Symptom-based differential diagnosis approach US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Symptom-based differential diagnosis approach. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Symptom-based differential diagnosis approach US Medical PG Question 1: A 55-year-old man with a past medical history of obesity and hyperlipidemia suddenly develops left-sided chest pain and shortness of breath while at work. He relays to coworkers that the pain is intense and has spread to his upper left arm over the past 10 minutes. He reports it feels a lot like the “heart attack” he had a year ago. He suddenly collapses and is unresponsive. Coworkers perform cardiopulmonary resuscitation for 18 minutes until emergency medical services arrives. Paramedics pronounce him dead at the scene. Which of the following is the most likely cause of death in this man?
- A. Pericarditis
- B. Aortic dissection
- C. Atrial fibrillation
- D. Ventricular tachycardia (Correct Answer)
- E. Free wall rupture
Symptom-based differential diagnosis approach Explanation: ***Ventricular tachycardia***
- The patient's history of MI **1 year ago** creates a substrate of **scarred myocardium** that predisposes to life-threatening ventricular arrhythmias.
- The current presentation of sudden chest pain radiating to the arm suggests **acute re-infarction**, which triggers electrical instability in already compromised myocardium.
- **Ventricular tachycardia (VT)** degenerating to **ventricular fibrillation (VF)** is the **most common cause of sudden cardiac death** in patients with prior MI, especially during acute ischemic events.
- The rapid collapse and death within minutes, despite CPR, is classic for fatal ventricular arrhythmia.
*Free wall rupture*
- Free wall rupture is a **mechanical complication** that occurs **3-14 days** (typically days 3-7) after an **acute MI**, not 1 year later.
- By 1 year post-MI, the ventricular wall has either healed with fibrous scar tissue or formed a chronic ventricular aneurysm.
- While this would cause sudden death via cardiac tamponade, the **timing makes this unlikely** in this scenario.
*Pericarditis*
- Pericarditis causes **pleuritic chest pain** that is sharp, positional, and typically relieved by leaning forward.
- It is **not an immediate cause of sudden cardiac death** and would not explain the rapid collapse and unresponsiveness.
- While post-MI (Dressler) pericarditis can occur weeks after MI, it doesn't cause this presentation.
*Aortic dissection*
- Aortic dissection presents with **sudden, severe, tearing chest pain** often radiating to the back.
- While potentially fatal, the patient's description of pain "a lot like the heart attack he had a year ago" and his cardiac risk factors make **recurrent MI with fatal arrhythmia more likely**.
- No mention of blood pressure differential or pulse deficits that would suggest dissection.
*Atrial fibrillation*
- Atrial fibrillation is a **supraventricular arrhythmia** that causes palpitations, dyspnea, and irregular pulse.
- It is **not typically immediately fatal** in isolation and does not cause sudden collapse and death within minutes.
- While AF can lead to stroke or heart failure over time, it doesn't explain this acute sudden cardiac death.
Symptom-based differential diagnosis approach US Medical PG Question 2: A 16-year-old boy presents to the emergency department with abdominal pain and tenderness. The pain began approximately 2 days ago in the area just above his umbilicus and was crampy in nature. Earlier this morning, the pain moved laterally to his right lower abdomen. At that time, the pain in the right lower quadrant became severe and constant and woke him up from sleep. He decided to come to the hospital. The patient is nauseous and had a low-grade fever of 37.8°C (100.1°F). Other vitals are normal. Upon physical examination, the patient has rebound tenderness but a negative psoas sign while the remaining areas of his abdomen are non-tender. His rectal exam is normal. Laboratory tests show a white cell count of 15,000/mm3. Urinalysis and other laboratory findings were negative. What conclusion can be drawn about the nerves involved in the transmission of this patient’s pain during the physical exam?
- A. His pain is transmitted bilaterally by somatic afferent nerve fibers of the abdomen.
- B. His pain is transmitted by somatic afferent nerve fibers located in the right flank.
- C. His pain is transmitted by the pelvic nerves.
- D. His pain is transmitted by right somatic nerve fibers. (Correct Answer)
- E. His pain is mainly transmitted by the right splanchnic nerve.
Symptom-based differential diagnosis approach Explanation: ***His pain is transmitted by right somatic nerve fibers.***
- The **migration of pain from the periumbilical region to the right lower quadrant** and becoming **severe and constant** indicates parietal peritoneal irritation.
- **Somatic nerve fibers** innervate the parietal peritoneum and are responsible for transmitting **sharp, localized pain** typically associated with appendicitis in the right lower quadrant.
*His pain is transmitted bilaterally by somatic afferent nerve fibers of the abdomen.*
- While **visceral pain** from the initial appendiceal inflammation can be perceived bilaterally in the periumbilical region due to **bilateral innervation of visceral organs**, the **localized right lower quadrant pain** signifies involvement of **unilaterally innervated parietal peritoneum**.
- The physical exam findings of **rebound tenderness** strongly suggest **localized peritoneal inflammation**, which is transmitted by **unilateral somatic nerves** at the site of inflammation, not bilaterally across the abdomen.
*His pain is transmitted by somatic afferent nerve fibers located in the right flank.*
- The **right flank** refers to the lateral aspect of the abdomen, while the pain is specifically localized to the **right lower quadrant**.
- Although somatic nerves are involved, stating "right flank" is **too broad and imprecise** given the very specific localization of the pain to the right lower quadrant where the inflamed appendix is typically situated.
*His pain is transmitted by the pelvic nerves.*
- **Pelvic nerves** primarily carry parasympathetic fibers and visceral afferent fibers from pelvic organs, not the somatic pain from the parietal peritoneum in the right lower quadrant.
- Pain from **pelvic organs** or **pelvic peritoneum** would be transmitted via these nerves, but the localized pain here is distinctly higher than typical pelvic organ pain.
*His pain is mainly transmitted by the right splanchnic nerve.*
- **Splanchnic nerves** primarily carry **visceral afferent fibers** responsible for the dull, poorly localized, initial periumbilical pain of appendicitis.
- They do not transmit the **sharp, well-localized somatic pain** associated with parietal peritoneal irritation, which is characteristic of the pain migrating to the right lower quadrant.
Symptom-based differential diagnosis approach US Medical PG Question 3: A 72-year-old woman comes to the emergency department 1 hour after the sudden onset of a diffuse, dull, throbbing headache. She also reports blurred vision, nausea, and one episode of vomiting. She has a history of poorly controlled hypertension. A photograph of her fundoscopic examination is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Hemorrhagic lacunar stroke
- B. Transient ischemic attack
- C. Giant cell arteritis
- D. Hypertensive emergency (Correct Answer)
- E. Epidural hematoma
Symptom-based differential diagnosis approach Explanation: ***Hypertensive emergency***
- The patient's presentation of a **sudden headache**, along with **blurred vision** and nausea, suggests increased intracranial pressure due to severely elevated blood pressure.
- Poorly controlled hypertension is a significant risk factor, leading to possible **end-organ damage** such as hypertensive retinopathy with papilledema or hypertensive encephalopathy.
- Fundoscopic examination showing **papilledema** confirms elevated intracranial pressure, consistent with malignant hypertension.
*Hemorrhagic lacunar stroke*
- Lacunar strokes are **small subcortical infarcts** caused by occlusion of penetrating arteries and are typically **ischemic, not hemorrhagic**.
- They present with focal neurological deficits (pure motor stroke, pure sensory stroke, ataxic hemiparesis) rather than the **diffuse symptoms** and papilledema seen here.
- While hypertension is a risk factor, lacunar infarcts do not cause increased intracranial pressure or papilledema.
*Transient ischemic attack*
- Characterized by temporary neurological deficits that resolve within 24 hours, typically without severe headaches or sustained symptoms.
- Patients may experience **focal weakness or sensory changes** but would not have papilledema or signs of increased intracranial pressure.
- The persistent nature of this patient's symptoms makes TIA unlikely.
*Giant cell arteritis*
- This condition usually presents with **temporal headaches**, jaw claudication, and potential vision loss from arteritic anterior ischemic optic neuropathy.
- Vision loss in GCA is due to ischemic optic nerve damage, not papilledema from increased intracranial pressure.
- More common in older adults but is associated with systemic symptoms like fever, malaise, and elevated ESR/CRP.
*Epidural hematoma*
- Typically follows head trauma and presents with a **lucid interval**, followed by rapid deterioration from expanding hematoma.
- Usually caused by middle meningeal artery injury with classic lens-shaped hematoma on CT.
- The lack of trauma history and the chronic hypertension make this diagnosis unlikely.
Symptom-based differential diagnosis approach US Medical PG Question 4: A 75-year-old woman presents to her primary care physician with her son because she is convinced that people are stealing from her. Her son claims she has been misplacing her medications and money throughout the house. She recently lost her husband to old age and has become reclusive and no longer wants people to visit. Physical examination is unremarkable and the patient is oriented to person, time, and place. A mini-mental status examination (MMSE) is performed and she has difficulty recalling words after 5 minutes and also has problems with serial subtraction. Which of the following is the most likely diagnosis in this patient?
- A. Histrionic personality disorder
- B. Schizophrenia
- C. Delirium
- D. Schizoid personality disorder
- E. Dementia (Correct Answer)
Symptom-based differential diagnosis approach Explanation: ***Dementia***
- The patient has **primary cognitive impairment** evidenced by MMSE deficits (poor delayed recall, impaired serial subtraction) and functional decline (misplacing items).
- Her **delusions of theft are secondary to dementia**, a common behavioral and psychological symptom of dementia (BPSD), particularly in Alzheimer's disease.
- The **insidious onset** in a 75-year-old with progressive memory decline points to a neurodegenerative process.
- Orientation remains intact in early-to-moderate dementia, which doesn't rule out the diagnosis.
- The stressor (husband's death) may have unmasked or accelerated symptom recognition but doesn't explain the cognitive deficits.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, which are not evident in this presentation.
- Personality disorders are lifelong patterns, not new-onset conditions in elderly patients with cognitive decline.
- Does not explain the objective cognitive deficits on MMSE.
*Schizophrenia*
- Schizophrenia typically has onset in **late adolescence to early adulthood**, not at age 75.
- While late-onset schizophrenia exists, the **prominent cognitive impairment** (memory, executive function) as the PRIMARY feature points toward dementia rather than a primary psychotic disorder.
- Schizophrenia would show more pervasive psychotic symptoms without the specific pattern of memory and executive dysfunction seen here.
*Delirium*
- Delirium has **acute onset** (hours to days) with **fluctuating consciousness** and altered attention.
- This patient is **oriented to person, time, and place** and has a gradual, progressive course (misplacing items over time).
- No mention of acute medical illness, medication changes, or rapid cognitive fluctuation.
*Schizoid personality disorder*
- A lifelong pattern of **social detachment** and restricted emotional expression, not a new condition in late life.
- Does not explain the cognitive impairment, memory deficits, or delusional beliefs.
- The patient's reclusiveness is reactive to recent loss and concerns about theft, not a longstanding personality trait.
Symptom-based differential diagnosis approach US Medical PG Question 5: A 72-year-old woman comes to the emergency department 4 hours after the sudden onset of a diffuse, dull, throbbing headache. During this time, she also reports blurred vision, nausea, and one episode of vomiting. She has a history of hypertension and type 2 diabetes mellitus. Her medications include hydrochlorothiazide, lisinopril, atorvastatin, and metformin. She has smoked 1 pack of cigarettes daily for the past 30 years and drinks 1–2 glasses of wine per day. Her temperature is 36.6 °C (97.9 °F), pulse is 90/min, respirations are 14/min, and blood pressure is 185/110 mm Hg. Fundoscopic examination shows bilateral blurring of the optic disc margins. Physical and neurologic examinations show no other abnormalities. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Urinalysis shows 2+ protein but no WBCs or RBCs. Which of the following is the most likely diagnosis?
- A. Ischemic stroke
- B. Hypertensive emergency (Correct Answer)
- C. Transient ischemic attack
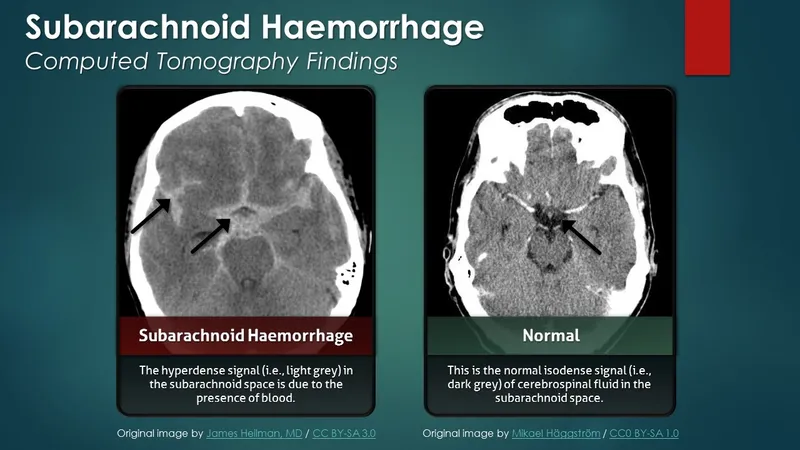
- D. Subarachnoid hemorrhage
- E. Idiopathic intracranial hypertension
Symptom-based differential diagnosis approach Explanation: ***Hypertensive emergency***
- The patient presents with **sudden onset of severe headache**, blurred vision, nausea, and vomiting, along with **markedly elevated blood pressure (185/110 mm Hg)** which are classic symptoms of hypertensive emergency.
- **Bilateral blurring of the optic disc margins (papilledema)** indicates end-organ damage to the central nervous system due to severe hypertension, further supporting this diagnosis.
*Ischemic stroke*
- While a cerebral infarct can cause sudden-onset headache, it typically presents with **focal neurological deficits**, which are absent in this patient.
- The symptoms described are more consistent with generalized intracranial pressure elevation rather than a localized ischemic event.
*Transient ischemic attack*
- A TIA involves **transient neurological deficits** that resolve completely, typically within an hour, and would not usually be associated with persistent symptoms like blurred vision and papilledema.
- The significant and sustained elevation in blood pressure with end-organ damage points away from a TIA.
*Subarachnoid hemorrhage*
- Often causes a **"thunderclap" headache** described as the worst headache of one's life, which is more severe and abrupt than the "dull, throbbing" headache mentioned.
- While it can cause nausea and vomiting, the absence of meningeal signs or focal neurological deficits, and the presence of severe uncontrolled hypertension with papilledema, make subarachnoid hemorrhage less likely.
*Idiopathic intracranial hypertension*
- This condition typically affects young, obese women and is characterized by symptoms of **increased intracranial pressure (headache, vision changes, papilledema)**, but without an identifiable cause.
- The patient's age (72 years), history of uncontrolled hypertension, and very high blood pressure suggest a secondary cause for her intracranial hypertension, specifically a hypertensive emergency.
Symptom-based differential diagnosis approach US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Symptom-based differential diagnosis approach Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Symptom-based differential diagnosis approach US Medical PG Question 7: A 55-year-old woman presents to the emergency department with retrosternal pain that started this evening. The patient states that her symptoms started as she was going to bed after taking her medications. She describes the pain as sudden in onset, worse with swallowing, and not associated with exertion. The patient has a past medical history of diabetes, anemia, and congestive heart failure and is currently taking metoprolol, insulin, metformin, iron, and lisinopril. Her temperature is 99.2°F (37.3°C), blood pressure is 125/63 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 100% on room air. Physical exam is notable for an obese woman who appears uncomfortable. An initial electrocardiogram (ECG) demonstrates sinus rhythm, and a set of troponins are pending. Which of the following is the most likely diagnosis?
- A. Spontaneous pneumothorax
- B. Myocardial infarction
- C. Esophageal rupture
- D. Pulmonary embolism
- E. Esophagitis (Correct Answer)
Symptom-based differential diagnosis approach Explanation: ***Esophagitis***
- The patient's presentation with **sudden onset retrosternal pain** that is **worse with swallowing** (odynophagia) shortly after taking medications and going to bed strongly suggests **pill-induced esophagitis**.
- Medications, especially those that are acidic or poorly dissolved like iron supplements (which the patient is taking), can cause direct mucosal injury if they remain in contact with the esophageal lining for too long.
*Spontaneous pneumothorax*
- This typically presents with **sudden onset pleuritic chest pain** and **shortness of breath**, often accompanied by ipsilateral diminished breath sounds.
- The patient's pain is described as worse with swallowing, not breathing, and there is no mention of respiratory distress or physical exam findings consistent with a pneumothorax.
*Myocardial infarction*
- While retrosternal pain is a hallmark, MI pain is typically described as **pressure-like** or **squeezing**, often **radiating** to the arm, neck, or jaw, and is usually **exertion-related**.
- The patient's pain is sudden, worse with swallowing, and specifically *not* associated with exertion, and her ECG is currently stable.
*Esophageal rupture*
- This is a catastrophic event usually presenting with **severe, acute, excruciating chest pain**, often following forceful vomiting, retching, or iatrogenic injury.
- While it causes odynophagia and retrosternal pain, the patient's symptoms are less severe, and there are no signs of mediastinitis or sepsis typically seen with rupture.
*Pulmonary embolism*
- A PE usually presents with **sudden onset dyspnea**, **pleuritic chest pain**, and sometimes **hemoptysis**.
- The patient's pain is primarily linked to swallowing and not described as pleuritic, and her oxygen saturation is 100% on room air, making PE less likely.
Symptom-based differential diagnosis approach US Medical PG Question 8: A 43-year-old woman presents to the neurology clinic in significant pain. She reports a sharp, stabbing electric-like pain on the right side of her face. The pain started suddenly 2 weeks ago. The pain is so excruciating that she can no longer laugh, speak, or eat her meals as these activities cause episodes of pain. She had to miss work last week as a result. Her attacks last about 3 minutes and go away when she goes to sleep. She typically has 2–3 attacks per day now. The vital signs include: blood pressure 132/84 mm Hg, heart rate 79/min, and respiratory rate 14/min. A neurological examination shows no loss of crude touch, tactile touch, or pain sensations on the right side of the face. The pupillary light and accommodation reflexes are normal. There is no drooping of her mouth, ptosis, or anhidrosis noted. Which of the following is the most likely diagnosis?
- A. Atypical facial pain
- B. Cluster headache
- C. Trigeminal neuralgia (Correct Answer)
- D. Bell’s palsy
- E. Basilar migraine
Symptom-based differential diagnosis approach Explanation: ***Trigeminal neuralgia***
- The patient's presentation of sudden, sharp, stabbing, electric-shock-like pain on one side of the face, triggered by activities like speaking, eating, and laughing, is highly characteristic of **trigeminal neuralgia**.
- The attacks are typically brief (lasting seconds to minutes), severe, and can cause significant functional impairment, consistent with the patient's report of missed work and inability to eat or speak.
*Atypical facial pain*
- This condition involves persistent, aching, or burning facial pain without clear neurological deficits, and it often does not have the paroxysmal, electric-shock quality seen in trigeminal neuralgia.
- Unlike **trigeminal neuralgia**, atypical facial pain is usually continuous rather than episodic and is not typically triggered by specific activities.
*Cluster headache*
- Characterized by severe, unilateral pain, often periorbital or temporal, accompanied by autonomic symptoms such as **lacrimation, conjunctival injection, nasal congestion, rhinorrhea, sweating, miosis, ptosis, and eyelid edema**.
- While very painful, the pain quality is usually deep and boring, not typically described as sharp, electric-shock like, and it is not triggered by facial movements like eating or speaking.
*Bell’s palsy*
- This condition involves **acute unilateral facial weakness or paralysis** due to inflammation of the facial nerve (CN VII), not pain as the primary symptom.
- While some patients may experience mild pain around the ear, the hallmark is facial muscle weakness leading to drooping of the mouth and inability to close the eye, which are absent in this patient.
*Basilar migraine*
- A rare type of migraine with aura symptoms originating from the brainstem, including **vertigo, dysarthria, tinnitus, bilateral visual symptoms, ataxia, and sometimes decreased level of consciousness**.
- While it can cause severe headache, it does not typically present with the described electric-shock-like facial pain triggered by movement, and the neurological examination did not reveal brainstem symptoms.
Symptom-based differential diagnosis approach US Medical PG Question 9: A previously healthy 33-year-old woman comes to the physician because of pain and sometimes numbness in her right thigh for the past 2 months. She reports that her symptoms are worse when walking or standing and are better while sitting. Three months ago, she started going to a fitness class a couple times a week. She is 163 cm (5 ft 4 in) tall and weighs 88 kg (194 lb); BMI is 33.1 kg/m2. Her vital signs are within normal limits. Examination of the skin shows no abnormalities. Sensation to light touch is decreased over the lateral aspect of the right anterior thigh. Muscle strength is normal. Tapping the right inguinal ligament leads to increased numbness of the affected thigh. The straight leg test is negative. Which of the following is the most appropriate next step in management of this patient?
- A. Advise patient to wear looser pants (Correct Answer)
- B. Reduction of physical activity
- C. MRI of the lumbar spine
- D. X-ray of the hip
- E. Blood work for inflammatory markers
Symptom-based differential diagnosis approach Explanation: ***Advise patient to wear looser pants***
- This patient presents with symptoms consistent with **meralgia paresthetica**, a condition caused by compression of the **lateral femoral cutaneous nerve (LFCN)**. Modifying clothing or belts that compress the inguinal ligament can relieve pressure on the nerve.
- Her increased weight, a recent increase in physical activity, and a positive Tinel's sign at the inguinal ligament (tapping leads to increased numbness) support this diagnosis.
*Reduction of physical activity*
- While excessive physical activity can contribute to meralgia paresthetica, simply reducing it without addressing the underlying compression might not fully resolve symptoms.
- The patient has recently increased physical activity, which could be a contributing factor, but it's not the primary or most direct intervention for nerve compression.
*MRI of the lumbar spine*
- An MRI of the lumbar spine would be considered if there were signs of **radiculopathy** or other spinal pathology, such as weakness, reflex changes, or a positive straight leg test, which are absent here.
- The symptoms are localized to the distribution of the LFCN, and the physical exam points away from a central spinal cause.
*X-ray of the hip*
- An X-ray of the hip would be indicated for suspected **hip joint pathology** or **bony abnormalities**, which are not suggested by the patient's symptoms (pain and numbness in the thigh, not hip joint pain).
- Meralgia paresthetica is a nerve entrapment syndrome, not a structural issue of the hip joint.
*Blood work for inflammatory markers*
- Inflammatory markers like **ESR** or **CRP** would be relevant if an **inflammatory arthritis**, infection, or systemic inflammatory condition was suspected, but the patient's symptoms are purely neurological and localized.
- There is no clinical evidence of inflammation, fever, or joint swelling to suggest an underlying inflammatory process.
Symptom-based differential diagnosis approach US Medical PG Question 10: A 27-year-old woman presents to her primary care physician for minor aches and pains in her bones and muscles. She states that these symptoms have persisted throughout her entire life but have worsened recently when she moved to attend college. The patient is physically active, and states that she eats a balanced diet. She is currently a full-time student and is sexually active with 1 partner. She states that she has been particularly stressed lately studying for final exams and occasionally experiences diarrhea. She has been taking acyclovir for a dermatologic herpes simplex virus infection with minimal improvement. On physical exam, the patient exhibits 4/5 strength in her upper and lower extremities, and diffuse tenderness over her limbs that is non-specific. Laboratory values are ordered as seen below:
Serum:
Na+: 144 mEq/L
Cl-: 102 mEq/L
K+: 4.7 mEq/L
HCO3-: 24 mEq/L
Ca2+: 5.0
Urea nitrogen: 15 mg/dL
Glucose: 81 mg/dL
Creatinine: 1.0 mg/dL
Alkaline phosphatase: 225 U/L
Aspartate aminotransferase (AST, GOT): 11 U/L
Alanine aminotransferase (ALT, GPT): 15 U/L
Which of the following is most likely associated with this patient’s presentation?
- A. Vitamin D deficiency (Correct Answer)
- B. Fibromyalgia
- C. Primary hyperparathyroidism
- D. Chronic fatigue syndrome
- E. Systemic lupus erythematosus
Symptom-based differential diagnosis approach Explanation: ***Correct: Vitamin D deficiency***
- The patient presents with the **classic biochemical findings of vitamin D deficiency**: **severe hypocalcemia (Ca2+ 5.0 mg/dL, normal 8.5-10.5)** and **elevated alkaline phosphatase (225 U/L)**.
- **Clinical features of osteomalacia** are present: diffuse bone and muscle pain, proximal muscle weakness (4/5 strength in extremities), and bone tenderness—all consistent with bone demineralization and secondary myopathy.
- **Risk factor identified**: Recent move to college may represent lifestyle changes including reduced sun exposure, dietary changes, or increased indoor time studying.
- The elevated alkaline phosphatase reflects increased osteoblastic activity attempting to compensate for undermineralized bone matrix.
- Severe vitamin D deficiency also impairs immune function, which may explain the herpes simplex infection with poor response to acyclovir.
*Incorrect: Chronic fatigue syndrome*
- Chronic fatigue syndrome (CFS) is a **diagnosis of exclusion** characterized by persistent unexplained fatigue for at least 6 months with **normal laboratory findings**.
- This patient has **significant biochemical abnormalities** (severe hypocalcemia, elevated alkaline phosphatase) that exclude CFS and point to a specific metabolic disorder.
- CFS does not cause hypocalcemia, elevated alkaline phosphatase, or objective muscle weakness on examination.
*Incorrect: Fibromyalgia*
- While fibromyalgia presents with widespread musculoskeletal pain, it is characterized by **normal laboratory studies** including normal calcium and alkaline phosphatase.
- The patient's severe hypocalcemia and elevated alkaline phosphatase exclude fibromyalgia as the primary diagnosis.
- Fibromyalgia typically requires identification of specific tender points on examination, which are not described here.
*Incorrect: Systemic lupus erythematosus*
- SLE typically presents with **multisystem involvement** including malar rash, photosensitivity, serositis, nephritis, and hematologic abnormalities.
- Laboratory findings would show **positive autoantibodies** (ANA, anti-dsDNA, anti-Smith), not isolated hypocalcemia with elevated alkaline phosphatase.
- The patient's normal liver and kidney function, absence of systemic features, and specific biochemical pattern do not support SLE.
*Incorrect: Primary hyperparathyroidism*
- Primary hyperparathyroidism is defined by **hypercalcemia** with elevated or inappropriately normal PTH levels.
- This patient has **severe hypocalcemia (Ca2+ 5.0)**, which is the **opposite** of what occurs in hyperparathyroidism.
- The biochemical pattern (low calcium, high alkaline phosphatase) is consistent with hypoparathyroidism or vitamin D deficiency, not hyperparathyroidism.
More Symptom-based differential diagnosis approach US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.