Red flags in headache US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Red flags in headache. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Red flags in headache US Medical PG Question 1: A 31-year-old woman presents to the emergency department with a history of fever and vomiting for 2 days and severe headache for a day. Past medical history is significant for migraine diagnosed 10 years ago, but she reports that her current headache is different. She describes the pain as generalized, dull, continuous, severe in intensity, and exacerbated by head movements. Physical examination reveals a blood pressure of 110/76 mm Hg and a temperature of 39.1°C (102.4°F). The patient is awake but in great distress due to pain. A pink-purple petechial rash covers her chest and legs. Extraocular movements are normal. She complains of neck pain and asks you to turn off the lights. Muscle strength is normal in all 4 limbs. Fundoscopic examination is normal. Baseline laboratory investigations are shown:
Laboratory test
Sodium 145 mEq/L
Potassium 3.2 mEq/L
Glucose 87 mg/dL
Creatinine 1.0 mg/dL
White blood cell count 18,900/mm3
Hemoglobin 13.4 g/dL
Platelets 165,000/mm3
INR 1.1
Aerobic and anaerobic blood cultures are taken and empiric antibiotics are started. A lumbar puncture is performed. Which of the following cerebrospinal fluid (CSF) findings are expected in this patient?
- A. CSF: WBC 640 cells/mm3, lymphocytic predominant, protein 180 mg/dL, glucose 24 mg/dL
- B. CSF: WBC 8,500 cells/mm3, neutrophil predominant, protein 112 mg/dL, glucose 15 mg/dL (Correct Answer)
- C. CSF: WBC 145 cells/mm3, lymphocytic predominant, protein 42 mg/dL, glucose 60 mg/dL
- D. CSF: WBC 4 cells/mm3, protein 35 mg/dL, glucose 66 mg/dL
- E. CSF: WBC 2 cells/mm3, protein 142 mg/dL, glucose 70 mg/dL
Red flags in headache Explanation: ***CSF: WBC 8,500 cells/mm3, neutrophil predominant, protein 112 mg/dL, glucose 15 mg/dL***
- The clinical presentation with **fever, severe headache, neck pain (photophobia indicated by asking to turn off lights), and petechial rash** is highly suggestive of **bacterial meningitis**, specifically meningococcal meningitis given the rash.
- **Bacterial meningitis** characteristically shows a **markedly elevated CSF white blood cell count (WBC) with neutrophil predominance**, **elevated protein**, and **very low glucose** due to bacterial consumption.
*CSF: WBC 640 cells/mm3, lymphocytic predominant, protein 180 mg/dL, glucose 24 mg/dL*
- While this CSF profile shows elevated protein and low glucose, the **lymphocytic predominance** typically points towards **viral meningitis** or other chronic inflammatory conditions, not acute bacterial meningitis.
- The high WBC count is more typical of bacterial meningitis, but the cell type is inconsistent with the typical presentation of acute bacterial infection.
*CSF: WBC 145 cells/mm3, lymphocytic predominant, protein 42 mg/dL, glucose 60 mg/dL*
- This CSF profile suggests **viral meningitis**, characterized by a **moderately elevated WBC count with lymphocytic predominance**, relatively normal or mildly elevated protein, and normal glucose.
- The patient's severe presentation with high fever, rash, and marked leukocytosis is more consistent with a bacterial process.
*CSF: WBC 4 cells/mm3, protein 35 mg/dL, glucose 66 mg/dL*
- This CSF profile represents **normal findings**, with a very low WBC count, normal protein, and normal glucose.
- These findings would not explain the patient's severe symptoms, high fever, and suspected meningitis.
*CSF: WBC 2 cells/mm3, protein 142 mg/dL, glucose 70 mg/dL*
- This profile shows normal WBCs and glucose but **elevated protein**. This combination can be seen in conditions like **Guillain-Barré syndrome** (cytoalbuminologic dissociation) or certain tumors.
- It does not fit the acute infectious picture of meningitis with fever and systemic inflammation.
Red flags in headache US Medical PG Question 2: A 72-year-old woman comes to the emergency department 4 hours after the sudden onset of a diffuse, dull, throbbing headache. During this time, she also reports blurred vision, nausea, and one episode of vomiting. She has a history of hypertension and type 2 diabetes mellitus. Her medications include hydrochlorothiazide, lisinopril, atorvastatin, and metformin. She has smoked 1 pack of cigarettes daily for the past 30 years and drinks 1–2 glasses of wine per day. Her temperature is 36.6 °C (97.9 °F), pulse is 90/min, respirations are 14/min, and blood pressure is 185/110 mm Hg. Fundoscopic examination shows bilateral blurring of the optic disc margins. Physical and neurologic examinations show no other abnormalities. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Urinalysis shows 2+ protein but no WBCs or RBCs. Which of the following is the most likely diagnosis?
- A. Ischemic stroke
- B. Hypertensive emergency (Correct Answer)
- C. Transient ischemic attack
- D. Subarachnoid hemorrhage
- E. Idiopathic intracranial hypertension
Red flags in headache Explanation: ***Hypertensive emergency***
- The patient presents with **sudden onset of severe headache**, blurred vision, nausea, and vomiting, along with **markedly elevated blood pressure (185/110 mm Hg)** which are classic symptoms of hypertensive emergency.
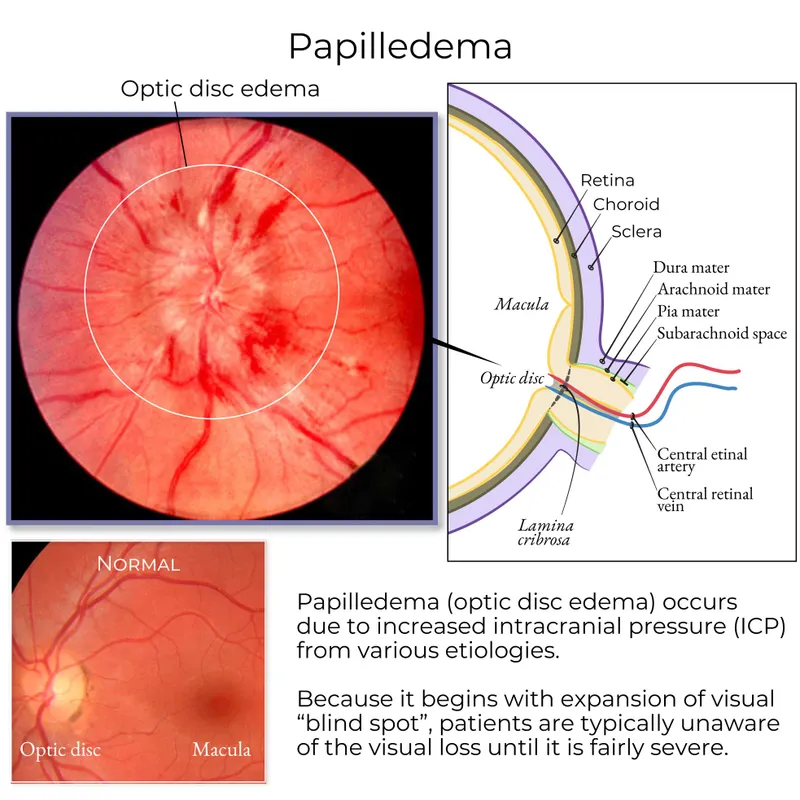
- **Bilateral blurring of the optic disc margins (papilledema)** indicates end-organ damage to the central nervous system due to severe hypertension, further supporting this diagnosis.
*Ischemic stroke*
- While a cerebral infarct can cause sudden-onset headache, it typically presents with **focal neurological deficits**, which are absent in this patient.
- The symptoms described are more consistent with generalized intracranial pressure elevation rather than a localized ischemic event.
*Transient ischemic attack*
- A TIA involves **transient neurological deficits** that resolve completely, typically within an hour, and would not usually be associated with persistent symptoms like blurred vision and papilledema.
- The significant and sustained elevation in blood pressure with end-organ damage points away from a TIA.
*Subarachnoid hemorrhage*
- Often causes a **"thunderclap" headache** described as the worst headache of one's life, which is more severe and abrupt than the "dull, throbbing" headache mentioned.
- While it can cause nausea and vomiting, the absence of meningeal signs or focal neurological deficits, and the presence of severe uncontrolled hypertension with papilledema, make subarachnoid hemorrhage less likely.
*Idiopathic intracranial hypertension*
- This condition typically affects young, obese women and is characterized by symptoms of **increased intracranial pressure (headache, vision changes, papilledema)**, but without an identifiable cause.
- The patient's age (72 years), history of uncontrolled hypertension, and very high blood pressure suggest a secondary cause for her intracranial hypertension, specifically a hypertensive emergency.
Red flags in headache US Medical PG Question 3: A 56-year-old woman presents with sudden-onset severe headache, nausea, vomiting, and neck pain for the past 90 minutes. She describes her headache as a ‘thunderclap’, followed quickly by severe neck pain and stiffness, nausea and vomiting. She denies any loss of consciousness, seizure, or similar symptoms in the past. Her past medical history is significant for an episode 6 months ago where she suddenly had trouble putting weight on her right leg, which resolved within hours. The patient denies any history of smoking, alcohol or recreational drug use. On physical examination, the patient has significant nuchal rigidity. Her muscle strength in the lower extremities is 4/5 on the right and 5/5 on the left. The remainder of the physical examination is unremarkable. A noncontrast CT scan of the head is normal. Which of the following is the next best step in the management of this patient?
- A. Diffusion-weighted magnetic resonance imaging of the brain
- B. IV tPA
- C. Placement of a ventriculoperitoneal (VP) shunt
- D. T1/T2 MRI of the head
- E. Lumbar puncture (Correct Answer)
Red flags in headache Explanation: ***Lumbar puncture***
- A **thunderclap headache**, nuchal rigidity, nausea, and vomiting despite a normal noncontrast CT scan, is highly suspicious for **subarachnoid hemorrhage (SAH)**. A lumbar puncture is the next diagnostic step to look for **xanthochromia** or **red blood cells** in the cerebrospinal fluid.
- The previous episode of transient leg weakness could indicate a prior **warning leak** from an **aneurysm**, increasing the suspicion for SAH.
*Diffusion-weighted magnetic resonance imaging of the brain*
- This imaging is primarily used to detect **acute ischemic stroke**, which presents differently.
- While helpful for ischemic events, it is **not the primary diagnostic test** for suspected SAH after a normal CT.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is a thrombolytic used in acute ischemic stroke, characterized by focal neurological deficits.
- It is **contraindicated** in SAH due to the significant risk of exacerbating intracranial bleeding.
*Placement of a ventriculoperitoneal (VP) shunt*
- A **VP shunt** is a surgical procedure to drain excess cerebrospinal fluid, typically used to treat **hydrocephalus**.
- This is a treatment for a complication (hydrocephalus) that may arise from SAH, but it is **not the initial diagnostic or management step** for an acute SAH.
*T1/T2 MRI of the head*
- While MRI can detect SAH, especially if performed with specific sequences (FLAIR), a **lumbar puncture is more sensitive for detecting SAH** when a CT scan is negative and clinical suspicion remains high.
- MRI is generally less accessible and more time-consuming than lumbar puncture in an emergency setting for suspected SAH.
Red flags in headache US Medical PG Question 4: A 62-year-old Caucasian male receiving treatment for stable angina experiences intermittent throbbing headaches. What is the most likely cause?
- A. Transient ischemic attack
- B. Beta adrenergic inactivation
- C. Acute hemorrhage
- D. Vasodilation of cerebral arteries (Correct Answer)
- E. Elevated creatine kinase
Red flags in headache Explanation: ***Vasodilation of cerebral arteries***
- Many medications used to treat **stable angina**, such as **nitrates**, achieve their therapeutic effect through **vasodilation**.
- This vasodilation can extend to the **cerebral arteries**, leading to an increase in intracranial arterial pulsatility, which is often perceived as a **throbbing headache**.
*Transient ischemic attack*
- A TIA typically presents with **focal neurological deficits** (e.g., weakness, numbness, speech difficulties) that resolve within 24 hours, not primarily with isolated headaches.
- While headache can occur, it's not the hallmark symptom and usually accompanies other transient neurological symptoms.
*Beta adrenergic inactivation*
- **Beta-blockers**, while used for angina, typically do not cause throbbing headaches; in fact, they are sometimes used to prevent migraines.
- **Inactivation** or withdrawal of beta-blockers might cause rebound symptoms but regular use is not linked to this type of headache.
*Acute hemorrhage*
- An **acute hemorrhage**, especially in the brain, often causes a **sudden, severe "thunderclap" headache** accompanied by neurological deficits, altered mental status, or signs of meningeal irritation, which are not described here as intermittent or mild.
- The description of "intermittent throbbing headaches" does not fit the typical presentation of an acute intracranial hemorrhage.
*Elevated creatine kinase*
- **Elevated creatine kinase (CK)** indicates muscle damage and is not directly related to headaches.
- While some medications (e.g., statins) can cause myopathy and elevated CK, this is not a common cause of headaches, particularly throbbing ones.
Red flags in headache US Medical PG Question 5: A 28-year-old woman presents with a 12-month history of headache, tinnitus, retrobulbar pain, and photopsias. She says the headaches are mild to moderate, intermittent, diffusely localized, and refractory to nonsteroidal anti-inflammatory drugs (NSAIDs). In addition, this past week, she began to have associated dizziness and photopsia with the headaches. Physical examination reveals a body temperature of 36.5°C (97.7°F), blood pressure of 140/80 mm Hg, and a respiratory rate of 13/min and regular. BMI is 29 kg/m2. Neurological examination is significant for peripheral visual field loss in the inferior nasal quadrant, diplopia, bilateral abducens nerve palsy, and papilledema. A T1/T2 MRI of the brain did not identify extra-axial or intra-axial masses or interstitial edema, and a lumbar puncture showed an opening pressure of 27 cm H2O, with a cerebrospinal fluid analysis within the normal range. Which of the following best describes the pathogenic mechanism underlying these findings?
- A. Systemic hypertension
- B. Increased cerebrospinal fluid production
- C. Aqueductal stenosis
- D. Arachnoid granulation adhesions
- E. Elevated intracranial venous pressure (Correct Answer)
Red flags in headache Explanation: ***Elevated intracranial venous pressure***
- The combination of **papilledema**, **abducens nerve palsy**, normal brain MRI, and normal CSF analysis with **elevated opening pressure** (27 cm H2O; normal <20-25 cm H2O) is classic for **idiopathic intracranial hypertension (IIH)**, also known as pseudotumor cerebri.
- The primary pathogenic mechanism in IIH is often thought to be impaired **CSF absorption** due to elevated **intracranial venous pressure**, particularly within the dural venous sinuses, which can be exacerbated by obesity.
*Systemic hypertension*
- While the patient has slightly elevated blood pressure (140/80 mmHg), **systemic hypertension** rarely directly causes **papilledema** or **abducens nerve palsy** without other signs of hypertensive encephalopathy or end-organ damage, which are not described.
- The elevated intracranial pressure is not directly explained by simply high systemic blood pressure, especially with normal brain imaging.
*Increased cerebrospinal production*
- **Increased CSF production** is a very rare cause of intracranial hypertension, typically associated with choroid plexus tumors.
- The normal CSF analysis and absence of a mass on MRI make this an unlikely primary mechanism.
*Aqueductal stenosis*
- **Aqueductal stenosis** would lead to **obstructive hydrocephalus**, characterized by ventricular enlargement on MRI, which was not observed in this patient.
- While it causes elevated ICP, the normal ventricular size rules out this specific structural obstruction.
*Arachnoid granulation adhesions*
- **Arachnoid granulation adhesions** could theoretically impair CSF absorption, leading to elevated intracranial pressure.
- However, direct evidence of such adhesions is not typically observed on routine MRI, and the underlying cause often relates to a more systemic issue affecting CSF outflow, such as the venous drainage problem described in the correct option.
Red flags in headache US Medical PG Question 6: A 47-year-old man presents to the clinic for an evaluation of intense itching of his right thigh region for the past few days. He states some ‘red bumps’ just began to form. The patient mentions that he was recently at a business conference in Miami. He has a past medical history of hypertension, diabetes type 2, and hyperlipidemia. He takes enalapril, metformin, and atorvastatin. He does not smoke or drink. His vitals are within normal limits today. On physical examination, a linear line with 3 red papules is present along the medial aspect of his right thigh. Additionally, there are small rows of bumps on his left leg and right forearm. Excoriations are also apparent in the same region. Which of the following is the most likely diagnosis?
- A. Scabies
- B. Bed bug bite (Correct Answer)
- C. Cutaneous larva migrans
- D. Flea bite
- E. Spider bite
Red flags in headache Explanation: ***Bed bug bite***
- The presence of **linear lesions** (often described as "breakfast, lunch, and dinner") and **rows of bumps** on exposed skin, especially after recent travel, is highly characteristic of **bed bug bites**.
- **Intense itching** and **red papules** appearing a few days after exposure further support this diagnosis.
*Scabies*
- While scabies also causes intense itching and red papules, it typically presents with **serpiginous burrows** in characteristic locations such as the finger webs, wrists, and axillae.
- Scabies is also more often associated with generalized pruritus rather than localized linear lesions from recent exposure.
*Cutaneous larva migrans*
- This condition is caused by hookworm larvae and presents with a **highly pruritic, intensely erythematous, raised, serpiginous tract** that migrates over time.
- The described lesions are more consistent with bites in a linear pattern rather than a migratory burrow.
*Flea bite*
- Flea bites often appear as **small, red, itchy bumps** usually clustered around ankles or areas covered by tight clothing.
- While itchy, they typically do not form the distinct linear "breakfast, lunch, and dinner" pattern seen with bed bugs.
*Spider bite*
- Most spider bites present as a **single lesion**, often with a central puncture mark, and can range from mild local reactions to necrotic lesions, depending on the spider.
- Bites from multiple spiders or multiple bites in a linear pattern are highly unusual and do not fit the description of lesions in rows.
Red flags in headache US Medical PG Question 7: A 67-year-old man with type 2 diabetes mellitus and benign prostatic hyperplasia comes to the physician because of a 2-day history of sneezing and clear nasal discharge. He has had similar symptoms occasionally in the past. His current medications include metformin and tamsulosin. Examination of the nasal cavity shows red, swollen turbinates. Which of the following is the most appropriate pharmacotherapy for this patient's condition?
- A. Nizatidine
- B. Diphenhydramine
- C. Amoxicillin
- D. Theophylline
- E. Desloratadine (Correct Answer)
Red flags in headache Explanation: **Desloratadine**
* This patient presents with symptoms consistent with **allergic rhinitis** (sneezing, clear nasal discharge, red/swollen turbinates, recurrent episodes). Desloratadine is a **second-generation antihistamine** that effectively treats these symptoms with minimal sedative effects, making it suitable for an elderly patient.
* It is a **non-sedating** antihistamine, which is crucial for elderly patients due to their increased sensitivity to sedative effects and potential for falls or cognitive impairment with first-generation antihistamines.
*Nizatidine*
* **Nizatidine** is an **H2-receptor antagonist** primarily used to treat gastroesophageal reflux disease (GERD) and peptic ulcers, not allergic rhinitis.
* It specifically blocks histamine H2 receptors in the stomach to reduce acid secretion and would not alleviate nasal congestion or sneezing.
*Diphenhydramine*
* **Diphenhydramine** is a **first-generation antihistamine** that is commonly used for allergic symptoms. However, it causes significant **sedation and anticholinergic side effects** (e.g., urinary retention, dry mouth, blurred vision).
* Given the patient's age and **benign prostatic hyperplasia (BPH)**, diphenhydramine is contraindicated. Its **anticholinergic effects** can inhibit bladder detrusor muscle contraction, leading to **urinary retention**, which is particularly problematic in elderly men with BPH who already have obstructive urinary symptoms.
*Amoxicillin*
* **Amoxicillin** is an **antibiotic** used to treat bacterial infections. This patient's symptoms (clear nasal discharge, sneezing, similar past episodes) are characteristic of **allergic or viral rhinitis**, not a bacterial infection.
* Using antibiotics for non-bacterial conditions contributes to **antibiotic resistance** and provides no therapeutic benefit for allergic symptoms.
*Theophylline*
* **Theophylline** is a **bronchodilator** primarily used for chronic respiratory conditions like asthma and COPD. It is not indicated for the treatment of allergic rhinitis.
* It has a **narrow therapeutic index** and can cause significant side effects (e.g., nausea, arrhythmias, seizures), making it an inappropriate and potentially dangerous choice for allergic rhinitis.
Red flags in headache US Medical PG Question 8: A 31-year-old man and his wife were referred to a genetic counselor. They are concerned about the chance that their children are likely to inherit certain conditions that run in their families. The wife's father and grandfather are both healthy, but her grandfather cannot see the color red. The husband is unaware if any member of his family has the same condition. The geneticist provides some details about genetic diseases and inheritance patterns, then orders lab tests to analyze the gene mutations carried by both partners. Which of the following are the correct terms regarding the genotype and phenotype of males affected by the condition described?
- A. Homozygote; reduced or incomplete penetrance
- B. Heterozygotes; reduced or incomplete penetrance
- C. Hemizygous; reduced or incomplete penetrance
- D. Heterozygotes; full penetrance
- E. Hemizygous; full penetrance (Correct Answer)
Red flags in headache Explanation: ***Hemizygous; full penetrance***
- The condition described (**red color blindness**) is an **X-linked recessive** trait, meaning males have only one X chromosome and are thus **hemizygous** for genes on the X chromosome.
- **Full penetrance** in X-linked recessive traits means that if a male inherits the affected X chromosome, he will express the phenotype of the condition.
*Homozygote; reduced or incomplete penetrance*
- **Homozygous** refers to having two identical alleles for a particular gene, which is not applicable to an X-linked gene in males as they only have one X chromosome.
- **Reduced or incomplete penetrance** means that a person with the genotype may or may not express the phenotype, which is typically not the case for males with X-linked recessive color blindness.
*Heterozygotes; reduced or incomplete penetrance*
- **Heterozygous** means having two different alleles for a gene; this term is not applicable to males regarding X-linked genes.
- Males are **hemizygous** for X-linked genes, meaning they only have one allele, not two different ones.
*Hemizygous; reduced or incomplete penetrance*
- While males are indeed **hemizygous** for X-linked genes like color blindness, the penetrance for red-green color blindness in males is generally considered to be **full**, meaning if they carry the mutated gene, they will express the trait.
- **Reduced penetrance** would imply that some males with the genotype might not exhibit color blindness, which is rare for this condition.
*Heterozygotes; full penetrance*
- The term **heterozygous** applies to individuals with two different alleles for a gene, which is not the genetic state of males for X-linked genes.
- While penetrance is full, the term **heterozygotes** is incorrect for defining the male genotype in this context.
Red flags in headache US Medical PG Question 9: A 43-year-old woman was admitted to the hospital after a fall. When the emergency services arrived, she was unresponsive, did not open her eyes, but responded to painful stimuli. The witnesses say that she had convulsions lasting about 30 seconds when she lost consciousness after a traumatic event. On her way to the hospital, she regained consciousness. On admission, she complained of intense headaches and nausea. She opened her eyes spontaneously, was responsive but confused, and was able to follow motor commands. Her vital signs are as follows: blood pressure, 150/90 mm Hg; heart rate, 62/min; respiratory rate, 13/min; and temperature, 37.3℃ (99.1℉). There are no signs of a skull fracture. The pupils are round, equal, and poorly reactive to light. She is unable to fully abduct both eyes. Ophthalmoscopy does not show papillary edema or retinal hemorrhages. She has nuchal rigidity and a positive Kernig sign. An urgent head CT does not show any abnormalities. Which of the following is a proper investigation to perform in this patient?
- A. Lumbar puncture (Correct Answer)
- B. Angiography
- C. Sonography
- D. Brain MRI
- E. EEG
Red flags in headache Explanation: ***Lumbar puncture***
- The patient's symptoms, including **severe headache**, **nuchal rigidity**, **positive Kernig sign**, and **abnormal oculomotor findings** (poorly reactive pupils, inability to abduct eyes), despite a normal head CT, are highly suggestive of **subarachnoid hemorrhage**. A lumbar puncture is essential to look for **xanthochromia** (yellowish discoloration of CSF due to bilirubin from lysed red blood cells), which confirms the diagnosis, especially when CT is negative in the first 6-12 hours.
- The history of a "traumatic event" followed by convulsions and transient loss of consciousness, along with a "lucid interval" then renewed symptoms (headache, confusion), raises suspicion for head injury leading to hemorrhagic event. The **elevated BP and bradycardia** (Cushing's reflex components), though not fully developed, also suggest increased intracranial pressure, further warranting investigation for hemorrhage.
*Angiography*
- While angiography (CTA or conventional) is performed **after a subarachnoid hemorrhage is confirmed** to identify the source of bleeding (e.g., aneurysm), it is not the *initial* diagnostic test to *confirm* the hemorrhage itself when CT is negative.
- Doing an angiography before ruling out significant hemorrhage via LP (when CT is negative) is premature and could expose the patient to unnecessary risks without a confirmed diagnosis.
*Sonography*
- **Sonography** (ultrasound) has **no role** in the acute diagnosis of subarachnoid hemorrhage or other intracranial pathology in adults.
- It is used for imaging the brain in neonates through the open fontanelles but is ineffective through the adult skull.
*Brain MRI*
- While an **MRI is more sensitive than CT for detecting subarachnoid hemorrhage** (especially subacute hemorrhage or small bleeds missed by CT), it is generally **less readily available** in an emergency setting than CT and LP.
- In cases where CT is negative but clinical suspicion for SAH is high, **lumbar puncture is typically the next step** as it can detect early SAH via xanthochromia, which might not be immediately visible on MRI. MRI may be used later to identify causes or small bleeds not picked up by CT.
*EEG*
- An **EEG (electroencephalogram)** is used to **evaluate seizure activity** and other types of brain dysfunction related to electrical activity.
- While the patient had convulsions, the primary concern given her overall presentation (severe headache, meningeal signs, altered mental status, and cranial nerve palsies) is **subarachnoid hemorrhage**, not solely seizure. An EEG would not help diagnose the underlying cause of her acute neurological deterioration.
Red flags in headache US Medical PG Question 10: A 47-year-old male with a medical history significant for hypertension, recurrent urinary tract infections, mitral valve prolapse, and diverticulosis experiences a sudden, severe headache while watching television on his couch. He calls 911 and reports to paramedics that he feels as if "someone shot me in the back of my head." He is rushed to the emergency room. On exam, he shows no focal neurological deficits but has significant nuchal rigidity and photophobia. Of the options below, what is the most likely etiology of this man's headache?
- A. Temporal Arteritis
- B. Brain Tumor
- C. Carotid Dissection
- D. Migraine
- E. Subarachnoid Hemorrhage (Correct Answer)
Red flags in headache Explanation: ***Subarachnoid Hemorrhage***
- The sudden onset of a "thunderclap" headache, often described as the "worst headache of my life" or feeling like "someone shot me in the back of my head", is a classic presentation of **subarachnoid hemorrhage (SAH)**.
- **Nuchal rigidity** (neck stiffness) and **photophobia** are common signs of meningeal irritation due to blood in the subarachnoid space.
*Temporal Arteritis*
- Typically presents in older individuals (usually >50 years old) with headache, **scalp tenderness**, jaw claudication, and visual disturbances, often associated with elevated inflammatory markers.
- The sudden, extremely severe nature and the patient's age (47) make this less likely.
*Brain Tumor*
- Headache associated with a brain tumor usually has a more **gradual onset** and progressive worsening, often accompanied by **focal neurological deficits** or seizures.
- The acute, severe "thunderclap" nature described here is not typical for a brain tumor headache.
*Carotid Dissection*
- Carotid dissection can cause a sudden headache, often unilateral, and may be associated with **neck pain**, neurological deficits (e.g., Horner's syndrome, transient ischemic attacks, stroke symptoms), or cranial nerve palsies.
- While it can present with acute headache, the description of "worst headache of my life" and prominent nuchal rigidity without focal deficits points more strongly to SAH.
*Migraine*
- Migraines typically have a **prodrome** or a more gradual onset, often accompanied by aura, photophobia, phonophobia, and nausea; they are usually recurrent.
- While migraines can be severe, the description of a sudden, explosive headache with associated nuchal rigidity is more characteristic of a serious underlying vascular event like SAH.
More Red flags in headache US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.