Urgent vs emergent conditions recognition US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Urgent vs emergent conditions recognition. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Urgent vs emergent conditions recognition US Medical PG Question 1: A 30-year-old woman seeks evaluation at a clinic complaining of shaking, chills, fevers, and headaches for the last 3 days. She recently returned from a trip to India, where she was visiting her family. There is no history of loss of consciousness or respiratory distress. The vital signs include temperature 38.9℃ (102.0℉), respiratory rate 19/min, blood pressure 120/80 mm Hg, and pulse 94/min (rapid and thready). On general examination, she is pale and the sclera is jaundiced. Laboratory studies show:
Hematocrit (Hct) 30%
Total bilirubin 2.6 mg/dL
Direct bilirubin 0.3 mg/dL
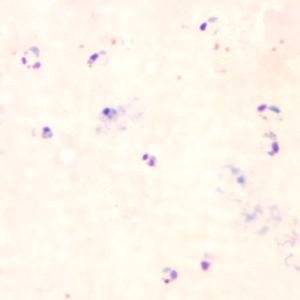
A peripheral smear is shown below. What is the most severe complication of this condition?
- A. Facial paralysis
- B. Rheumatoid arthritis
- C. Heart block
- D. Aplastic crisis
- E. Cerebral edema (Correct Answer)
Urgent vs emergent conditions recognition Explanation: ***Cerebral edema***
- The patient's symptoms (fever, chills, headache, recent travel to **India**), along with laboratory findings of **anemia (Hct 30%)** and **jaundice**, are highly suggestive of **malaria**. The peripheral smear showing multiple intraerythrocytic parasites (rings, trophozoites) further confirms this.
- Of the complications listed, **cerebral edema** (due to **cerebral malaria**) is the most severe and life-threatening complication of **Plasmodium falciparum infection**, which is prevalent in India and leads to significant mortality.
*Facial paralysis*
- **Facial paralysis** is not a typical or severe complication of uncomplicated or severe malaria.
- It is more commonly associated with conditions like Bell's palsy, stroke, or Lyme disease.
*Rheumatoid arthritis*
- **Rheumatoid arthritis** is a chronic autoimmune inflammatory condition affecting joints, not an acute complication of malaria.
- The clinical presentation is inconsistent with an acute infectious process like malaria.
*Heart block*
- While malaria can cause various cardiac complications, a direct **heart block** is not considered the most severe or common life-threatening complication, especially compared to cerebral malaria.
- Cardiac involvement in severe malaria is more often characterized by arrhythmias, myocarditis, or acute heart failure.
*Aplastic crisis*
- An **aplastic crisis** is a severe but rare complication of malaria, primarily seen in individuals with underlying **hematological disorders**, such as sickle cell disease or hereditary spherocytosis, which are not indicated here.
- While it causes profound anemia, **cerebral malaria** still carries a higher immediate mortality risk and is considered the most severe complication of **Plasmodium falciparum** infection.
Urgent vs emergent conditions recognition US Medical PG Question 2: A 50-year-old man with a history of stage 4 kidney disease was admitted to the hospital for an elective hemicolectomy. His past medical history is significant for severe diverticulitis. After the procedure he becomes septic and was placed on broad spectrum antibiotics. On morning rounds, he appear weak and complains of fatigue and nausea. His words are soft and he has difficulty answering questions. His temperature is 38.9°C (102.1°F), heart rate is 110/min, respiratory rate is 15/min, blood pressure 90/65 mm Hg, and saturation is 89% on room air. On physical exam, his mental status appears altered. He has a bruise on his left arm that spontaneously appeared overnight. His cardiac exam is positive for a weak friction rub. Blood specimens are collected and sent for evaluation. An ECG is performed (see image). What therapy will this patient most likely receive next?
- A. Send the patient for hemodialysis (Correct Answer)
- B. Perform a STAT pericardiocentesis
- C. Prepare the patient for renal transplant
- D. Treat the patient with aspirin
- E. Treat the patient with cyclophosphamide and prednisone
Urgent vs emergent conditions recognition Explanation: ***Send the patient for hemodialysis***
- This patient presents with symptoms of **uremic encephalopathy** and **uremic pericarditis** in the context of **stage 4 kidney disease**. The altered mental status, weakness, fatigue, nausea, and the development of a bruise (which could indicate uremic coagulopathy) are suggestive of severe uremia. The ECG shows widespread **ST elevation and PR depression**, particularly noticeable in leads like II, V2-V6, which is a classic finding for pericarditis. The **weak friction rub** confirms this clinical suspicion. Hemodialysis is crucial to rapidly remove uremic toxins and resolve both uremic encephalopathy and pericarditis.
- The ECG findings, including diffuse **ST elevation** with **PR depression**, are characteristic of **pericarditis**. In a patient with end-stage renal disease, **uremia** is a common cause of pericarditis, which can be life-threatening if not promptly treated with dialysis.
*Perform a STAT pericardiocentesis*
- While the patient has pericarditis, there are no immediate signs of **cardiac tamponade**, such as muffled heart sounds, jugular venous distension, or pulsus paradoxus, that would necessitate an emergency pericardiocentesis.
- The primary treatment for **uremic pericarditis** is typically **hemodialysis** to resolve the underlying uremic state, not direct fluid removal unless tamponade is present.
*Prepare the patient for renal transplant*
- **Renal transplant** is a long-term solution for end-stage renal disease, but it is not an acute intervention for immediate life-threatening uremic complications like uremic pericarditis and encephalopathy.
- The patient needs urgent stabilization and treatment of his current acute medical issues before transplant consideration.
*Treat the patient with aspirin*
- While aspirin can be used for some forms of pericarditis, it is generally **contraindicated** in patients with **uremic pericarditis** due to the increased risk of **gastric bleeding** and potential exacerbation of uremic coagulopathy.
- The primary treatment for uremic pericarditis is **dialysis**, not anti-inflammatory medications, as the inflammation is driven by uremic toxins.
*Treat the patient with cyclophosphamide and prednisone*
- **Immunosuppressants** like cyclophosphamide and prednisone are used for autoimmune or inflammatory conditions causing pericarditis, such as systemic lupus erythematosus.
- This patient's pericarditis is clearly linked to **uremia** from kidney disease, not an autoimmune condition, making immunosuppressive therapy inappropriate and potentially harmful.
Urgent vs emergent conditions recognition US Medical PG Question 3: A 27-year-old man presents to the emergency department for altered mental status. The patient was found napping in a local market and brought to the hospital. The patient has a past medical history of polysubstance abuse and is homeless. His temperature is 104°F (40.0°C), blood pressure is 100/52 mmHg, pulse is 133/min, respirations are 25/min, and oxygen saturation is 99% on room air. Physical exam is notable for an altered man. Cardiopulmonary exam reveals a murmur over the left lower sternal border. A bedside ultrasound reveals a vegetation on the tricuspid valve. The patient is ultimately started on IV fluids, norepinephrine, vasopressin, vancomycin, and piperacillin-tazobactam. A central line is immediately placed in the internal jugular vein and the femoral vein secondary to poor IV access. Cardiothoracic surgery subsequently intervenes to remove the vegetation. While recovering in the ICU, days 3-5 are notable for an improvement in the patient’s symptoms. Two additional peripheral IVs are placed while in the ICU on day 5, and the femoral line is removed. On day 6, the patient's fever and hemodynamic status worsen. Though he is currently responding and not complaining of any symptoms including headache, photophobia, neck stiffness, or pain, he states he is feeling weak. Jolt accentuation of headache is negative and his abdominal exam is benign. A chest radiograph, urinalysis, and echocardiogram are unremarkable though the patient’s blood cultures are positive when drawn. Which of the following is the best next step in management?
- A. Add micafungin to the patient’s antibiotics
- B. Perform a lumbar puncture
- C. Remove all peripheral IV’s and send for cultures
- D. Add cefepime to the patient’s antibiotics
- E. Remove the central line and send for cultures (Correct Answer)
Urgent vs emergent conditions recognition Explanation: **Correct: Remove the central line and send for cultures**
- The patient's worsening fever and hemodynamic instability on day 6, despite initial improvement, raise suspicion for a **catheter-related bloodstream infection (CRBSI)**, especially given the history of central line placement.
- **Prompt removal of the catheter** and sending the tip for culture is crucial for diagnosis and treatment of potential CRBSI, as the source of infection often resides within the biofilm on the catheter.
*Incorrect: Remove all peripheral IV's and send for cultures*
- While **peripheral IVs** can be a source of infection, the central line was placed earlier and is associated with a much higher risk of serious infection, especially in a critically ill patient.
- The patient's initial improvement followed by deterioration points more towards a **central line-associated infection** rather than new peripheral IVs placed only on day 5.
*Incorrect: Perform a lumbar puncture*
- Although the patient has altered mental status, the absence of focal neurological deficits, headache, photophobia, and neck stiffness, along with a negative **Jolt accentuation of headache**, makes **meningitis** less likely as the primary cause of deterioration.
- The more immediate and likely cause of worsening sepsis in this context is a **catheter-related infection**.
*Incorrect: Add micafungin to the patient's antibiotics*
- Adding an antifungal agent such as **micafungin** would be considered if there was a strong suspicion of a fungal infection, which is not indicated by the current blood cultures or clinical picture.
- Empiric antifungal therapy is typically reserved for patients with persistent fever refractory to broad-spectrum antibiotics, known fungal exposure, or specific risk factors.
*Incorrect: Add cefepime to the patient's antibiotics*
- The patient is already on **vancomycin and piperacillin-tazobactam**, which provides broad-spectrum coverage for both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*.
- Adding **cefepime** would broaden gram-negative coverage further but is usually unnecessary unless the current regimen is failing due to specific resistant organisms, and the more likely source of infection should be addressed first.
Urgent vs emergent conditions recognition US Medical PG Question 4: A 72-year-old woman comes to the emergency department 1 hour after the sudden onset of a diffuse, dull, throbbing headache. She also reports blurred vision, nausea, and one episode of vomiting. She has a history of poorly controlled hypertension. A photograph of her fundoscopic examination is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Hemorrhagic lacunar stroke
- B. Transient ischemic attack
- C. Giant cell arteritis
- D. Hypertensive emergency (Correct Answer)
- E. Epidural hematoma
Urgent vs emergent conditions recognition Explanation: ***Hypertensive emergency***
- The patient's presentation of a **sudden headache**, along with **blurred vision** and nausea, suggests increased intracranial pressure due to severely elevated blood pressure.
- Poorly controlled hypertension is a significant risk factor, leading to possible **end-organ damage** such as hypertensive retinopathy with papilledema or hypertensive encephalopathy.
- Fundoscopic examination showing **papilledema** confirms elevated intracranial pressure, consistent with malignant hypertension.
*Hemorrhagic lacunar stroke*
- Lacunar strokes are **small subcortical infarcts** caused by occlusion of penetrating arteries and are typically **ischemic, not hemorrhagic**.
- They present with focal neurological deficits (pure motor stroke, pure sensory stroke, ataxic hemiparesis) rather than the **diffuse symptoms** and papilledema seen here.
- While hypertension is a risk factor, lacunar infarcts do not cause increased intracranial pressure or papilledema.
*Transient ischemic attack*
- Characterized by temporary neurological deficits that resolve within 24 hours, typically without severe headaches or sustained symptoms.
- Patients may experience **focal weakness or sensory changes** but would not have papilledema or signs of increased intracranial pressure.
- The persistent nature of this patient's symptoms makes TIA unlikely.
*Giant cell arteritis*
- This condition usually presents with **temporal headaches**, jaw claudication, and potential vision loss from arteritic anterior ischemic optic neuropathy.
- Vision loss in GCA is due to ischemic optic nerve damage, not papilledema from increased intracranial pressure.
- More common in older adults but is associated with systemic symptoms like fever, malaise, and elevated ESR/CRP.
*Epidural hematoma*
- Typically follows head trauma and presents with a **lucid interval**, followed by rapid deterioration from expanding hematoma.
- Usually caused by middle meningeal artery injury with classic lens-shaped hematoma on CT.
- The lack of trauma history and the chronic hypertension make this diagnosis unlikely.
Urgent vs emergent conditions recognition US Medical PG Question 5: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Urgent vs emergent conditions recognition Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Urgent vs emergent conditions recognition US Medical PG Question 6: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Urgent vs emergent conditions recognition Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
Urgent vs emergent conditions recognition US Medical PG Question 7: A 29-year-old man presents to the emergency department with chest pain and fatigue for the past week. The patient is homeless and his medical history is not known. His temperature is 103°F (39.4°C), blood pressure is 97/58 mmHg, pulse is 140/min, respirations are 25/min, and oxygen saturation is 95% on room air. Physical exam is notable for scars in the antecubital fossa and a murmur over the left sternal border. The patient is admitted to the intensive care unit and is treated appropriately. On day 3 of his hospital stay, the patient presents with right-sided weakness in his arm and leg and dysarthric speech. Which of the following is the most likely etiology of his current symptoms?
- A. Herpes simplex virus encephalitis
- B. Septic emboli (Correct Answer)
- C. Intracranial hemorrhage
- D. Thromboembolic stroke
- E. Bacterial meningitis
Urgent vs emergent conditions recognition Explanation: ***Septic emboli***
- The patient's history of **intravenous drug use** (inferred from antecubital scars and homelessness), fever, hypotension, tachycardia, and a new murmur strongly suggest **infective endocarditis**.
- **Septic emboli** from an infected heart valve can dislodge and travel to the brain, causing a **stroke-like presentation** with focal neurological deficits such as right-sided weakness and dysarthria.
- This is the **most specific etiology** as it identifies both the embolic mechanism AND the infectious source.
*Herpes simplex virus encephalitis*
- While encephalitis can cause focal neurological deficits, it typically presents with **altered mental status, seizures**, and a distinct pattern on MRI (temporal lobe involvement), which is not the primary presentation here.
- The context of infective endocarditis makes **embolic events** a more direct and likely cause of acute focal deficits.
*Intracranial hemorrhage*
- Intracranial hemorrhage would typically cause a **sudden onset** of neurological deficits, often accompanied by severe headache, altered consciousness, and signs of increased intracranial pressure.
- Although endocarditis can rarely lead to mycotic aneurysms that rupture, **ischemic stroke** due to emboli is far more common than hemorrhage in this setting.
*Thromboembolic stroke*
- While septic emboli do cause an embolic stroke, **"thromboembolic stroke"** is a broader, less specific term that doesn't identify the **infectious etiology**.
- The term typically refers to sterile emboli from sources like atrial fibrillation, left ventricular thrombus, or atherosclerotic plaques.
- **"Septic emboli"** is the most precise answer as it specifically indicates emboli containing infected material from the endocarditis, which has important implications for treatment and prognosis.
*Bacterial meningitis*
- Meningitis typically presents with classic symptoms like **fever, headache, nuchal rigidity**, and altered mental status.
- While it can cause neurological complications, acute focal deficits like hemiparesis and dysarthria are more characteristic of a stroke or mass lesion, not diffuse meningeal inflammation.
Urgent vs emergent conditions recognition US Medical PG Question 8: A 28-year-old man is admitted to the emergency department with a gunshot wound to the abdomen. He complains of weakness and diffuse abdominal pain. Morphine is administered and IV fluids are started by paramedics at the scene. On admission, the patient’s blood pressure is 90/60 mm Hg, heart rate is 103/min, respiratory rate is 17/min, the temperature is 36.2℃ (97.1℉), and oxygen saturation is 94% on room air. The patient is responsive but lethargic. The patient is diaphoretic and extremities are pale and cool. Lungs are clear to auscultation. Cardiac sounds are diminished. Abdominal examination shows a visible bullet entry wound in the left upper quadrant (LUQ) with no corresponding exit wound on the flanks or back. The abdomen is distended and diffusely tender with a rebound. Aspiration of the nasogastric tube reveals bloody contents. Rectal examination shows no blood. Stool guaiac is negative. Which of the following is the next best step in management?
- A. Focused assessment with sonography for trauma (FAST)
- B. Abdominal CT
- C. Exploratory laparotomy (Correct Answer)
- D. Abdominal X-ray
- E. Diagnostic peritoneal lavage
Urgent vs emergent conditions recognition Explanation: ***Exploratory laparotomy***
- The patient presents with clear signs of **hemodynamic instability** (BP 90/60 mmHg, HR 103/min, lethargy, cool extremities, diminished cardiac sounds) following a **gunshot wound to the abdomen**.
- In hemodynamically unstable trauma patients with penetrating abdominal injuries, immediate **exploratory laparotomy** is indicated to identify and control hemorrhage and repair organ damage.
*Focused assessment with sonography for trauma (FAST)*
- While FAST can detect free fluid (e.g., blood) in the abdomen, it is **not sufficient to rule out significant injury** in a hemodynamically unstable patient with a penetrating abdominal wound.
- A positive FAST in a stable patient might prompt further imaging, but in this unstable case, it would delay definitive surgical intervention.
*Abdominal CT*
- Abdominal CT is useful for evaluating intra-abdominal injuries in **hemodynamically stable** patients.
- Performing a CT on this unstable patient would delay critical surgical intervention and could lead to rapid deterioration in the scanner.
*Abdominal X-ray*
- An abdominal X-ray can sometimes identify the **location of a bullet** or **free air** under the diaphragm, but it has limited utility in assessing or quantifying intra-abdominal hemorrhage or solid organ injury.
- It is not the definitive diagnostic or therapeutic step for an unstable patient with a penetrating abdominal injury.
*Diagnostic peritoneal lavage*
- DPL is an invasive procedure that can detect intra-abdominal bleeding or perforation, but it has largely been **replaced by FAST and CT scans** in hemodynamically stable patients.
- For a hemodynamically unstable patient with a clear indication for surgery (penetrating trauma and instability), DPL would delay definitive surgical management and provides less information than direct visualization via laparotomy.
Urgent vs emergent conditions recognition US Medical PG Question 9: A 65-year-old woman comes to the physician for the evaluation of sharp, stabbing pain in the lower back for 3 weeks. The pain radiates to the back of her right leg and is worse at night. She reports decreased sensation around her buttocks and inner thighs. During the last several days, she has had trouble urinating. Three years ago, she was diagnosed with breast cancer and was treated with lumpectomy and radiation. Her only medication is anastrozole. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 12/min, and blood pressure is 130/70 mm Hg. Neurologic examination shows 4/5 strength in the left lower extremity and 2/5 strength in her right lower extremity. Knee and ankle reflexes are 1+ on the right. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Anterior spinal cord syndrome
- B. Cauda equina syndrome (Correct Answer)
- C. Conus medullaris syndrome
- D. Central cord syndrome
- E. Brown-sequard syndrome
Urgent vs emergent conditions recognition Explanation: ***Cauda equina syndrome***
- The patient's presentation with **severe low back pain**, **saddle anesthesia** (decreased sensation around buttocks and inner thighs), **bladder dysfunction** (trouble urinating), and **motor weakness** in the lower extremities is highly indicative of cauda equina syndrome. This can be caused by **spinal metastases** from her breast cancer.
- The **reduced squeeze tone** of the anal sphincter, despite normal resting tone, further supports the diagnosis, indicating dysfunction of the sacral nerve roots which are compressed in cauda equina syndrome.
*Anterior spinal cord syndrome*
- This syndrome typically presents with **motor paralysis**, loss of **pain** and **temperature** sensation below the lesion, but preservation of **proprioception** and **vibration sense**.
- It does not typically cause **saddle anesthesia** or **bladder dysfunction** to the extent seen in this patient.
*Conus medullaris syndrome*
- Conus medullaris syndrome involves the lower part of the spinal cord (T12-L2) and typically presents with **symmetric motor weakness**, **early onset bladder and bowel dysfunction**, and often **perianal numbness**.
- While there is bladder dysfunction, the described **asymmetric weakness** and prominent **radicular pain** radiating down one leg are more characteristic of cauda equina syndrome, which affects nerve roots rather than the spinal cord itself.
*Central cord syndrome*
- This syndrome usually results from hyperextension injuries and leads to **greater motor impairment in the upper extremities** than in the lower extremities.
- It is often associated with a **'shawl-like' distribution** of sensory loss and does not typically present with the same severe lower extremity weakness, saddle anesthesia, or bladder dysfunction as seen in this patient.
*Brown-Sequard syndrome*
- This syndrome is characterized by **hemisection of the spinal cord**, resulting in **ipsilateral motor paralysis** and loss of **proprioception and vibration sensation** below the level of the lesion.
- It also causes **contralateral loss of pain and temperature sensation** starting a few segments below the lesion, which does not match the patient's symptoms of bilateral sensory and motor deficits with saddle anesthesia.
Urgent vs emergent conditions recognition US Medical PG Question 10: A 43-year-old woman was admitted to the hospital after a fall. When the emergency services arrived, she was unresponsive, did not open her eyes, but responded to painful stimuli. The witnesses say that she had convulsions lasting about 30 seconds when she lost consciousness after a traumatic event. On her way to the hospital, she regained consciousness. On admission, she complained of intense headaches and nausea. She opened her eyes spontaneously, was responsive but confused, and was able to follow motor commands. Her vital signs are as follows: blood pressure, 150/90 mm Hg; heart rate, 62/min; respiratory rate, 13/min; and temperature, 37.3℃ (99.1℉). There are no signs of a skull fracture. The pupils are round, equal, and poorly reactive to light. She is unable to fully abduct both eyes. Ophthalmoscopy does not show papillary edema or retinal hemorrhages. She has nuchal rigidity and a positive Kernig sign. An urgent head CT does not show any abnormalities. Which of the following is a proper investigation to perform in this patient?
- A. Lumbar puncture (Correct Answer)
- B. Angiography
- C. Sonography
- D. Brain MRI
- E. EEG
Urgent vs emergent conditions recognition Explanation: ***Lumbar puncture***
- The patient's symptoms, including **severe headache**, **nuchal rigidity**, **positive Kernig sign**, and **abnormal oculomotor findings** (poorly reactive pupils, inability to abduct eyes), despite a normal head CT, are highly suggestive of **subarachnoid hemorrhage**. A lumbar puncture is essential to look for **xanthochromia** (yellowish discoloration of CSF due to bilirubin from lysed red blood cells), which confirms the diagnosis, especially when CT is negative in the first 6-12 hours.
- The history of a "traumatic event" followed by convulsions and transient loss of consciousness, along with a "lucid interval" then renewed symptoms (headache, confusion), raises suspicion for head injury leading to hemorrhagic event. The **elevated BP and bradycardia** (Cushing's reflex components), though not fully developed, also suggest increased intracranial pressure, further warranting investigation for hemorrhage.
*Angiography*
- While angiography (CTA or conventional) is performed **after a subarachnoid hemorrhage is confirmed** to identify the source of bleeding (e.g., aneurysm), it is not the *initial* diagnostic test to *confirm* the hemorrhage itself when CT is negative.
- Doing an angiography before ruling out significant hemorrhage via LP (when CT is negative) is premature and could expose the patient to unnecessary risks without a confirmed diagnosis.
*Sonography*
- **Sonography** (ultrasound) has **no role** in the acute diagnosis of subarachnoid hemorrhage or other intracranial pathology in adults.
- It is used for imaging the brain in neonates through the open fontanelles but is ineffective through the adult skull.
*Brain MRI*
- While an **MRI is more sensitive than CT for detecting subarachnoid hemorrhage** (especially subacute hemorrhage or small bleeds missed by CT), it is generally **less readily available** in an emergency setting than CT and LP.
- In cases where CT is negative but clinical suspicion for SAH is high, **lumbar puncture is typically the next step** as it can detect early SAH via xanthochromia, which might not be immediately visible on MRI. MRI may be used later to identify causes or small bleeds not picked up by CT.
*EEG*
- An **EEG (electroencephalogram)** is used to **evaluate seizure activity** and other types of brain dysfunction related to electrical activity.
- While the patient had convulsions, the primary concern given her overall presentation (severe headache, meningeal signs, altered mental status, and cranial nerve palsies) is **subarachnoid hemorrhage**, not solely seizure. An EEG would not help diagnose the underlying cause of her acute neurological deterioration.
More Urgent vs emergent conditions recognition US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.