Red flags in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Red flags in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Red flags in pregnancy US Medical PG Question 1: A 25-year-old pregnant woman at 28 weeks gestation presents with a headache. Her pregnancy has been managed by a nurse practitioner. Her temperature is 99.0°F (37.2°C), blood pressure is 164/104 mmHg, pulse is 100/min, respirations are 22/min, and oxygen saturation is 98% on room air. Physical exam is notable for a comfortable appearing woman with a gravid uterus. Laboratory tests are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 6,700/mm^3 with normal differential
Platelet count: 100,500/mm^3
Serum:
Na+: 141 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 25 mEq/L
BUN: 21 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.0 mg/dL
AST: 32 U/L
ALT: 30 U/L
Urine:
Color: Amber
Protein: Positive
Blood: Negative
Which of the following is the most likely diagnosis?
- A. HELLP syndrome
- B. Acute fatty liver disease of pregnancy
- C. Preeclampsia
- D. Severe preeclampsia (Correct Answer)
- E. Eclampsia
Red flags in pregnancy Explanation: ***Severe preeclampsia***
- The patient exhibits **hypertension** (BP 164/104 mmHg), **proteinuria** (positive urine protein), and **thrombocytopenia** (platelet count 100,500/mm^3). The elevated BUN and creatinine also suggest **renal dysfunction**.
- The blood pressure reading 164/104 mmHg meets the criteria for **severe range blood pressure** (systolic ≥160 mmHg or diastolic ≥110 mmHg), classifying this as severe preeclampsia. Headaches are also a symptom of severe preeclampsia.
*HELLP syndrome*
- While **thrombocytopenia** is present, the **liver enzymes (AST/ALT)** are not elevated (AST 32 U/L, ALT 30 U/L), which would be a primary diagnostic criterion for HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets).
- There is no evidence of **hemolysis**, such as elevated bilirubin or schistocytes on a peripheral smear, which is also required for HELLP diagnosis.
*Acute fatty liver disease of pregnancy*
- This condition presents with significantly elevated **liver enzymes**, **jaundice**, and often severe **hypoglycemia** and **coagulopathy**, none of which are evident in this patient's lab results.
- While it can cause elevated BUN and creatinine, it typically involves **more prominent liver dysfunction** than seen here.
*Preeclampsia*
- This patient meets the criteria for preeclampsia (hypertension and proteinuria), but her **blood pressure** (164/104 mmHg), **thrombocytopenia** (platelet count 100,500/mm^3), and elevated **creatinine** (1.0 mg/dL) all point to features that classify it as *severe* preeclampsia.
- Preeclampsia without severe features generally involves blood pressure values below 160/110 mmHg and no evidence of significant organ dysfunction or severe laboratory abnormalities.
*Eclampsia*
- Eclampsia is defined as the occurrence of new-onset **grand mal seizures** in a woman with preeclampsia.
- The patient presents with a **headache** but is described as "comfortable appearing" and there is no mention of seizures.
Red flags in pregnancy US Medical PG Question 2: A 25-year-old primigravida woman at 35 weeks estimated gestational age presents with a headache for the past 5 hours. She describes the headache as severe and incapacitating and showing no response to acetaminophen. In the emergency department, her blood pressure is found to be 150/100 mm Hg, pulse is 88/min, respiratory rate is 30/min, and temperature is 37.0°C (98.6°F). Her records show that her blood pressure was the same yesterday during her regular antenatal visit. Chest auscultation reveals bilateral crackles along the lung base. Abdominal examination reveals a gravid uterus consistent with a gestational age of 32 weeks and a floating fetus in a cephalic presentation. Pelvic examination is performed which shows a closed firm cervix with no evidence of bleeding or discharge. Moderate pitting edema is noted and neurologic examination shows generalized hyperreflexia. Laboratory findings are significant for the following:
Hemoglobin 12.5 g/dL
Platelets 185,000/μL
Serum creatinine 0.4 mg/dL
Spot urine creatinine 110 mg/dL
Spot urine protein 360 mg/dL
AST 40 IU/L
Which of the following is the most likely diagnosis in this patient?
- A. Gestational hypertension
- B. Eclampsia
- C. Preeclampsia without severe features
- D. HELLP syndrome
- E. Preeclampsia with severe features (Correct Answer)
Red flags in pregnancy Explanation: ***Preeclampsia with severe features***
- This patient meets criteria for preeclampsia with severe features based on a **blood pressure ≥160/110 mm Hg** (or ≥140/90 mm Hg with severe features), **new-onset proteinuria**, and symptoms such as **severe headache**, **pulmonary edema** (bilateral crackles), and **hyperreflexia**. The blood pressure was 150/100, which is elevated. The proteinuria is significant, and the **spot urine protein-to-creatinine ratio is 3.27**, which is greater than 0.3.
- The severe headache, pulmonary edema, and hyperreflexia are all indicative of severe features, requiring prompt management to prevent complications like eclampsia.
*Gestational hypertension*
- **Gestational hypertension** is diagnosed when there is persistent hypertension (BP ≥140/90 mmHg) after 20 weeks of gestation **without proteinuria** or other signs of end-organ damage.
- This patient has significant proteinuria and symptoms of end-organ compromise (headache, pulmonary edema, hyperreflexia), which rules out gestational hypertension.
*Eclampsia*
- **Eclampsia** is characterized by the onset of **seizures** in a woman with preeclampsia, which is not described in this case.
- While the patient has severe features of preeclampsia and is at high risk for eclampsia, she has not yet experienced a seizure.
*Preeclampsia without severe features*
- **Preeclampsia without severe features** involves hypertension and proteinuria **without** any of the severe signs or symptoms.
- This patient presents with a **severe headache**, **pulmonary edema**, and **hyperreflexia**, all of which are defining characteristics of preeclampsia with severe features.
*HELLP syndrome*
- **HELLP syndrome** is a severe form of preeclampsia characterized by **Hemolysis**, **Elevated Liver enzymes**, and **Low Platelet count**.
- This patient's laboratory results show **normal platelets (185,000/μL)** and **normal AST (40 IU/L)**, ruling out HELLP syndrome.
Red flags in pregnancy US Medical PG Question 3: A 28-year-old woman, gravida 2, para 1, at 30 weeks' gestation comes to the physician because of headache for the past 5 days. Her pregnancy has been uncomplicated to date. Pregnancy and vaginal delivery of her first child were uncomplicated. The patient does not smoke or drink alcohol. She does not use illicit drugs. Medications include folic acid and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 82/min, and blood pressure is 150/92 mm Hg. Physical examination reveals 2+ pitting edema in the lower extremities. Laboratory studies show:
Hemoglobin 11.8 g/dL
Platelet count 290,000/mm3
Urine
pH 6.3
Protein 2+
WBC negative
Bacteria occasional
Nitrites negative
The patient is at increased risk of developing which of the following complications?
- A. Abruptio placentae (Correct Answer)
- B. Polyhydramnios
- C. Uterine rupture
- D. Spontaneous abortion
- E. Placenta previa
Red flags in pregnancy Explanation: ***Abruptio placentae***
- The patient presents with **preeclampsia** (new-onset hypertension after 20 weeks gestation, proteinuria, and edema), which is a significant risk factor for **placental abruption**.
- Preeclampsia can lead to **vasoconstriction** and **decidual hemorrhage**, causing premature separation of the placenta from the uterine wall.
*Polyhydramnios*
- **Polyhydramnios** is an excess of amniotic fluid, typically associated with **fetal anomalies** (e.g., esophageal atresia, anencephaly) or **maternal diabetes**, none of which are indicated here.
- While it can complicate pregnancy, it is not directly linked to preeclampsia as a primary complication.
*Uterine rupture*
- **Uterine rupture** is a rare but catastrophic event, most commonly associated with a **prior Cesarean section**, extensive uterine surgery, or **traumatic injury**.
- This patient had an uncomplicated vaginal delivery previously, and there are no signs suggesting a heightened risk for uterine rupture.
*Spontaneous abortion*
- **Spontaneous abortion** occurs before 20 weeks of gestation. This patient is at **30 weeks' gestation**, making spontaneous abortion highly unlikely.
- The term for pregnancy loss after 20 weeks is stillbirth, which is also not the most immediate or direct complication linked to preeclampsia for the mother.
*Placenta previa*
- **Placenta previa** occurs when the placenta covers the cervical os, a condition diagnosed by **ultrasound** and presenting with **painless vaginal bleeding**.
- Preeclampsia does not directly cause placenta previa; these are distinct obstetric complications with different etiologies.
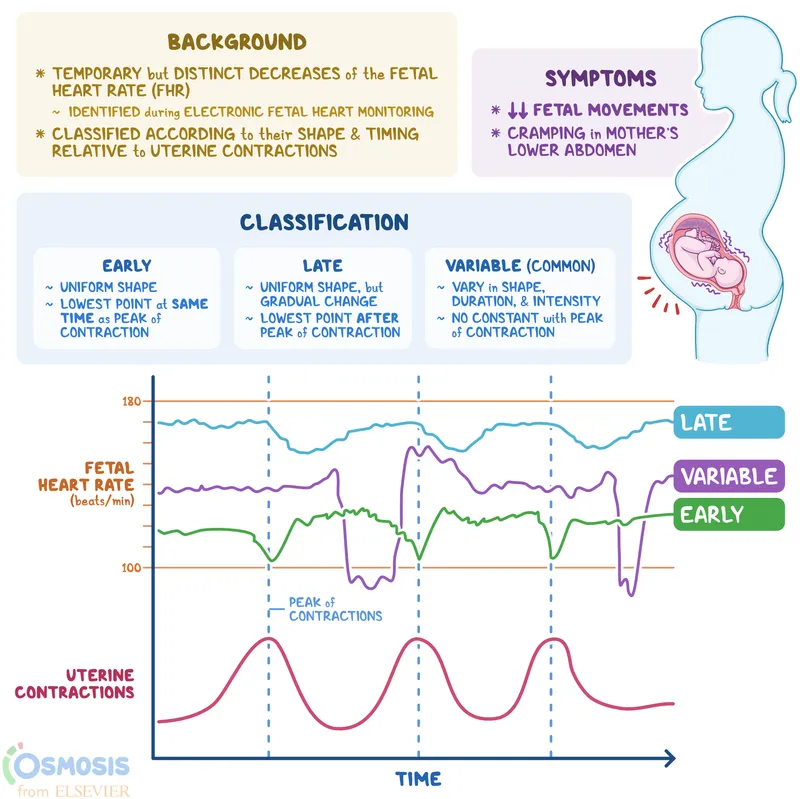
Red flags in pregnancy US Medical PG Question 4: A 32-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the emergency department because of vaginal bleeding for the past hour. The patient reports that she felt contractions prior to the onset of the bleeding, but the contractions stopped after the bleeding started. She also has severe abdominal pain. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 110/min, respirations are 17/min, and blood pressure is 90/60 mm Hg. Examination shows diffuse abdominal tenderness with no rebound or guarding; no contractions are felt. The fetal heart rate shows recurrent variable decelerations. Which of the following is the most likely diagnosis?
- A. Uterine inertia
- B. Amniotic fluid embolism
- C. Uterine rupture (Correct Answer)
- D. Vasa previa
- E. Abruptio placentae
Red flags in pregnancy Explanation: ***Uterine rupture***
- The patient's history of a prior **cesarean section**, sudden onset of **vaginal bleeding** and **severe abdominal pain**, resolution of contractions, and signs of **hypovolemic shock** (tachycardia, hypotension) coupled with fetal distress (variable decelerations) are highly indicative of uterine rupture.
- Diffuse abdominal tenderness without rebound or guarding, and no palpable contractions, are also consistent with rupture.
*Uterine inertia*
- This condition is characterized by **weak or uncoordinated uterine contractions** leading to prolonged labor, but it does not typically present with acute vaginal bleeding, sudden severe abdominal pain, or hypovolemic shock.
- Fetal distress in uterine inertia would more likely be due to prolonged labor rather than acute compromise following a sudden event.
*Amniotic fluid embolism*
- This is a rare, life-threatening obstetric emergency characterized by sudden **cardiovascular collapse, respiratory distress**, and **coagulopathy**, often occurring during labor or immediately postpartum.
- While it can cause fetal distress, vaginal bleeding and severe abdominal pain are not primary presenting symptoms.
*Vasa previa*
- Characterized by **painless vaginal bleeding** when fetal vessels within the membranes cross the internal cervical os, making them vulnerable to rupture during cervical dilation or amniotomy.
- The bleeding is typically fetal blood, and fetal distress occurs rapidly, but the mother would not experience severe abdominal pain or signs of hypovolemic shock unless the bleeding is substantial and prolonged.
*Abruptio placentae*
- This involves the **premature separation of the placenta**, causing painful vaginal bleeding, uterine tenderness, and frequent, strong contractions.
- While it can cause hypovolemic shock and fetal distress, the description of contractions stopping after bleeding started, along with a previous C-section scar, points more specifically to uterine rupture rather than an abruption.
Red flags in pregnancy US Medical PG Question 5: A 31-year-old G1P0 woman with a history of hypertension presents to the emergency department because she believes that she is in labor. She is in her 38th week of pregnancy and her course has thus far been uncomplicated. This morning, she began feeling painful contractions and noted vaginal bleeding after she fell off her bike while riding to work. She is experiencing lower abdominal and pelvic pain between contractions as well. Her temperature is 97.6°F (36.4°C), blood pressure is 177/99 mmHg, pulse is 100/min, respirations are 20/min, and oxygen saturation is 98% on room air. Physical exam is notable for a gravid and hypertonic uterus and moderate blood in the vaginal vault. Ultrasound reveals no abnormalities. Which of the following is the most likely diagnosis?
- A. Uterine rupture
- B. Abruptio placentae (Correct Answer)
- C. Placenta previa
- D. Normal labor
- E. Vasa previa
Red flags in pregnancy Explanation: ***Abruptio placentae***
- Vaginal bleeding after **trauma** (fall off bike), **hypertension**, and a **hypertonic uterus** with **lower abdominal/pelvic pain** between contractions are classic signs of placental abruption.
- Abruption occurs when the **placenta prematurely separates** from the uterine wall, leading to bleeding and uterine irritability.
*Uterine rupture*
- While uterine rupture involves abdominal pain and bleeding, it typically presents with **fetal distress**, **loss of uterine tone**, and a feeling of **'ripping'** or tearing, none of which are described.
- A uterine rupture is more common in women with a history of **prior C-section** or uterine surgery, which is not mentioned here.
*Placenta previa*
- Characterized by **painless vaginal bleeding** in the late second or third trimester, often with a soft, non-tender uterus.
- The presence of **painful contractions**, a **hypertonic uterus**, and a clear cause of trauma rules out placenta previa.
*Normal labor*
- While this patient is in labor, the presence of **significant vaginal bleeding**, **post-traumatic onset**, and **severe lower abdominal pain** between contractions are not typical for uncomplicated normal labor.
- Normal labor contractions are usually regular and progress, but the associated symptoms point to a more serious underlying issue.
*Vasa previa*
- Characterized by **fetal blood vessels** running within the membranes over the cervical os, leading to **painless vaginal bleeding** when these vessels rupture.
- This condition is often associated with **fetal distress** and **fetal hemorrhage**, which is not indicated here, and bleeding typically occurs upon rupture of membranes, not from trauma.
Red flags in pregnancy US Medical PG Question 6: A 29-year-old woman presents to a medical office complaining of fatigue, nausea, and vomiting for 1 week. Recently, the smell of certain foods makes her nauseous. Her symptoms are more pronounced in the mornings. The emesis is clear-to-yellow without blood. She has had no recent travel out of the country. The medical history is significant for peptic ulcer, for which she takes pantoprazole. The blood pressure is 100/60 mm Hg, the pulse is 70/min, and the respiratory rate is 12/min. The physical examination reveals pale mucosa and conjunctiva, and bilateral breast tenderness. The LMP was 9 weeks ago. What is the most appropriate next step in the management of this patient?
- A. Beta-HCG levels and a transvaginal ultrasound (Correct Answer)
- B. Beta-HCG levels and a transabdominal ultrasound
- C. Beta-HCG levels and a pelvic CT
- D. Abdominal x-ray
- E. Abdominal CT with contrast
Red flags in pregnancy Explanation: ***Beta-HCG levels and a transvaginal ultrasound***
- The patient's symptoms (fatigue, nausea, vomiting, morning sickness, breast tenderness, and **amenorrhea** for 9 weeks) strongly suggest **early pregnancy**.
- **Urine or serum beta-HCG** confirms pregnancy, and a **transvaginal ultrasound** is crucial for confirming an **intrauterine pregnancy**, estimating gestational age, and ruling out complications like ectopic pregnancy, especially at this early stage when transabdominal ultrasound might not provide clear images.
*Beta-HCG levels and a transabdominal ultrasound*
- While beta-HCG levels are appropriate, a **transabdominal ultrasound** may not be sufficient to visualize an early intrauterine pregnancy at 9 weeks due to limited resolution compared to transvaginal ultrasound.
- A definitive confirmation of **intrauterine pregnancy** is critical to rule out an **ectopic pregnancy**, which is better achieved with transvaginal imaging in early gestation.
*Beta-HCG levels and a pelvic CT*
- **CT scans** expose the patient to significant **ionizing radiation**, which is **contraindicated in pregnancy** unless absolutely necessary for life-threatening conditions.
- While it could identify some pelvic pathologies, it is **not the primary imaging modality** for confirming or evaluating early pregnancy due to radiation risks and inferior soft tissue resolution for early gestational sacs compared to ultrasound.
*Abdominal x-ray*
- An **abdominal X-ray** involves **ionizing radiation** and offers very limited diagnostic value for early pregnancy, as it cannot visualize the gestational sac, fetus, or fetal heart activity.
- It is **contraindicated** in suspected pregnancy due to the risk of fetal harm.
*Abdominal CT with contrast*
- **Abdominal CT with contrast** involves both **ionizing radiation** and **contrast agents**, both of which pose significant risks to a developing fetus.
- It is an **inappropriate initial step** for suspected pregnancy and offers no specific diagnostic benefits for confirming or characterizing early gestation.
Red flags in pregnancy US Medical PG Question 7: A previously healthy 29-year-old Taiwanese woman comes to the emergency department with vaginal bleeding and pelvic pressure for several hours. Over the past 2 weeks, she had intermittent nausea and vomiting. A home urine pregnancy test was positive 10 weeks ago. She has had no prenatal care. Her pulse is 80/min and blood pressure is 150/98 mm Hg. Physical examination shows warm and moist skin. Lungs are clear to auscultation bilaterally. Her abdomen is soft and non-distended. Bimanual examination shows a uterus palpated at the level of the umbilicus. Her serum beta human chorionic gonadotropin concentration is 110,000 mIU/mL. Urine dipstick is positive for protein and ketones. Transvaginal ultrasound shows a central intrauterine mass with hypoechoic spaces; there is no detectable fetal heart rate. An x-ray of the chest shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Serial beta-hCG measurement
- B. Bed rest and doxylamine therapy
- C. Methotrexate therapy
- D. Suction curettage (Correct Answer)
- E. Insulin therapy
Red flags in pregnancy Explanation: ***Suction curettage***
- The patient's symptoms (vaginal bleeding, pelvic pressure, nausea/vomiting), signs (hypertension, large for gestational age uterus at the umbilicus corresponding to 20 weeks gestation, proteinuria), and laboratory findings (markedly elevated beta-hCG of 110,000 mIU/mL) are highly suggestive of a **hydatidiform mole**.
- A **transvaginal ultrasound** showing a central intrauterine mass with **hypoechoic spaces** (often described as a 'snowstorm' or 'grape-like' appearance) and no fetal heart rate confirms the diagnosis of a **molar pregnancy**. The most appropriate and urgent management is **suction curettage** to remove the abnormal pregnancy tissue, which also serves a diagnostic purpose.
*Serial beta-hCG measurement*
- While **serial beta-hCG** measurements are crucial for monitoring after treatment of a molar pregnancy to detect persistent trophoblastic disease, they are not the initial management step for an active molar pregnancy with acute symptoms.
- This step would delay the necessary removal of the abnormal tissue and risk complications such as hemorrhage or progression to **gestational trophoblastic neoplasia (GTN)**.
*Bed rest and doxylamine therapy*
- **Bed rest and doxylamine** are treatments for benign conditions like **hyperemesis gravidarum** or threatened abortion, which do not align with the severe symptoms, physical findings, and ultrasound characteristics of this patient's condition.
- This approach would be completely inadequate and inappropriate for a molar pregnancy.
*Methotrexate therapy*
- **Methotrexate** is a chemotherapy agent used to treat **persistent gestational trophoblastic neoplasia (GTN)** or **choriocarcinoma** following molar pregnancy evacuation, or in cases of ectopic pregnancy.
- It is not the primary treatment for the initial removal of a molar pregnancy itself, which requires surgical evacuation.
*Insulin therapy*
- **Insulin therapy** is used to manage **gestational diabetes mellitus (GDM)** or pre-existing diabetes in pregnancy.
- There is no clinical or laboratory evidence (e.g., elevated glucose) to suggest diabetes in this patient, and it is unrelated to the primary diagnosis of molar pregnancy.
Red flags in pregnancy US Medical PG Question 8: A 55-year-old man presents to his primary care physician for trouble swallowing. The patient claims that he used to struggle when eating food if he did not chew it thoroughly, but now he occasionally struggles with liquids as well. He also complains of a retrosternal burning sensation whenever he eats. He also claims that he feels his throat burns when he lays down or goes to bed. Otherwise, the patient has no other complaints. The patient has a past medical history of obesity, diabetes, constipation, and anxiety. His current medications include insulin, metformin, and lisinopril. On review of systems, the patient endorses a 5 pound weight loss recently. The patient has a 22 pack-year smoking history and drinks alcohol with dinner. His temperature is 99.5°F (37.5°C), blood pressure is 177/98 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note an overweight man in no current distress. Abdominal exam is within normal limits. Which of the following is the best next step in management?
- A. Endoscopy (Correct Answer)
- B. Omeprazole trial
- C. Manometry
- D. Barium swallow
- E. CT scan
Red flags in pregnancy Explanation: ***Endoscopy***
- The patient presents with **dysphagia to solids and liquids**, significant for **recent weight loss**, and a **history of smoking**, all of which are **alarm symptoms** necessitating an upper endoscopy to rule out malignancy.
- While he has **GERD symptoms** as well (retrosternal burning), the presence of alarm features mandates a direct investigation of the upper GI tract rather than empirical treatment.
*Omeprazole trial*
- An empirical trial of **PPIs** like omeprazole is appropriate for classic GERD symptoms without alarm features.
- However, **dysphagia to solids and liquids with associated weight loss**, especially in a patient with a significant **smoking history**, are alarm symptoms that require direct visualization via endoscopy, not just symptom management.
*Manometry*
- **Esophageal manometry** is used to evaluate the motility of the esophagus and diagnose conditions like achalasia or esophageal spasm.
- While the patient has dysphagia, **alarm symptoms (weight loss, smoking history)** raise concern for mechanical obstruction or malignancy, which should be investigated before motility disorders.
*Barium swallow*
- A **barium swallow** can identify structural abnormalities like strictures, masses, or webs, and also assess motility.
- However, in the context of alarm symptoms, a **barium swallow is less sensitive** for detecting subtle mucosal changes or early malignancy compared to endoscopy, and any positive findings would still prompt an endoscopy.
*CT scan*
- A **CT scan of the chest and abdomen** is useful for assessing extraluminal pathology, mediastinal involvement, or distant metastases.
- While it may eventually be part of staging if a malignancy is found, the **initial investigation for esophageal symptoms and alarm features** focuses on direct luminal visualization with endoscopy to identify the primary pathology.
Red flags in pregnancy US Medical PG Question 9: A 67-year-old man with type 2 diabetes mellitus and benign prostatic hyperplasia comes to the physician because of a 2-day history of sneezing and clear nasal discharge. He has had similar symptoms occasionally in the past. His current medications include metformin and tamsulosin. Examination of the nasal cavity shows red, swollen turbinates. Which of the following is the most appropriate pharmacotherapy for this patient's condition?
- A. Nizatidine
- B. Diphenhydramine
- C. Amoxicillin
- D. Theophylline
- E. Desloratadine (Correct Answer)
Red flags in pregnancy Explanation: **Desloratadine**
* This patient presents with symptoms consistent with **allergic rhinitis** (sneezing, clear nasal discharge, red/swollen turbinates, recurrent episodes). Desloratadine is a **second-generation antihistamine** that effectively treats these symptoms with minimal sedative effects, making it suitable for an elderly patient.
* It is a **non-sedating** antihistamine, which is crucial for elderly patients due to their increased sensitivity to sedative effects and potential for falls or cognitive impairment with first-generation antihistamines.
*Nizatidine*
* **Nizatidine** is an **H2-receptor antagonist** primarily used to treat gastroesophageal reflux disease (GERD) and peptic ulcers, not allergic rhinitis.
* It specifically blocks histamine H2 receptors in the stomach to reduce acid secretion and would not alleviate nasal congestion or sneezing.
*Diphenhydramine*
* **Diphenhydramine** is a **first-generation antihistamine** that is commonly used for allergic symptoms. However, it causes significant **sedation and anticholinergic side effects** (e.g., urinary retention, dry mouth, blurred vision).
* Given the patient's age and **benign prostatic hyperplasia (BPH)**, diphenhydramine is contraindicated. Its **anticholinergic effects** can inhibit bladder detrusor muscle contraction, leading to **urinary retention**, which is particularly problematic in elderly men with BPH who already have obstructive urinary symptoms.
*Amoxicillin*
* **Amoxicillin** is an **antibiotic** used to treat bacterial infections. This patient's symptoms (clear nasal discharge, sneezing, similar past episodes) are characteristic of **allergic or viral rhinitis**, not a bacterial infection.
* Using antibiotics for non-bacterial conditions contributes to **antibiotic resistance** and provides no therapeutic benefit for allergic symptoms.
*Theophylline*
* **Theophylline** is a **bronchodilator** primarily used for chronic respiratory conditions like asthma and COPD. It is not indicated for the treatment of allergic rhinitis.
* It has a **narrow therapeutic index** and can cause significant side effects (e.g., nausea, arrhythmias, seizures), making it an inappropriate and potentially dangerous choice for allergic rhinitis.
Red flags in pregnancy US Medical PG Question 10: A 14-year-old boy presents with abdominal pain and diarrhea after returning from an East Asian vacation. Stool sample reveals the presence of red and white blood cells. Stool culture shows growth of immobile, non-lactose fermenting gram-negative rods. The attending physician explains to the medical students that the bacteria function by invading intestinal M-cells. The bacterium responsible for this patient's infection is:
- A. Shigella dysenteriae (Correct Answer)
- B. Salmonella enteritidis
- C. Helicobacter pylori
- D. Escherichia coli
- E. Vibrio cholerae
Red flags in pregnancy Explanation: ***Shigella dysenteriae***
- The combination of **abdominal pain**, **bloody diarrhea** (red and white blood cells in stool), **immobile, non-lactose fermenting gram-negative rods**, and **invasion of M-cells** is classic for *Shigella* infection.
- *Shigella* species, particularly *S. dysenteriae*, cause **dysentery** by directly invading and destroying the intestinal epithelium, often in M-cells, leading to inflammation and ulceration.
*Salmonella enteritidis*
- While *Salmonella enteritidis* is also a **non-lactose fermenting gram-negative rod** and can cause diarrhea, it is typically **motile** (unlike the immobile bacteria described) and invades enterocytes, not specifically M-cells for its primary pathogenic mechanism.
- While it can cause bloody diarrhea, the **immotility** and primary M-cell invasion point away from *Salmonella*.
*Helicobacter pylori*
- *Helicobacter pylori* is a **spiral-shaped, gram-negative bacterium** primarily associated with gastritis and peptic ulcers, not acute bloody diarrhea.
- It colonizes the stomach lining and is not characteristically an immobile, non-lactose fermenting rod found in diarrheal stool.
*Vibrio cholerae*
- *Vibrio cholerae* causes **profuse watery diarrhea** (cholera) and is characterized by a **comma-shaped gram-negative rod** that is highly motile.
- It does not cause bloody diarrhea or invade M-cells; its pathogenicity is due to the production of an enterotoxin.
*Escherichia coli*
- While *E. coli* is a **gram-negative rod** and some strains can cause diarrhea (e.g., EHEC, ETEC), most strains are **lactose fermenting**.
- Pathogenic *E. coli* strains have various mechanisms, but the specific combination of **immobile, non-lactose fermenting rods with M-cell invasion** leading to dysentery is not characteristic of common diarrheagenic *E. coli*.
More Red flags in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.