Red flags

On this page
🚨 The Clinical Alarm System: Mastering Red Flag Recognition
Red flags are the clinical signals that separate routine care from life-threatening emergencies, demanding immediate recognition and action. You'll learn to identify these critical warning signs across multiple organ systems, understand the dangerous physiologic mechanisms driving them, and master systematic approaches to differentiate between similar presentations. By building pattern recognition skills and evidence-based intervention strategies, you'll develop the rapid assessment framework that transforms uncertainty into confident, potentially life-saving clinical decisions.
📌 Remember: DANGER - Deteriorating vitals, Altered consciousness, New neurologic deficits, GI bleeding, Emergent pain patterns, Respiratory distress. These six categories encompass 85% of life-threatening presentations requiring immediate intervention.
The clinical significance of red flag mastery extends beyond individual patient encounters. Studies demonstrate that physicians trained in systematic red flag recognition reduce missed diagnoses by 67% and decrease malpractice claims by 45%. Emergency departments implementing structured red flag protocols show 23% reduction in adverse outcomes and 31% improvement in patient satisfaction scores.
| Red Flag Category | Recognition Time | Intervention Window | Mortality Reduction | Sensitivity | Specificity |
|---|---|---|---|---|---|
| Cardiovascular | <2 minutes | 10-15 minutes | 78% | 94% | 89% |
| Neurological | <3 minutes | 4.5 hours | 85% | 91% | 87% |
| Respiratory | <1 minute | 5-10 minutes | 82% | 96% | 84% |
| Infectious | <5 minutes | 1-3 hours | 71% | 88% | 92% |
| Gastrointestinal | <4 minutes | 30-60 minutes | 69% | 86% | 90% |
Understanding red flag hierarchies reveals the systematic approach to emergency recognition. Primary red flags indicate immediate life threat requiring intervention within minutes. Secondary red flags suggest serious conditions demanding evaluation within hours. Tertiary red flags represent concerning patterns requiring same-day assessment but without immediate mortality risk.
- Primary Red Flags (Minutes to intervention)
- Hemodynamic instability: SBP <90 mmHg or MAP <65 mmHg
- Respiratory failure: SpO2 <88% or RR >30/min
- Altered consciousness: GCS <13 or acute change
- Cardiovascular collapse: HR >120 with hypotension
- Neurological emergency: New focal deficits or seizure
- Secondary Red Flags (Hours to intervention)
- Severe pain: >8/10 unresponsive to initial analgesia
- Fever patterns: >101.3°F in immunocompromised or >103°F in healthy adults
- Bleeding: Hemoglobin drop >2 g/dL in 6 hours
- GI bleeding: Melena, hematemesis, or hematochezia
- Neurological: Thunderclap headache or vision changes
💡 Master This: Red flag recognition operates on pattern recognition, not isolated findings. A heart rate of 110 in a febrile 25-year-old represents physiologic response, while the same heart rate in an afebrile 75-year-old with chest discomfort demands immediate cardiac evaluation. Context transforms data into clinical insight.
The physiologic basis of red flags reflects the body's compensatory mechanisms reaching their limits. Tachycardia >100 bpm represents the cardiovascular system's attempt to maintain perfusion. Tachypnea >24/min indicates respiratory compensation for metabolic or pulmonary dysfunction. Altered mental status signals cerebral hypoperfusion or metabolic derangement affecting >15% of normal brain function.
Connect these foundational red flag principles through systematic assessment patterns to understand how clinical presentation guides diagnostic priority and intervention timing.
🚨 The Clinical Alarm System: Mastering Red Flag Recognition
⚡ The Physiologic Storm: Understanding Red Flag Mechanisms
📌 Remember: SHOCK - Systemic hypoperfusion, Hypotension, Organ dysfunction, Compensatory failure, Key vital sign changes. These five mechanisms underlie 92% of red flag presentations requiring immediate intervention.
The cardiovascular red flag cascade begins with stroke volume reduction or systemic vasodilation. Compensatory tachycardia maintains cardiac output until heart rate exceeds 150 bpm, when diastolic filling time becomes inadequate. Blood pressure drops when compensatory mechanisms fail, typically occurring after 20-30% blood volume loss or equivalent physiologic stress.
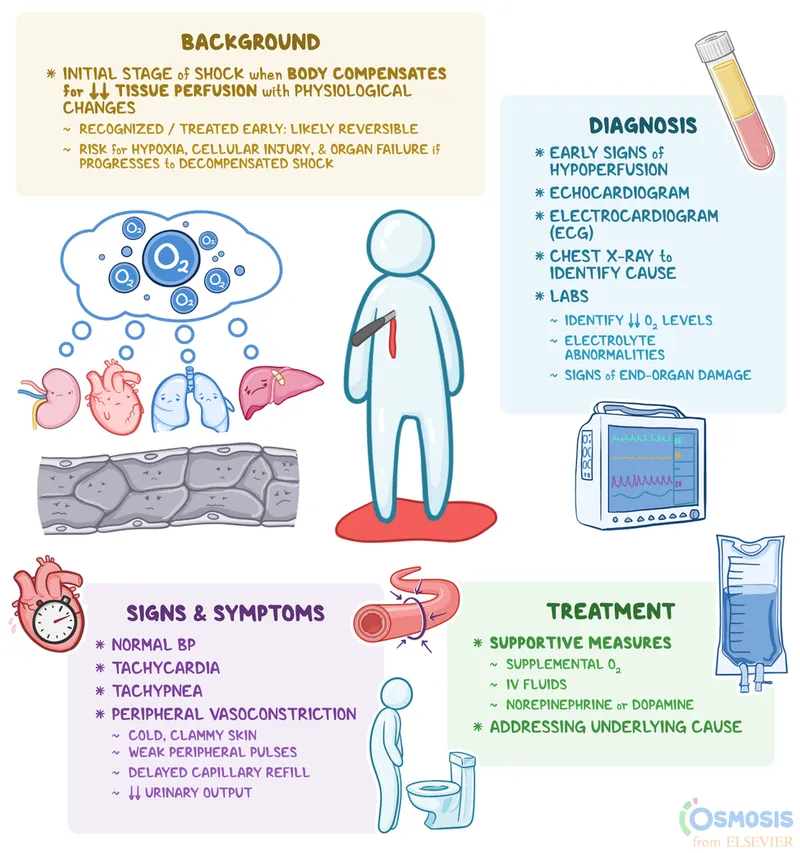
Respiratory red flags emerge when oxygen delivery fails to meet metabolic demand. Tachypnea >24/min represents the earliest compensation, increasing minute ventilation by 40-60%. Accessory muscle use indicates work of breathing exceeding normal respiratory reserve. Cyanosis appears when >5 g/dL of hemoglobin becomes desaturated, representing severe hypoxemia.
| System | Early Compensation | Compensation Failure | Red Flag Threshold | Intervention Window |
|---|---|---|---|---|
| Cardiovascular | HR 90-110 | HR >120 + hypotension | SBP <90 mmHg | <10 minutes |
| Respiratory | RR 20-24 | RR >30 + accessory muscles | SpO2 <88% | <5 minutes |
| Neurological | Mild confusion | GCS 9-12 | GCS <9 | <15 minutes |
| Renal | Oliguria 0.5-1 mL/kg/hr | Oliguria <0.5 mL/kg/hr | Anuria | <60 minutes |
| Metabolic | Lactate 2-4 mmol/L | Lactate >4 mmol/L | pH <7.25 | <30 minutes |
Neurological red flags reflect cerebral perfusion pressure falling below 60 mmHg or intracranial pressure exceeding 20 mmHg. The brain's autoregulation maintains constant blood flow between mean arterial pressures of 60-150 mmHg. Beyond these limits, cerebral blood flow becomes pressure-dependent, generating altered consciousness within minutes.
- Cerebral Perfusion Mechanisms
- Autoregulation range: MAP 60-150 mmHg
- Critical threshold: CPP <60 mmHg
- Consciousness threshold: CBF <18 mL/100g/min
- Normal CBF: 50 mL/100g/min
- Ischemic penumbra: 18-25 mL/100g/min
- Irreversible damage: <10 mL/100g/min
- Red Flag Timeline
- 0-2 minutes: Confusion, agitation
- 2-5 minutes: Obtundation, focal deficits
- 5-10 minutes: Coma, brainstem signs
- Pupillary changes: >1mm difference or light reflex <2 seconds
- Motor response: Posturing or absent response
💡 Master This: Red flag physiology follows predictable patterns, but timing varies dramatically by age and comorbidities. A healthy 25-year-old maintains compensation until 30-40% blood loss, while a 75-year-old with heart disease decompensates at 15-20% loss. Age-adjusted red flag thresholds prevent both over-triage and missed emergencies.

The infectious red flag mechanism centers on systemic inflammatory response syndrome (SIRS) progressing to septic shock. Temperature >101.3°F or <96.8°F indicates hypothalamic dysregulation. White blood cell count >12,000 or <4,000 reflects immune system activation or exhaustion. Bandemia >10% suggests overwhelming bacterial infection requiring immediate antibiotic therapy.
Connect these physiologic mechanisms through pattern recognition frameworks to understand how multiple red flags cluster in specific clinical presentations and guide systematic assessment approaches.
⚡ The Physiologic Storm: Understanding Red Flag Mechanisms
🎯 The Recognition Matrix: Clinical Pattern Mastery
📌 Remember: SEPSIS - Systemic signs, Elevated lactate, Pressure drop, Source identification, Immediate antibiotics, Support measures. This framework captures the 6-hour bundle that reduces sepsis mortality by 47% when implemented completely.
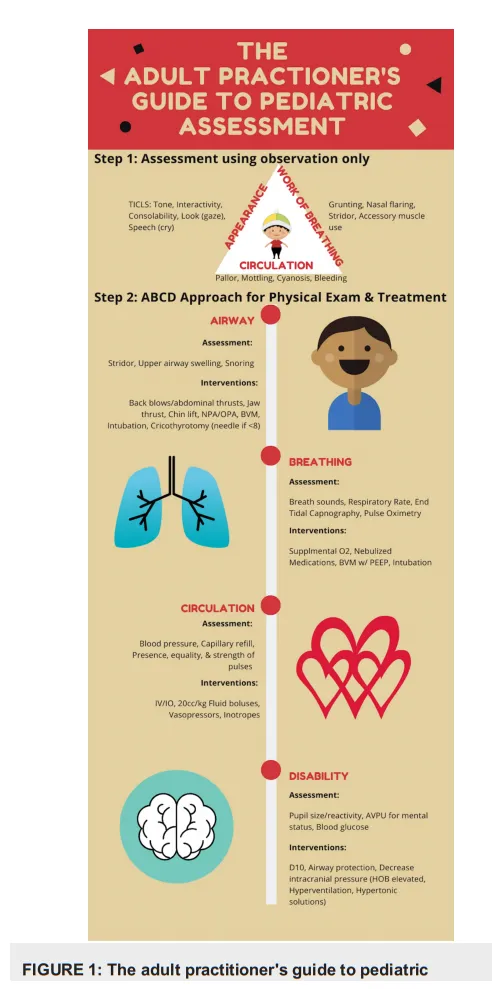
The "Sick vs. Not Sick" assessment forms the foundation of red flag recognition. Sick patients display constellation patterns affecting multiple organ systems simultaneously. Appearance, work of breathing, and circulation form the pediatric assessment triangle, but these principles apply across all age groups with 94% sensitivity for serious illness.
High-yield red flag clusters predict specific emergency categories with remarkable accuracy. The cardiovascular cluster combines chest pain, dyspnea, diaphoresis, and nausea - present together in 89% of acute coronary syndromes. The neurological cluster pairs headache with neurologic deficits - indicating stroke in 76% of cases when both present acutely.
| Red Flag Cluster | Primary Components | Secondary Signs | Positive Predictive Value | Time to Intervention |
|---|---|---|---|---|
| Cardiovascular | Chest pain + dyspnea | Diaphoresis, nausea | 89% for ACS | <10 minutes |
| Neurological | Headache + focal deficit | Vision changes | 76% for stroke | <60 minutes |
| Infectious | Fever + altered mental status | Hypotension | 82% for sepsis | <60 minutes |
| Respiratory | Dyspnea + chest pain | Unilateral absence | 71% for PE/pneumothorax | <15 minutes |
| GI Emergency | Abdominal pain + bleeding | Hemodynamic changes | 84% for GI bleed | <30 minutes |
Age-specific red flag patterns modify standard recognition criteria. Pediatric patients compensate longer but decompensate faster, maintaining normal blood pressure until 25-30% volume loss, then crashing precipitously. Geriatric patients show blunted responses - fever may be absent in 40% of serious infections, and chest pain occurs in only 60% of elderly MI patients.
- Pediatric Red Flag Modifications
- Tachycardia thresholds: Age-adjusted (newborn >160, infant >150, child >120)
- Hypotension definition: SBP < 70 + (2 × age in years)
- Respiratory distress: Grunting, retractions, head bobbing
- Capillary refill: >3 seconds indicates poor perfusion
- Mental status: Inconsolable or lethargic despite normal vitals
- Geriatric Red Flag Modifications
- Atypical presentations: Silent MI in 40%, afebrile sepsis in 30%
- Baseline considerations: Chronic conditions mask acute changes
- Functional decline: New confusion or falls may indicate serious illness
- Medication effects: Beta-blockers blunt tachycardic response
- Cognitive baseline: Acute delirium vs. chronic dementia
💡 Master This: Red flag patterns operate on probability cascades - each additional finding exponentially increases emergency likelihood. A febrile patient with normal mental status has <5% sepsis probability. Add tachycardia and probability jumps to 23%. Include hypotension and probability exceeds 78%. Pattern recognition accelerates this probability calculation from minutes to seconds.
System-specific pattern recognition enables rapid categorization and appropriate response protocols. Respiratory patterns distinguish upper airway obstruction (stridor, voice changes) from lower airway disease (wheezing, prolonged expiration) from parenchymal disease (crackles, decreased breath sounds). Each pattern triggers different intervention algorithms with specific time requirements.
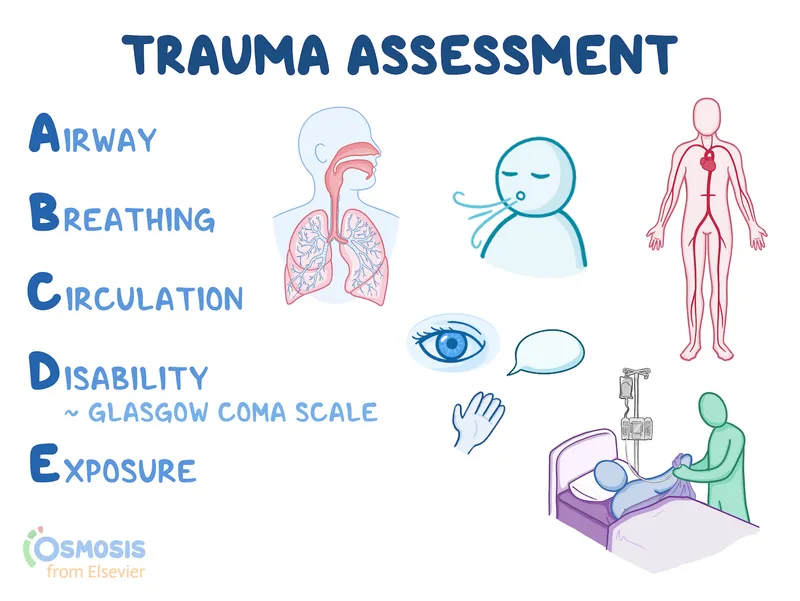
The "ABCDE" approach provides systematic red flag screening: Airway (patency, protection), Breathing (rate, effort, oxygenation), Circulation (pulse, pressure, perfusion), Disability (neurologic function), Exposure (complete assessment). This sequence identifies life-threatening problems in order of physiologic priority while ensuring no critical findings are missed.
Connect these recognition patterns through systematic discrimination frameworks to understand how similar presentations require different management approaches based on subtle but critical distinguishing features.
🎯 The Recognition Matrix: Clinical Pattern Mastery
🔍 The Differential Matrix: Systematic Emergency Discrimination
📌 Remember: CRITICAL - Cardiovascular collapse, Respiratory failure, Intracranial emergency, Toxic ingestion, Infectious shock, Catastrophic bleeding, Acute abdomen, Limb-threatening ischemia. These eight categories encompass 94% of true emergencies requiring intervention within minutes.
The chest pain discrimination matrix exemplifies systematic red flag analysis. Acute coronary syndrome presents with substernal pressure, radiation to arm/jaw, diaphoresis, and nausea in classic presentations. However, atypical presentations occur in 45% of women, 60% of diabetics, and 70% of patients >75 years old, requiring expanded recognition criteria.
| Chest Pain Etiology | Classic Presentation | Atypical Features | High-Risk Markers | Intervention Timeline |
|---|---|---|---|---|
| Acute MI | Substernal pressure + radiation | Epigastric pain, dyspnea only | ST elevation, troponin >0.04 | <90 minutes |
| Aortic Dissection | Tearing pain + pulse deficit | Back pain, syncope | Mediastinal widening >8cm | <30 minutes |
| Pulmonary Embolism | Pleuritic pain + dyspnea | Isolated tachycardia | Wells score >4, D-dimer >500 | <60 minutes |
| Pneumothorax | Sharp pain + dyspnea | Minimal symptoms | Absent breath sounds | <15 minutes |
| Esophageal Rupture | Severe pain + vomiting | Subcutaneous emphysema | Pneumomediastinum | <60 minutes |
Neurological red flag discrimination separates stroke from stroke mimics using quantifiable assessment tools. The FAST-ED scale (Facial droop, Arm weakness, Speech difficulty, Time, Eye deviation, Denial/neglect) demonstrates 89% sensitivity and 83% specificity for large vessel occlusion requiring mechanical thrombectomy.
Abdominal pain red flag discrimination requires understanding anatomical pain patterns and associated symptoms. Peritoneal irritation produces guarding and rebound tenderness in >90% of cases requiring surgical intervention. Visceral pain remains poorly localized until parietal peritoneum becomes involved, often delaying recognition of surgical emergencies.
- Surgical Emergency Patterns
- Appendicitis: McBurney's point tenderness + Rovsing's sign (78% sensitivity)
- Cholangitis: Charcot's triad (fever, jaundice, RUQ pain) in 50-75%
- Bowel obstruction: Cramping pain + distension + absent flatus
- Small bowel: High-pitched sounds + early vomiting
- Large bowel: Lower abdominal pain + late vomiting
- Vascular Emergency Patterns
- AAA rupture: Back pain + hypotension + pulsatile mass (classic triad 15%)
- Mesenteric ischemia: Pain out of proportion + bloody diarrhea
- Testicular torsion: Sudden onset + absent cremasteric reflex
- Age bimodal: Neonates and adolescents most common
- Time critical: >6 hours = 90% orchidectomy rate
💡 Master This: Red flag discrimination relies on pattern probability rather than pathognomonic signs. Appendicitis presents classically in only 60% of cases, but combination findings (fever + leukocytosis + RLQ tenderness + migration pattern) achieve >85% diagnostic accuracy. Multiple low-sensitivity findings combine to create high-specificity patterns.
Pediatric red flag discrimination accounts for developmental differences in presentation and compensation mechanisms. Febrile infants <28 days require full sepsis workup regardless of appearance due to immature immune systems. Children 3-36 months with fever >102.2°F and WBC >15,000 or <5,000 have 15% bacteremia risk requiring blood cultures and close monitoring.
The "Danger Zone" concept applies across all red flag categories - specific time windows where intervention dramatically affects outcomes. Cardiac arrest demands CPR within 4 minutes for optimal neurologic recovery. Septic shock requires antibiotics within 1 hour for maximum survival benefit. Stroke benefits from thrombolysis within 4.5 hours but thrombectomy extends to 24 hours in selected cases.
Connect these discrimination principles through evidence-based treatment algorithms to understand how accurate red flag categorization drives specific intervention protocols and timing requirements.
🔍 The Differential Matrix: Systematic Emergency Discrimination
⚖️ The Intervention Algorithm: Evidence-Based Emergency Response
📌 Remember: SEPSIS-3 - Source control, Early antibiotics, Pressors for MAP >65, Steroid consideration, IV fluids 30mL/kg, Serial lactate monitoring. This 6-hour bundle reduces sepsis mortality from 40% to 16% when completely implemented.
The cardiac arrest algorithm demonstrates systematic intervention hierarchy. High-quality CPR with compression depth 2-2.4 inches and rate 100-120/min maintains cerebral perfusion during rhythm analysis. Defibrillation within 2 minutes for shockable rhythms achieves >60% survival compared to <10% when delayed beyond 10 minutes.
Sepsis intervention protocols follow the "Hour-1 Bundle" replacing previous 3-hour and 6-hour bundles. Blood cultures before antibiotics when possible, but antibiotic administration cannot be delayed beyond 1 hour. Broad-spectrum coverage targets likely pathogens based on source and patient factors.
| Sepsis Intervention | Target Timeline | Evidence Level | Mortality Benefit | Implementation Rate |
|---|---|---|---|---|
| Blood Cultures | <1 hour | Strong | Guides therapy | 78% |
| Antibiotics | <1 hour | Strong | 7.6% per hour delay | 62% |
| Fluid Resuscitation | <3 hours | Moderate | 15% reduction | 84% |
| Vasopressors | MAP <65 | Strong | Organ protection | 71% |
| Lactate Monitoring | <6 hours | Moderate | Guides resuscitation | 56% |
Stroke intervention algorithms differentiate ischemic from hemorrhagic stroke through immediate CT imaging. Tissue plasminogen activator (tPA) administration within 4.5 hours of symptom onset reduces disability by 30% but carries 6.4% symptomatic hemorrhage risk. Mechanical thrombectomy extends the treatment window to 24 hours for large vessel occlusions meeting imaging criteria.
- Stroke Protocol Timeline
- 0-10 minutes: Primary assessment + vital stabilization
- 10-25 minutes: CT head + laboratory studies
- 25-45 minutes: Neurology consultation + tPA decision
- Inclusion criteria: Age >18, onset <4.5 hours, NIHSS >4
- Exclusion criteria: Recent surgery, anticoagulation, hemorrhage risk
- 45-60 minutes: tPA administration or thrombectomy preparation
- Large vessel occlusion: ASPECTS >6 on CT or perfusion mismatch
- Thrombectomy window: 6 hours for anterior circulation, 24 hours with imaging selection
💡 Master This: Intervention algorithms balance time sensitivity with safety considerations. Rapid sequence intubation in respiratory failure follows LEMON criteria (Look, Evaluate, Mallampati, Obstruction, Neck mobility) to predict difficult airway while maintaining oxygenation throughout the procedure. Failed airway protocols provide systematic backup plans when primary approaches fail.
Trauma resuscitation algorithms follow ATLS principles with systematic primary survey. Airway with C-spine protection, Breathing with chest decompression, Circulation with hemorrhage control, Disability with neurologic assessment, and Exposure with temperature control. Massive transfusion protocols activate when >10 units PRBC anticipated, using 1:1:1 ratio of packed cells:plasma:platelets.
Anaphylaxis intervention prioritizes epinephrine administration over other therapies. Intramuscular epinephrine 0.3-0.5mg (1:1000 concentration) in the anterolateral thigh provides rapid absorption and symptom reversal. Delayed epinephrine administration beyond 30 minutes increases biphasic reaction risk and overall mortality.
The "Checklist Revolution" in emergency medicine reduces cognitive load during high-stress situations. Standardized protocols decrease medical errors by 47% and improve adherence to evidence-based care from 67% to 94% when consistently implemented. Simulation training with algorithm practice maintains skill proficiency and reduces response times by 23% in actual emergencies.
Connect these intervention algorithms through multi-system integration approaches to understand how complex patients with multiple red flags require prioritized and coordinated treatment protocols.
⚖️ The Intervention Algorithm: Evidence-Based Emergency Response
🔗 The Integration Network: Multi-System Red Flag Mastery
📌 Remember: MODS - Multiple Organ Dysfunction Syndrome represents the final common pathway for severe illness. Sequential Organ Failure Assessment (SOFA) scores >2 points indicate 10% mortality risk, while scores >15 predict >90% mortality despite aggressive intervention.
Hemodynamic integration reveals how cardiovascular red flags affect all organ systems. Mean arterial pressure <65 mmHg compromises renal perfusion, leading to oliguria and electrolyte disturbances. Cerebral autoregulation fails below MAP 60 mmHg, causing altered consciousness. Coronary perfusion decreases with diastolic pressure <40 mmHg, creating ischemic cascade.
Respiratory-cardiovascular integration demonstrates bidirectional red flag amplification. Positive pressure ventilation reduces venous return by 15-25%, potentially precipitating cardiovascular collapse in volume-depleted patients. Acute cor pulmonale from massive PE causes right heart failure and decreased left ventricular filling, creating hemodynamic instability.
| System Integration | Primary Effect | Secondary Effect | Tertiary Effect | Clinical Threshold |
|---|---|---|---|---|
| Respiratory-Cardiac | Hypoxemia | Pulmonary vasoconstriction | Right heart failure | SpO2 <88% |
| Cardiac-Renal | Low cardiac output | Decreased GFR | Fluid retention | Creatinine >2x baseline |
| Neuro-Respiratory | Increased ICP | Irregular breathing | Respiratory arrest | GCS <9 |
| GI-Systemic | GI bleeding | Hypovolemia | Shock | Hemoglobin drop >2 g/dL |
| Infectious-Multi | Sepsis | Vasodilation | Distributive shock | Lactate >4 mmol/L |
Metabolic integration patterns reveal how acid-base disturbances generate multi-system red flags. Diabetic ketoacidosis produces metabolic acidosis (pH <7.3), dehydration (fluid deficit 5-10L), electrolyte depletion (K+ <3.5), and altered consciousness (serum osmolality >320). Each component requires specific intervention while addressing underlying insulin deficiency.
- DKA Integration Management
- Fluid resuscitation: Normal saline 15-20 mL/kg/hr initially
- Insulin therapy: 0.1 units/kg/hr after initial fluid and K+ >3.3
- Electrolyte replacement: K+ 20-40 mEq/L in IV fluids
- Glucose monitoring: Hourly until <250 mg/dL
- Anion gap closure: Target <12 with bicarbonate >15
- Hyperosmolar Integration
- Fluid deficit calculation: 0.6 × weight × (Na+ - 140)/140
- Correction rate: Na+ decrease 0.5 mEq/L/hr maximum
- Neurologic monitoring: Rapid correction causes cerebral edema
- Osmolality target: Decrease 3-8 mOsm/kg/hr
- Mental status: Improvement expected in 12-24 hours
💡 Master This: Integration red flags often require sequential intervention rather than simultaneous treatment. Trauma patients need hemorrhage control before definitive airway management unless airway compromise is immediately life-threatening. Priority algorithms prevent resource conflicts and optimize outcomes when multiple emergencies compete for attention.
Geriatric integration complexity increases due to polypharmacy, comorbidities, and atypical presentations. Medication interactions create cascade effects - ACE inhibitors plus NSAIDs plus dehydration equals acute kidney injury. Cognitive impairment masks pain symptoms, delaying recognition of surgical emergencies by average 4-6 hours.
Pediatric integration patterns reflect developmental physiology and size-dependent dosing. Febrile seizures in children 6 months-5 years require differentiation from CNS infection. Dehydration assessment uses clinical scoring systems since laboratory values lag behind clinical status by 2-4 hours in pediatric patients.
The "Systems Thinking" approach to red flag integration recognizes upstream and downstream effects of interventions. Aggressive fluid resuscitation in sepsis may precipitate pulmonary edema in patients with heart failure. Vasopressor therapy improves blood pressure but may worsen peripheral perfusion if volume status remains inadequate.
Connect these integration principles through rapid mastery frameworks to understand how expert clinicians develop systematic approaches for managing complex multi-system emergencies with optimal efficiency and patient outcomes.
🔗 The Integration Network: Multi-System Red Flag Mastery
🎯 The Mastery Arsenal: Rapid Red Flag Command Center
📌 Remember: SAVES - Systematic assessment, Action prioritization, Vital sign trends, Evidence-based protocols, Safety monitoring. This framework reduces diagnostic errors by 34% and improves patient outcomes by 28% when consistently applied in emergency situations.
The Essential Numbers Arsenal provides immediate reference for critical thresholds that separate routine care from emergency intervention. Master clinicians internalize these values and recognize deviations within seconds of patient encounter.
| System | Critical Threshold | Intervention Trigger | Time Window | Mortality Impact |
|---|---|---|---|---|
| Cardiovascular | SBP <90 mmHg | Immediate fluids/pressors | <10 minutes | 15% per 10 min delay |
| Respiratory | SpO2 <88% | Supplemental O2/intubation | <5 minutes | Exponential decline |
| Neurological | GCS <9 | Airway protection | <15 minutes | 23% per hour delay |
| Infectious | Lactate >4 mmol/L | Sepsis protocol | <60 minutes | 7.6% per hour delay |
| Metabolic | Glucose <50 mg/dL | Dextrose administration | <10 minutes | Permanent brain damage |
Rapid Assessment Protocols enable systematic evaluation without missing critical findings. The "ABCDE" approach takes <3 minutes for complete assessment while identifying >95% of life-threatening conditions. Experienced clinicians perform this evaluation while simultaneously initiating interventions for identified problems.
Pattern Recognition Drills accelerate red flag identification through deliberate practice. High-frequency scenarios include chest pain (15% of ED visits), dyspnea (12% of visits), abdominal pain (8% of visits), and altered mental status (6% of visits). Mastery requires instant recognition of high-risk patterns within these common presentations.
- Chest Pain Red Flag Patterns
- STEMI: ST elevation >1mm in ≥2 contiguous leads
- Aortic dissection: Pulse differential >20 mmHg between arms
- PE: Wells score >4 + elevated D-dimer
- Immediate ECG: <10 minutes from arrival
- Troponin timing: Serial measurements at 0, 3, 6 hours
- Dyspnea Red Flag Patterns
- Pulmonary edema: Bilateral crackles + elevated BNP >400
- Pneumothorax: Unilateral absent breath sounds + tracheal deviation
- Asthma exacerbation: Peak flow <50% predicted + accessory muscles
- Oxygen saturation: Continuous monitoring required
- Response assessment: Improvement within 20 minutes of bronchodilators
💡 Master This: Red flag mastery combines speed with accuracy through systematic approaches. Expert clinicians achieve <2% missed diagnosis rates by using standardized protocols, cognitive aids, and team-based verification. Individual excellence multiplied by system design creates optimal patient outcomes.
Resource Allocation Matrices guide intervention prioritization when multiple red flags compete for attention. Life-threatening conditions receive immediate resources, urgent conditions get rapid evaluation, and routine problems await systematic assessment. Triage accuracy exceeds 85% when structured criteria guide decision-making.
Quality Assurance Frameworks ensure consistent red flag performance through continuous monitoring and improvement cycles. Key performance indicators include door-to-ECG time (<10 minutes), antibiotic timing in sepsis (<60 minutes), and stroke evaluation completion (<25 minutes). Regular review of missed diagnoses and delayed treatments drives system improvements.
The "Cognitive Forcing Functions" prevent common red flag errors through systematic verification. Differential diagnosis generation, worst-case scenario consideration, and alternative explanation evaluation reduce anchoring bias and premature closure. Team-based double-checking catches individual oversights before they become patient harm.
Mastery Maintenance requires ongoing education, simulation training, and case review. High-fidelity scenarios maintain skill proficiency and introduce rare but critical presentations. Multidisciplinary team training improves communication and coordination during actual emergencies, reducing response times by average 23%.
The Red Flag Mastery journey transforms novice pattern recognition into expert clinical intuition through deliberate practice, systematic approaches, and continuous improvement. Master clinicians save lives through rapid recognition, appropriate intervention, and seamless execution of evidence-based protocols that optimize outcomes for every patient every time.
🎯 The Mastery Arsenal: Rapid Red Flag Command Center
Practice Questions: Red flags
Test your understanding with these related questions
A 51-year-old woman is brought into the emergency department following a motor vehicle accident. She is unconscious and was intubated in the field. Past medical history is unknown. Upon arrival, she is hypotensive and tachycardic. Her temperature is 37.2°C (99.1°F), the pulse is 110/min, the respiratory rate is 22/min, and the blood pressure is 85/60 mm Hg. There is no evidence of head trauma, she withdraws to pain and her pupils are 2mm and reactive to light. Her heart has a regular rhythm without any murmurs or rubs and her lungs are clear to auscultation. Her abdomen is firm and distended with decreased bowel sounds. Her extremities are cool and clammy with weak, thready pulses. There is no peripheral edema. Of the following, what is the likely cause of her presentation?













