Antiplatelet therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antiplatelet therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antiplatelet therapy US Medical PG Question 1: A 53-year-old man is brought to the emergency department because of wheezing and shortness of breath that began 1 hour after he took a new medication. Earlier in the day he was diagnosed with stable angina pectoris and prescribed a drug that irreversibly inhibits cyclooxygenase-1 and 2. He has chronic rhinosinusitis and asthma treated with inhaled β-adrenergic agonists and corticosteroids. His respirations are 26/min. Examination shows multiple small, erythematous nasal mucosal lesions. After the patient is stabilized, therapy for primary prevention of coronary artery disease should be switched to a drug with which of the following mechanisms of action?
- A. Direct inhibition of Factor Xa
- B. Sequestration of Ca2+ ions
- C. Potentiation of antithrombin III
- D. Blockage of P2Y12 component of ADP receptors (Correct Answer)
- E. Inhibition of vitamin K epoxide reductase
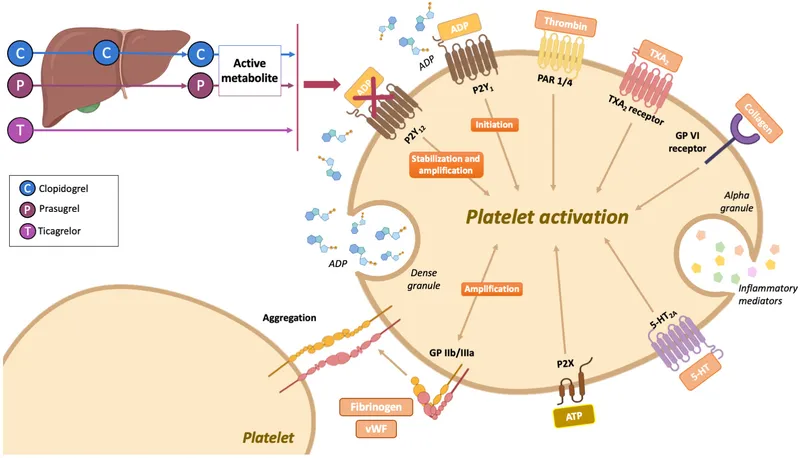
Antiplatelet therapy Explanation: ***Blockage of P2Y12 component of ADP receptors***
- The patient experienced an asthma exacerbation suspected to be due to **aspirin-exacerbated respiratory disease (AERD)**, which is triggered by **aspirin** (a non-selective COX inhibitor).
- Given the need for antiplatelet therapy for CAD, a **P2Y12 receptor antagonist** such as **clopidogrel** is a suitable alternative to aspirin in patients with AERD, as it does not interact with the cyclooxygenase pathway.
*Direct inhibition of Factor Xa*
- This mechanism of action describes drugs like **rivaroxaban** or **apixaban**, which are primarily used as anticoagulants for conditions like atrial fibrillation or venous thromboembolism.
- While they prevent clot formation, they are not typically used for primary prevention of **coronary artery disease (CAD)** in lieu of antiplatelet agents like aspirin or P2Y12 inhibitors.
*Sequestration of Ca2+ ions*
- This refers to **calcium channel blockers (CCBs)**, which are used to treat hypertension, angina, and certain arrhythmias.
- While CCBs can be used to manage angina symptoms, they do not provide the necessary **antiplatelet effect** for primary prevention of cardiovascular events in CAD.
*Potentiation of antithrombin III*
- This is the mechanism of action for **heparins** (e.g., unfractionated heparin, low molecular weight heparin) and related drugs like fondaparinux.
- **Heparins are anticoagulants** used for acute thrombosis or prophylaxis in specific situations, but they are not used for chronic **primary prevention of CAD** in stable patients.
*Inhibition of vitamin K epoxide reductase*
- This describes the mechanism of **warfarin**, a vitamin K antagonist used as an anticoagulant for conditions like atrial fibrillation, prosthetic heart valves, or venous thromboembolism.
- Warfarin is an anticoagulant, not an antiplatelet agent, and is not indicated for **primary prevention of CAD** in this context.
Antiplatelet therapy US Medical PG Question 2: A 66-year-old woman presents to the emergency department complaining of palpitations. She says that she has been experiencing palpitations and lightheadedness for the past 6 months, but before this morning the episodes usually resolved on their own. The patient's medical history is significant for a transient ischemia attack 2 months ago, hypertension, and diabetes. She takes aspirin, metformin, and lisinopril. She states her grandfather died of a stroke, and her mom has a "blood disorder." An electrocardiogram is obtained that shows an irregularly irregular rhythm with rapid ventricular response, consistent with atrial fibrillation. She is given intravenous metoprolol, which resolves her symptoms. In addition to starting a beta-blocker for long-term management, the patient meets criteria for anticoagulation. Both unfractionated heparin and warfarin are started. Five days later, the patient begins complaining of pain and swelling of her left lower extremity. A Doppler ultrasound reveals thrombosis in her left popliteal and tibial veins. A complete blood count is obtained that shows a decrease in platelet count from 245,000/mm^3 to 90,000/mm^3. Coagulation studies are shown below:
Prothrombin time (PT): 15 seconds
Partial thromboplastin time (PTT): 37 seconds
Bleeding time: 14 minutes
Which of the following is the most likely diagnosis?
- A. Thrombotic thrombocytopenic purpura
- B. Type I heparin-induced thrombocytopenia
- C. Warfarin toxicity
- D. Idiopathic thrombocytopenia purpura
- E. Type II heparin-induced thrombocytopenia (Correct Answer)
Antiplatelet therapy Explanation: ***Type II heparin-induced thrombocytopenia***
- This diagnosis is strongly supported by the patient's **recent heparin exposure**, a significant **drop in platelet count** (from 245,000 to 90,000/mm^3, a >50% reduction), and new onset **thrombosis** (popliteal and tibial vein thrombosis).
- Type II HIT involves antibody formation against **heparin-platelet factor 4 (PF4) complexes**, leading to platelet activation, aggregation, and paradoxical thrombosis, often occurring 5-10 days after heparin initiation.
*Thrombotic thrombocytopenic purpura*
- While TTP involves microangiopathic hemolytic anemia, thrombocytopenia, and organ damage including neurological symptoms, the prompt onset of thrombosis after heparin strongly points away from TTP and towards **heparin-related complications**.
- This patient’s symptoms are primarily thrombotic, and typical TTP findings like **schistocytes on blood smear** and **severe ADAMTS13 deficiency** are not mentioned.
*Type I heparin-induced thrombocytopenia*
- Type I HIT is characterized by a **mild, non-immune-mediated platelet drop** (usually not below 100,000/mm^3) that occurs within the first 2 days of heparin therapy.
- It is **rarely associated with thrombosis**, which makes it an unlikely diagnosis given the severe platelet drop and new thromboses.
*Warfarin toxicity*
- Warfarin toxicity typically causes **bleeding complications** due to over-anticoagulation, rather than thrombosis, and is characterized by a **prolonged PT/INR**.
- Although the patient's bleeding time is prolonged, the thrombotic events and significant platelet drop point away from warfarin toxicity as the primary diagnosis.
*Idiopathic thrombocytopenia purpura*
- ITP is an autoimmune disorder causing **isolated thrombocytopenia** (often severe) and **bleeding**, but it is generally *not* associated with paradoxical thrombosis.
- The temporal relationship with heparin exposure and the thrombotic events are inconsistent with a primary diagnosis of unprovoked ITP.
Antiplatelet therapy US Medical PG Question 3: A 54-year-old man is brought to the emergency department 1 hour after the sudden onset of shortness of breath, severe chest pain, and sweating. He has hypertension and type 2 diabetes mellitus. He has smoked one pack and a half of cigarettes daily for 20 years. An ECG shows ST-segment elevations in leads II, III, and avF. The next hospital with a cardiac catheterization unit is more than 2 hours away. Reperfusion pharmacotherapy is initiated. Which of the following is the primary mechanism of action of this medication?
- A. Conversion of plasminogen to plasmin (Correct Answer)
- B. Inhibition of glutamic acid residue carboxylation
- C. Blocking of adenosine diphosphate receptors
- D. Direct inhibition of thrombin activity
- E. Prevention of thromboxane formation
Antiplatelet therapy Explanation: ***Conversion of plasminogen to plasmin***
- **Fibrinolytic** (thrombolytic) drugs, like **tissue plasminogen activator (tPA)**, work by converting plasminogen to plasmin, which then degrades the **fibrin mesh** of a **blood clot**.
- This action helps to **restore blood flow** in cases of ST-segment elevation myocardial infarction (STEMI) where primary **percutaneous coronary intervention (PCI)** is not immediately available.
*Inhibition of glutamic acid residue carboxylation*
- This is the mechanism of action of **warfarin**, an anticoagulant that inhibits the synthesis of **vitamin K-dependent clotting factors** (II, VII, IX, X, protein C, and protein S).
- While important for long-term anticoagulation, it does not provide immediate reperfusion in an acute STEMI.
*Blocking of adenosine diphosphate receptors*
- This describes the mechanism of action of **P2Y12 inhibitors** such as **clopidogrel**, **prasugrel**, and **ticagrelor**.
- These drugs are **antiplatelet agents** that prevent platelet aggregation, but they do not directly dissolve an existing thrombus to restore blood flow in STEMI.
*Direct inhibition of thrombin activity*
- This is the mechanism of action of **direct thrombin inhibitors** like **dabigatran** and **bivalirudin**.
- These drugs primarily prevent clot formation or extension and are not used as primary reperfusion agents for acute STEMI due to an existing occlusive thrombus.
*Prevention of thromboxane formation*
- This is the primary mechanism of action of **aspirin**, which irreversibly inhibits **cyclooxygenase-1 (COX-1)**, thereby reducing the production of thromboxane A2.
- Aspirin is an important antiplatelet drug in STEMI management but does not provide reperfusion by dissolving the clot.
Antiplatelet therapy US Medical PG Question 4: A 70-year-old male presents for an annual exam. His past medical history is notable for shortness of breath when he sleeps, and upon exertion. Recently he has experienced dyspnea and lower extremity edema that seems to be worsening. Both of these symptoms have resolved since he was started on several medications and instructed to weigh himself daily. Which of the following is most likely a component of his medical management?
- A. Lidocaine
- B. Verapamil
- C. Carvedilol (Correct Answer)
- D. Aspirin
- E. Ibutilide
Antiplatelet therapy Explanation: ***Carvedilol***
- The patient exhibits classic symptoms of **heart failure**, such as **dyspnea on exertion**, **orthopnea** (shortness of breath when he sleeps), and **lower extremity edema**.
- **Beta-blockers** like carvedilol are essential for managing **chronic heart failure** by reducing myocardial oxygen demand and improving cardiac function.
*Lidocaine*
- **Lidocaine** is primarily an **antiarrhythmic drug** used for acute treatment of **ventricular arrhythmias**, not for chronic heart failure management.
- It works by blocking sodium channels and has no direct benefit in addressing the underlying pathophysiology of heart failure.
*Verapamil*
- **Verapamil** is a **non-dihydropyridine calcium channel blocker** typically used for hypertension, angina, and supraventricular tachyarrhythmias.
- It can have **negative inotropic effects**, which are generally contraindicated or used with extreme caution in patients with **systolic heart failure** due to its potential to worsen cardiac function.
*Aspirin*
- **Aspirin** is an **antiplatelet agent** used for primary or secondary prevention of **atherosclerotic cardiovascular disease** (e.g., in patients with coronary artery disease).
- It does not directly manage the symptoms or pathophysiology of **heart failure** unless there is a coexisting ischemic etiology.
*Ibutilide*
- **Ibutilide** is an **antiarrhythmic drug** specifically used for the rapid conversion of **atrial flutter and atrial fibrillation** of recent onset to sinus rhythm.
- It is not a medication used for the long-term management of **heart failure** symptoms described in the patient.
Antiplatelet therapy US Medical PG Question 5: Drug A is an experimental compound being investigated for potential use as a protectant against venous thrombosis. Binding assays reveal that the drug’s primary mechanism of action is to block carboxylation of glutamic acid residues in certain serum proteins. Drug A is most similar to which of the following:
- A. Streptokinase
- B. Bivalirudin
- C. Warfarin (Correct Answer)
- D. Heparin
- E. Rivaroxaban
Antiplatelet therapy Explanation: ***Warfarin***
- Warfarin inhibits **vitamin K epoxide reductase**, enzyme responsible for regenerating active vitamin K.
- Active vitamin K is a cofactor for the **gamma-carboxylation of glutamic acid residues** on factors II, VII, IX, X and protein C and S. Thus, warfarin blocks their activation, inhibiting coagulation.
*Steptokinase*
- **Streptokinase** is a **thrombolytic drug** that catalyzes the conversion of **plasminogen to plasmin**, an enzyme that degrades fibrin clots.
- Its mechanism of action is focused on **breaking down existing clots**, rather than preventing their formation by affecting coagulation factor synthesis.
*Bivalirudin*
- **Bivalirudin** is a direct **thrombin inhibitor**, binding directly to the active site and exosite I of thrombin to prevent its action.
- It does not interfere with the **carboxylation of glutamic acid residues** but rather directly inhibits the final common pathway of coagulation.
*Heparin*
- **Heparin** works by potentiating the action of **antithrombin III**, which in turn inactivates thrombin and factor Xa.
- Its mechanism involves accelerating the natural anticoagulant system, rather than inhibiting the **synthesis or activation of coagulation factors** through carboxylation.
*Rivaroxaban*
- **Rivaroxaban** is a **direct factor Xa inhibitor**, which blocks the activity of free and clot-bound factor Xa.
- It directly interferes with the coagulation cascade downstream of the carboxylation step, and does not affect the **vitamin K-dependent carboxylation process**.
Antiplatelet therapy US Medical PG Question 6: A 69-year-old man is brought by his son to the emergency department with weakness in his right arm and leg. The man insists that he is fine and blames his son for "creating panic". Four hours ago the patient was having tea with his wife when he suddenly dropped his teacup. He has had difficulty moving his right arm since then and cannot walk because his right leg feels stuck. He has a history of hypertension and dyslipidemia, for which he currently takes lisinopril and atorvastatin, respectively. He is allergic to aspirin and peanuts. A computerized tomography (CT) scan shows evidence of an ischemic stroke. Which medication would most likely prevent such attacks in this patient in the future?
- A. Celecoxib
- B. Abciximab
- C. Urokinase
- D. Clopidogrel (Correct Answer)
- E. Alteplase
Antiplatelet therapy Explanation: ***Clopidogrel***
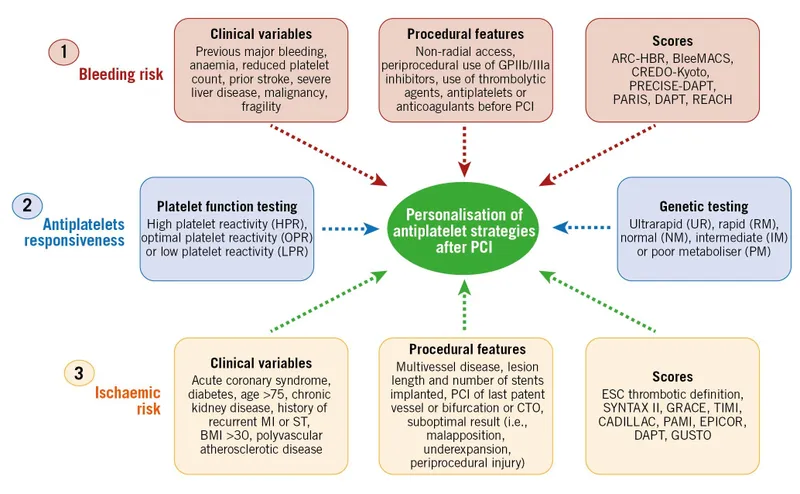
- This patient has suffered an **ischemic stroke** and has a **contraindication to aspirin** due to allergy. **Clopidogrel**, an **alternative antiplatelet agent**, is the most appropriate long-term secondary prevention medication to reduce the risk of future thrombotic events.
- As a **P2Y12 inhibitor**, clopidogrel prevents platelet aggregation, thereby reducing the likelihood of clot formation in patients at high risk for cardiovascular events.
*Celecoxib*
- **Celecoxib** is a **COX-2 selective NSAID** primarily used for pain and inflammation. It has no role in the prevention of ischemic stroke.
- While NSAIDs can have antiplatelet effects through COX-1 inhibition, **COX-2 selective inhibitors like celecoxib generally have a prothrombotic effect** and are not indicated for stroke prevention.
*Abciximab*
- **Abciximab** is a **glycoprotein IIb/IIIa inhibitor** that potently prevents platelet aggregation. It is typically used in acute settings, such as during percutaneous coronary intervention (PCI), and not for long-term stroke prevention.
- Its potent antiplatelet effect and **risk of bleeding** make it unsuitable for chronic outpatient management.
*Urokinase*
- **Urokinase** is a **thrombolytic agent** used to dissolve existing blood clots in acute conditions like pulmonary embolism or acute myocardial infarction. It is not indicated for the prevention of future ischemic strokes.
- Thrombolytics carry a **significant risk of hemorrhage** and are solely for acute clot lysis, not chronic prevention.
*Alteplase*
- **Alteplase** is a **tissue plasminogen activator (tPA)**, a thrombolytic used in the **acute treatment of ischemic stroke** within a specific time window to dissolve clots and restore blood flow.
- It is an **acute rescue therapy** and is not used for long-term secondary prevention of stroke due to its high bleeding risk and short duration of action.
Antiplatelet therapy US Medical PG Question 7: A 73-year-old man presents to the outpatient clinic complaining of chest pain with exertion. He states that resting for a few minutes usually resolves the chest pain. Currently, he takes 81 mg of aspirin daily. He has a blood pressure of 127/85 mm Hg and heart rate of 75/min. Physical examination reveals regular heart sounds and clear lung sounds bilateral. Which medication regimen below should be added?
- A. Metoprolol and a statin daily. Sublingual nitroglycerin as needed. (Correct Answer)
- B. Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.
- C. Amlodipine and a statin daily. Sublingual nitroglycerin as needed.
- D. Amlodipine daily. Sublingual nitroglycerin as needed.
- E. Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.
Antiplatelet therapy Explanation: ***Metoprolol and a statin daily. Sublingual nitroglycerin as needed.***
- This patient presents with symptoms consistent with **stable angina** (**chest pain with exertion, relieved by rest**). The recommended medical therapy includes **antiplatelet agents** (aspirin, already prescribed), **beta-blockers** (metoprolol) for symptom control and improved survival post-MI, and **high-intensity statins** for lipid management and plaque stabilization. **Sublingual nitroglycerin** is crucial for acute symptom relief.
- Beta-blockers like metoprolol decrease myocardial **oxygen demand** by reducing heart rate and contractility, effectively treating angina. Statins are essential for **atherosclerosis management**.
*Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.*
- While clopidogrel is an **antiplatelet agent**, aspirin is typically the first-line choice for stable angina unless there's an intolerance or compelling reason for dual antiplatelet therapy (e.g., recent stent placement), which is not indicated here.
- Amlodipine, a **calcium channel blocker**, can be used for angina but is usually a second-line agent if beta-blockers are contraindicated or insufficient; it doesn't offer the mortality benefit seen with beta-blockers post-MI.
*Amlodipine and a statin daily. Sublingual nitroglycerin as needed.*
- This regimen includes a **statin** and sublingual nitroglycerin, which are appropriate. However, it uses amlodipine instead of a beta-blocker, which is generally the preferred initial therapy for angina due to its benefits in reducing myocardial oxygen demand and improving outcomes, especially in patients with a history of MI or heart failure.
- Beta-blockers provide superior **mortality reduction benefits** in patients with coronary artery disease compared to calcium channel blockers.
*Amlodipine daily. Sublingual nitroglycerin as needed.*
- This option misses two critical components of comprehensive treatment for stable angina: a **statin** for lipid management and plaque stabilization, and a **beta-blocker** for primary symptom control and long-term cardiac protection.
- Relying solely on amlodipine and sublingual nitroglycerin would leave the patient incompletely treated for their underlying **coronary artery disease**.
*Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.*
- This option lacks a **statin**, which is a cornerstone of therapy for stable angina to manage atherosclerosis.
- While metoprolol is appropriate and ranolazine can be used as an add-on therapy for refractory angina, it's not typically a first-line agent and doesn't replace the need for a statin.
Antiplatelet therapy US Medical PG Question 8: A 64-year-old woman comes to the emergency room because of a sudden weakness in her right arm and leg. She has atrial fibrillation, tinea unguium, gastroesophageal reflux disease, hypertension, and hypercholesterolemia. Current medications include warfarin, enalapril, simvastatin, lansoprazole, hydrochlorothiazide, griseofulvin, and ginkgo biloba. Two weeks ago, she had an appointment with her podiatrist. Physical examination shows sagging of her right lower face and decreased muscle strength in her right upper and lower extremity. Babinski sign is positive on the right. Her prothrombin time is 14 seconds (INR = 1.5). Which of the following drugs is the most likely underlying cause of this patient's current condition?
- A. Ginkgo biloba
- B. Lansoprazole
- C. Enalapril
- D. Griseofulvin (Correct Answer)
- E. Simvastatin
Antiplatelet therapy Explanation: ***Griseofulvin***
- Has been shown to **reduce the effectiveness of warfarin** by inducing hepatic enzymes, leading to a subtherapeutic INR and increased risk of thrombotic events like stroke.
- The patient's **INR of 1.5 is subtherapeutic** for atrial fibrillation, which normally requires an INR between 2.0 and 3.0 to prevent stroke.
*Ginkgo biloba*
- Is known to **increase the risk of bleeding** when taken with anticoagulants like warfarin, potentially leading to a higher INR and hemorrhagic stroke.
- In this case, the patient's **INR is subtherapeutic**, which points away from a bleeding diathesis caused by ginkgo biloba.
*Lansoprazole*
- While it can interact with warfarin, **proton pump inhibitors (PPIs)** typically **increase the INR** by inhibiting warfarin metabolism, increasing bleeding risk.
- The patient's **subtherapeutic INR** makes lansoprazole less likely to be the cause of the thrombotic event.
*Enalapril*
- As an **ACE inhibitor**, enalapril generally has **no significant direct interaction with warfarin** that would lead to a subtherapeutic INR or increased stroke risk in this way.
- It is primarily used for hypertension and heart failure, and its effects would not explain the observed subtherapeutic INR and thrombotic stroke.
*Simvastatin*
- Can **increase the effect of warfarin** by inhibiting its metabolism, leading to an **elevated INR** and increased bleeding risk.
- The patient's **low INR** suggests that simvastatin is not the cause of the subtherapeutic anticoagulation or stroke.
Antiplatelet therapy US Medical PG Question 9: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Antiplatelet therapy Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
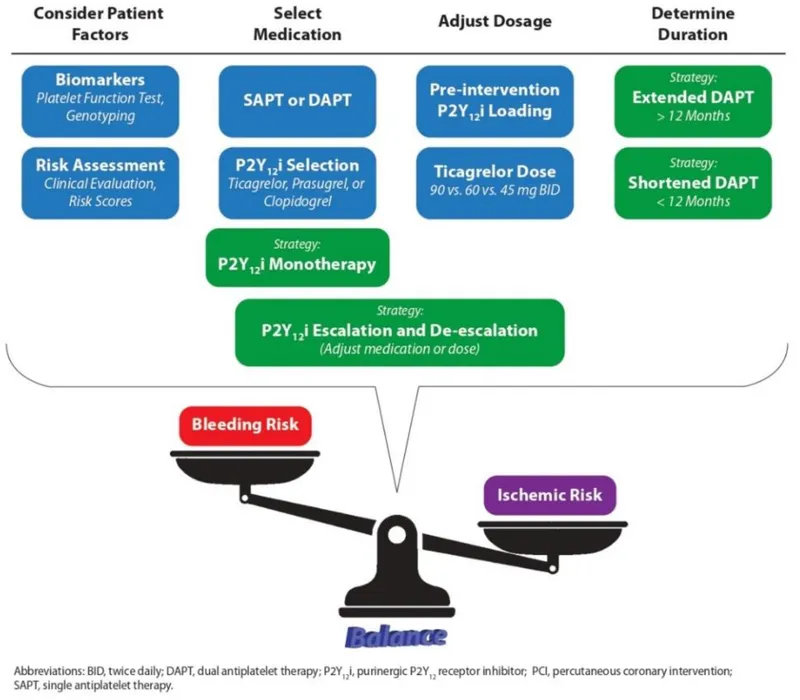
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
Antiplatelet therapy US Medical PG Question 10: A 71-year-old woman presents with a transient episode of right arm and hand weakness that resolved in approximately one hour. Her symptoms started while she was gardening. Her past medical history is notable for hypertension, diabetes, anxiety, and dyslipidemia. Her current medications include insulin, metformin, and fluoxetine. Examination reveals a left carotid bruit. Ultrasound duplex of her carotid arteries demonstrates right and left carotid stenosis of 35% and 50%, respectively. Which of the following is the best next step in management?
- A. Bilateral carotid endarterectomy
- B. Left carotid endarterectomy only
- C. Aspirin (Correct Answer)
- D. Observation
- E. Warfarin
Antiplatelet therapy Explanation: ***Aspirin***
- This patient suffered a **transient ischemic attack (TIA)** given her transient focal neurological deficit. Given that her carotid stenosis is **moderate (35% and 50%)**, **antiplatelet therapy** with aspirin is the initial and best next step to prevent future strokes.
- Aspirin helps prevent platelet aggregation, reducing the risk of **thrombus formation** in already stenotic vessels.
*Bilateral carotid endarterectomy*
- This is not the best next step, as **carotid endarterectomy** is generally reserved for symptomatic patients with **high-grade stenosis** (e.g., typically >70%).
- Performing bilateral procedures at once carries higher risks than staged procedures or medical management for moderate stenosis.
*Left carotid endarterectomy only*
- This is not indicated. While symptoms occurred on the right side (implying a left-sided lesion), a **left carotid endarterectomy** is primarily considered for **high-grade stenosis** in symptomatic patients.
- Her left carotid stenosis is 50%, which is considered moderate and not an immediate indication for surgery.
*Observation*
- This is inappropriate as the patient has experienced a **TIA**, indicating a high risk of future stroke.
- Without intervention, including antiplatelet therapy, the risk of a debilitating stroke is significantly increased.
*Warfarin*
- **Warfarin** is an anticoagulant used for conditions like atrial fibrillation or deep vein thrombosis but is **not the primary treatment for TIA due to carotid stenosis**.
- Its use in this context may increase the risk of bleeding without providing superior benefit to aspirin in preventing arterial clots from carotid plaques.
More Antiplatelet therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.