Red flags in neurological complaints US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Red flags in neurological complaints. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Red flags in neurological complaints US Medical PG Question 1: A 58-year-old woman is brought to the emergency room by her husband complaining, “I can’t see out of my right eye.” She was watching television last night when she covered her left eye due to an itch and discovered that she could not see. The patient denies any precipitating event, pain, swelling, flashes, floaters, or headaches. Her past medical history is significant for uncontrolled hypertension and angina. Her medications include hydrochlorothiazide, lisinopril, atorvastatin, and nitroglycerin as needed. Her physical examination is unremarkable. Fundus examination demonstrates generalized pallor and slight disc edema with no hemorrhages. What is the most likely explanation for this patient’s symptoms?
- A. Inflammation of the temporal artery
- B. Occlusion of the ophthalmic artery by embolus (Correct Answer)
- C. Optic neuritis
- D. Detachment of the retina
Red flags in neurological complaints Explanation: ***Occlusion of the ophthalmic artery by embolus***
- The sudden, painless monocular vision loss ("I can't see out of my right eye") in a patient with risk factors like **uncontrolled hypertension** and **angina** (suggesting atherosclerosis) is highly indicative of an **ophthalmic artery occlusion**, likely due to an **embolus**.
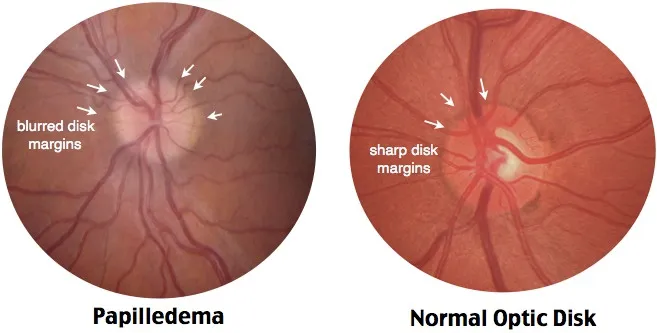
- **Fundus examination** findings of **generalized pallor** and **slight disc edema with no hemorrhages** further support this, as it reflects ischemia without significant venous congestion.
*Inflammation of the temporal artery*
- This typically presents with **temporal headache**, **jaw claudication**, and elevated inflammatory markers like **ESR**, none of which are mentioned here.
- While it can cause sudden vision loss (due to **anterior ischemic optic neuropathy**), the absence of other classic symptoms makes it less likely, and funduscopic findings often include a **pale, swollen optic disc**.
*Optic neuritis*
- Often causes **painful monocular vision loss** and is associated with **multiple sclerosis**.
- Funduscopic examination may show a normal optic disc if retrobulbar, or **optic disc hyperemia** and swelling if papillitis, but not generalized retinal pallor.
*Detachment of the retina*
- Usually presents with symptoms like **flashes, floaters**, and a **"curtain-like" visual field defect**, which the patient specifically denies.
- Fundus examination would reveal the detached retina, not generalized pallor of the fundus.
Red flags in neurological complaints US Medical PG Question 2: A 67-year-old man presents to the emergency department for a headache. The patient states his symptoms started thirty minutes ago. He states he experienced a sudden and severe headache while painting his house, causing him to fall off the ladder and hit his head. He has also experienced two episodes of vomiting and difficulty walking since the fall. The patient has a past medical history of hypertension, obesity, and atrial fibrillation. His current medications include lisinopril, rivaroxaban, atorvastatin, and metformin. His temperature is 99.5°F (37.5°C), blood pressure is 150/105 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. On physical exam, the patient localizes his headache to the back of his head. Cardiac exam reveals a normal rate and rhythm. Pulmonary exam reveals minor bibasilar crackles. Neurological exam is notable for minor weakness of the muscles of facial expression. Examination of cranial nerve three reveals a notable nystagmus. Heel to shin exam is abnormal bilaterally. The patient's gait is notably ataxic. A non-contrast CT scan of the head is currently pending. Which of the following is the most likely diagnosis?
- A. Pontine hemorrhage
- B. Cerebellar hemorrhage (Correct Answer)
- C. Subarachnoid hemorrhage
- D. Thalamic hemorrhage
- E. Subdural hematoma
Red flags in neurological complaints Explanation: ***Cerebellar hemorrhage***
- The sudden onset of a **severe headache**, localized to the back of the head, combined with **ataxia**, nystagmus, and minor facial weakness, in a patient on **anticoagulation** (rivaroxaban) for atrial fibrillation, strongly suggests a cerebellar hemorrhage.
- **Vomiting** and **difficulty walking** are common symptoms due to the cerebellar involvement and increased intracranial pressure.
*Pontine hemorrhage*
- Pontine hemorrhages typically present with **quadriplegia**, profound **coma**, and **pinpoint pupils**, which are not observed in this patient.
- While it can cause sudden headache and vomiting, the specific neurological deficits (ataxia, nystagmus, mild facial weakness) are less characteristic of a pontine lesion.
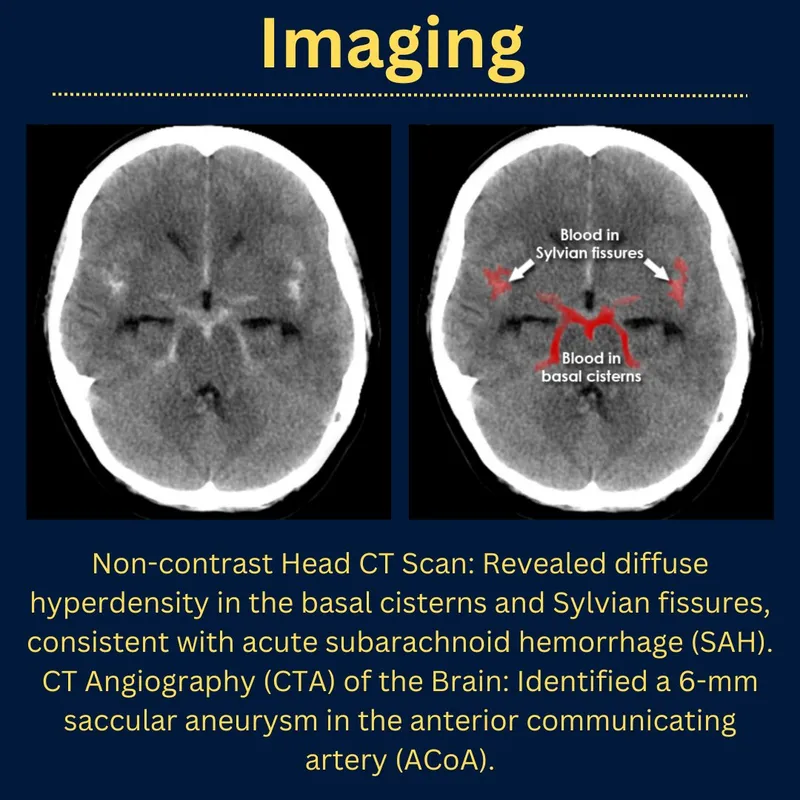
*Subarachnoid hemorrhage*
- Characterized by a **"thunderclap" headache** (sudden and severe), often described as the "worst headache of my life," and can cause focal neurological deficits depending on the location of rupture.
- While the sudden onset and severity fit, the specific cerebellar signs (**nystagmus**, **ataxia**, posterior headache) point more directly to a cerebellar lesion, and the fall causing head trauma suggests a hemorrhage within the brain parenchyma.
*Thalamic hemorrhage*
- Thalamic hemorrhages commonly present with **contralateral hemisensory loss**, hemiparesis, and sometimes pupillary abnormalities.
- The patient's presentation with prominent **ataxia**, nystagmus, and posterior headache is less typical for a thalamic hemorrhage.
*Subdural hematoma*
- Subdural hematomas usually result from **trauma** and can have a more **insidious onset** (especially chronic subdural hematomas in elderly or anticoagulated patients).
- While the fall might suggest this, the acute onset of severe headache and the specific neurological signs like **ataxia** and nystagmus are more indicative of an intraparenchymal hemorrhage (like cerebellar) rather than a subdural collection compressing the brain surface.
Red flags in neurological complaints US Medical PG Question 3: A 25-year-old male patient presents to your clinic in significant distress. He states he has excruciating, stabbing pain around the left side of his head, and his left eye will not stop tearing. These types of headaches have been occurring for the past week every morning when he awakens and last around 60 minutes. He denies any aura, nausea, or vomiting. He denies any other past medical history. What is this patient's diagnosis?
- A. Cluster headache (Correct Answer)
- B. Trigeminal neuralgia
- C. Migraine headache
- D. Short-lasting unilateral neuralgiform headaches with conjunctival injection and tearing (SUNCT) syndrome
- E. Chronic paroxysmal hemicrania (CPH)
Red flags in neurological complaints Explanation: ***Cluster headache***
- This patient's symptoms are classic for a cluster headache: **excruciating unilateral pain** around the orbit, **lacrimation** (tearing), and a **circadian rhythm** (occurring at a similar time each day, often upon awakening).
- The **brief duration** (60 minutes) and the absence of aura, nausea, or vomiting further support this diagnosis.
*Trigeminal neuralgia*
- Characterized by **sudden, severe, electric shock-like facial pain** along the distribution of the trigeminal nerve, often triggered by touch or movement.
- While the pain is severe and unilateral, it typically involves the face and not specifically orbital tearing, and the duration is usually seconds to minutes, not an hour.
*Migraine headache*
- Migraines are typically associated with **pulsating pain**, often unilateral, and accompanied by **nausea, vomiting, photophobia, and phonophobia**.
- Although unilateral, the described tearing, stabbing pain, and short duration without associated symptoms like nausea or vomiting make migraine less likely.
*Short-lasting unilateral neuralgiform headaches with conjunctival injection and tearing (SUNCT) syndrome*
- SUNCT is characterized by **very frequent (up to 200 times a day), short-duration (5-240 seconds) jabs of unilateral pain** with prominent autonomic features like conjunctival injection and tearing.
- The duration of the attacks (60 minutes) in this patient is too long for SUNCT syndrome.
*Chronic paroxysmal hemicrania (CPH)*
- CPH involves **frequent (5-40 per day), moderate to severe unilateral pain attacks** lasting 2-45 minutes, associated with autonomic symptoms.
- A key differentiating feature is its **absolute responsiveness to indomethacin**, and while similar to cluster, the attacks are typically shorter and more frequent than described here.
Red flags in neurological complaints US Medical PG Question 4: A 73-year-old man noted a rapid onset of severe dizziness and difficulty swallowing while watching TV at home. His wife reports that he had difficulty forming sentences and his gait was unsteady at this time. Symptoms were severe within 1 minute and began to improve spontaneously after 10 minutes. He has had type 2 diabetes mellitus for 25 years and has a 50 pack-year smoking history. On arrival to the emergency department 35 minutes after the initial development of symptoms, his manifestations have largely resolved with the exception of a subtle nystagmus and ataxia. His blood pressure is 132/86 mm Hg, the heart rate is 84/min, and the respiratory rate is 15/min. After 45 minutes, his symptoms are completely resolved, and neurological examination is unremarkable. Which of the following is the most likely cause of this patient’s condition?
- A. Anterior cerebral artery occlusion
- B. Middle cerebral artery occlusion
- C. Posterior cerebral artery occlusion
- D. Lenticulostriate artery occlusion
- E. Vertebral artery occlusion (Correct Answer)
Red flags in neurological complaints Explanation: ***Vertebral artery occlusion***
- The patient's symptoms of **severe dizziness**, **difficulty swallowing**, **dysarthria**, **unsteady gait**, **nystagmus**, and **ataxia** are classic manifestations of **posterior circulation ischemia**, which is supplied by the vertebral and basilar arteries.
- The rapid onset, transient nature, and complete resolution of symptoms suggest a **transient ischemic attack (TIA)** affecting the posterior cerebral circulation, often due to **vertebral artery stenosis** or a **vertebral artery embolus**.
*Anterior cerebral artery occlusion*
- Occlusion of the anterior cerebral artery typically causes **contralateral leg weakness**, sensory loss, and behavioral changes, which are not seen in this patient.
- Symptoms like dizziness and dysphagia are **not characteristic** of anterior cerebral artery involvement.
*Middle cerebral artery occlusion*
- Middle cerebral artery occlusion commonly presents with **contralateral arm and facial weakness**, aphasia (if the dominant hemisphere is affected), and visual field defects.
- The patient's symptoms are localized to the **brainstem/cerebellum**, not the MCA territory.
*Posterior cerebral artery occlusion*
- While the posterior cerebral artery is part of the posterior circulation, its occlusion primarily causes **contralateral homonymous hemianopia** and, if severe, memory deficits or alexia.
- It typically **does not cause severe dizziness**, dysphagia, or gait ataxia as prominent initial symptoms.
*Lenticulostriate artery occlusion*
- Lenticulostriate arteries supply deep structures like the **basal ganglia** and **internal capsule**. Occlusion typically leads to **pure motor** or **pure sensory lacunar strokes**.
- This patient's constellation of symptoms (dizziness, dysphagia, ataxia) is **too widespread for a typical lacunar infarct** in the lenticulostriate territory.
Red flags in neurological complaints US Medical PG Question 5: A 69-year-old male presents to the emergency room with back pain. He has a history of personality disorder and metastatic prostate cancer and was not a candidate for surgical resection. He began chemotherapy but discontinued due to unremitting nausea. He denies any bowel or bladder incontinence. He has never had pain like this before and is demanding morphine. The nurse administers IV morphine and he feels more comfortable. Vital signs are stable. On physical examination you note tenderness to palpation along the lower spine, weakness in the bilateral lower extremities, left greater than right. Neurological examination is also notable for hyporeflexia in the knee and ankle jerks bilaterally. You conduct a rectal examination, which reveals saddle anesthesia. Regarding this patient, what is the most likely diagnosis and the appropriate next step in management?
- A. The most likely diagnosis is cauda equina syndrome and the patient should be rushed to radiation
- B. The most likely diagnosis is conus medullaris syndrome and steroids should be started prior to MRI
- C. The most likely diagnosis is cauda equina syndrome and steroids should be started prior to MRI (Correct Answer)
- D. The most likely diagnosis is conus medullaris syndrome and steroids should be started after MRI
- E. The most likely diagnosis is cauda equina syndrome and steroids should be started after MRI
Red flags in neurological complaints Explanation: ***The most likely diagnosis is cauda equina syndrome and steroids should be started prior to MRI***
- The patient's presentation with **back pain**, **bilateral lower extremity weakness** (left > right), **hyporeflexia**, and **saddle anesthesia** are classic signs of **cauda equina syndrome**. This is often caused by compression of the nerve roots below the spinal cord, commonly from metastasis in patients with a history of prostate cancer.
- Given the suspected **spinal cord compression** due to metastatic disease, initiating **high-dose corticosteroids** (like dexamethasone) before imaging is crucial to reduce edema around the spinal cord and preserve neurological function. An **urgent MRI** is the next step to confirm the diagnosis and localize the compression.
*The most likely diagnosis is cauda equina syndrome and the patient should be rushed to radiation*
- While **cauda equina syndrome** is the correct diagnosis, **radiation** is typically a definitive treatment modality for metastatic compression, not an immediate next step before confirming the extent and location of compression with imaging.
- **Corticosteroids** are the immediate priority to reduce swelling and improve neurological outcomes while awaiting definitive imaging and treatment planning.
*The most likely diagnosis is conus medullaris syndrome and steroids should be started prior to MRI*
- **Conus medullaris syndrome** typically presents with more symmetrical symptoms, often including early-onset **bladder and bowel dysfunction** and **hyperreflexia** (or mixed reflexes), which are not fully consistent with this patient's presentation of hyporeflexia and lack of incontinence.
- Although steroids would be appropriate for suspected compression before MRI for either syndrome, the specific symptom profile strongly favors cauda equina over conus.
*The most likely diagnosis is conus medullaris syndrome and steroids should be started after MRI*
- The patient's symptoms (weakness, hyporeflexia, saddle anesthesia) are more indicative of **cauda equina syndrome** rather than **conus medullaris syndrome** (which often involves hyperreflexia and earlier bowel/bladder dysfunction).
- Delaying **corticosteroids** until after the MRI in suspected spinal cord compression can lead to irreversible neurological damage, as they help reduce edema immediately.
*The most likely diagnosis is cauda equina syndrome and steroids should be started after MRI*
- While **cauda equina syndrome** is the correct diagnosis, waiting for an **MRI** before initiating **corticosteroids** would be a critical delay.
- **Early administration of steroids** is vital in cases of suspected spinal cord compression to reduce inflammation and preserve neurological function, even before definitive imaging.
Red flags in neurological complaints US Medical PG Question 6: A 56-year-old woman presents with sudden-onset severe headache, nausea, vomiting, and neck pain for the past 90 minutes. She describes her headache as a ‘thunderclap’, followed quickly by severe neck pain and stiffness, nausea and vomiting. She denies any loss of consciousness, seizure, or similar symptoms in the past. Her past medical history is significant for an episode 6 months ago where she suddenly had trouble putting weight on her right leg, which resolved within hours. The patient denies any history of smoking, alcohol or recreational drug use. On physical examination, the patient has significant nuchal rigidity. Her muscle strength in the lower extremities is 4/5 on the right and 5/5 on the left. The remainder of the physical examination is unremarkable. A noncontrast CT scan of the head is normal. Which of the following is the next best step in the management of this patient?
- A. Diffusion-weighted magnetic resonance imaging of the brain
- B. IV tPA
- C. Placement of a ventriculoperitoneal (VP) shunt
- D. T1/T2 MRI of the head
- E. Lumbar puncture (Correct Answer)
Red flags in neurological complaints Explanation: ***Lumbar puncture***
- A **thunderclap headache**, nuchal rigidity, nausea, and vomiting despite a normal noncontrast CT scan, is highly suspicious for **subarachnoid hemorrhage (SAH)**. A lumbar puncture is the next diagnostic step to look for **xanthochromia** or **red blood cells** in the cerebrospinal fluid.
- The previous episode of transient leg weakness could indicate a prior **warning leak** from an **aneurysm**, increasing the suspicion for SAH.
*Diffusion-weighted magnetic resonance imaging of the brain*
- This imaging is primarily used to detect **acute ischemic stroke**, which presents differently.
- While helpful for ischemic events, it is **not the primary diagnostic test** for suspected SAH after a normal CT.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is a thrombolytic used in acute ischemic stroke, characterized by focal neurological deficits.
- It is **contraindicated** in SAH due to the significant risk of exacerbating intracranial bleeding.
*Placement of a ventriculoperitoneal (VP) shunt*
- A **VP shunt** is a surgical procedure to drain excess cerebrospinal fluid, typically used to treat **hydrocephalus**.
- This is a treatment for a complication (hydrocephalus) that may arise from SAH, but it is **not the initial diagnostic or management step** for an acute SAH.
*T1/T2 MRI of the head*
- While MRI can detect SAH, especially if performed with specific sequences (FLAIR), a **lumbar puncture is more sensitive for detecting SAH** when a CT scan is negative and clinical suspicion remains high.
- MRI is generally less accessible and more time-consuming than lumbar puncture in an emergency setting for suspected SAH.
Red flags in neurological complaints US Medical PG Question 7: A 78-year-old woman with a history of cerebrovascular accident (CVA) presents to the emergency department with slurred speech, diplopia and dizziness that has persisted for eight hours. Upon further questioning you find that since her CVA one year ago, she has struggled with depression and poor nutrition. Her dose of paroxetine has been recently increased. Additionally, she is on anti-seizure prophylaxis due to sequelae from her CVA. CT scan reveals an old infarct with no acute pathology. Vital signs are within normal limits. On physical exam you find the patient appears frail. She is confused and has nystagmus and an ataxic gait. What would be an appropriate next step?
- A. Lower the dose of her anti-seizure medication (Correct Answer)
- B. Start total parenteral nutrition (TPN)
- C. Administer tissue plasminogen activator (tPA)
- D. Start trimethoprim-sulfamethoxazole (TMP-SMX)
- E. Increase the dose of her anti-seizure medication
Red flags in neurological complaints Explanation: ***Lower the dose of her anti-seizure medication***
- The patient presents with classic symptoms of **anti-seizure medication toxicity**, including **slurred speech, diplopia, dizziness, nystagmus, and ataxia**, which are common with drugs like **phenytoin** or **carbamazepine**.
- Given her **frailty**, poor nutrition, and recent CVA, she is likely more susceptible to adverse drug effects, making a dose reduction the most appropriate next step to resolve the toxicity.
*Start total parenteral nutrition (TPN)*
- While the patient has **poor nutrition**, her acute symptoms are neurological and suggest a drug-related issue, not a primary nutritional emergency requiring TPN.
- TPN carries its own risks and is not indicated as an immediate treatment for drug toxicity or acute neurological symptoms in this context.
*Administer tissue plasminogen activator (tPA)*
- The patient's symptoms have been present for **eight hours**, exceeding the typical **time window for thrombolytic therapy** for acute ischemic stroke, which is generally 3 to 4.5 hours.
- The **CT scan shows an old infarct** with no acute pathology, ruling out an acute ischemic stroke that would warrant tPA.
*Start trimethoprim-sulfamethoxazole (TMP-SMX)*
- There is **no indication of an infection** in the provided clinical picture; her symptoms are neurological and consistent with medication toxicity.
- Administering an antibiotic without evidence of infection is inappropriate and could lead to unnecessary side effects.
*Increase the dose of her anti-seizure medication*
- The patient is exhibiting clear signs of **anti-seizure medication toxicity** (slurred speech, diplopia, dizziness, nystagmus, ataxia).
- Increasing the dose would exacerbate these symptoms and could lead to more severe adverse events, making it a dangerous and inappropriate action.
Red flags in neurological complaints US Medical PG Question 8: A 75-year-old woman presents with sudden loss of vision. She says that she was reading when suddenly she was not able to see the print on half of the page. Her symptoms started 4 hours ago and are accompanied by a severe posterior headache. Vital signs reveal the following: blood pressure 119/76 mm Hg, pulse 89/min, SpO2 98% on room air. The patient was unable to recognize her niece when she arrived to see her. A noncontrast CT of the head shows no evidence of hemorrhagic stroke. What is the most likely diagnosis in this patient?
- A. Lacunar stroke
- B. Middle cerebral artery stroke
- C. Vertebrobasilar stroke
- D. Subarachnoid hemorrhage
- E. Posterior cerebral artery stroke (Correct Answer)
Red flags in neurological complaints Explanation: ***Posterior cerebral artery stroke***
- The sudden severe posterior headache along with **unilateral vision loss** and **prosopagnosia** (inability to recognize familiar faces) are characteristic signs of a **posterior cerebral artery (PCA) stroke**.
- PCA occlusion often affects the **occipital lobe** (vision) and can extend to the **temporal lobe** (facial recognition).
*Lacunar stroke*
- This type of stroke results from the occlusion of small penetrating arteries and typically causes **pure motor** or **pure sensory deficits**, not complex visual or recognition problems.
- While headache can occur, the specific combination of symptoms points away from a lacunar infarct.
*Middle cerebral artery stroke*
- MCA stroke commonly presents with **contralateral hemiparesis**, **aphasia** (if dominant hemisphere), and **hemianopia** but usually not isolated unilateral vision loss or severe posterior headache with prosopagnosia.
- The symptoms are more consistent with involvement of the posterior circulation.
*Vertebrobasilar stroke*
- A vertebrobasilar stroke can cause **visual disturbances**, but it is typically associated with other **brainstem symptoms** like vertigo, ataxia, or cranial nerve deficits, which are not described here.
- The specific presentation of unilateral vision loss and prosopagnosia is less typical for a vertebrobasilar stroke affecting widespread brainstem structures.
*Subarachnoid hemorrhage*
- While a **sudden severe headache (thunderclap headache)** is a hallmark of SAH, it usually presents with meningeal irritation symptoms like **neck stiffness** and often altered mental status, and the visual deficits are usually different (e.g., oculomotor nerve palsy).
- The patient's focal neurological deficits, specifically prosopagnosia and unilateral visual field loss, are more indicative of an ischemic event in a specific vascular territory.
Red flags in neurological complaints US Medical PG Question 9: A previously healthy 40-year-old woman comes to the physician because of a 3-day history of fever, headaches, and fatigue. She also reports a persistent tingling sensation in her right hand and numbness in her right arm that started this morning. Physical examination shows pallor, mild scleral icterus, and petechiae on her forearms and legs. On mental status examination, she appears confused and is only oriented to person. Laboratory studies show:
Hemoglobin 11.1 g/dL
Platelet count 39,500/mm3
Bleeding time 9 minutes
Prothrombin time 14 seconds
Partial thromboplastin time 35 seconds
Serum
Creatinine 1.7 mg/dL
Total bilirubin 2.1 mg/dL
A peripheral blood smear shows fragmented erythrocytes. Which of the following is the most likely underlying cause of this patient's condition?
- A. Antibodies against double-stranded DNA
- B. Mutation of the PIGA gene
- C. Antibodies against GpIIb/IIIa
- D. Antibodies against ADAMTS13 (Correct Answer)
- E. Absence of platelet GpIIb/IIIa receptors
Red flags in neurological complaints Explanation: ***Antibodies against ADAMTS13***
- This patient presents with a classic pentad of symptoms: **fever**, **neurologic symptoms** (confusion, tingling, numbness), **renal failure** (creatinine 1.7 mg/dL), **thrombocytopenia** (platelet count 39,500/mm3), and **microangiopathic hemolytic anemia** (pallor, scleral icterus, fragmented erythrocytes on smear). This constellation of findings is highly suggestive of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is primarily caused by a deficiency of the **ADAMTS13 enzyme**, often due to **autoantibodies** that inhibit its activity. ADAMTS13 is responsible for cleaving large **von Willebrand factor (vWF) multimers**, and its deficiency leads to the accumulation of these large multimers, promoting platelet aggregation and microthrombi formation.
*Antibodies against double-stranded DNA*
- Antibodies against double-stranded DNA (**anti-dsDNA antibodies**) are characteristic of **Systemic Lupus Erythematosus (SLE)**, which can present with various systemic symptoms.
- While SLE can cause thrombocytopenia and renal involvement, it typically does not cause the severe **microangiopathic hemolytic anemia** with schistocytes or the combination of symptoms seen in this patient to the extent of TTP.
*Mutation of the PIGA gene*
- A **mutation of the *PIGA* gene** is responsible for **Paroxysmal Nocturnal Hemoglobinuria (PNH)**, a clonal stem cell disorder characterized by hemolytic anemia, thrombosis, and bone marrow failure.
- While PNH involves hemolysis, it typically lacks the prominent neurological symptoms, severe thrombocytopenia with microangiopathic features, and renal failure seen in TTP.
*Antibodies against GpIIb/IIIa*
- **Antibodies against GpIIb/IIIa** (glycoprotein IIb/IIIa) receptors are the hallmark of **Immune Thrombocytopenic Purpura (ITP)**, causing accelerated platelet destruction.
- ITP primarily causes **isolated thrombocytopenia** and mucocutaneous bleeding, but it does not cause microangiopathic hemolytic anemia, renal failure, or neurological symptoms that are prominent in this patient.
*Absence of platelet GpIIb/IIIa receptors*
- The **absence of platelet GpIIb/IIIa receptors** is characteristic of **Glanzmann's thrombasthenia**, a rare inherited disorder of platelet function.
- Glanzmann's thrombasthenia leads to **mucocutaneous bleeding** due to impaired platelet aggregation, but it does not cause thrombocytopenia, hemolytic anemia, renal failure, or neurological symptoms.
Red flags in neurological complaints US Medical PG Question 10: A 47-year-old man presents to the clinic for an evaluation of intense itching of his right thigh region for the past few days. He states some ‘red bumps’ just began to form. The patient mentions that he was recently at a business conference in Miami. He has a past medical history of hypertension, diabetes type 2, and hyperlipidemia. He takes enalapril, metformin, and atorvastatin. He does not smoke or drink. His vitals are within normal limits today. On physical examination, a linear line with 3 red papules is present along the medial aspect of his right thigh. Additionally, there are small rows of bumps on his left leg and right forearm. Excoriations are also apparent in the same region. Which of the following is the most likely diagnosis?
- A. Scabies
- B. Bed bug bite (Correct Answer)
- C. Cutaneous larva migrans
- D. Flea bite
- E. Spider bite
Red flags in neurological complaints Explanation: ***Bed bug bite***
- The presence of **linear lesions** (often described as "breakfast, lunch, and dinner") and **rows of bumps** on exposed skin, especially after recent travel, is highly characteristic of **bed bug bites**.
- **Intense itching** and **red papules** appearing a few days after exposure further support this diagnosis.
*Scabies*
- While scabies also causes intense itching and red papules, it typically presents with **serpiginous burrows** in characteristic locations such as the finger webs, wrists, and axillae.
- Scabies is also more often associated with generalized pruritus rather than localized linear lesions from recent exposure.
*Cutaneous larva migrans*
- This condition is caused by hookworm larvae and presents with a **highly pruritic, intensely erythematous, raised, serpiginous tract** that migrates over time.
- The described lesions are more consistent with bites in a linear pattern rather than a migratory burrow.
*Flea bite*
- Flea bites often appear as **small, red, itchy bumps** usually clustered around ankles or areas covered by tight clothing.
- While itchy, they typically do not form the distinct linear "breakfast, lunch, and dinner" pattern seen with bed bugs.
*Spider bite*
- Most spider bites present as a **single lesion**, often with a central puncture mark, and can range from mild local reactions to necrotic lesions, depending on the spider.
- Bites from multiple spiders or multiple bites in a linear pattern are highly unusual and do not fit the description of lesions in rows.
More Red flags in neurological complaints US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.