Red flags in geriatric patients US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Red flags in geriatric patients. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Red flags in geriatric patients US Medical PG Question 1: An 82-year-old woman is brought to the emergency department after losing consciousness at her nursing home. She had been watching TV for several hours and while getting up to use the bathroom, she fell and was unconscious for several seconds. She felt dizzy shortly before the fall. She does not have a headache or any other pain. She has a history of hypertension, intermittent atrial fibrillation, and stable angina pectoris. Current medications include warfarin, aspirin, hydrochlorothiazide, and a nitroglycerin spray as needed. Her temperature is 36.7°C (98.1°F), pulse is 100/min and regular, and blood pressure is 102/56 mm Hg. Physical exam shows a dry tongue. A fold of skin that is pinched on the back of her hand unfolds after 2 seconds. Cardiopulmonary examination shows no abnormalities. Further evaluation of this patient is most likely to show which of the following findings?
- A. Elevated serum concentration of cardiac enzymes
- B. Elevated serum creatine kinase concentration
- C. Absent P waves on ECG
- D. Elevated blood urea nitrogen concentration (Correct Answer)
- E. Hypodense lesions on CT scan of the head
Red flags in geriatric patients Explanation: ***Elevated blood urea nitrogen concentration***
- The patient presents with symptoms of **dehydration**, including a dry tongue, decreased skin turgor (skin fold taking 2 seconds to unfold), and **orthostatic hypotension** (dizziness upon standing, low blood pressure).
- Dehydration leads to **prerenal acute kidney injury**, characterized by an elevated blood urea nitrogen (BUN) concentration, often with an elevated BUN:creatinine ratio.
*Elevated serum concentration of cardiac enzymes*
- While the patient has a history of angina, there are no classic symptoms of an acute coronary syndrome such as **chest pain**, radiation, or ECG changes that would suggest myocardial injury warranting elevated cardiac enzymes.
- The syncope is more consistent with a **hemodynamic cause** (dehydration/hypotension) rather than a primary cardiac event like an MI.
*Elevated serum creatine kinase concentration*
- This is a non-specific marker for muscle damage and would be elevated if the patient experienced significant muscle injury from the fall.
- However, there is no mention of **trauma** or prolonged immobilization that would lead to rhabdomyolysis or significant muscle breakdown.
*Absent P waves on ECG*
- The patient has a history of **intermittent atrial fibrillation**, but her pulse is currently 100/min and **regular**, which indicates her current rhythm is likely not atrial fibrillation.
- Absence of P waves would specifically indicate **atrial fibrillation** or another atrial arrhythmia, but her regular pulse suggests a more sinus or junctional rhythm.
*Hypodense lesions on CT scan of the head*
- A CT scan of the head would be indicated to rule out **intracranial hemorrhage** or other structural brain lesions, especially given the fall and syncope.
- However, there are no focal neurological deficits, severe headache, or other signs strongly suggestive of a new stroke or hemorrhage, and the primary cause of syncope appears to be orthostatic hypotension due to hypovolemia.
Red flags in geriatric patients US Medical PG Question 2: An 84-year-old man presents to the emergency department for a loss of consciousness. The patient states that he was using the bathroom when he lost consciousness and fell, hitting his head on the counter. The patient has a past medical history of diabetes, hypertension, obesity, factor V leiden, constipation, myocardial infarction, and vascular claudication. His current medications include lisinopril, atorvastatin, valproic acid, propranolol, insulin, metformin, and sodium docusate. The patient denies use of illicit substances. His temperature is 99.5°F (37.5°C), blood pressure is 167/98 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam reveals an elderly man sitting comfortably in his stretcher. Cardiac exam reveals a systolic murmur heard at the right upper sternal border that radiates to the carotids. Pulmonary exam reveals mild bibasilar crackles. Neurological exam reveals 5/5 strength in his upper and lower extremities with normal sensation. The patient's gait is mildly unstable. The patient is unable to give a urine sample in the emergency department and states that he almost fainted again when he tried to. Which of the following is the most likely diagnosis?
- A. Seizure
- B. Cardiac arrhythmia
- C. Postural hypotension
- D. Situational syncope (Correct Answer)
- E. Transient ischemic attack
Red flags in geriatric patients Explanation: ***Situational syncope***
- The patient's loss of consciousness while **straining during defecation** (using the bathroom) is highly suggestive of **situational syncope**, which is a type of **reflex syncope** triggered by specific actions.
- His complaint of almost fainting again when trying to provide a urine sample reinforces the diagnosis, as **micturition (urination) syncope** is another common form of situational syncope.
*Seizure*
- While a loss of consciousness occurred, the patient's presentation lacks typical features of a seizure such as a **postictal state**, tongue biting, or tonic-clonic movements.
- The trigger (straining) and the near-syncopal episode with micturition are inconsistent with a primary seizure disorder.
*Cardiac arrhythmia*
- Although the patient has a history of myocardial infarction and is on **propranolol** (a beta-blocker), there are no specific findings on physical exam or in the history to strongly suggest an arrhythmia as the cause of syncope.
- An arrhythmia-induced syncope typically doesn't have such a clear situational trigger like defecation or urination.
*Postural hypotension*
- Postural hypotension is characterized by a significant drop in blood pressure upon standing, leading to symptoms like dizziness or syncope.
- While the patient is on several medications that could contribute to hypotension (e.g., lisinopril, propranolol), the syncope was specifically associated with straining, not just standing up.
*Transient ischemic attack*
- A TIA involves **transient neurological deficits** such as weakness, sensory changes, or speech disturbances, which typically last minutes to hours.
- A transient loss of consciousness without focal neurological symptoms is not characteristic of a TIA.
Red flags in geriatric patients US Medical PG Question 3: A 66-year-old man is brought into the emergency department by his daughter for a change in behavior. Yesterday the patient seemed more confused than usual and was asking the same questions repetitively. His symptoms have not improved over the past 24 hours, thus the decision to bring him in today. Last year, the patient was almost completely independent but he then suffered a "series of falls," after which his ability to care for himself declined. After this episode he was no longer able to cook for himself or pay his bills but otherwise had been fine up until this episode. The patient has a past medical history of myocardial infarction, hypertension, depression, diabetes mellitus type II, constipation, diverticulitis, and peripheral neuropathy. His current medications include metformin, insulin, lisinopril, hydrochlorothiazide, sodium docusate, atorvastatin, metoprolol, fluoxetine, and gabapentin. On exam you note a confused man who is poorly kept. He has bruises over his legs and his gait seems unstable. He is alert to person and place, and answers some questions inappropriately. The patient's pulse is 90/minute and his blood pressure is 170/100 mmHg. Which of the following is the most likely diagnosis?
- A. Normal aging
- B. Lewy body dementia
- C. Vascular dementia (Correct Answer)
- D. Pseudodementia (depression-related cognitive impairment)
- E. Alzheimer's dementia
Red flags in geriatric patients Explanation: ***Vascular dementia***
- This diagnosis is strongly supported by the patient's **stepwise decline** in cognitive function following a "series of falls" (likely small strokes or transient ischemic attacks) and his extensive history of **vascular risk factors** including hypertension, diabetes, and previous myocardial infarction.
- The acute worsening of confusion over 24 hours, coupled with pre-existing impaired executive function (inability to cook or pay bills), is characteristic of **vascular dementia's fluctuating course** and presentation often linked to new cerebrovascular events.
*Incorrect: Normal aging*
- **Normal aging** involves a very gradual and mild decline in cognitive functions, primarily affecting processing speed and memory recall, without significant impairment in daily activities.
- This patient's rapid, stepwise decline and inability to perform instrumental activities of daily living (IADLs) such as cooking and managing finances go beyond what is considered normal cognitive changes with aging.
*Incorrect: Lewy body dementia*
- **Lewy body dementia** is characterized by prominent **fluctuations in attention and alertness**, recurrent visual hallucinations, and spontaneous parkinsonism, none of which are explicitly mentioned as primary features in this patient's presentation.
- While fluctuations in confusion are present, the history of a clear stepwise decline post-falls and significant vascular risk factors points away from Lewy body dementia as the most likely primary cause.
*Incorrect: Pseudodementia (depression-related cognitive impairment)*
- **Pseudodementia** refers to cognitive impairment that occurs in the context of **major depression**, where patients may exhibit poor concentration, memory difficulties, and psychomotor slowing that mimics dementia.
- While this patient is on fluoxetine for depression, the **stepwise decline** after clear vascular events (falls), multiple vascular risk factors, and impaired executive function point to a true neurodegenerative process rather than depression-induced cognitive changes, which typically improve with treatment of the underlying mood disorder.
*Incorrect: Alzheimer's dementia*
- **Alzheimer's dementia** typically presents with a **gradual and progressive decline** in memory, particularly episodic memory, followed by other cognitive domains over several years.
- The patient's history of a clear **stepwise decline** in function after acute events (falls) and the strong presence of **vascular risk factors** make vascular dementia a more fitting diagnosis than Alzheimer's, which is not typically associated with such a sudden, step-like progression.
Red flags in geriatric patients US Medical PG Question 4: A 70-year-old man with a history of Alzheimer dementia presents to the emergency department with a change in his behavior. The patient has been more confused recently and had a fever. Upon presentation, he is too confused to answer questions. His temperature is 103°F (39.4°C), blood pressure is 102/68 mmHg, pulse is 157/min, respirations are 22/min, and oxygen saturation is 99% on room air. The patient is given 3 liters of IV fluids and acetaminophen and his vitals improve. He is also less confused. The patient is asking where he is and becomes combative and strikes a nurse when he finds out he has to be admitted to the hospital. He is given diphenhydramine for sedation and put in soft restraints. His mental status subsequently worsens and he becomes much more aggressive, spitting at nurses and attempting to bite his restraints. He also complains of abdominal pain. A post void residual volume is notable for a urine volume of 750 mL. Which of the following is the etiology of this patient's recent mental status change?
- A. Diphenhydramine (Correct Answer)
- B. Lorazepam
- C. Haloperidol
- D. Acute infection
- E. Olanzapine
Red flags in geriatric patients Explanation: ***Diphenhydramine***
- This patient exhibited a **paradoxical reaction** (increased agitation and aggression) to diphenhydramine, which is an **anticholinergic** medication.
- Anticholinergic drugs can worsen confusion and agitation, especially in elderly patients or those with pre-existing **dementia**.
*Lorazepam*
- **Benzodiazepines** like lorazepam primarily work on **GABA receptors** to produce sedative and anxiolytic effects.
- While sometimes used for agitation, it typically causes sedation rather than increased aggression in the elderly; a paradoxical reaction is less common than with anticholinergics.
*Haloperidol*
- Haloperidol is a **first-generation antipsychotic** used to treat acute agitation and psychosis, primarily by blocking **dopamine D2 receptors**.
- Its typical effect would be to decrease agitation and aggression, not worsen mental status in this manner.
*Acute infection*
- The patient initially presented with signs of an acute infection (fever, increased confusion), which improved after initial treatment with IV fluids and acetaminophen, indicating the initial symptoms were likely due to infection.
- The subsequent worsening after diphenhydramine points to a new etiology for the mental status change, rather than a resurgence of the infection.
*Olanzapine*
- Olanzapine is a **second-generation antipsychotic** that blocks serotonin and dopamine receptors, often used for acute agitation.
- Like haloperidol, it would be expected to reduce agitation and aggression, not exacerbate it, and was not administered to the patient according to the vignette.
Red flags in geriatric patients US Medical PG Question 5: An 82-year-old woman comes to the physician because of difficulty sleeping and increasing fatigue. Over the past 3 months she has been waking up early and having trouble falling asleep at night. During this period, she has had a decreased appetite and a 3.2-kg (7-lb) weight loss. Since the death of her husband one year ago, she has been living with her son and his wife. She is worried and feels guilty because she does not want to impose on them. She has stopped going to meetings at the senior center because she does not enjoy them anymore and also because she feels uncomfortable asking her son to give her a ride, especially since her son has had a great deal of stress lately. She is 155 cm (5 ft 1 in) tall and weighs 51 kg (110 lb); BMI is 21 kg/m2. Vital signs are within normal limits. Physical examination shows no abnormalities. On mental status examination, she is tired and has a flattened affect. Cognition is intact. Which of the following is the most appropriate initial step in management?
- A. Begin mirtazapine therapy
- B. Begin cognitive-behavioral therapy
- C. Notify adult protective services
- D. Assess for suicidal ideation (Correct Answer)
- E. Recommend relocation to a nursing home
Red flags in geriatric patients Explanation: ***Assess for suicidal ideation***
- The patient exhibits several **risk factors for depression**, including **insomnia**, **early morning awakening**, **anorexia**, **weight loss**, and significant **anhedonia** (lack of enjoyment in activities).
- Given her age, recent loss of her husband, social withdrawal, feelings of guilt, and significant emotional distress, it is crucial to first assess for **suicidal ideation** before initiating other treatments.
- **Elderly patients with depression have elevated suicide risk**, especially with recent bereavement and social isolation. Safety assessment is the **mandatory first step** in managing any patient with major depressive symptoms.
*Begin mirtazapine therapy*
- While **mirtazapine** is an effective antidepressant that could address several of her symptoms (insomnia, poor appetite, depression), it should only be considered after a **thorough safety assessment**, particularly for suicide risk.
- Starting medication without assessing for immediate danger may overlook critical safety concerns.
*Begin cognitive-behavioral therapy*
- **Cognitive-behavioral therapy (CBT)** is an effective treatment for depression and could be beneficial for this patient.
- However, similar to medication, it is a subsequent treatment step. The immediate priority is to rule out **suicidal intent** given the severity of her depressive symptoms.
*Notify adult protective services*
- There is no direct evidence of **abuse or neglect** in the provided information that would warrant involving adult protective services.
- Her feelings of guilt and worry about burdening her family, while contributing to her depression, do not indicate that her son or daughter-in-law are harming her.
*Recommend relocation to a nursing home*
- While the patient is elderly and potentially depressed, there is no medical or social necessity presented that indicates she requires or would benefit from a **nursing home** at this stage.
- This step would be premature and does not address the immediate mental health concerns or potential safety issues.
Red flags in geriatric patients US Medical PG Question 6: A 70-year-old man presents with a complaint of progressive dyspnea on minimal exertion. The patient reports being quite active and able to climb 3 flights of stairs in his building 10 years ago, whereas now he feels extremely winded when climbing a single flight. At first, he attributed this to old age but has more recently begun noticing that he feels similarly short of breath when lying down. He denies any recent fevers, cough, chest pain, nausea, vomiting, or diarrhea. He denies any past medical history except for two hospitalizations over the past 10 years for "the shakes." Family history is negative for any heart conditions. Social history is significant for a 10 pack-year smoking history. He currently drinks "a few" drinks per night. On exam, his vitals are: BP 120/80, HR 85, RR 14, and SpO2 97%. He is a mildly obese man who appears his stated age. Physical exam is significant for a normal heart exam with a few crackles heard at the bases of both lungs. Abdominal exam is significant for an obese abdomen and a liver edge palpated 2-3 cm below the costal margin. He has 2+ edema present in both lower extremities. Lab results reveal a metabolic panel significant for a sodium of 130 mEq/L but otherwise normal. Complete blood count, liver function tests, and coagulation studies are normal as well. An EKG reveals signs of left ventricular enlargement with a first degree AV block. A cardiac catheterization report from 5 years ago reveals a moderately enlarged heart but patent coronary arteries. Which of the following is the most likely cause of this individual's symptoms?
- A. Nephrotic syndrome
- B. Diastolic heart failure
- C. Ischemic cardiomyopathy
- D. Toxic cardiomyopathy (Correct Answer)
- E. Liver failure
Red flags in geriatric patients Explanation: ***Toxic cardiomyopathy***
- The patient's history of heavy alcohol consumption ("a few drinks per night") and two past hospitalizations for "**the shakes**" (suggesting **alcohol withdrawal**) are strong indicators of **alcoholic cardiomyopathy**.
- **Alcoholic cardiomyopathy** causes progressive left ventricular enlargement and dysfunction, leading to symptoms like **dyspnea on exertion**, **orthopnea**, **peripheral edema**, and **hepatomegaly**, all of which are present.
*Diastolic heart failure*
- While dyspnea and orthopnea are present, the EKG showing **left ventricular enlargement** and the cardiac catheterization reporting a **moderately enlarged heart** suggest **systolic dysfunction** rather than isolated diastolic dysfunction.
- **Diastolic heart failure** typically presents with preserved ejection fraction and abnormalities in ventricular relaxation or filling, which are not explicitly described or directly implied as the primary issue here.
*Ischemic cardiomyopathy*
- The **cardiac catheterization from 5 years ago** reported **patent coronary arteries**, making **ischemic heart disease** an unlikely primary cause of the current cardiac enlargement and symptoms.
- Although smoking is a risk factor for ischemia, the absence of coronary artery disease on prior catherization and the prominent history of alcohol abuse point elsewhere.
*Nephrotic syndrome*
- Although the patient has **edema** and **hyponatremia**, there is no mention of **significant proteinuria** (a hallmark of nephrotic syndrome) or elevated creatinine, and renal function tests are otherwise normal.
- **Nephrotic syndrome** would not explain the **left ventricular enlargement**, **dyspnea**, or the marked history of alcohol abuse and its cardiotoxic effects.
*Liver failure*
- While the patient has **peripheral edema** and **hepatomegaly**, his **liver function tests are normal**, arguing against significant **cirrhosis or liver failure** as the primary cause of his symptoms.
- The primary symptoms of **dyspnea**, **orthopnea**, and **left ventricular enlargement** point more directly to a cardiac origin rather than liver failure.
Red flags in geriatric patients US Medical PG Question 7: An 83-year-old man is being seen in the hospital for confusion. The patient was admitted 4 days ago for pneumonia. He has been improving on ceftriaxone and azithromycin. Then 2 nights ago he had an episode of confusion. He was unsure where he was and attempted to leave. He was calmed down by nurses with redirection. He had a chest radiograph that was stable from admission, a normal EKG, and a normal urinalysis. This morning he was alert and oriented. Then this evening he became confused and agitated again. The patient has a history of benign prostatic hyperplasia, severe dementia, and osteoarthritis. He takes tamsulosin in addition to the newly started antibiotics. Upon physical examination, the patient is alert but orientated only to name. He tries to get up, falls back onto the bed, and grabs his right knee. He states, “I need to get to work. My boss is waiting, but my knee hurts.” He tries to walk again, threatens the nurse who stops him, and throws a plate at the wall. In addition to reorientation, which of the following is the next best step in management?
- A. Morphine
- B. Lorazepam
- C. Haloperidol (Correct Answer)
- D. Rivastigmine
- E. Physical restraints
Red flags in geriatric patients Explanation: ***Haloperidol***
- The patient exhibits **delirium** with acute agitation, threatening behavior, and violent actions (throwing objects), representing an **imminent safety risk** to himself and staff.
- After **non-pharmacological interventions** (reorientation) have failed, **low-dose haloperidol** is appropriate for managing **severe agitation** in delirium when there is risk of harm.
- While antipsychotics have an FDA black box warning for increased mortality in elderly patients with dementia and recent evidence questions their efficacy in delirium, they remain indicated for **acute agitation with safety concerns** as a short-term intervention.
- Haloperidol is preferred over atypical antipsychotics in acute hospital settings due to availability in parenteral forms and lower anticholinergic burden.
*Morphine*
- While the patient mentions knee pain (likely from osteoarthritis), his **primary issue** is acute agitation and delirium, not pain management.
- **Opioids** can worsen delirium and confusion in elderly patients through anticholinergic effects and sedation.
- Pain should be addressed, but not as the primary intervention for violent, agitated behavior.
*Lorazepam*
- **Benzodiazepines** are generally **contraindicated in delirium** as they worsen confusion, increase fall risk, and can cause paradoxical agitation in elderly patients.
- The **only exceptions** are delirium from alcohol or benzodiazepine withdrawal, or seizures—none of which apply to this patient.
- Lorazepam would likely exacerbate rather than improve this patient's mental status.
*Rivastigmine*
- **Rivastigmine** is an acetylcholinesterase inhibitor for chronic management of **dementia symptoms**, not acute delirium.
- It has **no role** in managing acute behavioral disturbances and takes weeks to show any effect.
- Studies have not shown benefit of cholinesterase inhibitors in preventing or treating delirium.
*Physical restraints*
- Physical restraints should be used only as a **last resort** when pharmacological and non-pharmacological interventions have failed and there is immediate, serious risk of harm.
- Restraints can **increase agitation**, cause injuries, lead to delirium worsening, and are associated with increased morbidity and mortality.
- They do not address the underlying cause and should be avoided when other options are available.
Red flags in geriatric patients US Medical PG Question 8: A 33-year-old woman comes to the physician because of vision impairment in her right eye for the past 2 weeks. During this period, she was unable to distinguish colors with her right eye. She also reports pain with eye movement. She has no double vision. She occasionally has headaches that are relieved by ibuprofen. One year ago, she had a similar episode that affected her left eye and resolved spontaneously. She has no history of serious illness. She works at a library and enjoys reading, even in poor lighting conditions. Her vital signs are within normal limits. The pupils are equal, round, and reactive to light and accommodation. Without correction, visual acuity is 20/50 in the left eye, and 20/100 in the right eye. With spectacles, the visual acuity is 20/20 in the left eye and 20/100 in the right eye. Slit lamp examination shows no abnormalities. A CT scan of the head shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Narrow-angle glaucoma
- B. Retinal detachment
- C. Macular degeneration
- D. Retinitis pigmentosa
- E. Optic neuritis (Correct Answer)
Red flags in geriatric patients Explanation: ***Optic neuritis***
- This condition presents with **acute monocular vision loss**, **pain with eye movement**, and **dyschromatopsia** (inability to distinguish colors), which are classic symptoms of optic neuritis.
- The recurrent nature affecting different eyes (**recurrent episodes in each eye**) and the spontaneous resolution are highly suggestive of **demyelinating disease**, such as **multiple sclerosis**, of which optic neuritis is often the initial presentation.
*Narrow-angle glaucoma*
- **Narrow-angle glaucoma** typically presents with **sudden, severe eye pain**, blurred vision, headache, and halos around lights due to acutely elevated intraocular pressure.
- The examination would reveal a **mid-dilated pupil** and **conjunctival injection**, which are not described in this patient.
*Retinal detachment*
- Patients with **retinal detachment** usually report a sudden onset of **floaters**, **flashes of light**, and a **"curtain" or "shadow" obscuring part of their vision**.
- **Pain with eye movement** and **dyschromatopsia** are not typical features of retinal detachment.
*Macular degeneration*
- **Macular degeneration** primarily affects central vision, causing **blurred or distorted vision**, particularly reading difficulty, and difficulty recognizing faces.
- It usually presents in **older individuals** and is not characterized by pain with eye movement or sudden, recurrent episodes of vision loss with dyschromatopsia.
*Retinitis pigmentosa*
- **Retinitis pigmentosa** is a group of inherited eye diseases that cause progressive vision loss, beginning with **night blindness** and then gradual **peripheral vision loss** (tunnel vision).
- The patient's acute monocular vision loss with pain and dyschromatopsia is not typical of the slow, progressive nature of retinitis pigmentosa.
Red flags in geriatric patients US Medical PG Question 9: A 21-year-old man presents with fever, headache, and clouded sensorium for the past 3 days. His fever is low-grade. He says his headache is mild-to-moderate in intensity and associated with nausea, vomiting, and photophobia. There is no history of a sore throat, pain on urination, abdominal pain, or loose motions. He smokes 1–2 cigarettes daily and drinks alcohol socially. Past medical history and family history are unremarkable. His vital signs include: blood pressure 120/80 mm Hg, pulse 106/min, temperature 37.3°C (99.2°F). On physical examination, he is confused, disoriented, and agitated. Extraocular movements are intact. The neck is supple on flexion. He is moving all his 4 limbs spontaneously. A noncontrast CT scan of the head is within normal limits. A lumbar puncture is performed, and cerebrospinal fluid results are still pending. The patient is started on empiric intravenous acyclovir. Which of the following clinical features favors encephalitis rather than meningitis?
- A. Photophobia
- B. Clouded sensorium (Correct Answer)
- C. Headache
- D. Fever
- E. Nausea and vomiting
Red flags in geriatric patients Explanation: ***Clouded sensorium***
- **Altered mental status**, including confusion, disorientation, agitation, and clouded sensorium, is the hallmark feature that distinguishes **encephalitis** from meningitis
- **Encephalitis** involves direct inflammation of the **brain parenchyma**, leading to impaired brain function and altered consciousness
- While meningitis can cause irritability, profound changes in consciousness like disorientation and confusion are characteristic of **brain tissue involvement** rather than isolated meningeal inflammation
- The patient's confusion, disorientation, and agitation indicate parenchymal dysfunction, making encephalitis the more likely diagnosis
*Photophobia*
- Photophobia is a common symptom in **both meningitis and encephalitis**, reflecting meningeal irritation
- It results from inflammation of the meninges and does not indicate brain parenchymal involvement
- This symptom is **not a differentiating factor** between the two conditions
*Headache*
- Headache is a prominent symptom in **both meningitis and encephalitis** due to meningeal inflammation and increased intracranial pressure
- While often severe in meningitis, it can also occur in encephalitis when meningeal irritation is present (meningoencephalitis)
- Headache alone **does not specifically favor** one diagnosis over the other
*Fever*
- Fever is a systemic response to infection and inflammation, present in **both meningitis and encephalitis**
- It reflects the body's immune response to the infectious agent
- The presence of fever **does not help distinguish** between inflammation of the meninges alone versus inflammation involving the brain parenchyma
*Nausea and vomiting*
- Nausea and vomiting can occur in **both meningitis and encephalitis**, often associated with meningeal irritation and increased intracranial pressure
- These symptoms result from stimulation of the vomiting center and are common in many CNS infections
- These symptoms are **not specific enough to differentiate** between the two conditions
Red flags in geriatric patients US Medical PG Question 10: A 72-year-old man is brought to the physician by his wife for memory issues over the last 7 months. The patient's wife feels that he has gradually become more forgetful. He commonly misplaces his car keys and forgets his children's names. He seems to have forgotten how to make dinner and sometimes serves uncooked noodles or raw meat. One night he parked his car in a neighbor's bushes and was found wandering the street. He has a history of hypertension, hyperlipidemia, and COPD. Current medications include atorvastatin, metoprolol, ipratropium, and fluticasone. Vital signs are within normal limits. He is alert and oriented to person and place only. Neurologic examination shows no focal findings. His Mini-Mental State Examination score is 19/30. A complete blood count and serum concentrations of electrolytes, urea nitrogen, creatinine, thyroid-stimulating hormone, liver function tests, vitamin B12 (cobalamin), and folate are within the reference range. Which of the following is the most appropriate next step in diagnosis?
- A. Electroencephalography
- B. PET scan
- C. MRI of the brain (Correct Answer)
- D. Lumbar puncture
- E. Neuropsychologic testing
Red flags in geriatric patients Explanation: ***MRI of the brain***
- An **MRI of the brain** is crucial for evaluating **structural causes of cognitive impairment**, such as tumors, strokes, hydrocephalus, or significant atrophy that might explain the patient's rapidly progressing memory loss and functional decline.
- Given the patient's age, rapidly worsening dementia symptoms, and normal initial lab work, imaging is essential to rule out **reversible or treatable causes** and to characterize the extent of neurodegeneration.
*Electroencephalography*
- **EEG** is primarily used to detect **seizure activity** or to evaluate for rapidly progressive encephalopathies like Creutzfeldt-Jakob disease, which is not indicated by the patient's presentation.
- The patient's symptoms are consistent with a dementia syndrome, not acute encephalopathy or seizures.
*PET scan*
- A **PET scan** (e.g., FDG-PET or amyloid-PET) can provide information about metabolic activity or amyloid plaques, useful for **differentiating types of dementia** (e.g., Alzheimer's disease).
- However, it is an advanced test typically considered after structural imaging has ruled out other causes and when the diagnosis remains unclear.
*Lumbar puncture*
- **Lumbar puncture** is performed to analyze **cerebrospinal fluid (CSF)** for biomarkers (e.g., tau, Aβ42 levels) to help diagnose specific neurodegenerative diseases like Alzheimer's or to rule out infectious/inflammatory causes.
- It's usually reserved for cases where other investigations are inconclusive or specific conditions are strongly suspected, and structural imaging has been performed.
*Neuropsychologic testing*
- **Neuropsychologic testing** provides a detailed assessment of various cognitive domains and can help to **characterize the pattern and severity of cognitive impairment**.
- While valuable, it is usually performed after initial medical workup and structural imaging to understand the functional impact of any identified brain changes or to further delineate the type of cognitive disorder.
More Red flags in geriatric patients US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
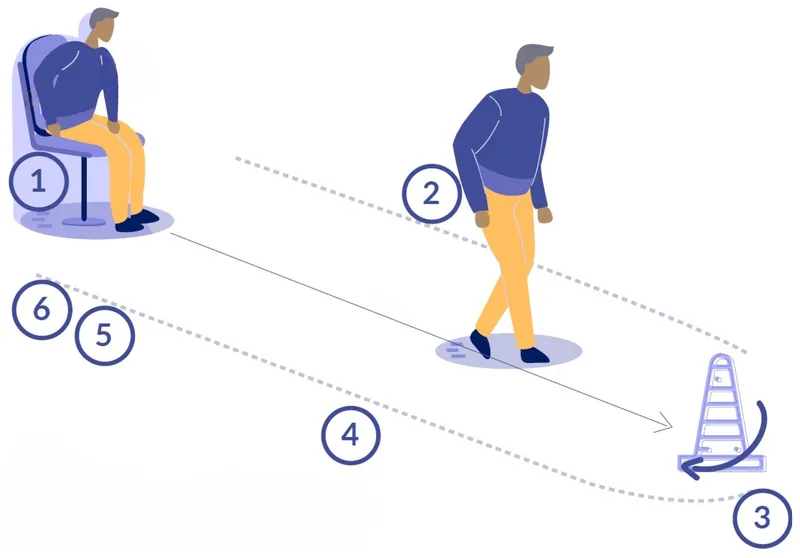 test showing patient rising from a chair, walking 3 meters, turning, and sitting back down)
test showing patient rising from a chair, walking 3 meters, turning, and sitting back down)