often involving oxidative stress and inflammation.
- While it can worsen myocardial function, it is a complication of reperfusion that causes *additional damage*, not a phenomenon that explains the *recovery* of cardiac function after reperfusion.
Complications of MI US Medical PG Question 4: A 73-year-old man presents to the emergency department with acute substernal chest pain that began a few hours ago. The pain is described as a "pressure" that radiates to his left arm. His past medical history is significant for hypertension and hyperlipidemia. He is on chlorthalidone for his hypertension and simvastatin for hyperlipidemia. He has a 30 pack-year history of smoking and drinks 1-2 beers on weekends. His EKG shows ST depressions in the anterior precordial leads and he is given the proper medications and sent for emergency revascularization. Seven days later, he develops dyspnea that worsens in the supine position. Bibasilar crackles are heard on pulmonary auscultation. Cardiac exam reveals a new 3/6 holosystolic murmur best heard at the apex with radiation to the axilla. What is the most likely etiology of this patient's new symptoms?
- A. Ventricular wall aneurysm
- B. Restrictive pericarditis
- C. Papillary muscle rupture (Correct Answer)
- D. Aortic stenosis
- E. Arrhythmia
Complications of MI Explanation: ***Papillary muscle rupture***
- The sudden onset of **dyspnea**, **bibasilar crackles**, and a **new holosystolic murmur** after an acute myocardial infarction (MI) strongly suggests **mitral regurgitation**, often caused by papillary muscle rupture.
- This complication typically occurs **3-7 days post-MI** and leads to acute left heart failure, as described by the patient's worsening symptoms in the supine position and pulmonary edema.
*Ventricular wall aneurysm*
- A ventricular aneurysm is a late complication of MI, typically developing **weeks to months** later, not within 7 days.
- While it can cause heart failure and arrhythmias, a **new holosystolic murmur** is not a characteristic finding.
*Restrictive pericarditis*
- This condition involves the stiffening of the pericardium, leading to impaired ventricular filling, but it is typically a more **chronic process** and is not an acute complication of MI.
- The classic physical finding of a new holosystolic murmur with acute dyspnea is not consistent with restrictive pericarditis.
*Aortic stenosis*
- Aortic stenosis is a chronic valvular disease, usually presenting with a **systolic ejection murmur** best heard at the right upper sternal border, not a holosystolic murmur post-MI.
- While it can cause dyspnea, the acute onset following an MI with a new murmur suggests a different etiology.
*Arrhythmia*
- An arrhythmia can cause dyspnea and heart failure symptoms, but it would not explain the presence of a **new holosystolic murmur**, which indicates a structural cardiac issue.
- While common post-MI, the specific constellation of symptoms points to a mechanical complication.
Complications of MI US Medical PG Question 5: A 40-year-old Caucasian male presents to the emergency room after being shot in the arm in a hunting accident. His shirt is soaked through with blood. He has a blood pressure of 65/40, a heart rate of 122, and his skin is pale, cool to the touch, and moist. This patient is most likely experiencing all of the following EXCEPT:
- A. Decreased sarcomere length in the myocardium
- B. Increased stroke volume (Correct Answer)
- C. Confusion and irritability
- D. Decreased preload
- E. Increased thromboxane A2
Complications of MI Explanation: ***Increased stroke volume***
- The patient is experiencing **hypovolemic shock** due to significant blood loss, meaning their **cardiac output** is severely compromised.
- In shock, the heart attempts to compensate by increasing **heart rate**, but **stroke volume** is typically decreased due to reduced **preload**.
*Decreased sarcomere length in the myocardium*
- In situations of significant blood loss and **decreased preload**, there is less venous return to the heart, leading to reduced end-diastolic volume.
- According to the **Frank-Starling law**, reduced end-diastolic volume results in shorter initial sarcomere length, which reduces the force of contraction and thus, **stroke volume**.
*Confusion and irritability*
- **Hypovolemic shock** leads to widespread **tissue hypoperfusion**, especially to vital organs like the brain.
- Reduced cerebral blood flow results in impaired brain function, manifesting as **confusion, irritability**, and altered mental status.
*Decreased preload*
- Significant blood loss leads to a reduction in the **total circulating blood volume**.
- This reduction directly decreases the venous return to the heart, thus lowering the **end-diastolic volume** and subsequently, the **preload**.
*Increased thromboxane A2*
- In response to **vascular injury and bleeding**, the body initiates hemostasis, a critical component of which is platelet aggregation.
- **Thromboxane A2** is a potent vasoconstrictor and platelet aggregator released by activated platelets to form a **platelet plug** and help stop bleeding.
Complications of MI US Medical PG Question 6: A 72-year-old man presents to the emergency department because of difficulty breathing and sharp chest pain. The chest pain increases in intensity with lying down, and it radiates to the scapular ridge. Approximately 3 weeks ago, he had an anterior ST-elevation myocardial infarction, which was treated with intravenous alteplase. He was discharged home in a stable condition. Current vital signs include a temperature of 38.1 (100.5°F), blood pressure of 131/91 mm Hg, and pulse of 99/min. On examination, heart sounds are distant and a scratching sound is heard on the left sternal border. ECG reveals widespread concave ST elevations in the precordial leads and PR depressions in leads V2-V6. Which of the following is the most likely cause of this patient condition?
- A. Recurrent infarction
- B. Myocarditis
- C. Aortic dissection
- D. Dressler’s syndrome (Correct Answer)
- E. Ventricular aneurysm
Complications of MI Explanation: ***Dressler’s syndrome***
- This syndrome, also known as **post-myocardial infarction syndrome**, typically presents weeks to months after an MI and is characterized by pleuritic chest pain, fever, and pericardial friction rub.
- The **widespread ST elevations (concave)** and **PR depressions** on ECG are classic findings of pericarditis, which is the underlying pathology of Dressler's syndrome.
*Recurrent infarction*
- While an MI can cause chest pain, the pain associated with infarction is typically **retrosternal, crushing**, and does not improve with leaning forward or worsen with lying down.
- ECG findings of recurrent MI would show **convex ST elevations** in a specific coronary artery territory, not widespread concave ST elevation.
*Myocarditis*
- Myocarditis can cause chest pain, fever, and ECG changes (including ST elevations), but it is primarily an **inflammation of the heart muscle** often due to viral infection.
- In this case, the **pericardial friction rub** and history of recent MI strongly point towards pericardial inflammation, not primarily myocardial inflammation.
*Aortic dissection*
- Aortic dissection presents with **severe, tearing chest pain** that often radiates to the back, but it typically has an abrupt onset and is not associated with a pericardial friction rub or widespread ST elevations.
- The ECG findings of pericarditis do not support acute aortic dissection.
*Ventricular aneurysm*
- A ventricular aneurysm is a late complication of MI and can lead to symptoms like heart failure or arrhythmias, but it does **not typically cause acute pericarditic chest pain** or associated ECG findings.
- While it can cause persistent ST elevation, it would not be widespread and concave, and it wouldn't be associated with a friction rub.
Complications of MI US Medical PG Question 7: A previously healthy 33-year-old woman comes to the emergency department because she could feel her heart racing intermittently for the last 2 hours. Each episode lasts about 10 minutes. She does not have any chest pain. Her mother died of a heart attack and her father had an angioplasty 3 years ago. She has smoked a half pack of cigarettes daily for 14 years. She drinks one to two beers daily. She appears anxious. Her temperature is 37.6°C (98.1°F), pulse is 160/min, and blood pressure is 104/76 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. An ECG is shown. Which of the following is the most appropriate initial step in management?
- A. Intravenous adenosine
- B. Aspirin
- C. Intravenous procainamide
- D. Vagal maneuvers (Correct Answer)
- E. Coronary angioplasty
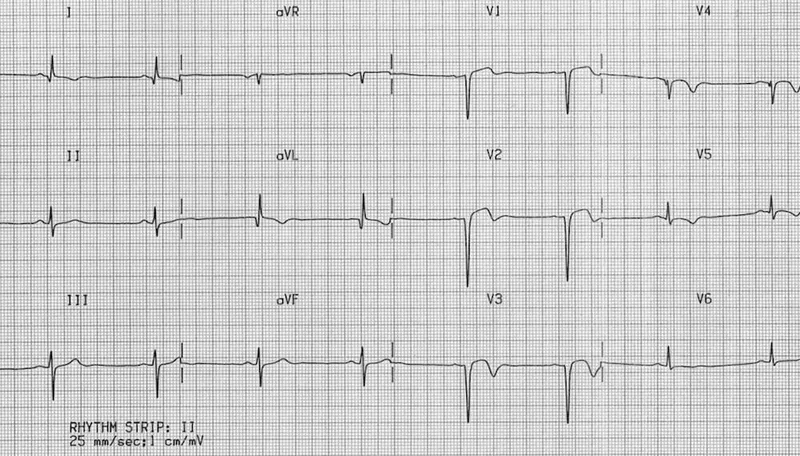
Complications of MI Explanation: ***Vagal maneuvers***
- The ECG shows a **narrow complex tachycardia** at a rate of 160/min. Given the patient's stable hemodynamics (BP 104/76 mm Hg), **vagal maneuvers** are the most appropriate initial step to attempt to terminate the re-entrant rhythm, such as Valsalva maneuver or carotid sinus massage.
- Vagal maneuvers increase **parasympathetic tone** to the heart, which can slow conduction through the AV node and potentially break the re-entrant circuit causing the supraventricular tachycardia (SVT).
*Intravenous adenosine*
- **Adenosine** is a treatment for **narrow complex tachycardia** if vagal maneuvers fail, but it is not the *initial* step in a hemodynamically stable patient.
- It works by transiently blocking the **AV node**, interrupting re-entrant pathways.
*Intravenous procainamide*
- **Procainamide** is an antiarrhythmic typically used for **wide complex tachycardia** or for narrow complex tachycardias that are refractory to vagal maneuvers and adenosine, or when there is evidence of pre-excitation.
- It is not the first-line treatment for a stable **narrow complex tachycardia**.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used in the management of acute coronary syndromes or for cardiovascular disease prevention.
- It has no role in the immediate termination of a **tachyarrhythmia** like the one presented.
*Coronary angioplasty*
- **Coronary angioplasty** is a procedure used to open blocked or narrowed coronary arteries, usually for **acute coronary syndromes** or chronic stable angina.
- The patient presents with a **tachyarrhythmia** and no signs of acute ischemia (no chest pain, although risk factors are present), making angioplasty an inappropriate initial management step.
Complications of MI US Medical PG Question 8: Two days after being admitted for acute myocardial infarction, a 61-year-old man has sharp, substernal chest pain that worsens with inspiration and improves when leaning forward. Cardiac examination shows a scratchy sound best heard over the left sternal border. Histopathological examination of the infarcted myocardial tissue is most likely to show which of the following findings?
- A. Neutrophilic infiltration
- B. Collagenous scar tissue
- C. Normal myocardium
- D. Coagulative necrosis (Correct Answer)
- E. Granulation tissue with macrophages
Complications of MI Explanation: ***Coagulative necrosis***
- The patient's clinical presentation (sharp, substernal chest pain, worsening with inspiration, improving while leaning forward, and a scratchy pericardial friction rub) indicates **post-MI fibrinous pericarditis**, a common complication occurring 2-4 days after myocardial infarction.
- At **day 2 post-MI**, the infarcted myocardium demonstrates **coagulative necrosis** as the primary and most characteristic histopathological finding, representing irreversible ischemic cell death with preserved tissue architecture.
- While neutrophilic infiltration is also present at this timepoint, coagulative necrosis of the cardiomyocytes themselves is the defining pathological feature that distinguishes irreversible myocardial injury.
*Neutrophilic infiltration*
- **Neutrophilic infiltration** is indeed present at day 2 post-MI (peaks at days 1-3) as part of the acute inflammatory response to clear necrotic debris.
- However, neutrophils represent the **reactive inflammatory response** rather than the primary pathological change in the infarcted cardiomyocytes themselves.
- The question asks about the most characteristic histopathological finding, which is the **coagulative necrosis** of the myocardial cells, not the secondary inflammatory infiltrate.
*Collagenous scar tissue*
- **Collagenous scar tissue** forms much later during the remodeling phase, typically **7 weeks or more** after MI, representing the final stage of healing.
- At day 2, the tissue is still in the acute phase of coagulative necrosis and early inflammation, far too early for mature fibrous scar formation.
*Normal myocardium*
- The patient has sustained an **acute myocardial infarction** with irreversible injury to cardiac tissue.
- Histopathological examination of the infarcted region would show clear abnormalities, not **normal myocardium**.
*Granulation tissue with macrophages*
- **Granulation tissue** with fibroblasts, new capillaries, and macrophages begins forming during the proliferative phase, typically starting around **days 5-7** post-MI.
- At day 2, it is too early for granulation tissue formation; the tissue is still dominated by coagulative necrosis and acute neutrophilic inflammation.
Complications of MI US Medical PG Question 9: An 80-year-old man presents to the emergency department because of gnawing substernal chest pain that started an hour ago and radiates to his neck and left jaw. A 12-lead ECG is obtained and shows ST-segment elevation with newly developing Q waves. He is admitted for treatment. 4 days after hospitalization he suddenly develops altered mental status, and his blood pressure falls from 115/75 mm Hg to 80/40 mm Hg. Physical examination shows jugular venous distention, pulsus paradoxus, and distant heart sounds. What is the most likely cause of this patient's condition?
- A. Pericardial inflammation
- B. Compression of heart chambers by blood in the pericardial space (Correct Answer)
- C. Arrhythmia caused by ventricular fibrillation
- D. Rupture of papillary muscle
- E. Acute pulmonary edema from left heart failure
Complications of MI Explanation: ***Compression of heart chambers by blood in the pericardial space***
- The patient's initial presentation with ST-elevation myocardial infarction (STEMI) and subsequent development of **hypotension**, **jugular venous distention**, **pulsus paradoxus**, and **distant heart sounds** (Beck's triad) is highly indicative of **cardiac tamponade.**
- In the context of a recent MI, this constellation of symptoms strongly suggests a **cardiac free wall rupture**, leading to blood accumulation in the pericardial sac and compression of the heart.
- Free wall rupture typically occurs **3-7 days post-MI** and is a life-threatening mechanical complication.
*Pericardial inflammation*
- While pericardial inflammation (pericarditis) can occur post-MI, it typically manifests with **pleuritic chest pain** that is relieved by leaning forward and is often associated with a **pericardial friction rub.**
- It does not typically lead to acute, severe hypotension, pulsus paradoxus, or sudden circulatory collapse in this manner without significant effusion and tamponade physiology.
*Arrhythmia caused by ventricular fibrillation*
- **Ventricular fibrillation** would cause immediate cardiac arrest and loss of consciousness, not a gradual development of hypotension, JVD, and pulsus paradoxus.
- While arrhythmias are common post-MI, the specific physical findings point away from isolated VFib as the primary cause of hemodynamic collapse.
*Acute pulmonary edema from left heart failure*
- **Acute pulmonary edema** is a manifestation of **left heart failure**, characterized by severe dyspnea, orthopnea, and crackles on lung auscultation.
- While left heart failure can cause hypotension in cardiogenic shock, it would not typically present with the classic signs of cardiac tamponade such as pulsus paradoxus, distant heart sounds, and prominent JVD without pulmonary congestion findings.
*Rupture of papillary muscle*
- **Papillary muscle rupture** leads to severe **acute mitral regurgitation**, causing acute pulmonary edema, a new holosystolic murmur, and often cardiogenic shock.
- While it can lead to hypotension, it doesn't typically present with the classic signs of cardiac tamponade such as pulsus paradoxus and distant heart sounds; instead, a loud murmur would be prominent.
Complications of MI US Medical PG Question 10: Four days after being admitted to the intensive care unit for acute substernal chest pain and dyspnea, an 80-year-old man is evaluated for hypotension. Coronary angiography on admission showed an occlusion in the left anterior descending artery, and a drug-eluting stent was placed successfully. The patient has a history of hypertension and type 2 diabetes mellitus. Current medications include aspirin, clopidogrel, metoprolol, lisinopril, and atorvastatin. His temperature is 37.2 °C (99 °F), pulse is 112/min, respirations are 21/min, and blood pressure is 72/50 mm Hg. Cardiac examination shows a normal S1 and S2 and a new harsh, holosystolic murmur heard best at the left sternal border. There is jugular venous distention and a right parasternal heave. The lungs are clear to auscultation. Pitting edema extends up to the knees bilaterally. An ECG shows Q waves in the inferior leads. Which of the following is the most likely cause of this patient’s hypotension?
- A. Post-infarction fibrinous pericarditis
- B. Ascending aortic dissection rupture
- C. Interventricular septum rupture (Correct Answer)
- D. Left ventricular free wall rupture
- E. Left ventricular aneurysm rupture
Complications of MI Explanation: ***Interventricular septum rupture***
- A **harsh, holosystolic murmur** heard best at the **left sternal border** 4 days after an **acute MI (LAD occlusion with stenting)** is highly suggestive of interventricular septum rupture.
- VSR typically occurs **3-5 days post-MI** when myocardial necrosis weakens the septum, and can occur with both anterior and inferior infarctions.
- The rupture creates a **left-to-right shunt**, leading to **hypotension** (decreased systemic cardiac output), **JVD** and **right parasternal heave** (RV volume overload), and biventricular failure.
- The holosystolic murmur at the left sternal border with a palpable thrill is pathognomonic for VSR.
*Post-infarction fibrinous pericarditis*
- This would typically present with a **pericardial friction rub** and potentially pleuritic chest pain, not a holosystolic murmur.
- While it can cause pericardial effusion and tamponade leading to hypotension, the specific murmur described points away from this diagnosis.
*Ascending aortic dissection rupture*
- This would present with **sudden, severe tearing chest pain** radiating to the back and often a new **aortic regurgitation murmur** (diastolic, not systolic).
- The patient's presentation with a holosystolic murmur and recent MI points to a post-infarction mechanical complication.
*Left ventricular free wall rupture*
- This is catastrophic and typically presents with **sudden profound hypotension**, **electromechanical dissociation**, and rapid death.
- Patients usually do not survive long enough for examination findings like a new murmur to develop; they present with acute tamponade and cardiovascular collapse.
*Left ventricular aneurysm rupture*
- A true LV aneurysm is a **late complication** (weeks to months post-MI), not occurring at day 4.
- It would not typically cause a new, harsh holosystolic murmur indicative of an acute shunting process.
- Aneurysm rupture would present similarly to free wall rupture with tamponade.
More Complications of MI US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.