Anticoagulation in ACS US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anticoagulation in ACS. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anticoagulation in ACS US Medical PG Question 1: A 43-year-old woman was admitted to the hospital for anticoagulation following a pulmonary embolism. She was found to have a deep venous thrombosis on further workup after a long plane ride coming back from visiting China. She denies any personal history of blood clots in her past, but she says that her mother has also had to be treated for pulmonary embolism in the recent past. Her past medical history is significant for preeclampsia, hypertension, polycystic ovarian syndrome, and hypercholesterolemia. She currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and she currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 111/min, and respiratory rate 23/min. On physical examination, her pulses are bounding and complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 81% on room air, with a new oxygen requirement of 8 L by face mask. On day 6 of combined heparin and warfarin anticoagulation, her platelet count decreases from 182,000/mcL to 63,000/mcL. Her international normalized ratio (INR) is not yet therapeutic. What is the next best step in therapy?
- A. Continue heparin and warfarin until INR is therapeutic for 24 hours
- B. Discontinue heparin and warfarin (Correct Answer)
- C. Continue heparin and warfarin, and administer vitamin K
- D. Discontinue heparin; continue warfarin
- E. Continue heparin; discontinue warfarin
Anticoagulation in ACS Explanation: ***Discontinue heparin and warfarin***
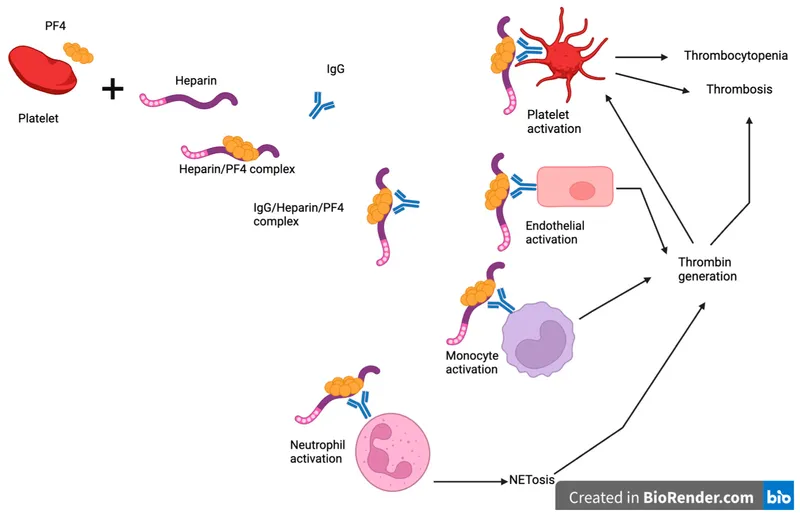
- The significant drop in platelet count (from 182,000 to 63,000/mcL) on day 6 of heparin therapy strongly suggests **heparin-induced thrombocytopenia (HIT)**, an immune-mediated adverse drug reaction.
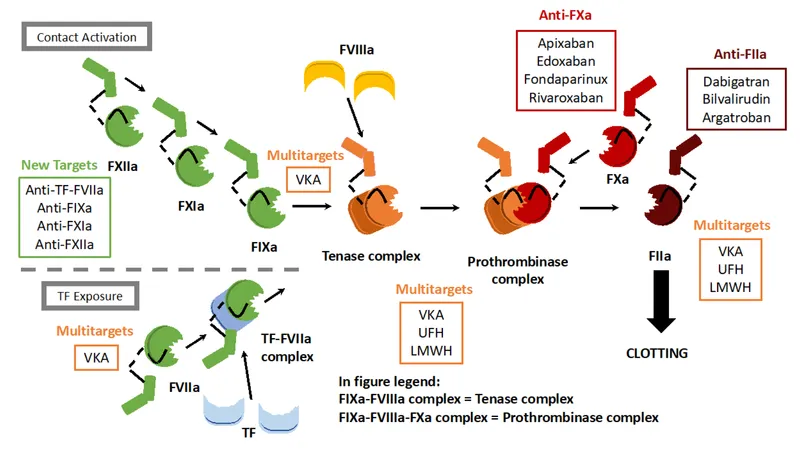
- **Immediate management requires:** (1) discontinuation of ALL heparin products, and (2) initiation of an alternative non-heparin anticoagulant such as a direct thrombin inhibitor (argatroban, bivalirudin) or fondaparinux.
- Warfarin must NOT be continued as monotherapy in HIT because it causes transient **hypercoagulability** due to depletion of protein C and S before depleting clotting factors, which can worsen thrombotic complications.
- **Among the options provided**, discontinuing both heparin and warfarin is the correct first step, with the understanding that alternative anticoagulation would be initiated immediately in practice.
*Continue heparin and warfarin until INR is therapeutic for 24 hours*
- Continuing heparin would be dangerous given the suspected **HIT**, as it could lead to further platelet activation, worsening thrombocytopenia, and an increased risk of **paradoxical thrombosis**.
- While achieving therapeutic anticoagulation is important for PE/DVT, the priority is managing the acute, life-threatening complication of HIT.
*Continue heparin and warfarin, and administer vitamin K*
- Administering vitamin K would reverse warfarin effects, which is contraindicated in a patient requiring anticoagulation for PE and DVT unless there is active bleeding or supratherapeutic INR.
- Continuing heparin in the setting of suspected **HIT** is contraindicated and would exacerbate the prothrombotic state.
*Discontinue heparin; continue warfarin*
- While discontinuing heparin is correct in suspected **HIT**, continuing warfarin alone is **dangerous** and contraindicated.
- Warfarin monotherapy in acute HIT causes transient **hypercoagulability** due to rapid depletion of protein C and S (shorter half-lives) before depletion of clotting factors II, IX, and X, leading to increased thrombotic risk including **warfarin-induced venous limb gangrene**.
- An **alternative non-heparin anticoagulant** (direct thrombin inhibitor or fondaparinux) must be initiated before warfarin can be safely restarted.
*Continue heparin; discontinue warfarin*
- Continuing heparin in the presence of a rapid and significant drop in platelet count is **contraindicated** due to the high suspicion of **HIT**.
- Discontinuing warfarin alone would leave the patient exposed to continued HIT complications while still receiving the offending agent (heparin).
Anticoagulation in ACS US Medical PG Question 2: A primary care physician who focuses on treating elderly patients is researching recommendations for secondary prevention. She is particularly interested in recommendations regarding aspirin, as she has several patients who ask her if they should take it. Of the following, which patient should be started on lifelong aspirin as monotherapy for secondary prevention of atherosclerotic cardiovascular disease?
- A. An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits
- B. A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago
- C. A 67-year-old female who has diabetes mellitus and atrial fibrillation
- D. A 45-year-old female with no health problems
- E. A 63-year-old male with a history of a transient ischemic attack (Correct Answer)
Anticoagulation in ACS Explanation: **A 63-year-old male with a history of a transient ischemic attack**
- A patient with a history of **Transient Ischemic Attack (TIA)** has a high risk of subsequent stroke and should be on **lifelong aspirin monotherapy** for secondary prevention of **atherosclerotic cardiovascular disease (ASCVD)**.
- Aspirin helps prevent further thrombotic events by inhibiting platelet aggregation, making it a cornerstone for secondary prevention after TIA or ischemic stroke.
*An 83-year-old female with a history of a hemorrhagic stroke 1 year ago without residual deficits*
- Aspirin is generally **contraindicated** in patients with a history of **hemorrhagic stroke** due to the increased risk of recurrent bleeding.
- In such cases, the risks of aspirin therapy typically **outweigh the benefits** for cardiovascular prevention.
*A 75-year-old male who had a drug-eluting coronary stent placed 3 days ago*
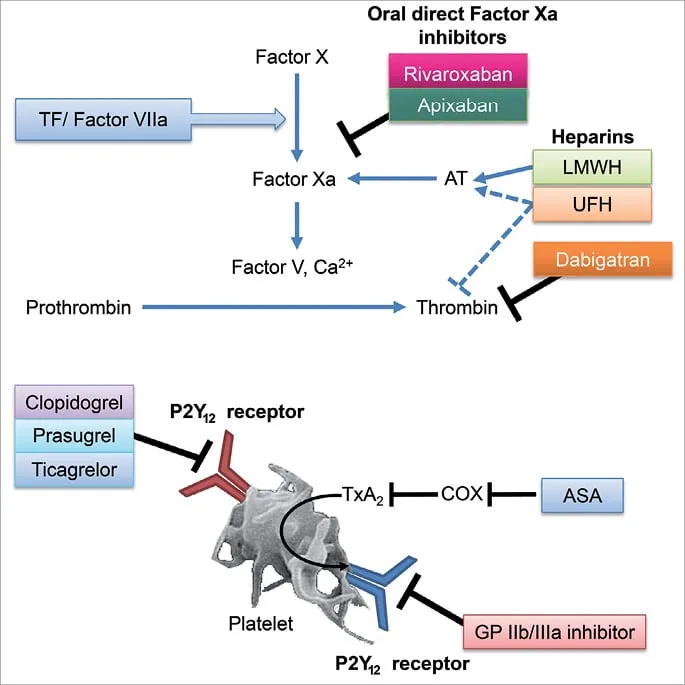
- A patient with a recently placed **drug-eluting stent (DES)** requires **dual antiplatelet therapy (DAPT)**, typically aspirin plus a P2Y12 inhibitor, for a specific duration (e.g., 6-12 months), not aspirin monotherapy.
- Monotherapy with aspirin alone would be **insufficient** to prevent stent thrombosis in the immediate post-stenting period.
*A 67-year-old female who has diabetes mellitus and atrial fibrillation*
- This patient has two significant risk factors requiring specific management: **diabetes mellitus** for cardiovascular risk and **atrial fibrillation** for stroke risk.
- For atrial fibrillation, **anticoagulation with warfarin or a direct oral anticoagulant (DOAC)** is typically indicated, which makes aspirin monotherapy either unnecessary or potentially harmful if used alone.
*A 45-year-old female with no health problems*
- There is no indication for **aspirin primary prevention** in this patient, especially given the increased risk of bleeding without a clear cardiovascular benefit.
- Guidelines currently recommend against routine aspirin use for primary prevention in healthy individuals due to the **unfavorable risk-benefit ratio**.
Anticoagulation in ACS US Medical PG Question 3: A 71-year-old man develops worsening chest pressure while shoveling snow in the morning. He tells his wife that he has a squeezing pain that is radiating to his jaw and left arm. His wife calls for an ambulance. On the way, he received chewable aspirin and 3 doses of sublingual nitroglycerin with little relief of pain. He has borderline diabetes and essential hypertension. He has smoked 15–20 cigarettes daily for the past 37 years. His blood pressure is 172/91 mm Hg, the heart rate is 111/min and the temperature is 36.7°C (98.0°F). On physical examination in the emergency department, he looks pale, very anxious and diaphoretic. His ECG is shown in the image. Troponin levels are elevated. Which of the following is the best next step in the management of this patient condition?
- A. CT scan of the chest with contrast
- B. Echocardiography
- C. Fibrinolysis
- D. Clopidogrel, atenolol, anticoagulation and monitoring (Correct Answer)
- E. Oral nifedipine
Anticoagulation in ACS Explanation: ***Clopidogrel, atenolol, anticoagulation and monitoring***
- The ECG shows **ST depression in multiple leads (II, III, aVF, V3-V6)** and **ST elevation in aVR and V1**, which is highly suggestive of **non-ST elevation myocardial infarction (NSTEMI)** or a **posterior MI/extensive anterior ischemia**. Given the elevated troponin, the patient has an NSTEMI.
- Initial management for NSTEMI includes **dual antiplatelet therapy (aspirin and clopidogrel)**, **anticoagulation (e.g., heparin)**, and **beta-blockers (atenolol)**, along with continuous monitoring.
*CT scan of the chest with contrast*
- A CT scan with contrast would be indicated if **aortic dissection** was suspected, but the classic ECG findings and elevated troponins point away from that diagnosis as the primary concern.
- While other causes of chest pain should be considered, the **ECG and troponin elevation** make **acute coronary syndrome (ACS)** the most immediate and critical diagnosis.
*Echocardiography*
- Echocardiography is useful for assessing **cardiac function, wall motion abnormalities, and valvular disease**, but it is generally not the immediate next step in an NSTEMI after the initial stabilization and medication.
- It could be performed later to evaluate for complications such as **ventricular dysfunction** or **valvular issues**.
*Fibrinolysis*
- **Fibrinolysis** is indicated for **ST-elevation myocardial infarction (STEMI)** when PCI is not readily available, or for other thrombotic events, but not for NSTEMI.
- In NSTEMI, the primary treatment strategy includes **antiplatelets, anticoagulants**, and often **early invasive procedures (PCI)**, if indicated by risk stratification.
*Oral nifedipine*
- **Nifedipine**, a dihydropyridine calcium channel blocker, can be used for hypertension or angina, but it is **not first-line** therapy for **acute coronary syndrome**.
- **Beta-blockers like atenolol** are preferred in ACS to reduce myocardial oxygen demand and improve outcomes, whereas nifedipine can sometimes acutely worsen ischemia due to reflex tachycardia.
Anticoagulation in ACS US Medical PG Question 4: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
Anticoagulation in ACS Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
Anticoagulation in ACS US Medical PG Question 5: A 56-year-old man comes to the emergency department because of progressive swelling and pain in his left calf for 1 day. He does not have shortness of breath or chest pain. He has hypertension and chronic kidney disease. Current medications include enalapril, aspirin, simvastatin, and vitamin D. His temperature is 100.4°F (38°C), pulse is 84/min, and blood pressure is 135/92 mm Hg. Physical examination shows tenderness and swelling of the left lower extremity. A venous Doppler ultrasonography shows a thrombus in the left popliteal vein. Treatment with unfractionated heparin is begun. Two days later, physical examination shows improvement of symptoms. Laboratory studies at admission and 2 days after admission show:
Admission Two days after admission
Hemoglobin 11.2 g/dL 11.1 g/dL
Leukocyte count 5,500/mm3 6,100/mm3
Platelet count 230,000/mm3 170,000/mm3
Serum
Prothrombin time 12 seconds 13 seconds
Partial thromboplastin time 30 seconds 55 seconds
Estimated glomerular filtration rate 29 mL/min/1.73 m2 28 mL/min/1.73 m2
Which of the following is the most appropriate next step in management?
- A. Switch to warfarin
- B. Obtain serum immunoassay
- C. Switch to enoxaparin
- D. Discontinue heparin and initiate argatroban (Correct Answer)
- E. Continue unfractionated heparin
Anticoagulation in ACS Explanation: ***Discontinue heparin and initiate argatroban***
- The **26% drop in platelet count** (from 230,000 to 170,000/mm³) occurring **2 days after starting unfractionated heparin (UFH)** raises high suspicion for **heparin-induced thrombocytopenia (HIT)**.
- When HIT is suspected (intermediate to high probability by 4T score), the **most critical next step** is to **immediately discontinue all heparin products** and **start a non-heparin anticoagulant**.
- **Argatroban** is the preferred alternative in this patient with **chronic kidney disease (eGFR 28 mL/min)** as it is hepatically metabolized and safe in renal impairment.
- HIT antibody testing should be obtained concurrently, but **therapeutic anticoagulation must not be delayed** while awaiting results.
*Obtain serum immunoassay*
- While **HIT antibody testing** (heparin-PF4 immunoassay) should be obtained to confirm the diagnosis, it is **not the most appropriate next step**.
- The priority is to **stop heparin exposure immediately** and provide alternative anticoagulation to prevent thrombotic complications.
- Testing can and should be done concurrently with changing anticoagulation.
*Switch to warfarin*
- Initiating **warfarin alone** in suspected or confirmed HIT is **contraindicated** and can cause **venous limb gangrene** due to rapid depletion of protein C before clotting factors.
- Warfarin should only be started after platelet count recovery (>150,000/mm³) and after at least 5 days of therapeutic non-heparin anticoagulation.
*Switch to enoxaparin*
- **Enoxaparin** (low-molecular-weight heparin) has **>90% cross-reactivity** with HIT antibodies.
- Switching to LMWH in suspected HIT is **contraindicated** as it will perpetuate platelet activation and thrombosis.
*Continue unfractionated heparin*
- Continuing UFH with a significant **platelet drop** is dangerous and will worsen **HIT**, leading to life-threatening **arterial and venous thrombosis**.
- Immediate discontinuation is imperative.
Anticoagulation in ACS US Medical PG Question 6: Drug A is an experimental compound being investigated for potential use as a protectant against venous thrombosis. Binding assays reveal that the drug’s primary mechanism of action is to block carboxylation of glutamic acid residues in certain serum proteins. Drug A is most similar to which of the following:
- A. Streptokinase
- B. Bivalirudin
- C. Warfarin (Correct Answer)
- D. Heparin
- E. Rivaroxaban
Anticoagulation in ACS Explanation: ***Warfarin***
- Warfarin inhibits **vitamin K epoxide reductase**, enzyme responsible for regenerating active vitamin K.
- Active vitamin K is a cofactor for the **gamma-carboxylation of glutamic acid residues** on factors II, VII, IX, X and protein C and S. Thus, warfarin blocks their activation, inhibiting coagulation.
*Steptokinase*
- **Streptokinase** is a **thrombolytic drug** that catalyzes the conversion of **plasminogen to plasmin**, an enzyme that degrades fibrin clots.
- Its mechanism of action is focused on **breaking down existing clots**, rather than preventing their formation by affecting coagulation factor synthesis.
*Bivalirudin*
- **Bivalirudin** is a direct **thrombin inhibitor**, binding directly to the active site and exosite I of thrombin to prevent its action.
- It does not interfere with the **carboxylation of glutamic acid residues** but rather directly inhibits the final common pathway of coagulation.
*Heparin*
- **Heparin** works by potentiating the action of **antithrombin III**, which in turn inactivates thrombin and factor Xa.
- Its mechanism involves accelerating the natural anticoagulant system, rather than inhibiting the **synthesis or activation of coagulation factors** through carboxylation.
*Rivaroxaban*
- **Rivaroxaban** is a **direct factor Xa inhibitor**, which blocks the activity of free and clot-bound factor Xa.
- It directly interferes with the coagulation cascade downstream of the carboxylation step, and does not affect the **vitamin K-dependent carboxylation process**.
Anticoagulation in ACS US Medical PG Question 7: A 35-year-old woman is brought to the emergency department 30 minutes after the onset of severe dyspnea. On arrival, she is unresponsive. Her pulse is 160/min, respirations are 32/min, and blood pressure is 60/30 mm Hg. CT angiography of the chest shows extensive pulmonary embolism in both lungs. She is given a drug that inhibits both thrombin and factor Xa. Which of the following medications was most likely administered?
- A. Fondaparinux
- B. Ticagrelor
- C. Unfractionated heparin (Correct Answer)
- D. Apixaban
- E. Tenecteplase
Anticoagulation in ACS Explanation: ***Unfractionated heparin***
- **Unfractionated heparin** inhibits both **thrombin (factor IIa)** and **factor Xa** by binding to **antithrombin III**, which then inactivates these coagulation factors.
- Given the patient's severe, life-threatening **pulmonary embolism** with **hemodynamic instability** (shock, unresponsive, severe hypotension), rapid-acting intravenous unfractionated heparin is the anticoagulant of choice for immediate effect.
*Fondaparinux*
- **Fondaparinux** is a synthetic **pentasaccharide** that selectively inhibits **factor Xa** but does not directly inhibit thrombin.
- It is typically administered subcutaneously and has a slower onset of action compared to intravenous unfractionated heparin, making it less suitable for emergent, life-threatening situations where immediate full anticoagulation is critical.
*Ticagrelor*
- **Ticagrelor** is an **oral antiplatelet agent** that works by inhibiting the P2Y12 receptor on platelets, preventing platelet aggregation.
- It does not inhibit thrombin or factor Xa and is primarily used in acute coronary syndromes to prevent arterial thrombosis, not for acute treatment of venous thromboembolism like pulmonary embolism.
*Apixaban*
- **Apixaban** is an **oral direct factor Xa inhibitor** that does not inhibit thrombin.
- While effective for venous thromboembolism, its oral administration means a slower onset of action and it is generally not used as the initial anticoagulant for hemodynamically unstable pulmonary embolism where immediate, titratable intravenous anticoagulation is required.
*Tenecteplase*
- **Tenecteplase** is a **fibrinolytic (thrombolytic) agent** that works by converting plasminogen to plasmin, leading to the breakdown of fibrin clots.
- While it is a treatment option for massive pulmonary embolism with hemodynamic instability, it is not an anticoagulant and does not inhibit thrombin or factor Xa; its mechanism of action is clot lysis, not preventing new clot formation via coagulation factor inhibition.
Anticoagulation in ACS US Medical PG Question 8: A 74-year-old man presents to the emergency department with shortness of breath that started about 30 minutes ago. He is also experiencing chest pain on deep inspiration. He has several significant medical conditions including chronic obstructive pulmonary disease, hypertension, and dyslipidemia. He used to smoke about 3 packs of cigarettes every day until last year when he quit. He was in the emergency room 2 weeks ago for a hemorrhagic stroke which was promptly treated. He currently weighs 97.5 kg (215 lb). His respirations are 20/min, the blood pressure is 110/80 mm Hg, and the pulse is 105/min. On physical examination, Homan's sign is positive. An ECG and chest X-ray are performed. His current oxygen saturation is at 87% and D-dimer results are positive. He is wheeled in for a CT scan. What is the most appropriate initial treatment for this patient?
- A. Subcutaneous fondaparinux
- B. Greenfield filter (Correct Answer)
- C. Surgical thrombectomy
- D. Unfractionated heparin
- E. Warfarin
Anticoagulation in ACS Explanation: ***Greenfield filter (IVC filter)***
- This patient presents with **acute pulmonary embolism (PE)** evidenced by sudden **shortness of breath**, **pleuritic chest pain**, **tachycardia (105/min)**, **hypoxemia (87%)**, and **positive D-dimer**. The positive **Homan's sign** suggests deep vein thrombosis as the source.
- The critical factor is his **recent hemorrhagic stroke 2 weeks ago**, which represents an **absolute contraindication to anticoagulation** in the acute/subacute period due to the high risk of re-bleeding.
- **IVC filter placement** is specifically indicated for patients with **venous thromboembolism (VTE) who have contraindications to anticoagulation**, which precisely describes this clinical scenario.
- The filter prevents further emboli from reaching the lungs while avoiding the bleeding risks associated with anticoagulants.
*Subcutaneous fondaparinux*
- While **fondaparinux** is a factor Xa inhibitor commonly used for PE treatment, it is still an **anticoagulant** that significantly increases bleeding risk.
- A **recent hemorrhagic stroke (2 weeks ago)** is an **absolute contraindication** to any form of anticoagulation, including fondaparinux, due to the substantial risk of intracranial re-bleeding.
- Standard guidelines recommend avoiding anticoagulation for at least 2-4 weeks (often longer) after intracranial hemorrhage.
*Unfractionated heparin*
- **Unfractionated heparin (UFH)** is a standard treatment for acute PE but is absolutely **contraindicated** in this patient due to the **recent hemorrhagic stroke**.
- UFH would carry an unacceptable risk of causing recurrent intracranial bleeding in the subacute post-stroke period.
*Surgical thrombectomy*
- **Surgical embolectomy** is reserved for patients with **massive PE causing hemodynamic instability** (cardiogenic shock, persistent hypotension) who have failed or have contraindications to thrombolysis.
- This patient is **hemodynamically stable** with a blood pressure of 110/80 mmHg, making surgical intervention unnecessarily invasive and inappropriate as initial management.
*Warfarin*
- **Warfarin** is an oral anticoagulant used for long-term VTE management but has a **slow onset of action** (requires 5-7 days to reach therapeutic levels), making it unsuitable for acute PE treatment.
- More importantly, like all anticoagulants, warfarin is **absolutely contraindicated** in this patient due to the recent hemorrhagic stroke and high re-bleeding risk.
Anticoagulation in ACS US Medical PG Question 9: A 61-year-old man presents to the primary care clinic to establish care. He has not seen a physician for many years. He has no complaints or concerns but, on further questioning, does have some vague abdominal discomfort. He has no known past medical history and takes no medications. His social history is notable for injecting heroin throughout his late-teens and 20s, but he has been clean and sober for over a decade. At the clinic, the vital signs include: heart rate 90/min, respiratory rate 17/min, blood pressure 110/65 mm Hg, and temperature 37.0°C (98.6°F). The physical exam shows a slightly distended abdomen. The laboratory studies are notable for a platelet count of 77,000/uL and an international normalized ratio (INR) of 1.7. Which of the following is the next best step in the diagnosis of this patient?
- A. Bone marrow biopsy
- B. HIV ELISA
- C. Hepatitis C antibody (Correct Answer)
- D. Platelet aggregation assay
- E. Anti-nuclear antibody test
Anticoagulation in ACS Explanation: ***Hepatitis C antibody***
- The patient's history of **intravenous drug use** and the laboratory findings of **thrombocytopenia** and **elevated INR** strongly suggest chronic liver disease, most commonly caused by **hepatitis C virus (HCV) infection**.
- An **anti-HCV antibody test** is the appropriate initial screening test for HCV infection.
*Bone marrow biopsy*
- A bone marrow biopsy would be considered for unexplained **pancytopenia** or other specific hematological disorders, but the current clinical picture points to a more likely extra-medullary cause for the cytopenias related to liver disease.
- While it could identify issues with platelet production, it's not the first step when liver dysfunction is highly suspected.
*HIV ELISA*
- While a history of intravenous drug use is a risk factor for **HIV**, the patient's current symptoms and lab findings (thrombocytopenia, elevated INR, abdominal discomfort) are more characteristic of **chronic liver disease** rather than primary HIV complications.
- HIV testing would be reasonable as part of general health screening for this patient population, but it is not the *next best step* for the presenting concerns.
*Platelet aggregation assay*
- This assay evaluates platelet function, which is useful for diagnosing qualitative platelet disorders (e.g., Glanzmann's thrombasthenia, Bernard-Soulier syndrome).
- This patient has **thrombocytopenia** (low platelet *count*), not a functional disorder, and the elevated INR points away from primary platelet dysfunction.
*Anti-nuclear antibody test*
- An **ANA test** is used to screen for autoimmune diseases like **Systemic Lupus Erythematosus (SLE)**.
- While SLE can cause thrombocytopenia, the constellation of an elevated INR and a history of intravenous drug use makes liver disease a much more probable cause of the patient's symptoms.
Anticoagulation in ACS US Medical PG Question 10: A 64-year-old man comes to the emergency department complaining of fatigue and abdominal distension. He has a remote history of intravenous drug use. Vital signs include a normal temperature, blood pressure of 120/80 mm Hg, and a pulse of 75/min. Physical examination reveals jaundice and a firm liver. Abdominal ultrasonography shows liver surface nodularity, moderate splenomegaly, and increased diameter of the portal vein. Complete blood count of the patient is shown:
Hemoglobin 14 g/dL
Mean corpuscular volume 90/μm3
Mean corpuscular hemoglobin 30 pg/cell
Mean corpuscular hemoglobin concentration 34%
Leukocyte count 7,000/mm3
Platelet count 50,000/mm3
Which of the following best represents the mechanism of low platelet count in this patient?
- A. Platelet sequestration (Correct Answer)
- B. Dilutional effect
- C. Bone marrow-based disorder
- D. Increased platelet clearance
- E. Genetic disorder
Anticoagulation in ACS Explanation: ***Platelet sequestration***
- The patient's history of IV drug use, jaundice, abdominal distension, firm liver, splenomegaly, and increased portal vein diameter are highly suggestive of **portal hypertension** due to **cirrhosis**, which often leads to **splenomegaly**.
- An enlarged spleen (splenomegaly) sequesters a disproportionately high percentage of the body's platelets, leading to **thrombocytopenia**, even if total platelet production is normal.
- **Splenic sequestration** is the **primary mechanism** of thrombocytopenia in cirrhosis with portal hypertension; up to **90% of platelets** can be sequestered in an enlarged spleen.
- Additionally, the diseased liver produces less **thrombopoietin (TPO)**, which contributes to reduced platelet production, but sequestration remains the dominant mechanism.
*Dilutional effect*
- A dilutional effect on platelet count typically occurs with **massive transfusions** of packed red blood cells and crystalloids, which is not indicated in this patient's presentation.
- While fluid overload can dilute blood components, the patient's symptoms point specifically to a **liver pathology** and related complications, not simply volume expansion.
*Bone marrow-based disorder*
- A primary bone marrow disorder would likely affect other cell lines as well, but the patient's hemoglobin and leukocyte counts are within normal limits, making a general **bone marrow suppression** less likely.
- Furthermore, the strong evidence of **cirrhosis and portal hypertension** provides a more direct and common explanation for isolated thrombocytopenia in this context.
*Increased platelet clearance*
- While increased platelet clearance can cause thrombocytopenia (e.g., in immune thrombocytopenia or thrombotic microangiopathies), there are no signs of increased destruction or consumption in this case.
- Conditions involving increased clearance usually present with other features like petechiae, purpura, or schistocytes, which are not mentioned.
- The clinical picture is most consistent with **sequestration** rather than **destruction**.
*Genetic disorder*
- Genetic disorders causing thrombocytopenia typically present much earlier in life or have a family history, which does not fit this patient's age and clinical presentation.
- The patient's history of **IV drug use** and the findings of advanced liver disease indicate an **acquired condition**, not a congenital one.
More Anticoagulation in ACS US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.