Red flags in musculoskeletal complaints US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Red flags in musculoskeletal complaints. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
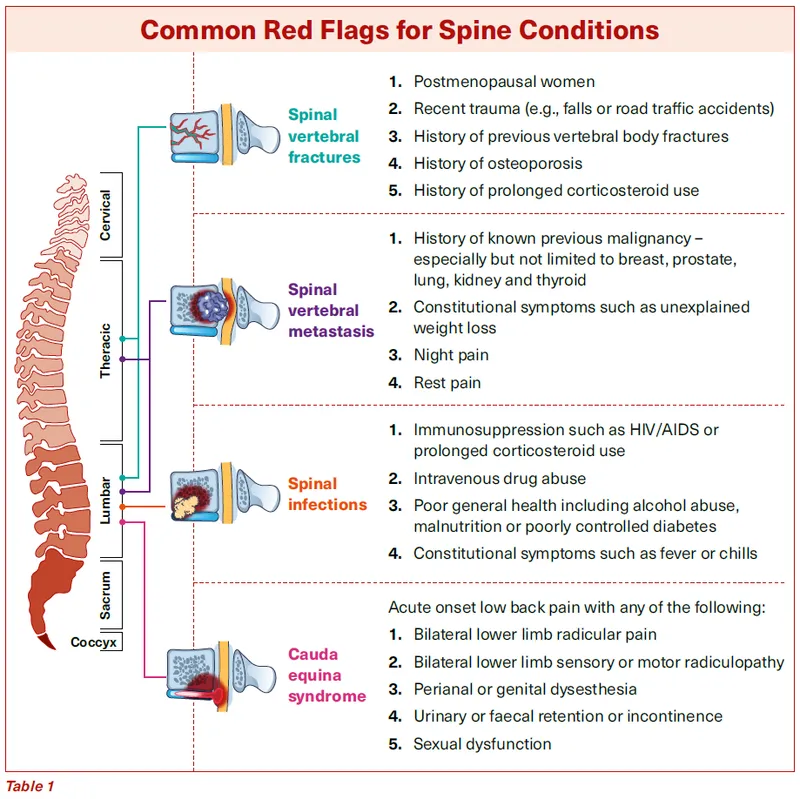
Red flags in musculoskeletal complaints US Medical PG Question 1: A 33-year-old man with a history of IV drug and alcohol abuse presents to the emergency department with back pain. He states that his symptoms started 3 days ago and have been gradually worsening. His temperature is 102°F (38.9°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for tenderness over the mid thoracic spine. Laboratory values are only notable for a leukocytosis and an elevated ESR and CRP. Which of the following is the most likely diagnosis?
- A. Degenerative spine disease
- B. Herniated nucleus pulposus
- C. Musculoskeletal strain
- D. Osteomyelitis (Correct Answer)
- E. Spinal epidural hematoma
Red flags in musculoskeletal complaints Explanation: ***Osteomyelitis***
- The patient's history of **IV drug abuse** is a major risk factor for **hematogenous osteomyelitis**, especially vertebral osteomyelitis.
- The presence of **fever**, **localized spinal tenderness**, **leukocytosis**, and elevated **ESR** and **CRP** are classic signs of infection.
*Degenerative spine disease*
- This condition typically presents with **chronic pain** and insidious onset, not acute fever and inflammatory markers.
- While it can cause back pain, it is not associated with systemic signs of infection or a rapid worsening course like in this case.
*Herniated nucleus pulposus*
- Primarily causes **radicular pain** and neurological deficits due to nerve compression, often without systemic symptoms.
- There are no signs of infection, fever, or elevated inflammatory markers associated with a simple herniated disc.
*Musculoskeletal strain*
- This would present with localized pain, but rarely with **fever**, **leukocytosis**, and markedly elevated inflammatory markers.
- It is typically a self-limiting condition with symptoms that would not progressively worsen over three days with systemic signs of infection.
*Spinal epidural hematoma*
- This is characterized by sudden, severe back pain and often rapid onset neurological deficits, particularly in patients on anticoagulants or with coagulopathies.
- It would not typically present with **fever** and elevated inflammatory markers suggestive of an infection.
Red flags in musculoskeletal complaints US Medical PG Question 2: A 36-year-old man is seen in the emergency department for back pain that has been getting progressively worse over the last 4 days. Upon further questioning, he also notes that he has been having a tingling and burning sensation rising up from his feet to his knees bilaterally. The patient states he is having difficulty urinating and having bowel movements over the last several days. His temperature is 97.4°F (36.3°C), blood pressure is 122/80 mmHg, pulse is 85/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for weak leg flexion bilaterally along with decreased anal sphincter tone. Which of the following is the best next step in management?
- A. Emergency surgery
- B. CT
- C. Pulmonary function tests
- D. Lumbar puncture
- E. MRI (Correct Answer)
Red flags in musculoskeletal complaints Explanation: ***MRI***
- The patient's symptoms (back pain, ascending paresthesias, bladder/bowel dysfunction, and decreased anal sphincter tone) are highly suggestive of **cauda equina syndrome**. An **MRI of the spine** is the gold standard for diagnosing this condition, as it can visualize the spinal cord and nerve roots directly.
- Early diagnosis and intervention with MRI are crucial to prevent **permanent neurological deficits** in cauda equina syndrome.
*Emergency surgery*
- While emergency surgery might be the next step *after* diagnosis, it is **not the initial diagnostic step**. The cause of the cauda equina syndrome (e.g., disc herniation, tumor) must first be identified.
- Performing surgery without proper imaging could lead to operating on the wrong level or for the wrong pathology.
*CT*
- A **CT scan** can provide information about bony structures but is generally **inferior to MRI** for visualizing soft tissue structures like the spinal cord, nerve roots, and intervertebral discs, which are critical in cauda equina syndrome.
- It may miss subtle compressions or pathologies of the nerve roots.
*Pulmonary function tests*
- **Pulmonary function tests** are used to assess lung function and are **irrelevant** to the patient's acute neurological symptoms and back pain.
- This test would not provide any diagnostic information for suspected cauda equina syndrome.
*Lumbar puncture*
- A **lumbar puncture** is primarily used to analyze cerebrospinal fluid for conditions like infection or inflammation (e.g., meningitis, Guillain-Barré syndrome).
- While Guillain-Barré can cause ascending paralysis, the prominent back pain, bowel/bladder dysfunction, and decreased anal sphincter tone make **cauda equina syndrome** a more likely diagnosis, for which LP is not the primary diagnostic tool.
Red flags in musculoskeletal complaints US Medical PG Question 3: A 61-year-old man presents to the emergency room with a painful, swollen left leg. He states that his symptoms began that morning after a long flight from Australia. He denies shortness of breath, chest pain, or cough. On review of systems, he notes that he has been constipated recently and had several episodes of bright red blood per rectum. He has not noticed any weight loss, fevers, or night sweats. He has a past medical history of a deep vein thrombosis 4 years ago during a hospitalization for community acquired pneumonia and was treated with warfarin for 3 months afterward. He also has chronic hepatitis C from previous intravenous drug use. The patient has a 30 pack-year smoking history and has never had a colonoscopy. His father is 84-years-old and has chronic kidney disease from diabetes, and his mother passed away from a massive pulmonary embolus when pregnant with his younger sister. In the emergency room, his temperature is 98.7°F (37.1°C), blood pressure is 142/85 mm/Hg, pulse is 79/min, and respirations are 14/min. On exam, he is in no acute distress. His left calf is larger in caliber than the right calf which is red and tender to palpation. Dorsiflexion of the foot worsens the pain. His abdomen is soft, nontender, and nondistended without hepatomegaly. The remainder of the physical exam is unremarkable. Labs are shown below:
Hemoglobin: 13.0 g/dL
Leukocyte count: 6,000/mm^3
Platelets: 160,000/mm^3
Aspartate aminotransferase: 15 U/L
Alanine aminotransferase: 19 U/L
Alkaline phosphatase: 81 IU/L
Hepatitis C antibody: reactive
Hepatitis C titer: 0 copies/mL
Which of the following is the most likely cause of this patient’s condition?
- A. Increased estrogen levels
- B. Loss of antithrombin III in urine
- C. Protein C deficiency
- D. Resistance of factor V to inactivation by protein C (Correct Answer)
- E. Malignancy
Red flags in musculoskeletal complaints Explanation: ***Resistance of factor V to inactivation by protein C***
- This patient has **Factor V Leiden mutation**, the most common inherited thrombophilia (present in 5% of Caucasians)
- **Key diagnostic clues**: Recurrent DVT (even if provoked events have lower thresholds in Factor V Leiden) and **strong family history** - mother with massive PE during pregnancy is highly suggestive, as pregnancy unmasks inherited thrombophilias
- Factor V Leiden causes **resistance to activated protein C**, leading to prolonged clotting and increased VTE risk
- While the rectal bleeding raises concern for malignancy, the **family history of thromboembolism** points to an inherited predisposition as the underlying cause
*Malignancy*
- Malignancy causes hypercoagulability through multiple mechanisms (tissue factor release, inflammatory cytokines, platelet activation)
- The patient's **rectal bleeding, constipation, age 61, and lack of screening colonoscopy** are concerning for colorectal cancer
- Malignancy is a strong consideration and warrants urgent colonoscopy
- However, the **family history of massive PE in mother during pregnancy** more strongly suggests an inherited thrombophilia as the primary cause, though malignancy could be a coexisting/triggering factor
*Increased estrogen levels*
- Estrogen increases synthesis of clotting factors and decreases anticoagulant proteins, raising DVT risk
- Seen with oral contraceptives, hormone replacement therapy, or pregnancy
- This patient is a **61-year-old male**, making estrogen-related thrombosis extremely unlikely
*Loss of antithrombin III in urine*
- Occurs in **nephrotic syndrome** (proteinuria >3.5 g/day, hypoalbuminemia, edema, hyperlipidemia)
- Loss of antithrombin III causes hypercoagulability
- This patient has **no proteinuria, normal liver enzymes, no edema**, and no other features of nephrotic syndrome
*Protein C deficiency*
- Hereditary protein C deficiency is a rare thrombophilia causing recurrent VTE
- While possible, **Factor V Leiden is 10-20 times more common** than protein C deficiency
- The family history pattern (mother with PE in pregnancy) is more characteristic of Factor V Leiden
Red flags in musculoskeletal complaints US Medical PG Question 4: A 75-year-old man comes to the physician because of a 2-week history of sharp, stabbing pain in the lower back that radiates to the back of his left leg. He also has had a loss of sensitivity around his buttocks and inner thighs as well as increased trouble urinating the last week. Two years ago, he was diagnosed with prostate cancer and was treated with radiation therapy. Neurologic examination shows reduced strength and reflexes in the left lower extremity; the right side is normal. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Central cord syndrome
- B. Conus medullaris syndrome
- C. Anterior spinal cord syndrome
- D. Brown-sequard syndrome
- E. Cauda equina syndrome (Correct Answer)
Red flags in musculoskeletal complaints Explanation: ***Cauda equina syndrome***
- The patient presents with **bilateral sensory loss in the perineal region** (**saddle anesthesia**) and **new-onset urinary dysfunction** (trouble urinating, reduced squeeze tone), which are classic symptoms of cauda equina syndrome.
- The **sharp, stabbing radicular pain** radiating down the leg indicates nerve root involvement, characteristic of cauda equina rather than conus medullaris.
- The **asymmetric motor weakness** (left leg only) supports cauda equina syndrome, as compression can preferentially affect specific nerve roots, whereas conus medullaris typically causes more symmetric bilateral deficits.
- The history of **prostate cancer** and **radiation therapy** suggests a potential metastatic lesion compressing the cauda equina nerves.
*Central cord syndrome*
- This syndrome primarily affects the **upper extremities more than the lower extremities** and typically results from hyperextension injuries in older individuals.
- It often presents with **dissociated sensory loss** (loss of pain and temperature sensation) below the level of the lesion, which is not the primary complaint here.
*Conus medullaris syndrome*
- Affects the **sacral spinal cord segments (S3-S5)**, leading to **symmetrical motor and sensory deficits**, often with prominent early **bowel and bladder dysfunction**.
- While it causes saddle anesthesia and urinary symptoms, the **asymmetrical motor weakness** (left leg only) and **prominent radicular pain** extending down the leg are more characteristic of cauda equina syndrome.
- Conus lesions typically present with more **symmetric bilateral deficits** rather than the unilateral pattern seen here.
*Anterior spinal cord syndrome*
- Characterized by **bilateral motor paralysis** and **loss of pain and temperature sensation** below the lesion, with **preservation of proprioception and vibratory sensation**.
- It would not typically present with the isolated **saddle anesthesia** and **radicular pain** described in the patient.
*Brown-sequard syndrome*
- Results from a **hemicord lesion**, causing **ipsilateral motor paralysis** and loss of proprioception/vibration below the lesion, and **contralateral loss of pain and temperature sensation**.
- The patient's symptoms of **bilateral saddle anesthesia** and **bowel/bladder dysfunction** do not align with the characteristic unilateral sensory and motor presentation of Brown-Sequard syndrome.
Red flags in musculoskeletal complaints US Medical PG Question 5: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
Red flags in musculoskeletal complaints Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
Red flags in musculoskeletal complaints US Medical PG Question 6: A 33-year-old man presents to the emergency department with back pain. He is currently intoxicated but states that he is having severe back pain and is requesting morphine and lorazepam. The patient has a past medical history of alcohol abuse, drug seeking behavior, and IV drug abuse and does not routinely see a physician. His temperature is 102°F (38.9°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for tenderness over the thoracic and lumbar spine. The pain is exacerbated with flexion of the spine. The patient’s laboratory values are notable for the findings below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 16,500/mm^3 with normal differential
Platelet count: 197,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.2 mg/dL
CRP: 5.2 mg/L
Further imaging is currently pending. Which of the following is the most likely diagnosis?
- A. Musculoskeletal strain
- B. Spinal epidural abscess (Correct Answer)
- C. Spinal epidural hematoma
- D. Malingering
- E. Herniated nucleus pulposus
Red flags in musculoskeletal complaints Explanation: ***Spinal epidural abscess***
- The patient's history of **IV drug abuse**, **fever (102°F)**, **tachycardia**, and **elevated CRP and WBC count** are highly suggestive of an infection like a spinal epidural abscess.
- **Back pain exacerbated by spinal flexion** is a common symptom, and while the patient's drug-seeking behavior might initially mask clinical suspicion, the objective signs of infection warrant immediate further investigation.
*Musculoskeletal strain*
- This typically presents with localized back pain, but it would not explain the **fever**, **tachycardia**, **elevated WBC count**, or **elevated CRP**.
- A musculoskeletal strain is not associated with the systemic inflammatory response seen in this patient.
*Spinal epidural hematoma*
- While it can cause severe back pain, a spinal epidural hematoma is usually associated with **trauma**, **anticoagulant use**, or underlying **coagulopathy**, none of which are explicitly mentioned or supported by the labs here.
- It would not typically present with **fever** or an **elevated WBC count**.
*Malingering*
- Although the patient has a history of **drug-seeking behavior**, the presence of objective signs like **fever**, **tachycardia**, and **inflammatory markers (elevated CRP and WBC count)** strongly contradict a diagnosis of malingering.
- It would be dangerous and inappropriate to dismiss these physical findings as purely behavioral.
*Herniated nucleus pulposus*
- This condition causes back pain, often with **radicular symptoms**, but it is not associated with **fever**, **tachycardia**, or systemic inflammatory markers.
- While it can cause pain exacerbated by flexion, the **infectious signs** point away from a simple herniation.
Red flags in musculoskeletal complaints US Medical PG Question 7: A 69-year-old male presents to the emergency room with back pain. He has a history of personality disorder and metastatic prostate cancer and was not a candidate for surgical resection. He began chemotherapy but discontinued due to unremitting nausea. He denies any bowel or bladder incontinence. He has never had pain like this before and is demanding morphine. The nurse administers IV morphine and he feels more comfortable. Vital signs are stable. On physical examination you note tenderness to palpation along the lower spine, weakness in the bilateral lower extremities, left greater than right. Neurological examination is also notable for hyporeflexia in the knee and ankle jerks bilaterally. You conduct a rectal examination, which reveals saddle anesthesia. Regarding this patient, what is the most likely diagnosis and the appropriate next step in management?
- A. The most likely diagnosis is cauda equina syndrome and the patient should be rushed to radiation
- B. The most likely diagnosis is conus medullaris syndrome and steroids should be started prior to MRI
- C. The most likely diagnosis is cauda equina syndrome and steroids should be started prior to MRI (Correct Answer)
- D. The most likely diagnosis is conus medullaris syndrome and steroids should be started after MRI
- E. The most likely diagnosis is cauda equina syndrome and steroids should be started after MRI
Red flags in musculoskeletal complaints Explanation: ***The most likely diagnosis is cauda equina syndrome and steroids should be started prior to MRI***
- The patient's presentation with **back pain**, **bilateral lower extremity weakness** (left > right), **hyporeflexia**, and **saddle anesthesia** are classic signs of **cauda equina syndrome**. This is often caused by compression of the nerve roots below the spinal cord, commonly from metastasis in patients with a history of prostate cancer.
- Given the suspected **spinal cord compression** due to metastatic disease, initiating **high-dose corticosteroids** (like dexamethasone) before imaging is crucial to reduce edema around the spinal cord and preserve neurological function. An **urgent MRI** is the next step to confirm the diagnosis and localize the compression.
*The most likely diagnosis is cauda equina syndrome and the patient should be rushed to radiation*
- While **cauda equina syndrome** is the correct diagnosis, **radiation** is typically a definitive treatment modality for metastatic compression, not an immediate next step before confirming the extent and location of compression with imaging.
- **Corticosteroids** are the immediate priority to reduce swelling and improve neurological outcomes while awaiting definitive imaging and treatment planning.
*The most likely diagnosis is conus medullaris syndrome and steroids should be started prior to MRI*
- **Conus medullaris syndrome** typically presents with more symmetrical symptoms, often including early-onset **bladder and bowel dysfunction** and **hyperreflexia** (or mixed reflexes), which are not fully consistent with this patient's presentation of hyporeflexia and lack of incontinence.
- Although steroids would be appropriate for suspected compression before MRI for either syndrome, the specific symptom profile strongly favors cauda equina over conus.
*The most likely diagnosis is conus medullaris syndrome and steroids should be started after MRI*
- The patient's symptoms (weakness, hyporeflexia, saddle anesthesia) are more indicative of **cauda equina syndrome** rather than **conus medullaris syndrome** (which often involves hyperreflexia and earlier bowel/bladder dysfunction).
- Delaying **corticosteroids** until after the MRI in suspected spinal cord compression can lead to irreversible neurological damage, as they help reduce edema immediately.
*The most likely diagnosis is cauda equina syndrome and steroids should be started after MRI*
- While **cauda equina syndrome** is the correct diagnosis, waiting for an **MRI** before initiating **corticosteroids** would be a critical delay.
- **Early administration of steroids** is vital in cases of suspected spinal cord compression to reduce inflammation and preserve neurological function, even before definitive imaging.
Red flags in musculoskeletal complaints US Medical PG Question 8: A 65-year-old woman comes to the physician for the evaluation of sharp, stabbing pain in the lower back for 3 weeks. The pain radiates to the back of her right leg and is worse at night. She reports decreased sensation around her buttocks and inner thighs. During the last several days, she has had trouble urinating. Three years ago, she was diagnosed with breast cancer and was treated with lumpectomy and radiation. Her only medication is anastrozole. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 12/min, and blood pressure is 130/70 mm Hg. Neurologic examination shows 4/5 strength in the left lower extremity and 2/5 strength in her right lower extremity. Knee and ankle reflexes are 1+ on the right. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Anterior spinal cord syndrome
- B. Cauda equina syndrome (Correct Answer)
- C. Conus medullaris syndrome
- D. Central cord syndrome
- E. Brown-sequard syndrome
Red flags in musculoskeletal complaints Explanation: ***Cauda equina syndrome***
- The patient's presentation with **severe low back pain**, **saddle anesthesia** (decreased sensation around buttocks and inner thighs), **bladder dysfunction** (trouble urinating), and **motor weakness** in the lower extremities is highly indicative of cauda equina syndrome. This can be caused by **spinal metastases** from her breast cancer.
- The **reduced squeeze tone** of the anal sphincter, despite normal resting tone, further supports the diagnosis, indicating dysfunction of the sacral nerve roots which are compressed in cauda equina syndrome.
*Anterior spinal cord syndrome*
- This syndrome typically presents with **motor paralysis**, loss of **pain** and **temperature** sensation below the lesion, but preservation of **proprioception** and **vibration sense**.
- It does not typically cause **saddle anesthesia** or **bladder dysfunction** to the extent seen in this patient.
*Conus medullaris syndrome*
- Conus medullaris syndrome involves the lower part of the spinal cord (T12-L2) and typically presents with **symmetric motor weakness**, **early onset bladder and bowel dysfunction**, and often **perianal numbness**.
- While there is bladder dysfunction, the described **asymmetric weakness** and prominent **radicular pain** radiating down one leg are more characteristic of cauda equina syndrome, which affects nerve roots rather than the spinal cord itself.
*Central cord syndrome*
- This syndrome usually results from hyperextension injuries and leads to **greater motor impairment in the upper extremities** than in the lower extremities.
- It is often associated with a **'shawl-like' distribution** of sensory loss and does not typically present with the same severe lower extremity weakness, saddle anesthesia, or bladder dysfunction as seen in this patient.
*Brown-Sequard syndrome*
- This syndrome is characterized by **hemisection of the spinal cord**, resulting in **ipsilateral motor paralysis** and loss of **proprioception and vibration sensation** below the level of the lesion.
- It also causes **contralateral loss of pain and temperature sensation** starting a few segments below the lesion, which does not match the patient's symptoms of bilateral sensory and motor deficits with saddle anesthesia.
Red flags in musculoskeletal complaints US Medical PG Question 9: A 33-year-old man presents to his primary care physician for left-sided knee pain. The patient has a history of osteoarthritis but states that he has been unable to control his pain with escalating doses of ibuprofen and naproxen. His past medical history includes diabetes mellitus and hypertension. His temperature is 102.0°F (38.9°C), blood pressure is 167/108 mmHg, pulse is 100/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals a warm and tender joint that is very tender to the touch and with passive range of motion. The patient declines a gait examination secondary to pain. Which of the following is the best next step in management?
- A. Colchicine
- B. Antibiotics
- C. Arthrocentesis (Correct Answer)
- D. IV steroids
- E. Rest, elevation, and ice
Red flags in musculoskeletal complaints Explanation: ***Arthrocentesis***
- The patient presents with unilateral, **acutely painful**, **warm**, and **tender joint** along with **fever**, suggesting a possible **septic joint**.
- **Arthrocentesis** is the definitive diagnostic procedure to rule out **septic arthritis** by analyzing synovial fluid for cell count, culture, and crystal analysis.
*Colchicine*
- Colchicine is used to treat **gout flares**; however, a definitive diagnosis of gout requires **synovial fluid analysis** for crystals, and **septic arthritis** must be ruled out first.
- The patient's presentation with **fever** and **unilateral warmth/tenderness** makes **septic arthritis** a critical concern that takes precedence over presumptive gout treatment.
*Antibiotics*
- While **septic arthritis** is highly suspected, initiating antibiotics without **synovial fluid culture** is premature and can compromise diagnostic accuracy.
- **Arthrocentesis** is necessary to identify the causative organism and guide appropriate **antibiotic therapy**.
*IV steroids*
- **Systemic steroids** could potentially worsen an underlying **septic infection** by suppressing the immune response.
- They are used in inflammatory arthropathies, but **septic arthritis** must be excluded before considering such treatment.
*Rest, elevation, and ice*
- These are supportive measures for joint pain but do not address the underlying cause of the patient's acute, febrile joint pain, especially the potential for **septic arthritis**.
- Delaying proper diagnosis and treatment of a **septic joint** can lead to significant morbidity including **joint destruction** and **sepsis**.
Red flags in musculoskeletal complaints US Medical PG Question 10: A 35-year-old male presents to his primary care physician with pain along the bottom of his foot. The patient is a long-time runner but states that the pain has been getting worse recently. He states that when running and at rest he has a burning and aching pain along the bottom of his foot that sometimes turns to numbness. Taking time off from training does not improve his symptoms. The patient has a past medical history of surgical repair of his Achilles tendon, ACL, and medial meniscus. He is currently not taking any medications. The patient lives with his wife and they both practice a vegan lifestyle. On physical exam the patient states that he is currently not experiencing any pain in his foot but rather is experiencing numbness/tingling along the plantar surface of his foot. Strength is 5/5 and reflexes are 2+ in the lower extremities. Which of the following is the most likely diagnosis?
- A. Vitamin B12 deficiency
- B. Common fibular nerve compression
- C. Tarsal tunnel syndrome (Correct Answer)
- D. Plantar fasciitis
- E. Herniated disc
Red flags in musculoskeletal complaints Explanation: ***Tarsal tunnel syndrome***
- The patient presents with **burning/aching pain** and **numbness/tingling along the plantar surface of the foot**, symptoms highly indicative of **tarsal tunnel syndrome**, which involves compression of the **posterior tibial nerve**.
- His history of being a **long-time runner** and pain that doesn't improve with rest points to an overuse injury or nerve entrapment, fitting with tarsal tunnel syndrome.
*Vitamin B12 deficiency*
- While a vegan lifestyle can predispose to **vitamin B12 deficiency**, which causes neuropathy, the symptoms of **burning pain** and **numbness localized to the plantar foot** are more specific to nerve entrapment.
- Neuropathy due to B12 deficiency typically presents as a more generalized **stocking-glove distribution**, rather than being confined to the sole of the foot.
*Common fibular nerve compression*
- Compression of the **common fibular nerve** (also known as the common peroneal nerve) typically affects the **dorsum of the foot** and the lateral aspect of the lower leg, leading to **foot drop** or weakness in dorsiflexion, which is not described.
- The patient's symptoms are specifically on the **plantar surface**, inconsistent with common fibular nerve compression.
*Plantar fasciitis*
- **Plantar fasciitis** is characterized by **heel pain** that is typically worse with the **first steps in the morning** or after periods of rest, which improves with activity.
- While it causes foot pain in runners, the prominent **numbness and tingling** described by the patient are not typical symptoms of plantar fasciitis.
*Herniated disc*
- A **herniated disc** causing radiating pain (sciatica) would involve symptoms that typically originate in the **lower back** or buttock and radiate down the leg.
- While it can cause numbness, the **localization to the plantar foot** without accompanying back pain or proximal leg symptoms makes a herniated disc less likely.
More Red flags in musculoskeletal complaints US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.