ACS pathophysiology and classification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for ACS pathophysiology and classification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
ACS pathophysiology and classification US Medical PG Question 1: A 28-year-old male presents with sharp, stabbing chest pain that worsens when lying flat and improves when sitting forward. He reports a recent viral upper respiratory infection 2 weeks ago. On examination, a friction rub is heard on auscultation. His vital signs are stable.
An ECG is most likely to show which of the following findings in this patient?
- A. Diffuse, concave ST-segment elevations (Correct Answer)
- B. Peaked T waves and ST-segment elevations in leads V1-V6
- C. Sawtooth-appearance of P waves
- D. S waves in lead I, Q waves in lead III, and inverted T waves in lead III
- E. Alternating high and low amplitude QRS complexes
ACS pathophysiology and classification Explanation: ***Diffuse, concave ST-segment elevations***
- This is a hallmark ECG finding in **acute pericarditis**, along with **PR segment depression**, due to widespread inflammation of the epicardium.
- The chest pain described here (sharp, stabbing, worse when lying flat, improved by sitting forward) paired with a recent viral infection and a pericardial friction rub, is highly characteristic of **pericarditis**.
*Peaked T waves and ST-segment elevations in leads V1-V6*
- **Peaked T waves** are typically seen in early stages of hyperkalemia or myocardial ischemia, while **ST-segment elevations in specific leads (V1-V6)** are more indicative of an **ST-elevation myocardial infarction (STEMI)** involving the anterior wall.
- The diffuse nature of ST elevation in pericarditis, as opposed to regional changes, along with **PR depression**, differentiates it from STEMI.
*Sawtooth-appearance of P waves*
- A **sawtooth appearance of P waves** (often referred to as 'f waves') is characteristic of **atrial flutter**, a type of supraventricular tachycardia.
- This finding is unrelated to pericarditis, which primarily affects the pericardium and not the atrial electrical activity in this specific manner.
*S waves in lead I, Q waves in lead III, and inverted T waves in lead III*
- This pattern, known as the **S1Q3T3 pattern**, is a classic (though not always present) ECG finding suggestive of **acute pulmonary embolism**.
- While pulmonary embolism can cause chest pain, its presentation differs significantly from the positional relief and friction rub seen in pericarditis.
*Alternating high and low amplitude QRS complexes*
- This ECG finding, known as **electrical alternans**, is highly specific for a large **pericardial effusion** or **cardiac tamponade**, where the heart swings within the fluid-filled pericardial sac.
- Although pericarditis can lead to effusion, the presence of a friction rub and stable vital signs suggests acute pericarditis without significant tamponade at this stage, making diffuse ST elevation a more likely initial finding.
ACS pathophysiology and classification US Medical PG Question 2: A 74-year-old man presents with complaints of sudden severe crushing retrosternal pain. The pain radiated to his left arm shortly after it began, and he was subsequently rushed to the emergency department for evaluation. His troponins and creatine kinase-MB (CK-MB) were elevated. Unfortunately, the patient died within the next 2 hours and an autopsy was performed immediately. The gross examination of the heart will show?
- A. White, patchy, non-contractile scar
- B. Normal heart tissue (Correct Answer)
- C. Pallor of the infarcted tissue
- D. Abundant neutrophils
- E. Red granulation tissue surrounding the infarction
ACS pathophysiology and classification Explanation: ***Normal heart tissue***
- At **0-4 hours** following a myocardial infarction, the heart muscle shows **no gross changes** on autopsy examination.
- Although **coagulative necrosis** begins at the cellular level within minutes, these microscopic changes are **not visible** to the naked eye during gross examination.
- The patient died within **2 hours** of symptom onset, which falls within this early window where the heart appears **grossly normal** despite the acute infarction.
- Elevated **cardiac enzymes** (troponins, CK-MB) confirm myocardial injury has occurred, but gross pathological changes lag behind biochemical and microscopic changes.
*Pallor of the infarcted tissue*
- **Pallor** (pale discoloration) of infarcted myocardium typically becomes visible on gross examination at **4-12 hours** post-infarction.
- At 2 hours, this change has not yet developed sufficiently to be visible on gross inspection.
- Pallor results from **edema** and the accumulation of dead cells, which takes several hours to manifest grossly.
*White, patchy, non-contractile scar*
- A **white fibrotic scar** is characteristic of a **healed myocardial infarction**, which takes **several weeks to months** to form.
- This represents complete replacement of necrotic tissue by **collagenous scar tissue** (fibrosis).
- This is a chronic finding, not an acute one.
*Abundant neutrophils*
- **Neutrophil infiltration** is a microscopic finding that typically begins around **12-24 hours** after infarction, becoming abundant over the following days.
- Even when present, neutrophils are not visible on **gross examination**—they require microscopic evaluation.
- At 2 hours post-infarction, neutrophils have not yet migrated to the infarcted area.
*Red granulation tissue surrounding the infarction*
- **Granulation tissue** formation begins around **3-7 days** after infarction and involves proliferation of **capillaries** and **fibroblasts**.
- Grossly, this appears as a **hyperemic border** with central yellow softening.
- This represents the healing phase and would not be present within 2 hours of symptom onset.
ACS pathophysiology and classification US Medical PG Question 3: A 59-year-old man with angina pectoris comes to the physician because of a 6-month history of shortness of breath on exertion that improves with rest. He has hypertension and hyperlipidemia. Current medications include aspirin, metoprolol, and nitroglycerine. Echocardiography shows left ventricular septal and apical hypokinesis. Cardiac catheterization shows 96% occlusion of the left anterior descending artery. The patient undergoes angioplasty and placement of a stent. The patient's shortness of breath subsequently resolves and follow-up echocardiography one week later shows normal regional contractile function. Which of the following is the most accurate explanation for the changes in echocardiography?
- A. Myocardial scarring
- B. Unstable angina pectoris
- C. Stress cardiomyopathy
- D. Hibernating myocardium (Correct Answer)
- E. Cardiac remodeling
ACS pathophysiology and classification Explanation: ***Hibernating myocardium***
- This refers to chronically **ischemic but viable myocardium** that shows reduced contractility at rest due to persistent hypoperfusion, which improves or normalizes after revascularization.
- The resolution of symptoms and normalization of regional contractile function after stent placement in this patient with chronic angina and a highly occluded LAD artery is highly consistent with this phenomenon.
*Myocardial scarring*
- **Myocardial scarring** represents irreversible damage and fibrosis, typically resulting from a myocardial infarction (heart attack).
- Scarred tissue does not regain contractile function even after revascularization; the observed improvement in contractility rules out this explanation.
*Unstable angina pectoris*
- **Unstable angina** is characterized by new-onset angina, crescendo angina, or angina at rest, indicating an acute coronary syndrome.
- While the patient had angina, the prompt and complete resolution of contractile dysfunction post-revascularization points to a chronic ischemic state rather than an acute, potentially irreversible event or a transient episode of unstable angina that would not cause such persistent functional changes.
*Stress cardiomyopathy*
- Also known as **Takotsubo cardiomyopathy**, this condition involves transient left ventricular dysfunction, often triggered by severe emotional or physical stress, mimicking a myocardial infarction.
- It typically resolves spontaneously over weeks or months and is not caused by fixed coronary artery occlusion that improves with revascularization via stenting.
*Cardiac remodeling*
- **Cardiac remodeling** refers to changes in the size, shape, and function of the heart in response to chronic stress, such as hypertension or chronic ischemia.
- While the patient's long-standing hypertension and hyperlipidemia could lead to some remodeling, the rapid and complete improvement in regional contractility specifically after LAD revascularization best explains the phenomenon as hibernating myocardium, a specific type of physiological adaptation, rather than general remodeling.
ACS pathophysiology and classification US Medical PG Question 4: A 66-year-old man comes to the emergency department because of a 1-day history of chest pain, palpitations, and dyspnea on exertion. He had a similar episode 3 days ago and was diagnosed with an inferior wall myocardial infarction. He was admitted and a percutaneous transluminal coronary angioplasty was successfully done that day. A fractional flow reserve test during the procedure showed complete resolution of the stenosis. Laboratory tests including serum glucose, lipids, and blood count were within normal limits. He was discharged the day after the procedure on a drug regimen of aspirin, simvastatin, and isosorbide dinitrate. At the time of discharge, he had no chest pain or dyspnea. Presently, his vitals are normal and ECG at rest shows new T-wave inversion. Which of the following is the most reliable test for rapidly establishing the diagnosis in this patient?
- A. Creatine kinase MB
- B. Lactate dehydrogenase
- C. Copeptin
- D. Aspartate aminotransferase
- E. Cardiac troponin T (Correct Answer)
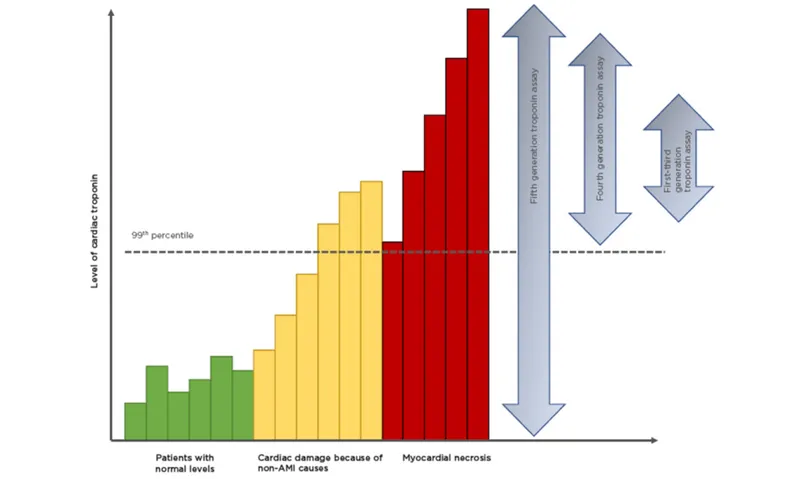
ACS pathophysiology and classification Explanation: ***Cardiac troponin T***
- **Cardiac troponin T** is a highly sensitive and specific biomarker for **myocardial injury**, making it the most reliable test for rapidly diagnosing acute coronary syndrome or re-infarction.
- Its elevation indicates ongoing **myocardial necrosis**, even after a recent MI, and is crucial for guiding immediate management.
*Creatine kinase MB*
- While CK-MB is used for diagnosing myocardial infarction, its levels can also be elevated in cases of **skeletal muscle injury** or **after cardiac procedures**, reducing its specificity in this context.
- CK-MB also has a **shorter window of elevation** compared to troponins, potentially missing later presentations of myocardial injury.
*Lactate dehydrogenase*
- **LDH** is a relatively **nonspecific marker** that can elevate due to various conditions affecting different organs (e.g., liver disease, hemolysis, renal injury).
- Its elevation onset is **slower** and its diagnostic window is longer, making it less suitable for rapid diagnosis of acute myocardial injury.
*Copeptin*
- **Copeptin** is a marker of **endogenous stress** and is often used in conjunction with troponins to rule out NSTEMI, especially at early presentation.
- However, it is not a direct marker of myocardial necrosis itself and is **not as specific** as troponin for diagnosing a re-infarction.
*Aspartate aminotransferase*
- **AST** is a **nonspecific enzyme** found in various tissues, including the liver, skeletal muscle, and heart.
- Elevated AST levels are frequently seen in **liver damage** and are not a primary biomarker for diagnosing acute myocardial infarction or re-infarction.
ACS pathophysiology and classification US Medical PG Question 5: A 56-year-old male died in a motor vehicle accident. Autopsy reveals extensive atherosclerosis of his left anterior descending artery marked by intimal smooth muscle and collagen proliferation. Which of the following is implicated in recruiting smooth muscle cells from the media to intima in atherosclerotic lesions?
- A. Vascular endothelial growth factor
- B. Platelet-derived growth factor (Correct Answer)
- C. Factor V Leiden
- D. IgE
- E. Prostacyclin
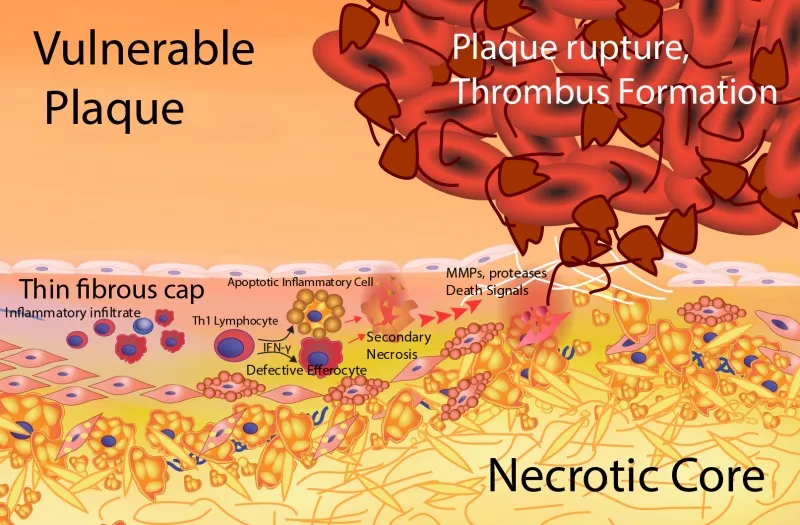
ACS pathophysiology and classification Explanation: ***Platelet-derived growth factor***
- **Platelet-derived growth factor (PDGF)** is a crucial **chemotactic** and **mitogenic** factor for **smooth muscle cells (SMCs)**, promoting their migration from the tunica media to the tunica intima and subsequent proliferation in atherosclerotic lesions.
- Released by activated platelets, macrophages, and endothelial cells, PDGF contributes significantly to the **fibroproliferative response** seen in **atherosclerosis**.
*Vascular endothelial growth factor*
- **Vascular endothelial growth factor (VEGF)** is primarily involved in **angiogenesis** and **vascular permeability**.
- While angiogenesis can play a role in advanced atherosclerotic plaques, VEGF is not the primary mediator of **smooth muscle cell migration** and proliferation into the intima.
*Factor V Leiden*
- **Factor V Leiden** is a **genetic mutation** that increases the risk of **thrombosis** due to resistance to inactivation by activated protein C.
- It is a risk factor for **venous thromboembolism** and does not directly recruit smooth muscle cells to the intima in atherosclerosis.
*IgE*
- **Immunoglobulin E (IgE)** is an antibody class primarily involved in **allergic reactions** and **parasitic infections**.
- IgE has no direct role in the recruitment or proliferation of **smooth muscle cells** in the context of atherosclerosis.
*Prostacyclin*
- **Prostacyclin (PGI2)** is a **vasodilator** and a potent **inhibitor of platelet aggregation**.
- It works to prevent thrombus formation and has a protective role against atherosclerosis, rather than promoting **smooth muscle cell migration**.
ACS pathophysiology and classification US Medical PG Question 6: A 47-year-old man presents as a new patient at an outpatient clinic. He has never seen a physician before, but was motivated by his 40-year-old brother's recent heart attack and seeks to optimize his health. In particular, he read that uncontrolled atherosclerosis can lead to a heart attack. Which molecule is downregulated in response to the advent of atherosclerosis?
- A. Tumor necrosis factor
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Interleukin 1
- E. Thromboxane A2
ACS pathophysiology and classification Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is a potent **vasodilator** and **anti-inflammatory** molecule produced by endothelial cells. In atherosclerosis, endothelial dysfunction leads to reduced NO bioavailability.
- Decreased NO production contributes to vasoconstriction, increased platelet aggregation, and enhanced smooth muscle cell proliferation, all of which promote **atherosclerotic plaque formation** and progression.
*Tumor necrosis factor*
- **Tumor necrosis factor-alpha (TNF-α)** is a **pro-inflammatory cytokine** that plays a significant role in the pathogenesis of atherosclerosis.
- It is **upregulated** in response to atherosclerotic plaque formation, contributing to endothelial activation, leukocyte recruitment, and smooth muscle cell proliferation.
*Serotonin*
- **Serotonin (5-hydroxytryptamine)** is primarily known for its role as a neurotransmitter but also acts as a **vasoconstrictor** and promotes platelet aggregation.
- While it can be released from activated platelets in the context of vascular injury, it is not consistently **downregulated** in atherosclerosis; rather, its effects can contribute to disease progression.
*Interleukin 1*
- **Interleukin-1 (IL-1)**, particularly IL-1β, is a major **pro-inflammatory cytokine** critically involved in the immune response in atherosclerosis.
- It is **upregulated** in atherosclerotic plaques, contributing to systemic inflammation, endothelial dysfunction, and vascular smooth muscle cell activation.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is a potent **vasoconstrictor** and **platelet aggregator** produced by activated platelets.
- Its levels are **increased** in atherosclerosis, contributing to hypercoagulability and increased risk of thrombotic events like myocardial infarction.
ACS pathophysiology and classification US Medical PG Question 7: A 72-year-old man comes to the physician because of a 2-month history of intermittent retrosternal chest pain and tightness on exertion. He has type 2 diabetes mellitus, osteoarthritis of the right hip, and hypertension. Current medications include insulin, ibuprofen, enalapril, and hydrochlorothiazide. Vital signs are within normal limits. His troponin level is within the reference range. An ECG at rest shows a right bundle branch block and infrequent premature ventricular contractions. The patient's symptoms are reproduced during adenosine stress testing. Repeat ECG during stress testing shows new ST depression of > 1 mm in leads V2, V3, and V4. Which of the following is the most important underlying mechanism of this patient's ECG changes?
- A. Diversion of blood flow from stenotic coronary arteries (Correct Answer)
- B. Transient atrioventricular nodal blockade
- C. Reduced left ventricular preload
- D. Ruptured cholesterol plaque within a coronary vessel
- E. Increased myocardial oxygen demand
ACS pathophysiology and classification Explanation: ***Diversion of blood flow from stenotic coronary arteries***
- The **adenosine stress test** induces **submaximal coronary vasodilation** in healthy vessels, diverting blood flow away from stenosed areas that are already maximally dilated, a phenomenon known as **coronary steal**.
- This **relative hypoperfusion** in areas supplied by stenotic arteries leads to myocardial ischemia, manifested as **new ST depression** on the ECG due to **subendocardial oxygen supply-demand mismatch**.
*Transient atrioventricular nodal blockade*
- While adenosine can cause transient AV nodal blockade, leading to AV blocks, this would manifest as specific changes in **PR interval** or **QRS drop-out**, not ST segment depression indicative of ischemia.
- The patient's symptoms and ECG changes point towards myocardial ischemia, not an AV conduction disturbance.
*Reduced left ventricular preload*
- Reduced preload can occur in certain cardiac conditions but is not the primary mechanism behind ST depression during an adenosine stress test.
- ECG changes due to reduced preload are usually nonspecific, such as **sinus tachycardia** or **low voltage**, and do not typically cause new ST depression in specific leads.
*Ruptured cholesterol plaque within a coronary vessel*
- A ruptured plaque with subsequent **thrombus formation** would lead to **acute coronary syndrome (ACS)**, characterized by persistent chest pain, **elevated troponins**, and potentially **ST elevation** or new **pathologic Q waves** if complete occlusion occurs.
- The patient's troponin level is normal, and his symptoms are intermittent and reproducible on stress testing, which is more consistent with **stable angina**.
*Increased myocardial oxygen demand*
- While increased myocardial oxygen demand is a component of angina pectoris, adenosine primarily causes **coronary vasodilation**, which can worsen ischemia in stenotic areas by diverting blood flow, rather than directly increasing myocardial oxygen demand itself.
- **Dobutamine stress testing** would be the test that primarily increases myocardial oxygen demand.
ACS pathophysiology and classification US Medical PG Question 8: A 60-year-old African American gentleman presents to the emergency department with sudden onset "vice-like" chest pain, diaphoresis, and pain radiating to his left shoulder. He has ST elevations on his EKG and elevated cardiac enzymes. Concerning his current pathophysiology, which of the following changes would you expect to see in this patient?
- A. No change in cardiac output; decreased venous return
- B. Increased cardiac output; increased systemic vascular resistance
- C. Decreased cardiac output; increased systemic vascular resistance (Correct Answer)
- D. Increased cardiac output; decreased systemic vascular resistance
- E. Decreased cardiac output; decreased venous return
ACS pathophysiology and classification Explanation: ***Decreased cardiac output; increased systemic vascular resistance***
- The patient's symptoms (chest pain, diaphoresis, ST elevations, elevated cardiac enzymes) are classic for an **acute myocardial infarction (MI)**, which directly impairs the heart's pumping function, leading to **decreased cardiac output**.
- In response to decreased cardiac output and reduced tissue perfusion, the body activates the **sympathetic nervous system** and **renin-angiotensin-aldosterone system**, causing **vasoconstriction** and thus **increased systemic vascular resistance** to maintain blood pressure.
*No change in cardiac output; decreased venous return*
- An acute MI significantly compromises the heart's ability to pump blood, meaning **cardiac output will almost certainly change** (decrease).
- While venous return might be affected, it's not the primary compensatory mechanism often leading to **decreased CO** in acute MI, which is largely due to impaired systolic function.
*Increased cardiac output; increased systemic vascular resistance*
- **Increased cardiac output** is highly unlikely in the context of an acute myocardial infarction because the heart muscle is damaged and unable to pump effectively.
- While **increased systemic vascular resistance** occurs as a compensatory mechanism, it's in response to a failed heart, not one that is effectively increasing its output.
*Increased cardiac output; decreased systemic vascular resistance*
- Both **increased cardiac output** and **decreased systemic vascular resistance** are typically signs of a hyperdynamic state (e.g., sepsis in its early stages) or vasodilation, which is contrary to the pathophysiology of an MI.
- An MI causes **cardiac dysfunction** and **compensatory vasoconstriction**, not increased output and vasodilation.
*Decreased cardiac output; decreased venous return*
- While **decreased cardiac output** is expected, **decreased venous return** is not the primary or most impactful immediate systemic response; the body often tries to maintain venous return initially to optimize filling pressures, although severe MI can eventually lead to overall circulatory collapse.
- The more prominent and immediate compensatory mechanism for a failing heart is often **increased systemic vascular resistance** to maintain perfusion pressure.
ACS pathophysiology and classification US Medical PG Question 9: Two days after undergoing an uncomplicated total thyroidectomy, a 63-year-old woman has acute, progressive chest pain. The pain is sharp and burning. She feels nauseated and short of breath. The patient has a history of hypertension, type 1 diabetes mellitus, medullary thyroid cancer, multiple endocrine neoplasia type 2A, anxiety, coronary artery disease, and gastroesophageal reflux disease. She smoked half a pack of cigarettes daily for 24 years but quit 18 years ago. Current medications include lisinopril, insulin glargine, insulin aspart, sertraline, aspirin, ranitidine, and levothyroxine. She appears anxious and diaphoretic. Her temperature is 37.4°C (99.3°F), pulse is 64/min, respirations are 17/min, and blood pressure is 148/77 mm Hg. The lungs are clear to auscultation. Examination shows a 3-cm linear incision over the anterior neck with 1 mm of surrounding erythema and mild serous discharge. The chest wall and abdomen are nontender. There is 5/5 strength in all extremities and decreased sensation to soft touch on the feet bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Obtain an ECG and troponin T levels (Correct Answer)
- B. Administer IV pantoprazole and schedule endoscopy
- C. Discontinue levothyroxine and obtain fT4 levels
- D. Administer IV levofloxacin and obtain chest radiograph
- E. Obtain urine and plasma metanephrine levels
ACS pathophysiology and classification Explanation: **Obtain an ECG and troponin T levels**
- The patient presents with acute, progressive **chest pain that is sharp and burning**, along with nausea and shortness of breath, which are classic symptoms of an acute coronary syndrome, especially given her history of **coronary artery disease**, hypertension, diabetes, and prior smoking.
- An **ECG** and **troponin T levels** are crucial first steps to evaluate for myocardial ischemia or infarction in this high-risk patient.
*Administer IV pantoprazole and schedule endoscopy*
- While the patient has a history of gastroesophageal reflux disease (GERD) and her pain is described as "burning," the **acuteness, progression, and associated symptoms** (nausea, shortness of breath) in a patient with significant cardiac risk factors make a GI cause less likely as the primary concern.
- Empiric treatment for GERD without first ruling out a life-threatening cardiac event would be inappropriate and potentially dangerous.
*Discontinue levothyroxine and obtain fT4 levels*
- The patient is taking levothyroxine after a thyroidectomy for medullary thyroid cancer, but there is no immediate indication of thyroid hormone imbalance (e.g., hyperthyroidism causing chest pain) that would warrant discontinuing her medication or rushing fT4 levels as the first step in an acute chest pain presentation.
- Her pulse of 64/min is not suggestive of hyperthyroidism, which typically causes tachycardia.
*Administer IV levofloxacin and obtain chest radiograph*
- While shortness of breath can be a symptom of pneumonia, the **sharp, burning nature of the chest pain**, coupled with the absence of fever (temperature 37.4°C is mild), cough, or abnormal lung sounds (lungs clear to auscultation), makes an acute infection like pneumonia less probable as the primary diagnosis.
- Antibiotics and a chest radiograph would be considered after ruling out more immediate life-threatening conditions like acute coronary syndrome.
*Obtain urine and plasma metanephrine levels*
- The patient has a history of multiple endocrine neoplasia type 2A (MEN2A), which includes medullary thyroid cancer and can be associated with pheochromocytoma (adrenal tumor secreting catecholamines). However, her blood pressure (148/77 mm Hg) is not acutely elevated to crisis levels, and her symptoms are more consistent with cardiac ischemia than a pheochromocytoma crisis.
- While metanephrine levels would be important for long-term follow-up of MEN2A, they are not the immediate next step for acute chest pain in a patient with known coronary artery disease.
ACS pathophysiology and classification US Medical PG Question 10: A 25-year-old man comes to the emergency department because of a 1-week-history of progressively worsening dyspnea and intermittent chest pain that increases on inspiration. He had an upper respiratory tract infection 2 weeks ago. His pulse is 115/min and blood pressure is 100/65 mm Hg. Examination shows inspiratory crackles bilaterally. His serum troponin I is 0.21 ng/mL (N < 0.1). An x-ray of the chest shows an enlarged cardiac silhouette and prominent vascular markings in both lung fields; costophrenic angles are blunted. A rhythm strip shows inverted T waves. Which of the following additional findings is most likely in this patient's condition?
- A. Opening snap with low-pitched diastolic rumble
- B. Elevated brain natriuretic peptide (Correct Answer)
- C. Sarcomere duplication
- D. Right ventricular dilation
- E. Electrical alternans
ACS pathophysiology and classification Explanation: ***Elevated brain natriuretic peptide***
- This patient presents with symptoms of **dyspnea**, **chest pain**, **tachycardia**, elevated **troponin I**, an enlarged **cardiac silhouette** with prominent vascular markings, and **blunted costophrenic angles**, all consistent with **cardiomyopathy** and heart failure, likely post-viral **myocarditis**.
- **Brain natriuretic peptide (BNP)** is released by myocardial cells in response to ventricular stretch and volume overload, making it a strong indicator for **heart failure**.
*Opening snap with low-pitched diastolic rumble*
- An **opening snap** followed by a **low-pitched diastolic rumble** is characteristic of **mitral stenosis**, a valvular disorder not suggested by the patient's acute presentation and other findings.
- Mitral stenosis would typically be associated with a history of **rheumatic fever** and more specific echocardiographic findings of valve abnormalities.
*Sarcomere duplication*
- **Sarcomere duplication** and disarray are characteristic pathological findings in **hypertrophic cardiomyopathy (HCM)**, an inherited genetic disorder.
- While HCM can cause dyspnea and chest pain, this patient's acute presentation following a viral infection and evidence of fluid overload are more indicative of an **acquired cardiomyopathy** such as myocarditis.
*Right ventricular dilation*
- While the patient has signs of **heart failure**, the chest X-ray shows an **enlarged cardiac silhouette** and **prominent vascular markings in both lung fields** and **blunted costophrenic angles**, suggesting **left ventricular failure** with fluid redistribution and pleural effusions.
- Significant **right ventricular dilation** would typically be associated with signs of right-sided heart failure like **peripheral edema** and **jugular venous distension**, which are not explicitly mentioned as primary findings.
*Electrical alternans*
- **Electrical alternans** is a specific ECG finding characterized by beat-to-beat variation in the QRS amplitude or axis, most commonly associated with **pericardial effusion** leading to cardiac tamponade.
- Although the patient has an enlarged cardiac silhouette, which could indicate effusion, the primary findings point more broadly to **myocardial dysfunction** and **heart failure** rather than tamponade.
More ACS pathophysiology and classification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.