Evidence basis for screening recommendations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Evidence basis for screening recommendations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Evidence basis for screening recommendations US Medical PG Question 1: A randomized controlled trial is conducted investigating the effects of different diagnostic imaging modalities on breast cancer mortality. 8,000 women are randomized to receive either conventional mammography or conventional mammography with breast MRI. The primary outcome is survival from the time of breast cancer diagnosis. The conventional mammography group has a median survival after diagnosis of 17.0 years. The MRI plus conventional mammography group has a median survival of 19.5 years. If this difference is statistically significant, which form of bias may be affecting the results?
- A. Recall bias
- B. Selection bias
- C. Misclassification bias
- D. Because this study is a randomized controlled trial, it is free of bias
- E. Lead-time bias (Correct Answer)
Evidence basis for screening recommendations Explanation: ***Lead-time bias***
- This bias occurs when a screening test diagnoses a disease earlier, making **survival appear longer** even if the actual time of death is unchanged.
- In this scenario, adding **MRI** may detect breast cancer at an earlier, asymptomatic stage, artificially extending the apparent survival duration from diagnosis without necessarily changing the ultimate prognosis.
*Recall bias*
- **Recall bias** applies to retrospective studies where subjects are asked to recall past exposures, and those with the outcome are more likely to remember potential exposures.
- It's irrelevant here as this is a **prospective randomized controlled trial** studying objective survival outcomes, not subjective past recollections.
*Selection bias*
- **Selection bias** occurs when participants are not randomly assigned to groups, leading to systematic differences between the groups influencing the outcome.
- This study is a **randomized controlled trial**, which is designed to minimize selection bias by ensuring participants have an equal chance of being assigned to either treatment arm.
*Misclassification bias*
- **Misclassification bias** happens when either the exposure or the outcome is incorrectly categorized, leading to erroneous associations.
- This study uses objective diagnostic imaging and survival data, thus reducing the likelihood of **misclassification of diagnosis or survival status**.
*Because this study is a randomized controlled trial, it is free of bias*
- While **randomized controlled trials (RCTs)** are considered the **gold standard** for minimizing bias, they are not entirely immune to all forms of bias.
- **Lead-time bias**, for instance, can still occur in RCTs involving screening or early diagnosis, as seen in this example, and other biases like **information bias** or **reporting bias** can also arise.
Evidence basis for screening recommendations US Medical PG Question 2: A scientist in Boston is studying a new blood test to detect Ab to the parainfluenza virus with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity even greater than what she had originally hoped for. She travels to South America to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with the parainfluenza virus. The scientist tests these 1,200 patients’ blood and finds that only 120 of them tested negative with her new test. Of the following options, which describes the sensitivity of the test?
- A. 82%
- B. 86%
- C. 98%
- D. 90% (Correct Answer)
- E. 84%
Evidence basis for screening recommendations Explanation: ***90%***
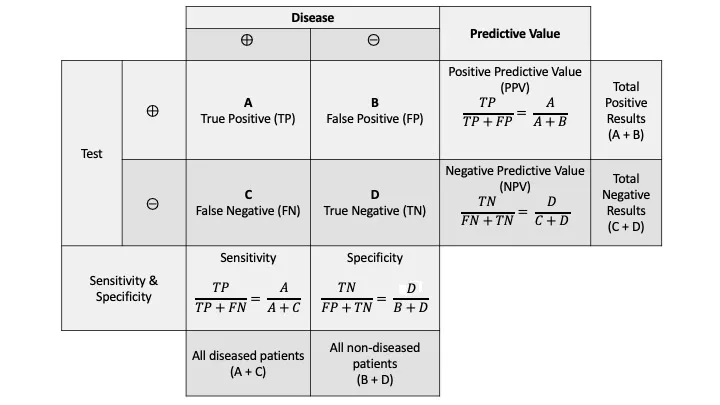
- **Sensitivity** is calculated as the number of **true positives** divided by the total number of individuals with the disease (true positives + false negatives).
- In this scenario, there were 1200 infected patients (total diseased), and 120 of them tested negative (false negatives). Therefore, 1200 - 120 = 1080 patients tested positive (true positives). The sensitivity is 1080 / 1200 = 0.90, or **90%**.
*82%*
- This value was the **original sensitivity** of the test before the scientist improved it.
- The question states that the scientist believes she has achieved a sensitivity "even greater than what she had originally hoped for."
*86%*
- This value is not directly derivable from the given data for the new test's sensitivity.
- It might represent an intermediate calculation or an incorrect interpretation of the provided numbers.
*98%*
- This would imply only 24 false negatives out of 1200 true disease cases, which is not the case (120 false negatives).
- A sensitivity of 98% would be significantly higher than the calculated 90% and the initial stated values.
*84%*
- This value is not derived from the presented data regarding the new test's performance.
- It could be mistaken for an attempt to add 2% to the original 82% sensitivity, but the actual data from the new test should be used.
Evidence basis for screening recommendations US Medical PG Question 3: You are reading through a recent article that reports significant decreases in all-cause mortality for patients with malignant melanoma following treatment with a novel biological infusion. Which of the following choices refers to the probability that a study will find a statistically significant difference when one truly does exist?
- A. Type II error
- B. Type I error
- C. Confidence interval
- D. p-value
- E. Power (Correct Answer)
Evidence basis for screening recommendations Explanation: ***Power***
- **Power** is the probability that a study will correctly reject the null hypothesis when it is, in fact, false (i.e., will find a statistically significant difference when one truly exists).
- A study with high power minimizes the risk of a **Type II error** (failing to detect a real effect).
*Type II error*
- A **Type II error** (or **beta error**) occurs when a study fails to reject a false null hypothesis, meaning it concludes there is no significant difference when one actually exists.
- This is the **opposite** of what the question describes, which asks for the probability of *finding* a difference.
*Type I error*
- A **Type I error** (or **alpha error**) occurs when a study incorrectly rejects a true null hypothesis, concluding there is a significant difference when one does not actually exist.
- This relates to the **p-value** and the level of statistical significance (e.g., p < 0.05).
*Confidence interval*
- A **confidence interval** provides a range of values within which the true population parameter is likely to lie with a certain degree of confidence (e.g., 95%).
- It does not directly represent the probability of finding a statistically significant difference when one truly exists.
*p-value*
- The **p-value** is the probability of observing data as extreme as, or more extreme than, that obtained in the study, assuming the null hypothesis is true.
- It is used to determine statistical significance, but it is not the probability of detecting a true effect.
Evidence basis for screening recommendations US Medical PG Question 4: A research group wants to assess the safety and toxicity profile of a new drug. A clinical trial is conducted with 20 volunteers to estimate the maximum tolerated dose and monitor the apparent toxicity of the drug. The study design is best described as which of the following phases of a clinical trial?
- A. Phase 0
- B. Phase III
- C. Phase V
- D. Phase II
- E. Phase I (Correct Answer)
Evidence basis for screening recommendations Explanation: ***Phase I***
- **Phase I clinical trials** involve a small group of healthy volunteers (typically 20-100) to primarily assess **drug safety**, determine a safe dosage range, and identify side effects.
- The main goal is to establish the **maximum tolerated dose (MTD)** and evaluate the drug's pharmacokinetic and pharmacodynamic profiles.
*Phase 0*
- **Phase 0 trials** are exploratory studies conducted in a very small number of subjects (10-15) to gather preliminary data on a drug's **pharmacodynamics and pharmacokinetics** in humans.
- They involve microdoses, not intended to have therapeutic effects, and thus cannot determine toxicity or MTD.
*Phase III*
- **Phase III trials** are large-scale studies involving hundreds to thousands of patients to confirm the drug's **efficacy**, monitor side effects, compare it to standard treatments, and collect information that will allow the drug to be used safely.
- These trials are conducted after safety and initial efficacy have been established in earlier phases.
*Phase V*
- "Phase V" is not a standard, recognized phase in the traditional clinical trial classification (Phase 0, I, II, III, IV).
- This term might be used in some non-standard research contexts or for post-marketing studies that go beyond Phase IV surveillance, but it is not a formal phase for initial drug development.
*Phase II*
- **Phase II trials** involve several hundred patients with the condition the drug is intended to treat, focusing on **drug efficacy** and further evaluating safety.
- While safety is still monitored, the primary objective shifts to determining if the drug works for its intended purpose and at what dose.
Evidence basis for screening recommendations US Medical PG Question 5: Two studies are reviewed for submission to an oncology journal. In Study A, a novel MRI technology is evaluated as a screening tool for ovarian cancer. The authors find that the mean survival time is 4 years in the control group and 10 years in the MRI-screened group. In Study B, cognitive behavioral therapy (CBT) and a novel antidepressant are used to treat patients with comorbid pancreatic cancer and major depression. Patients receiving the new drug are told that they are expected to have quick resolution of their depression, while those who do not receive the drug are not told anything about their prognosis. Which of the following describes the likely type of bias in Study A and Study B?
- A. Latency Bias; Golem effect
- B. Confounding; Golem effect
- C. Lead time bias; Golem effect
- D. Lead time bias; Pygmalion effect (Correct Answer)
- E. Latency bias; Pygmalion effect
Evidence basis for screening recommendations Explanation: ***Lead time bias; Pygmalion effect***
- In Study A, the MRI technology detects ovarian cancer earlier, artificially making the survival time appear longer simply due to earlier diagnosis, not necessarily improved outcomes, which is characteristic of **lead time bias**.
- In Study B, the patients receiving the new drug are told to expect quick resolution of their depression, leading to increased expectation of improvement, which describes the **Pygmalion effect** (a form of observer-expectancy effect where higher expectations lead to increased performance).
*Latency Bias; Golem effect*
- **Latency bias** refers to a delay in the manifestation of an outcome, which is not the primary issue in Study A's screening context.
- The **Golem effect** is a form of negative self-fulfilling prophecy where lower expectations placed upon individuals by superiors/researchers lead to poorer performance, which is opposite to what is described in Study B.
*Confounding; Golem effect*
- **Confounding** occurs when an unmeasured third variable is associated with both the exposure and the outcome, distorting the observed relationship; while confounding is common, the scenario in Study A specifically points to a screening effect on survival time.
- As mentioned, the **Golem effect** refers to negative expectations leading to poorer outcomes, which is not present in Study B.
*Lead time bias; Golem effect*
- **Lead time bias** correctly identifies the issue in Study A, as explaining the apparently longer survival as a result of earlier detection.
- However, the **Golem effect** incorrectly describes the scenario in Study B, where positive expectations are given, not negative ones.
*Latency bias; Pygmalion effect*
- **Latency bias** is not the primary bias described in Study A; the immediate impact of early detection on survival statistics points to lead time bias.
- The **Pygmalion effect** correctly describes the bias in Study B, where positive expectations from the researchers influence patient outcomes.
Evidence basis for screening recommendations US Medical PG Question 6: During an evaluation of a new diagnostic imaging modality for detecting salivary gland tumors, 90 patients tested positive out of the 100 patients who tested positive with the gold standard test. A total of 80 individuals tested negative with the new test out of the 100 individuals who tested negative with the gold standard test. What is the positive likelihood ratio for this test?
- A. 80/90
- B. 90/100
- C. 90/20 (Correct Answer)
- D. 90/110
- E. 10/80
Evidence basis for screening recommendations Explanation: ***90/20***
- The **positive likelihood ratio (LR+)** is calculated as **sensitivity / (1 - specificity)**. To calculate this, we first need to determine the values for true positives (TP), false positives (FP), true negatives (TN), and false negatives (FN).
- Given that 90 out of 100 actual positive patients tested positive, **TP = 90** and **FN = 100 - 90 = 10**. Also, 80 out of 100 actual negative patients tested negative, so **TN = 80** and **FP = 100 - 80 = 20**.
- **Sensitivity** is the true positive rate (TP / (TP + FN)) = 90 / (90 + 10) = 90 / 100.
- **Specificity** is the true negative rate (TN / (TN + FP)) = 80 / (80 + 20) = 80 / 100.
- Therefore, LR+ = (90/100) / (1 - 80/100) = (90/100) / (20/100) = **90/20**.
*80/90*
- This option incorrectly represents the components for the likelihood ratio. It seems to misinterpret the **true negative** count and the **true positive** count.
- It does not follow the formula for LR+ which is **sensitivity / (1 - specificity)**.
*90/100*
- This value represents the **sensitivity** of the test, which is the proportion of true positives among all actual positives.
- It does not incorporate the **false positive rate** (1 - specificity) in the denominator required for the positive likelihood ratio.
*90/110*
- This option incorrectly combines different values, possibly by confusing the denominator for sensitivity or specificity calculations.
- It does not correspond to the formula for the **positive likelihood ratio**.
*10/80*
- This value seems to relate to the inverse of the **false negative rate** (10/100) or misrepresents the relationship between false negatives and true negatives.
- It is not correctly structured to represent the **positive likelihood ratio (LR+)**.
Evidence basis for screening recommendations US Medical PG Question 7: A 65-year-old non-smoking woman with no symptoms comes to your clinic to establish care with a primary care provider. She hasn’t seen a doctor in 12 years and states that she feels very healthy. You realize that guidelines by the national cancer organization suggest that she is due for some cancer screening tests, including a mammogram for breast cancer, a colonoscopy for colon cancer, and a pap smear for cervical cancer. These three screening tests are most likely to be considered which of the following?
- A. Tertiary prevention
- B. Primary prevention
- C. Secondary prevention (Correct Answer)
- D. Cancer screening does not fit into these categories
- E. Quaternary prevention
Evidence basis for screening recommendations Explanation: ***Secondary prevention***
- **Secondary prevention** aims to detect and treat a disease early, before symptoms appear, to prevent its progression or recurrence.
- **Cancer screening tests** such as mammograms, colonoscopies, and Pap smears fit this category perfectly as they are performed in asymptomatic individuals to identify early-stage cancer or pre-cancerous lesions.
*Tertiary prevention*
- **Tertiary prevention** focuses on minimizing the impact of an established disease and improving quality of life through treatment and rehabilitation.
- This would involve managing existing cancer, not screening for it.
*Primary prevention*
- **Primary prevention** aims to prevent a disease from occurring in the first place, often through health promotion and risk reduction.
- Examples include vaccination, lifestyle modifications (e.g., healthy diet, exercise), or avoiding smoking.
*Cancer screening does not fit into these categories*
- This statement is incorrect as cancer screening is a well-established component of preventive healthcare.
- It clearly falls within the defined categories of prevention, specifically secondary prevention.
*Quaternary prevention*
- **Quaternary prevention** aims to protect patients from medical interventions that are likely to cause more harm than good, or to avoid over-medicalization.
- This concept is distinct from screening for diseases and focuses on ethical considerations in medical care.
Evidence basis for screening recommendations US Medical PG Question 8: A 46-year-old woman presents to her primary care physician for her annual examination. At her prior exam one year earlier, she had a Pap smear which was within normal limits. Which of the following health screenings is recommended for this patient?
- A. Colorectal screening (Correct Answer)
- B. Blood glucose and/or HbA1c screening
- C. Blood pressure at least once every 3 years
- D. Yearly Pap smear
- E. Bone mineral density screening
Evidence basis for screening recommendations Explanation: ***Colorectal screening***
- **Colorectal cancer screening** is generally recommended to start at age **45 years** for individuals at average risk.
- This patient is 46 years old, making immediate colorectal screening appropriate based on current guidelines.
*Blood glucose and/or HbA1c screening*
- **Blood glucose or HbA1c screening** for diabetes is recommended starting at age **35 for all adults** or earlier if there are risk factors such as obesity or a family history of diabetes.
- While this patient is 46, this screening should have already been initiated, and it is not the *most* uniquely recommended screening for this specific age that might have been overlooked.
*Blood pressure at least once every 3 years*
- **Blood pressure screening** should be performed **at least annually** for adults aged 40 and older, or more frequently if there are risk factors.
- Screening only every 3 years is insufficient for a 46-year-old patient.
*Yearly Pap smear*
- **Pap smear frequency** has changed; for women aged 30-65 with normal results, screening is recommended every **3 years** with cytology alone, or every 5 years with high-risk HPV testing alone or co-testing.
- A yearly Pap smear is no longer typical practice for a woman with normal prior results and no specific risk factors.
*Bone mineral density screening*
- **Bone mineral density (BMD) screening** for osteoporosis is typically recommended for women starting at age **65 years** or earlier if they have significant risk factors.
- This patient is 46 years old and has no mentioned risk factors, so BMD screening is not routinely indicated at this age.
Evidence basis for screening recommendations US Medical PG Question 9: You are reviewing raw data from a research study performed at your medical center examining the effectiveness of a novel AIDS screening examination. The study enrolled 250 patients with confirmed AIDS, and 240 of these patients demonstrated a positive screening examination. The control arm of the study enrolled 250 patients who do not have AIDS, and only 5 of these patients tested positive on the novel screening examination. What is the NPV of this novel test?
- A. 240 / (240 + 15)
- B. 240 / (240 + 5)
- C. 240 / (240 + 10)
- D. 245 / (245 + 10) (Correct Answer)
- E. 245 / (245 + 5)
Evidence basis for screening recommendations Explanation: ***245 / (245 + 10)***
- The **negative predictive value (NPV)** is calculated as **true negatives (TN)** divided by the sum of **true negatives (TN)** and **false negatives (FN)**.
- In this study, there are 250 patients with AIDS; 240 tested positive (true positives, TP), meaning 10 tested negative (false negatives, FN = 250 - 240). There are 250 patients without AIDS; 5 tested positive (false positives, FP), meaning 245 tested negative (true negatives, TN = 250 - 5). Therefore, NPV = 245 / (245 + 10).
*240 / (240 + 15)*
- This calculation incorrectly uses the number of **true positives** (240) in the numerator and denominator, which is relevant for **positive predictive value (PPV)**, not NPV.
- The denominator `(240 + 15)` does not correspond to a valid sum for calculating NPV from the given data.
*240 / (240 + 5)*
- This calculation incorrectly uses **true positives** (240) in the numerator, which is not part of the NPV formula.
- The denominator `(240 + 5)` mixes true positives and false positives, which is incorrect for NPV.
*240 / (240 + 10)*
- This incorrectly places **true positives** (240) in the numerator instead of **true negatives**.
- The denominator `(240+10)` represents **true positives + false negatives**, which is related to sensitivity, not NPV.
*245 / (245 + 5)*
- This calculation correctly identifies **true negatives** (245) in the numerator but incorrectly uses **false positives** (5) in the denominator instead of **false negatives**.
- The denominator for NPV should be **true negatives + false negatives**, which is 245 + 10.
Evidence basis for screening recommendations US Medical PG Question 10: A 27-year-old woman presents for her routine annual examination. She has no complaints. She has a 3-year-old child who was born via normal vaginal delivery with no complications. She had a Pap smear during her last pregnancy and the findings were normal. Her remaining past medical history is not significant, and her family history is also not significant. Recently, one of her close friends was diagnosed with breast cancer at the age of 36, and, after reading some online research, she wants to be checked for all types of cancer. Which of the following statements would be the best advice regarding the most appropriate screening tests for this patient?
- A. “Your last Pap smear 3 years ago was normal. We can repeat it after 2 more years.”
- B. “Remember that information on the internet is vague and unreliable. You don't need any screening tests at this time.”
- C. “Yes, you are right to be concerned. Let us do a mammogram and a blood test for CA-125.”
- D. “You need HPV (human papillomavirus) co-testing only.”
- E. “We should do a Pap smear now. Blood tests are not recommended for screening purposes.” (Correct Answer)
Evidence basis for screening recommendations Explanation: ***We should do a Pap smear now. Blood tests are not recommended for screening purposes.***
- The current guidelines recommend Pap smears every 3 years for women aged 21-29. Although her last Pap smear was 3 years ago, it was done during pregnancy, and a **repeat Pap smear is indicated now** as she is at the end of the 3-year interval.
- **Blood tests like CA-125 are not recommended for routine cancer screening** in asymptomatic women due to their low specificity and sensitivity, which can lead to false positives and unnecessary invasive procedures.
*“Your last Pap smear 3 years ago was normal. We can repeat it after 2 more years.”*
- While a 3-year interval is generally appropriate, her last Pap smear was done 3 years ago and was performed during pregnancy, making a **repeat Pap smear indicated now** to remain within current screening guidelines.
- Delaying the Pap smear for another two years would exceed the recommended 3-year interval for cervical cancer screening in her age group.
*“Remember that information on the internet is vague and unreliable. You don't need any screening tests at this time.”*
- While caution about internet information is valid, it is **inaccurate to suggest no screening tests are needed** as the patient is due for a Pap smear based on her age and last screening date.
- Dismissing a patient's concerns outright without acknowledging valid screening needs can harm patient-doctor trust and lead to missed opportunities for preventive care.
*“Yes, you are right to be concerned. Let us do a mammogram and a blood test for CA-125.”*
- **Routine mammograms are not recommended for women under 40** without specific risk factors (e.g., strong family history, genetic mutations), which are not present here.
- **CA-125 is primarily used for monitoring ovarian cancer treatment** or evaluating women with symptoms, not for general population screening due to its low specificity.
*“You need HPV (human papillomavirus) co-testing only.”*
- **HPV co-testing (HPV test + Pap smear) is recommended for women aged 30 and older**, or as a follow-up to abnormal Pap smear results.
- For women aged 21-29, **primary Pap smear screening alone is recommended** every 3 years.
More Evidence basis for screening recommendations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.