Probability ranking in differentials US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Probability ranking in differentials. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Probability ranking in differentials US Medical PG Question 1: A group of gastroenterologists is concerned about low colonoscopy screening rates. They decide to implement a free patient navigation program to assist local residents and encourage them to obtain colonoscopies in accordance with U.S. Preventive Services Task Force (USPSTF) guidelines. Local residents were recruited at community centers. Participants attended monthly meetings with patient navigators and were regularly reminded that their adherence to screening guidelines was being evaluated. Colonoscopy screening rates were assessed via chart review, which showed that 90% of participants adhered to screening guidelines. Data collected via chart review for local residents recruited at community centers who did not participate in the free patient navigation system found that 34% of that population adhered to USPSTF guidelines. Which of the following has most likely contributed to the observed disparity in colonoscopy screening rates?
- A. Recall bias
- B. Confirmation bias
- C. Reporting bias
- D. Hawthorne effect (Correct Answer)
- E. Sampling bias
Probability ranking in differentials Explanation: ***Hawthorne effect***
- The **Hawthorne effect** is a type of reactivity in which individuals modify an aspect of their behavior in response to their awareness of being observed.
- In this study, participants were aware that their adherence to screening guidelines was being evaluated, likely leading to increased compliance simply due to this awareness rather than the efficacy of the patient navigation program alone.
*Recall bias*
- **Recall bias** occurs when participants disproportionately remember or inaccurately recall past events, often due to their current health status or beliefs.
- This bias is less likely here as colonoscopy screening rates were assessed via **chart review**, an objective measure, rather than participant self-report.
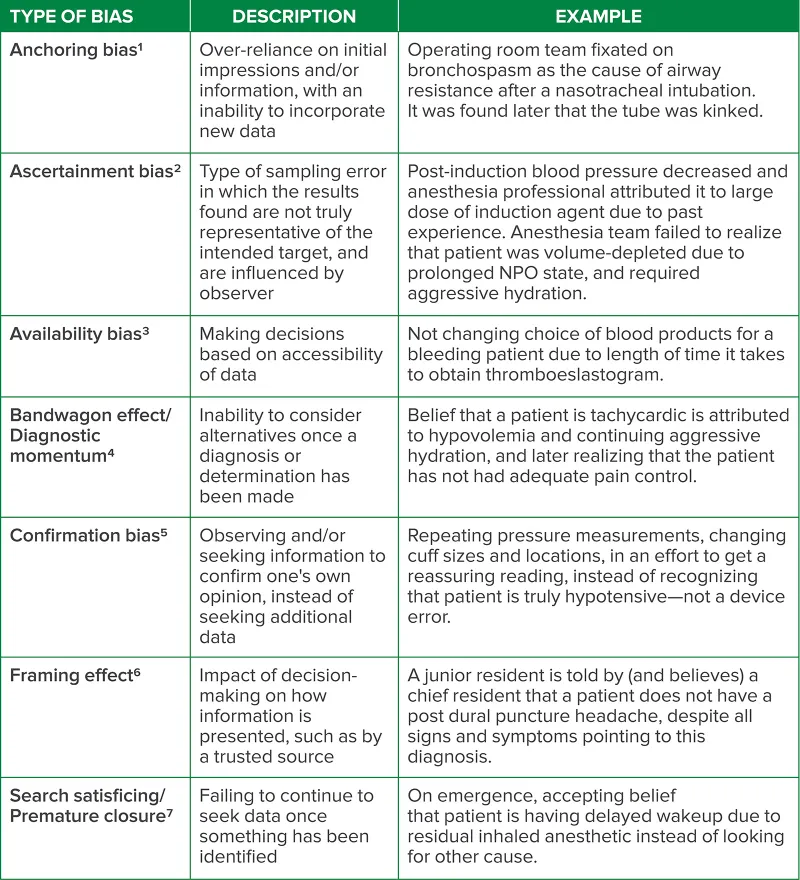
*Confirmation bias*
- **Confirmation bias** is the tendency to search for, interpret, favor, and recall information in a way that confirms one's preexisting beliefs or hypotheses.
- This bias typically affects the researchers or observers, not the participants' behavior in the observed manner, as the question focuses on the participants' increased screening rates.
*Reporting bias*
- **Reporting bias** refers to selective revealing or suppression of information during the reporting of research findings, and can occur when study participants selectively report symptoms or behaviors.
- While participants might selectively report, the data here was gathered through **chart review**, which is a more objective measure of actual behavior, making reporting bias less likely to explain the disparity in screening rates.
*Sampling bias*
- **Sampling bias** occurs when a sample is not representative of the population from which it is drawn, leading to skewed results.
- While there might be some sampling bias in who chose to participate in the free program, the observed disparity is specifically about behavior change in those *being observed*, pointing more strongly to the Hawthorne effect.
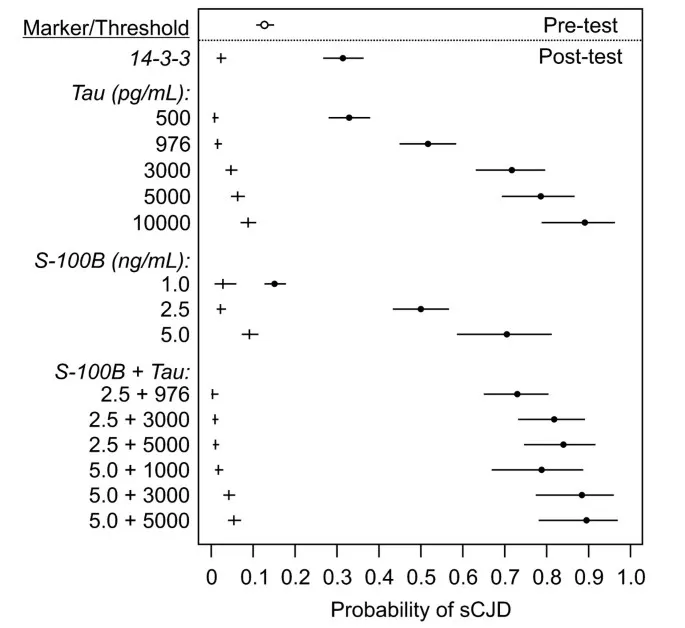
Probability ranking in differentials US Medical PG Question 2: A 14-month-old Caucasian boy is admitted to the pediatric clinic with an 8-month history of diarrhea, abdominal tenderness and concomitant failure to thrive. One of the possibilities that may cause these symptoms is Crohn’s disease, and on the basis of the attending pediatrician’s experience, the pre-test probability of this diagnosis was estimated at 40%. According to Fagan’s diagram (picture), if the likelihood ratio of a negative test result (LR-) is 0.04, what is the chance that this is the right diagnosis?
- A. 2.5% (Correct Answer)
- B. 25%
- C. 97.5%
- D. 40%
- E. 75%
Probability ranking in differentials Explanation: ***2.5%***
- To use **Fagan's nomogram**, draw a line connecting the **pre-test probability** (40%) on the left axis to the **likelihood ratio (LR-)** (0.04) on the middle axis.
- The point where this line intersects the **post-test probability** axis on the right provides the answer, which is approximately **2.5%**.
*25%*
- This value would result from a much higher LR- or a different pre-test probability, not matching the given parameters.
- If the LR- was significantly higher, like around 0.5, with the same pre-test probability, the post-test probability could be closer to 25%.
*97.5%*
- This high post-test probability would only occur with a strong **positive likelihood ratio (LR+)** and a high pre-test probability, indicating a very strong confirmation of the diagnosis.
- A **negative test result (LR-)** should decrease, not increase, the probability of the diagnosis.
*40%*
- This is the **pre-test probability**, not the post-test probability after incorporating the test result.
- The result of a diagnostic test (especially a negative one with a low LR-) should change the probability, so the post-test probability cannot be the same as the pre-test probability unless the LR is 1.
*75%*
- A post-test probability of 75% would indicate a significant increase in the likelihood of the disease, usually associated with a high **LR+** from a positive test result.
- This value is inconsistent with a negative test result and an LR- of 0.04, which should decrease the probability.
Probability ranking in differentials US Medical PG Question 3: A 17-year-old man is brought by his mother to his pediatrician in order to complete medical clearance forms prior to attending college. During the visit, his mother asks about what health risks he should be aware of in college. Specifically, she recently saw on the news that some college students were killed by a fatal car crash. She therefore asks about causes of death in this population. Which of the following is true about the causes of death in college age individuals?
- A. More of them die from homicide than suicide
- B. More of them die from suicide than injuries
- C. More of them die from cancer than suicide
- D. More of them die from homicide than injuries
- E. More of them die from homicide than cancer (Correct Answer)
Probability ranking in differentials Explanation: ***More of them die from homicide than cancer***
- While relatively rare, **homicide rates** for college-aged individuals (18-24 years) are generally higher than their rates of death due to **cancer**.
- **Cancer** is a leading cause of death in older populations but is much less common in young adults.
*More of them die from homicide than suicide*
- **Suicide** is a significantly more common cause of death than homicide among college-aged individuals.
- Data consistently shows that **suicide** ranks as one of the top causes of death in this demographic, often second only to unintentional injuries.
*More of them die from suicide than injuries*
- **Unintentional injuries** (including motor vehicle accidents, accidental poisoning, and falls) are the leading cause of death in the 18-24 age group.
- **Suicide** is typically the second leading cause, meaning more individuals die from injuries than from suicide.
*More of them die from cancer than suicide*
- As mentioned, **suicide** is a much more prevalent cause of death in young adults than cancer.
- **Cancer deaths** are relatively uncommon in this age group compared to other causes like injuries and suicide.
*More of them die from homicide than injuries*
- **Unintentional injuries** are the leading cause of death among college-aged individuals.
- **Homicide rates** are considerably lower than injury rates in this population.
Probability ranking in differentials US Medical PG Question 4: A medical research study is beginning to evaluate the positive predictive value of a novel blood test for non-Hodgkin’s lymphoma. The diagnostic arm contains 700 patients with NHL, of which 400 tested positive for the novel blood test. In the control arm, 700 age-matched control patients are enrolled and 0 are found positive for the novel test. What is the PPV of this test?
- A. 400 / (400 + 0) (Correct Answer)
- B. 700 / (700 + 300)
- C. 400 / (400 + 300)
- D. 700 / (700 + 0)
- E. 700 / (400 + 400)
Probability ranking in differentials Explanation: ***400 / (400 + 0) = 1.0 or 100%***
- The **positive predictive value (PPV)** is calculated as **True Positives / (True Positives + False Positives)**.
- In this scenario, **True Positives (TP)** are the 400 patients with NHL who tested positive, and **False Positives (FP)** are 0, as no control patients tested positive.
- This gives a PPV of 400/400 = **1.0 or 100%**, indicating that all patients who tested positive actually had the disease.
*700 / (700 + 300)*
- This calculation does not align with the formula for PPV based on the given data.
- The denominator `(700+300)` suggests an incorrect combination of various patient groups.
*400 / (400 + 300)*
- The denominator `(400+300)` incorrectly includes 300, which is the number of **False Negatives** (patients with NHL who tested negative), not False Positives.
- PPV focuses on the proportion of true positives among all positive tests, not all diseased individuals.
*700 / (700 + 0)*
- This calculation incorrectly uses the total number of patients with NHL (700) as the numerator, rather than the number of positive test results in that group.
- The numerator should be the **True Positives** (400), not the total number of diseased individuals.
*700 / (400 + 400)*
- This calculation uses incorrect values for both the numerator and denominator, not corresponding to the PPV formula.
- The numerator 700 represents the total number of patients with the disease, not those who tested positive, and the denominator incorrectly sums up values that don't represent the proper PPV calculation.
Probability ranking in differentials US Medical PG Question 5: A pharmaceutical corporation is developing a research study to evaluate a novel blood test to screen for breast cancer. They enrolled 800 patients in the study, half of which have breast cancer. The remaining enrolled patients are age-matched controls who do not have the disease. Of those in the diseased arm, 330 are found positive for the test. Of the patients in the control arm, only 30 are found positive. What is this test’s sensitivity?
- A. 330 / (330 + 30)
- B. 330 / (330 + 70) (Correct Answer)
- C. 370 / (30 + 370)
- D. 370 / (70 + 370)
- E. 330 / (400 + 400)
Probability ranking in differentials Explanation: ***330 / (330 + 70)***
- **Sensitivity** measures the proportion of actual **positives** that are correctly identified as such.
- In this study, there are **400 diseased patients** (half of 800). Of these, 330 tested positive (true positives), meaning 70 tested negative (false negatives). So sensitivity is **330 / (330 + 70)**.
*330 / (330 + 30)*
- This calculation represents the **positive predictive value**, which is the probability that subjects with a positive screening test truly have the disease. It uses **true positives / (true positives + false positives)**.
- It does not correctly calculate **sensitivity**, which requires knowing the total number of diseased individuals.
*370 / (30 + 370)*
- This expression is attempting to calculate **specificity**, which is the proportion of actual negatives that are correctly identified. It would be **true negatives / (true negatives + false positives)**.
- However, the numbers used are incorrect for specificity in this context given the data provided.
*370 / (70 + 370)*
- This formula is an incorrect combination of values and does not represent any standard epidemiological measure like **sensitivity** or **specificity**.
- It is attempting to combine false negatives (70) and true negatives (370 from control arm) in a non-standard way.
*330 / (400 + 400)*
- This calculation attempts to divide true positives by the total study population (800 patients).
- This metric represents the **prevalence of true positives within the entire study cohort**, not the test's **sensitivity**.
Probability ranking in differentials US Medical PG Question 6: A 57-year-old man presents to the emergency department for weight loss and abdominal pain. The patient states that he has felt steadily more fatigued over the past month and has lost 22 pounds without effort. Today, he fainted prompting his presentation. The patient has no significant past medical history. He does have a 33 pack-year smoking history and drinks 4 to 5 alcoholic drinks per day. His temperature is 99.5°F (37.5°C), blood pressure is 100/58 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you see a patient who is very thin and appears to be pale. Stool fecal occult blood testing is positive. A CT scan of the abdomen is performed demonstrating a mass in the colon with multiple metastatic lesions scattered throughout the abdomen. The patient is informed of his diagnosis of metastatic colon cancer. When the patient conveys the information to his family he focuses his efforts on discussing the current literature in the field and the novel therapies that have been invented. He demonstrates his likely mortality outcome which he calculated using the results of a large multi-center study. Which of the following is this patient most likely demonstrating?
- A. Intellectualization (Correct Answer)
- B. Dissociation
- C. Rationalization
- D. Optimism
- E. Pessimism
Probability ranking in differentials Explanation: ***Intellectualization***
- This defense mechanism involves **focusing on the intellectual aspects** of a stressful situation, using logical reasoning and factual analysis to avoid experiencing distressing emotions.
- The patient demonstrates this by discussing **literature, novel therapies, and mortality statistics** regarding his metastatic colon cancer.
*Dissociation*
- **Dissociation** involves a mental process that causes a lack of connection in a person's thoughts, memory, and sense of identity.
- This patient is actively engaging with the information, not disconnecting from it.
*Rationalization*
- **Rationalization** is creating logical but false explanations for unacceptable thoughts, feelings, or behaviors to justify them.
- The patient is not trying to justify his actions or feelings, but rather to understand his disease intellectually.
*Optimism*
- **Optimism** is a disposition to look on the favorable side of events or conditions and to expect the most favorable outcome.
- While hope for novel therapies could be seen as optimistic, his detailed calculation of mortality outcomes is a realistic, rather than purely optimistic, approach.
*Pessimism*
- **Pessimism** is a tendency to see the worst aspect of things or believe that the worst will happen.
- The patient is engaging with the facts of his diagnosis, even calculating his mortality outcome, which is not necessarily a pessimistic but rather a realistic and intellectual approach.
Probability ranking in differentials US Medical PG Question 7: A female presents with a 1 × 1 cm thyroid swelling. What is the next best step in management?
- A. I-131
- B. TSH (Correct Answer)
- C. TSH & T4
- D. T3 & T4
- E. FNAC
Probability ranking in differentials Explanation: ***Correct Option: TSH***
- **Thyroid-stimulating hormone (TSH)** is the most sensitive initial test to assess thyroid function when a thyroid nodule is discovered.
- An abnormal TSH level (either high or low) can guide further investigation into whether the nodule is associated with a functional thyroid disorder.
- **TSH should be the first test** according to American Thyroid Association guidelines for thyroid nodule evaluation.
*Incorrect Option: I-131*
- **I-131 (radioactive iodine therapy)** is a treatment modality for hyperthyroidism or thyroid cancer, not a diagnostic step for initial thyroid swelling evaluation.
- Administering I-131 before assessing thyroid function would be inappropriate and could lead to unnecessary or harmful intervention.
*Incorrect Option: TSH & T4*
- While TSH is crucial, adding **T4 (thyroxine)** as an initial step is often not necessary if TSH is normal, as TSH alone effectively screens for primary thyroid dysfunction.
- Measuring both TSH and T4 is typically reserved for situations where TSH is abnormal or when central hypothyroidism is suspected.
*Incorrect Option: T3 & T4*
- Measuring **T3 (triiodothyronine)** along with T4 as an initial screening for a thyroid nodule is generally not recommended.
- T3 levels are primarily used to diagnose **hyperthyroidism** or to evaluate the severity of thyrotoxicosis after an abnormal TSH and T4 have been identified.
*Incorrect Option: FNAC*
- While **Fine Needle Aspiration Cytology (FNAC)** is an essential diagnostic tool for thyroid nodules, it is typically performed after TSH assessment.
- FNAC is indicated for nodules >1 cm with suspicious ultrasound features, but **functional assessment with TSH comes first** to rule out hyperfunctioning nodules.
Probability ranking in differentials US Medical PG Question 8: What is the most appropriate initial investigation for a solitary thyroid nodule (STN)?
- A. I-123 scan
- B. Ultrasound (Correct Answer)
- C. Fine-needle aspiration (FNA) biopsy
- D. Thyroid function tests (TFTs)
- E. CT scan of the neck
Probability ranking in differentials Explanation: ***Ultrasound***
- **Ultrasound** is the initial investigation of choice for a solitary thyroid nodule (STN) because it can differentiate between **solid, cystic, or mixed lesions**, assess nodule size, and identify suspicious features (e.g., microcalcifications, irregular margins, internal vascularity).
- It also helps to determine if there are other nodules not palpable on physical examination, allowing for a more complete assessment of the **thyroid gland**.
*Fine-needle aspiration (FNA) biopsy*
- **FNA biopsy** is the most accurate diagnostic tool for evaluating the malignant potential of a thyroid nodule, but it is typically performed *after* an initial ultrasound has characterized the nodule.
- It requires guidance (often by ultrasound) to obtain an adequate sample for cytological analysis, making ultrasound a prerequisite for optimal FNA performance.
*Thyroid function tests (TFTs)*
- **TFTs (TSH, T3, T4)** are important for assessing the functional status of the thyroid gland (e.g., hyperthyroidism or hypothyroidism) and can provide context for the nodule.
- However, TFTs do not directly evaluate the **morphology or malignant potential** of the nodule itself, making them less appropriate as an initial, stand-alone investigation for an STN.
*I-123 scan*
- An **I-123 scan** (radioactive iodine uptake and scan) is used to determine if a nodule is "hot" (hyperfunctioning/benign) or "cold" (non-functioning/potentially malignant).
- It is typically reserved for cases where **TSH levels are suppressed**, suggesting a hyperfunctioning nodule, and is not the first-line imaging modality for initial characterization of all STNs.
*CT scan of the neck*
- **CT scan** can visualize thyroid nodules and assess for extrathyroidal extension or lymphadenopathy, but it is **not recommended as an initial investigation** for STN.
- It involves **radiation exposure**, is more expensive than ultrasound, and provides **less detailed characterization** of nodule morphology compared to ultrasound, making it a less appropriate first-line modality.
Probability ranking in differentials US Medical PG Question 9: A young patient presents to the OPD with recurrent colicky abdominal pain. Urine examination shows the presence of red blood cells (RBCs) and the following crystal shape in the figure. What is the most likely diagnosis?
- A. Cystine stone (Correct Answer)
- B. Glomerulonephritis
- C. Oxalate stone
- D. Polycystic kidney disease
- E. Uric acid stone
Probability ranking in differentials Explanation: ***Cystine stone***
- The image displays classic **hexagonal** crystals, which are pathognomonic for **cystine stones**.
- Recurrent colicky abdominal pain in a young patient with hematuria (RBCs in urine) is highly suggestive of **nephrolithiasis** (kidney stones), and the crystal morphology confirms cystine as the cause.
- Cystine stones are associated with **cystinuria**, an autosomal recessive disorder causing defective renal tubular reabsorption of cystine.
*Glomerulonephritis*
- While glomerulonephritis can cause hematuria, the presence of **hexagonal crystals** in the urine is not a feature of this condition.
- Glomerulonephritis typically involves **dysmorphic RBCs** and **RBC casts** in the urine, not hexagonal crystals.
*Oxalate stone*
- **Calcium oxalate crystals** typically appear as **envelope-shaped (dihydrate)** or **dumbbell-shaped (monohydrate)**.
- While oxalate stones are the most common cause of kidney stones and colicky pain, their crystal morphology is distinct from the hexagonal shape seen here.
*Polycystic kidney disease*
- Polycystic kidney disease is a genetic disorder characterized by **multiple cysts** in the kidneys, which can cause pain and hematuria.
- However, it does **not** typically present with specific crystal shapes like those shown in the image, as the primary pathology is structural, not related to crystal formation.
*Uric acid stone*
- **Uric acid crystals** typically appear as **rhomboid or diamond-shaped** crystals, often with a yellow-brown color.
- While uric acid stones can cause similar symptoms (colicky pain, hematuria), the crystal morphology is distinctly different from the hexagonal cystine crystals shown in the image.
- Uric acid stones are associated with **hyperuricemia**, **low urine pH**, and conditions like gout.
Probability ranking in differentials US Medical PG Question 10: An 11-year-old boy is brought to the emergency department 30 minutes after he was found screaming and clutching his head. He has had nausea and occasional episodes of vomiting for 1 week, fever and left-sided headaches for 2 weeks, and increasing tooth pain over the past 3 weeks. He has no history of ear or sinus infections. He is in moderate distress. His temperature is 38.7°C (101.7°F), pulse is 170/min, respirations are 19/min, and blood pressure is 122/85 mmHg. He is confused and only oriented to person. The pupils react sluggishly to light. Fundoscopic examination shows papilledema bilaterally. Extraocular movements are normal. Flexion of the neck causes hip flexion. Which of the following is the most likely diagnosis?
- A. Subarachnoid hemorrhage
- B. Cavernous sinus thrombosis
- C. Pyogenic brain abscess (Correct Answer)
- D. HSV encephalitis
- E. Medulloblastoma
Probability ranking in differentials Explanation: ***Pyogenic brain abscess***
- The patient's history of **increasing tooth pain** over three weeks, followed by fever, headache, nausea, vomiting, confusion, and **papilledema**, strongly suggests a pyogenic brain abscess originating from a dental infection.
- **Brudzinski's sign** (nuchal rigidity with **hip flexion upon neck flexion**) indicates meningeal irritation, and confusion with sluggish pupillary reaction are signs of increased intracranial pressure, consistent with an expanding mass lesion and inflammation.
*Subarachnoid hemorrhage*
- While it can cause sudden severe headache ("thunderclap"), nausea, vomiting, and meningeal signs, the **subacute onset** of symptoms (weeks) and the presence of prior dental pain make this diagnosis less likely.
- **Fever** with prolonged, progressive symptoms and signs of focal neurological deficits (which can be subtle like confusion and sluggish pupils) are not typical for SAH.
*Cavernous sinus thrombosis*
- This condition is typically associated with infections in the facial region or sinuses, leading to **ophthalmoplegia**, **proptosis**, and chemosis due to involvement of cranial nerves III, IV, VI, and the ophthalmic/maxillary branches of V.
- Although the patient has headache and fever, the absence of specific ocular signs like paralysis of extraocular muscles or proptosis makes this less probable.
*HSV encephalitis*
- While HSV encephalitis can cause fever, headache, altered mental status, and seizures, its onset is typically **acute to subacute** (days), and it often presents with **focal neurological deficits** or personality changes, not typically originating from dental pain.
- The preceding tooth pain and the relatively prolonged symptom timeline (weeks) are less characteristic of primary HSV encephalitis.
*Medulloblastoma*
- This is a common posterior fossa tumor in children, which can cause symptoms of increased ICP like headache, nausea, vomiting, and papilledema due to hydrocephalus.
- However, the presence of **fever** and a clear preceding **infectious source** (dental pain) points away from a primary tumor and more towards an infectious process like an abscess.
More Probability ranking in differentials US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.