Cancer screening recommendations (by cancer type) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cancer screening recommendations (by cancer type). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cancer screening recommendations (by cancer type) US Medical PG Question 1: A 68-year-old female presents to your office for her annual check-up. Her vitals are HR 85, T 98.8 F, RR 16, BP 125/70. She has a history of smoking 1 pack a day for 35 years, but states she quit five years ago. She had her last pap smear at age 64 and states all of her pap smears have been normal. She had her last colonoscopy at age 62, which was also normal. Which of the following is the next best test for this patient?
- A. Pap smear
- B. Chest radiograph
- C. Abdominal ultrasound
- D. Colonoscopy
- E. Chest CT scan (Correct Answer)
Cancer screening recommendations (by cancer type) Explanation: ***Chest CT scan***
- This patient is a 68-year-old female with a **35-pack-year smoking history** who quit 5 years ago, placing her in a high-risk group for lung cancer.
- **Low-dose computed tomography (LDCT)** for lung cancer screening is recommended annually for individuals aged 50-80 with a 20-pack-year smoking history who currently smoke or have quit within the past 15 years.
*Pap smear*
- A Pap smear is not indicated as she had her last one at age 64 and all previous results were normal.
- Guidelines recommend discontinuing Pap smears at age 65 if there is no history of moderate or severe dysplasia and three consecutive negative results within the last 10 years.
*Chest radiograph*
- A chest radiograph is a less sensitive and specific tool for detecting early lung cancer compared to LDCT.
- It misses a significant proportion of early-stage lung cancers and is not recommended for lung cancer screening.
*Abdominal ultrasound*
- An abdominal ultrasound is generally used to screen for conditions like abdominal aortic aneurysm in specific high-risk populations (males 65-75 who have ever smoked).
- There is no indication from the provided history for an abdominal ultrasound in this patient.
*Colonoscopy*
- This patient had a normal colonoscopy at age 62.
- Current guidelines recommend repeating colonoscopy every 10 years if the previous one was normal, so she is not due for another one yet.
Cancer screening recommendations (by cancer type) US Medical PG Question 2: A 32-year-old woman makes an appointment with her family physician for a new-employment physical examination. She has no complaints and the physical examination is unremarkable. The family history is negative for malignancies and inherited disorders. During the visit, she provides the results of a Pap smear taken last week, which reports the presence of atypical squamous cells of undetermined significance (ASC-US), along with a test for HPV, which was negative. The previous Pap smear was normal (negative for intraepithelial lesions or malignancy). When would you recommend that she have another Pap smear?
- A. 3 years (Correct Answer)
- B. 1 year
- C. Immediately
- D. 6 months
- E. 5 years
Cancer screening recommendations (by cancer type) Explanation: ***3 years***
- For women aged 21-65 with an **ASC-US Pap result AND a negative HPV test**, current guidelines recommend routine **co-testing every 3 years** or cytology alone every 3 years.
- A negative HPV test in the setting of ASC-US indicates a very low risk of high-grade disease, allowing for a return to routine screening intervals.
*1 year*
- A 1-year follow-up would typically be recommended for an **ASC-US Pap result** when the **HPV test is positive**, or if HPV testing was not performed.
- This shorter interval is appropriate when there's an increased risk of underlying cervical dysplasia.
*Immediately*
- Immediate repeat testing is generally reserved for more concerning findings, such as **high-grade squamous intraepithelial lesions (HSIL)**, atypical glandular cells (AGC), or frankly malignant results.
- ASC-US with negative HPV does not warrant immediate re-evaluation.
*6 months*
- A 6-month follow-up is not a standard recommendation for an **ASC-US with a negative HPV test**.
- It might be considered in specific circumstances for an ASC-US result with a positive HPV test, but not when HPV is negative.
*5 years*
- Routine screening with **co-testing (Pap and HPV)** is typically recommended every **5 years** for women aged 30-65 with **normal Pap and negative HPV results**.
- This patient has an ASC-US result, which necessitates a slightly shorter follow-up than routine screening.
Cancer screening recommendations (by cancer type) US Medical PG Question 3: A 35-year-old woman is presenting for a general wellness checkup. She is generally healthy and has no complaints. The patient does not smoke, drinks 1 alcoholic drink per day, and exercises 1 day per week. She recently had silicone breast implants placed 1 month ago. Her family history is notable for a heart attack in her mother and father at the age of 71 and 55 respectively. Her father had colon cancer at the age of 70. Her temperature is 99.0°F (37.2°C), blood pressure is 121/81 mmHg, pulse is 77/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is unremarkable. Which of the following is the most appropriate initial step in management?
- A. Alcohol cessation
- B. Colonoscopy at age 60
- C. Mammography at age 50
- D. Colonoscopy at age 40 (Correct Answer)
- E. Mammography now
Cancer screening recommendations (by cancer type) Explanation: ***Colonoscopy at age 40***
- This patient has a **first-degree relative (father) diagnosed with colorectal cancer at age 70**, which increases her risk compared to the average population.
- Current **USPSTF and ACS guidelines** recommend that individuals with a first-degree relative diagnosed with colorectal cancer at **age 60 or older** should begin screening at **age 40** (or 10 years before the age of diagnosis in the relative, whichever is earlier).
- Since her father was diagnosed at age 70, she should start screening at age 40 (which is 10 years earlier and also the recommended age for those with family history).
- At age 35, she does **not yet need** colonoscopy, but should plan for screening in 5 years.
*Colonoscopy now*
- This is **too early** based on current guidelines.
- Immediate colonoscopy at age 35 is not indicated in an asymptomatic patient whose father was diagnosed at age 70.
- Screening at age 40 provides adequate time for early detection while avoiding unnecessary early intervention.
*Colonoscopy at age 60*
- This is **too late** and ignores the increased risk from family history.
- Delaying screening until age 60 would miss the recommended earlier screening window for patients with first-degree relatives with CRC.
*Alcohol cessation*
- The patient drinks **1 alcoholic drink per day**, which is within recommended limits for women.
- While reducing alcohol consumption has general health benefits, this is not the most urgent preventive measure given her family history of colon cancer.
*Mammography now*
- Screening mammography typically begins at **age 40-50** for average-risk women.
- At age 35 with no specific high-risk factors (no BRCA mutation, no strong early-onset breast cancer family history), mammography is not indicated now.
*Mammography at age 50*
- While this may be appropriate for breast cancer screening depending on guidelines followed, it is **not the priority** given her significant family history of colorectal cancer requiring earlier intervention.
Cancer screening recommendations (by cancer type) US Medical PG Question 4: A 49-year-old woman presents to her primary care physician for a general check up. She has not seen a primary care physician for the past 20 years but states she has been healthy during this time frame. She had breast implants placed when she was 29 years old but otherwise has not had any surgeries. She is concerned about her risk for breast cancer given her friend was recently diagnosed. Her temperature is 97.0°F (36.1°C), blood pressure is 114/64 mmHg, pulse is 70/min, respirations are 12/min, and oxygen saturation is 98% on room air. Physical exam is unremarkable. Which of the following is the most appropriate workup for breast cancer for this patient?
- A. No intervention indicated at this time
- B. Sentinel node biopsy
- C. BRCA genetic testing
- D. Mammography (Correct Answer)
- E. Ultrasound
Cancer screening recommendations (by cancer type) Explanation: ***Mammography***
- The patient is 49 years old, making regular screening **mammography** the most appropriate initial workup for breast cancer, as guidelines recommend screening for women over 40.
- While breast implants can make mammograms more challenging, specialized techniques like **Eklund views** can be used to visualize breast tissue effectively.
*No intervention indicated at this time*
- This is incorrect because the patient's age (49) places her in the demographic for routine **breast cancer screening**.
- Delaying screening in this age group would increase the risk of detecting cancer at a later, less treatable stage.
*Sentinel node biopsy*
- **Sentinel node biopsy** is a procedure typically performed after a breast cancer diagnosis to stage the disease and determine lymph node involvement.
- It is not a screening tool and is therefore inappropriate as an initial workup in an asymptomatic patient without a known mass.
*BRCA genetic testing*
- **BRCA genetic testing** is indicated for individuals with a strong family history of breast or ovarian cancer, or those diagnosed with specific types of breast cancer at a young age.
- This patient has no such risk factors mentioned, making genetic testing unnecessary as a first-line screening step.
*Ultrasound*
- **Ultrasound** is often used as a follow-up to an abnormal mammogram or to evaluate specific palpable masses, especially in younger women with dense breasts.
- It is not typically recommended as a primary screening tool for breast cancer in a 49-year-old woman, especially without prior mammographic findings.
Cancer screening recommendations (by cancer type) US Medical PG Question 5: A 57-year-old man presents for his yearly wellness visit. He says he has been feeling well and has no complaints. No significant past medical history or current medications. The patient reports a 35-pack-year smoking history but says he quit 5 years ago. His family history is significant for lung cancer in his father who died at age 67. His vital signs include: temperature 36.8°C (98.2°F), pulse 95/min, respiratory rate 16/min, blood pressure 100/75 mm Hg. Physical examination is unremarkable. Laboratory findings are significant for the following:
Serum potassium 3.9 mEq/L
Serum sodium 140 mEq/L
Serum chloride 103 mEq/L
Serum calcium 2.5 mmol/L
BUN 15 mg/dL
Creatinine 0.8 mg/dL
Glucose 95 mg/dL
Magnesium 1.7 mEq/L
Phosphate 1.1 mmol/L
Hemoglobin 14 g/dL
Bicarbonate (HCO3-) 25 mEq/L
Bilirubin, total 0.9 mg/dL
Bilirubin, indirect 0.4 mg/dL
AST 10 U/L
ALT 19 U/L
Alkaline phosphatase 40 U/L
Albumin 3.6 g/dL
Which of the following preventative screening tests is recommended for this patient at this time?
- A. Abdominal ultrasound
- B. No screening indicated
- C. Low-dose CT scan (LDCT) of the chest (Correct Answer)
- D. ECG
- E. Chest X-ray
Cancer screening recommendations (by cancer type) Explanation: ***Low-dose CT scan (LDCT) of the chest***
- The patient meets the criteria for **lung cancer screening** due to his age (57), significant **smoking history** (35 pack-years), and quitting within the last 15 years (5 years ago).
- Guidelines recommend annual **LDCT** for individuals aged 50-80 with a 20+ pack-year smoking history who currently smoke or have quit within the past 15 years.
*Abdominal ultrasound*
- This test is not routinely recommended for asymptomatic individuals for general screening; its use is typically for specific symptoms or risks (e.g., abdominal pain, family history of abdominal aortic aneurysm).
- The patient has no symptoms or risk factors that would suggest the need for an abdominal ultrasound at this time.
*No screening indicated*
- Given the patient's **heavy smoking history** and age, there is a clear indication for **lung cancer screening**.
- Skipping screening would miss an opportunity for early detection of lung cancer, which is crucial for improving outcomes.
*ECG*
- An **ECG** screens for cardiac abnormalities but is not a primary screening tool for lung cancer.
- While smoking is a risk factor for cardiovascular disease, the immediate and most pressing screening need based on his history is related to lung cancer.
*Chest X-ray*
- A **chest X-ray** is generally not recommended for **lung cancer screening** in high-risk individuals because it has lower sensitivity compared to **LDCT** for detecting early-stage tumors.
- **LDCT** is the preferred method for lung cancer screening due to its superior ability to detect small, actionable lesions.
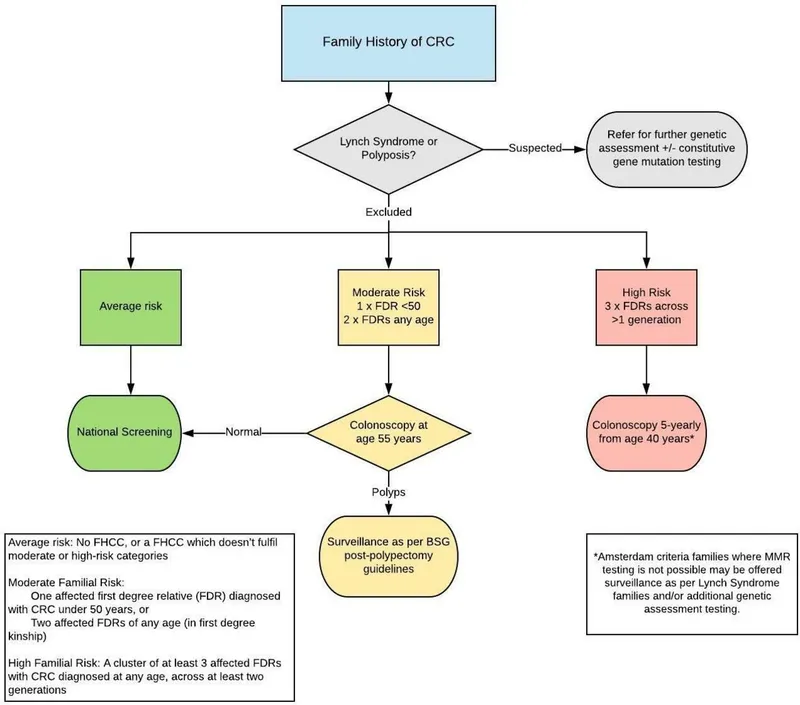
Cancer screening recommendations (by cancer type) US Medical PG Question 6: An 18-year-old man presents to his primary care provider before leaving for college. He has no complaints. His past medical history is significant for asthma, acne vulgaris, and infectious mononucleosis at age 16. His home medications include doxycycline and albuterol as needed. His family history is significant for colon cancer in his father at age 50, his paternal grandfather at age 55, and an uncle at age 45. His father underwent testing for mutations in the APC gene, which were negative. There is no family history of dental abnormalities or other malignancy. The patient denies any recent weight loss, abdominal pain, hematochezia, melena, or other changes in the appearance of his stools. This patient should be screened for colorectal cancer (CRC) under which of the following protocols?
- A. Colonoscopy every 5 years beginning at age 40 (Correct Answer)
- B. Colonoscopy every 10 years beginning at age 50
- C. Colonoscopy every 1-2 years beginning at age 25
- D. Prophylactic colectomy
- E. Fecal occult blood testing annually beginning at age 40
Cancer screening recommendations (by cancer type) Explanation: ***Colonoscopy every 5 years beginning at age 40***
- The patient has a strong family history of CRC, with a father diagnosed at age 50 and a paternal grandfather at age 55, placing him at increased risk.
- Current guidelines recommend that individuals with a first-degree relative diagnosed with CRC before age 60 should begin screening 10 years before the earliest diagnosis in the family, or at age 40, whichever comes first, with a colonoscopy every 5 years.
*Colonoscopy every 10 years beginning at age 50*
- This protocol is recommended for individuals with an **average risk** for colorectal cancer, which does not apply to this patient due to his strong family history.
- Starting screening at age 50 would be too late given the early onset of CRC in his family.
*Colonoscopy every 1-2 years beginning at age 25*
- This more aggressive screening schedule is typically reserved for individuals with identified **hereditary colorectal cancer syndromes**, such as **Familial Adenomatous Polyposis (FAP)** or **Lynch syndrome**.
- Though there is a strong family history, the negative APC gene testing and absence of other syndromic features (like dental abnormalities) make FAP less likely, and Lynch syndrome would typically involve other cancers.
*Prophylactic colectomy*
- **Prophylactic colectomy** is a major surgical procedure considered in rare cases of very high-risk hereditary syndromes, such as confirmed **Familial Adenomatous Polyposis (FAP)**, where the risk of CRC is almost 100%.
- This patient's family history, while significant, does not meet the criteria for such an extreme measure.
*Fecal occult blood testing annually beginning at age 40*
- While **fecal occult blood testing (FOBT)** is a valid screening method, it is typically used for individuals with average risk or in conjunction with other methods.
- Given the patient's strong family history of early-onset CRC, a **colonoscopy** is the more appropriate and comprehensive screening method.
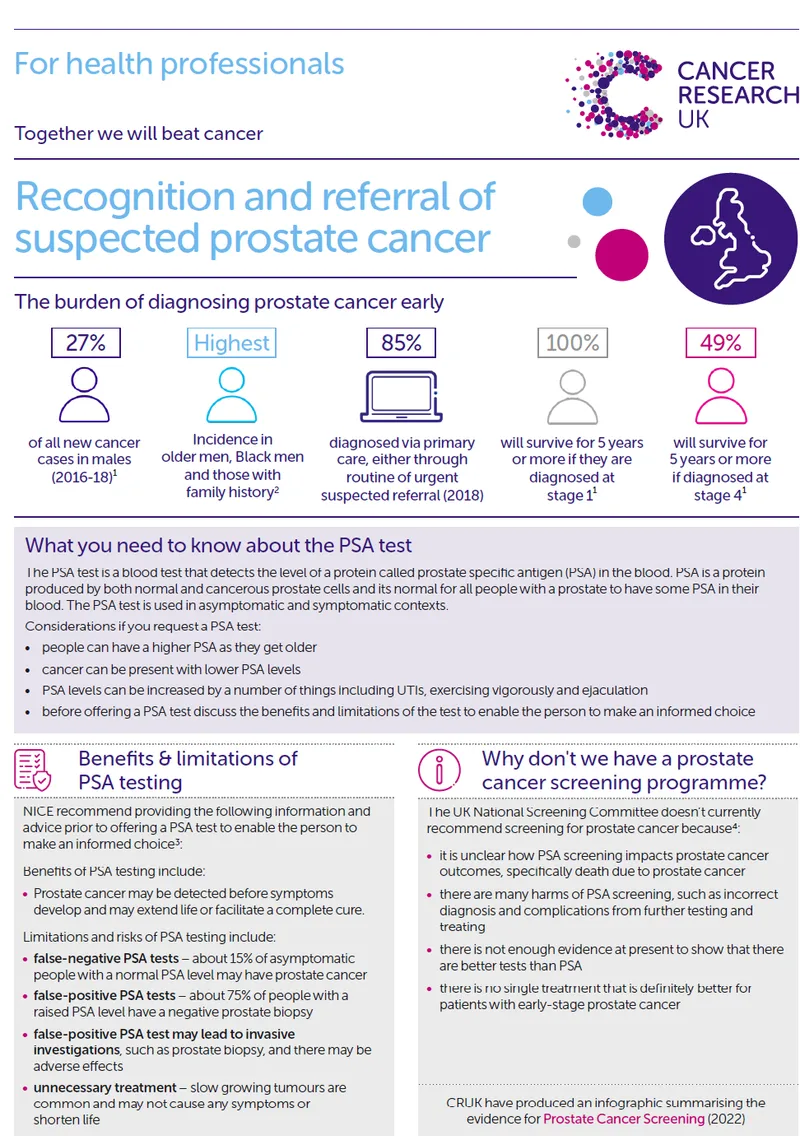
Cancer screening recommendations (by cancer type) US Medical PG Question 7: A 65-year-old African American man presents for follow-up examination with a 6-month history of urinary hesitancy, weak stream, and terminal dribbling, which is refractory to a combination therapy of finasteride and tamsulosin. The patient’s past medical history is otherwise unremarkable. His father and brother were diagnosed with prostate cancer at the age of 55 years. His vital signs are within normal limits. The patient has a normal anal sphincter tone and a bulbocavernosus muscle reflex. Digital rectal exam (DRE) reveals a prostate size equivalent to 2 finger pads with a hard nodule and without fluctuance or tenderness. Serum prostate-specific antigen (PSA) level is 5 ng/mL. Which of the following investigations is most likely to establish a definitive diagnosis?
- A. Magnetic resonance imaging (MRI)
- B. 4Kscore test
- C. Prostate Health Index (PHI)
- D. Image-guided needle biopsy (Correct Answer)
- E. PSA in 3 months
Cancer screening recommendations (by cancer type) Explanation: ***Image-guided needle biopsy***
- A definitive diagnosis of **prostate cancer** requires histological confirmation, which is achieved through a **biopsy**.
- The patient's presentation with a **hard nodule** on DRE, elevated PSA, and a strong family history of prostate cancer, despite treatment for BPH, strongly indicates the need for a biopsy.
*Magnetic resonance imaging (MRI)*
- While MRI can help in **staging prostate cancer** and guiding biopsies, it does not provide a definitive diagnosis on its own.
- An MRI may identify suspicious lesions but **cannot confirm malignancy** without tissue sampling.
*4Kscore test*
- The 4Kscore test estimates the **risk of high-grade prostate cancer** but does not provide a definitive diagnosis.
- It uses a panel of four prostate-specific kallikrein proteins, along with patient age, DRE status, and prior biopsy results, to calculate a risk score.
*Prostate Health Index (PHI)*
- The PHI is a blood test that combines total PSA, free PSA, and [-2]proPSA to assess the **probability of prostate cancer**.
- It helps in deciding whether a biopsy is needed, but like the 4Kscore, it is not a diagnostic tool in itself.
*PSA in 3 months*
- Re-checking PSA in 3 months would **delay definitive diagnosis** and treatment for a potentially aggressive cancer, especially given the palpable nodule and family history.
- The current PSA of 5 ng/mL, although not extremely high, combined with the suspicious DRE finding, warrants more immediate action.
Cancer screening recommendations (by cancer type) US Medical PG Question 8: A 19-year-old woman presents for a sports physical. She says she feels healthy and has no concerns. Past medical history is significant for depression and seasonal allergies. Current medications are fluoxetine and oral estrogen/progesterone contraceptive pills. Family history is significant for a sister with polycystic ovarian syndrome (PCOS). The patient denies current or past use of alcohol, recreational drugs, or smoking. She reports that she has been on oral birth control pills since age 14 and uses condoms inconsistently. No history of STDs. She is sexually active with her current boyfriend, who was treated for chlamydia 2 years ago. She received and completed the HPV vaccination series starting at age 11. Her vital signs include: temperature 36.8°C (98.2°F), pulse 97/min, respiratory rate 16/min, blood pressure 120/75 mm Hg. Physical examination is unremarkable. Which of the following are the recommended guidelines for cervical cancer screening for this patient at this time?
- A. Cytology (pap smear) and HPV DNA co-testing every 3 years
- B. Cytology (pap smear) every 3 years
- C. Cytology (pap smear) annually
- D. Cytology (pap smear) and HPV DNA co-testing every 5 years
- E. No cervical cancer screening is indicated at this time (Correct Answer)
Cancer screening recommendations (by cancer type) Explanation: ***No cervical cancer screening is indicated at this time***
- Current guidelines recommend initiating **cervical cancer screening** at age 21, regardless of sexual activity initiation.
- The patient is 19 years old, therefore, screening is not yet indicated per standard recommendations.
*Cytology (pap smear) and HPV DNA co-testing every 3 years*
- This option is incorrect because **co-testing** with cytology and HPV DNA is generally recommended for women aged 30-65 years, not for women under 21.
- While cytology every 3 years is a recommendation for women 21-29, co-testing is not the primary recommendation in this age group, and the patient is below the screening age.
*Cytology (pap smear) every 3 years*
- This screening interval is recommended for women aged 21-29 years, but the patient is currently 19 years old.
- Initiating screening earlier than 21 years is not recommended due to the high incidence of **transient HPV infections** and low risk of cervical cancer in younger individuals.
*Cytology (pap smear) annually*
- **Annual Pap smears** are no longer recommended for routine screening; guidelines have shifted to longer intervals due to the slow progression of cervical cancer and high rates of HPV clearance.
- Even if screening were indicated, annual cytology is not the current recommendation for any age group, especially not for a 19-year-old.
*Cytology (pap smear) and HPV DNA co-testing every 5 years*
- This screening strategy (**co-testing every 5 years**) is recommended for women aged 30-65 years.
- This patient is only 19 years old, making this recommendation inappropriate for her age.
Cancer screening recommendations (by cancer type) US Medical PG Question 9: A 19-year-old woman presents to the physician for a routine health maintenance examination. She has a past medical history of gastroesophageal reflux disease. She recently moved to a new city to begin her undergraduate studies. Her father was diagnosed with colon cancer at age 46. Her father's brother died because of small bowel cancer. Her paternal grandfather died because of stomach cancer. She takes a vitamin supplement. Current medications include esomeprazole and a multivitamin. She smoked 1 pack of cigarettes daily for 3 years but quit 2 years ago. She drinks 1–2 alcoholic beverages on the weekends. She appears healthy. Vital signs are within normal limits. Physical examination shows no abnormalities. Colonoscopy is unremarkable. Germline testing via DNA sequencing in this patient shows mutations in DNA repair genes MLH1 and MSH2. Which of the following will this patient most likely require at some point in her life?
- A. Celecoxib or sulindac therapy
- B. Surgical removal of a desmoid tumor
- C. Prophylactic proctocolectomy with ileoanal anastomosis
- D. Annual colonoscopy beginning at 20–25 years of age (Correct Answer)
- E. Measurement of carcinoembryonic antigen and CA 19-9 yearly
Cancer screening recommendations (by cancer type) Explanation: ***Annual colonoscopy beginning at 20–25 years of age***
- This patient's family history of multiple cancers at young ages (father with colon cancer at 46, uncle with small bowel cancer, grandfather with stomach cancer) combined with **germline mutations in MLH1 and MSH2** is highly indicative of **Lynch syndrome (hereditary non-polyposis colorectal cancer - HNPCC)**.
- Individuals with Lynch syndrome have a significantly increased risk of colorectal cancer, and screening with **annual colonoscopies starting at a young age (20-25 years or 2-5 years younger than the earliest age of diagnosis in the family)** is crucial for early detection and prevention.
*Celecoxib or sulindac therapy*
- **NSAID therapy** (like celecoxib or sulindac) is sometimes used for **chemoprevention in familial adenomatous polyposis (FAP)** to reduce polyp burden, especially in attenuated FAP.
- However, this patient's presentation and genetic findings point to **Lynch syndrome**, for which NSAID chemoprevention is not the primary or most effective strategy compared to surveillance.
*Surgical removal of a desmoid tumor*
- **Desmoid tumors** are benign but locally aggressive soft tissue tumors that are a characteristic **extracolonic manifestation of familial adenomatous polyposis (FAP)**, especially in patients with mutations in the APC gene.
- This patient has **Lynch syndrome**, which is associated with different extracolonic cancers (e.g., endometrial, ovarian, gastric, small bowel), but **desmoid tumors are not a typical feature of Lynch syndrome**.
*Prophylactic proctocolectomy with ileoanal anastomosis*
- **Prophylactic proctocolectomy** is the standard preventive surgery for individuals with **familial adenomatous polyposis (FAP)** to prevent the inevitable development of colorectal cancer due to hundreds to thousands of polyps.
- While Lynch syndrome carries a high risk of colorectal cancer, prophylactic colectomy is generally **not recommended as the initial management** given that surveillance via colonoscopy allows for removal of precancerous polyps and early-stage cancers, reserving surgery for when clinically indicated.
*Measurement of carcinoembryonic antigen and CA 19-9 yearly*
- **Carcinoembryonic antigen (CEA) and CA 19-9** are **tumor markers** that can be elevated in certain cancers (e.g., colorectal for CEA, pancreatic/biliary for CA 19-9).
- However, these markers have **poor sensitivity and specificity for screening healthy, asymptomatic individuals** at high risk for cancer and are primarily used for monitoring disease recurrence or treatment response in diagnosed cancers. They are not recommended for routine surveillance in Lynch syndrome.
Cancer screening recommendations (by cancer type) US Medical PG Question 10: A 46-year-old man presents with increasing fatigue and weakness for the past 3 months. He works as a lawyer and is handling a complicated criminal case which is very stressful, and he attributes his fatigue to his work. He lost 2.3 kg (5.0 lb) during this time despite no change in diet or activity level. His past history is significant for chronic constipation and infrequent episodes of bloody stools. Family history is significant for his father and paternal uncle who died of colon cancer and who were both known to possess a genetic mutation for the disease. He has never had a colonoscopy or had any genetic testing performed. Physical examination is significant for conjunctival pallor. A colonoscopy is performed and reveals few adenomatous polyps. Histopathologic examination shows high-grade dysplasia and genetic testing reveals the same mutation as his father and uncle. The patient is concerned about his 20-year-old son. Which of the following is the most appropriate advice regarding this patient's son?
- A. The son doesn't need to be tested now.
- B. An immediate colonoscopy should be ordered for the son.
- C. Screening can be started by 50 years of age as the son’s risk is similar to the general population.
- D. The son should undergo a prophylactic colonic resection.
- E. A genetic test followed by colonoscopy for the son should be ordered. (Correct Answer)
Cancer screening recommendations (by cancer type) Explanation: ***A genetic test followed by colonoscopy for the son should be ordered.***
- Given the patient's strong family history of **colon cancer** with a known genetic mutation and the patient's own diagnosis of **high-grade dysplasia** and the same mutation, his son is at a significantly increased risk.
- **Genetic testing** will determine if the son has inherited the mutation, and if positive, early and regular **colonoscopic surveillance** is crucial due to the highly aggressive nature of familial colon cancer syndromes.
*The son doesn't need to be tested now.*
- This statement is incorrect because the son is at a very high risk of inheriting a **known pathogenic genetic mutation** that predisposes to colon cancer.
- Delaying testing could lead to a delayed diagnosis of potentially cancerous or pre-cancerous lesions, missing the opportunity for **early intervention**.
*An immediate colonoscopy should be ordered for the son.*
- While a colonoscopy may be warranted, the initial step should be **genetic testing** to confirm the presence of the mutation.
- If the genetic test is negative, the urgency and frequency of colonoscopies would be different, potentially aligning with general population guidelines or slightly earlier, but not necessarily immediately at age 20 without genetic confirmation.
*Screening can be started by 50 years of age as the son’s risk is similar to the general population.*
- This advice is dangerously incorrect, as the son's risk is *not* similar to the general population due to a strong and **documented family history** of colon cancer with a **known genetic mutation**.
- Waiting until 50 years of age would likely result in delayed detection of advanced adenomas or even cancer, as familial syndromes typically present at a much **younger age**.
*The son should undergo a prophylactic colonic resection.*
- **Prophylactic colonic resection** is a major surgical procedure and is typically reserved for individuals with established diagnoses of certain high-risk syndromes, such as **Familial Adenomatous Polyposis (FAP)**, often after they have developed numerous polyps.
- This decision should only be made after **genetic confirmation** of the mutation, thorough evaluation of polyp burden, and shared decision-making with the patient and multidisciplinary team, and not as an initial step.
More Cancer screening recommendations (by cancer type) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.