Metacognition and diagnostic calibration US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metacognition and diagnostic calibration. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metacognition and diagnostic calibration US Medical PG Question 1: Two dizygotic twins present to the university clinic because they believe they are being poisoned through the school's cafeteria food. They have brought these concerns up in the past, but no other students or cafeteria staff support this belief. Both of them are average students with strong and weak subject areas as demonstrated by their course grade-books. They have no known medical conditions and are not known to abuse illicit substances. Which statement best describes the condition these patients have?
- A. A trial separation is likely to worsen symptoms.
- B. The disorder is its own disease entity in DSM-5.
- C. Antipsychotic medications are rarely beneficial.
- D. Can affect two or more closely related individuals. (Correct Answer)
- E. Cognitive behavioral therapy is a good first-line.
Metacognition and diagnostic calibration Explanation: ***Can affect two or more closely related individuals.***
- The shared delusional belief in **folie à deux**, also known as **shared psychotic disorder**, typically occurs in two or more people who are closely associated.
- In this case, the **dizygotic twins** sharing the same delusional belief about being poisoned from cafeteria food fits this pattern.
*A trial separation is likely to worsen symptoms.*
- **Separating the individuals** involved in **folie à deux** is often a crucial step in treatment, as it can help break the cycle of shared delusion and allow for individual therapy.
- Separation typically IMPROVES rather than worsens symptoms by removing the reinforcement of the shared delusion.
*The disorder is its own disease entity in DSM-5.*
- In the **DSM-5**, **folie à deux** is no longer considered a separate diagnostic category.
- Instead, it is classified under **Other Specified Schizophrenia Spectrum and Other Psychotic Disorder** or **Unspecified Schizophrenia Spectrum and Other Psychotic Disorder**, with the specific context of shared delusion noted.
*Antipsychotic medications are rarely beneficial.*
- **Antipsychotics** are actually commonly used in treating folie à deux, particularly for the **primary individual** who initially developed the delusion.
- They can be an important component of treatment, often combined with separation and psychotherapy.
*Cognitive behavioral therapy is a good first-line.*
- **Cognitive Behavioral Therapy (CBT)** can be beneficial, particularly after separation, to help individuals challenge and reframe their delusional beliefs.
- However, the **first-line intervention** for shared psychotic disorder is **separation of the involved individuals**, followed by individual therapy (which may include CBT) and medication as needed.
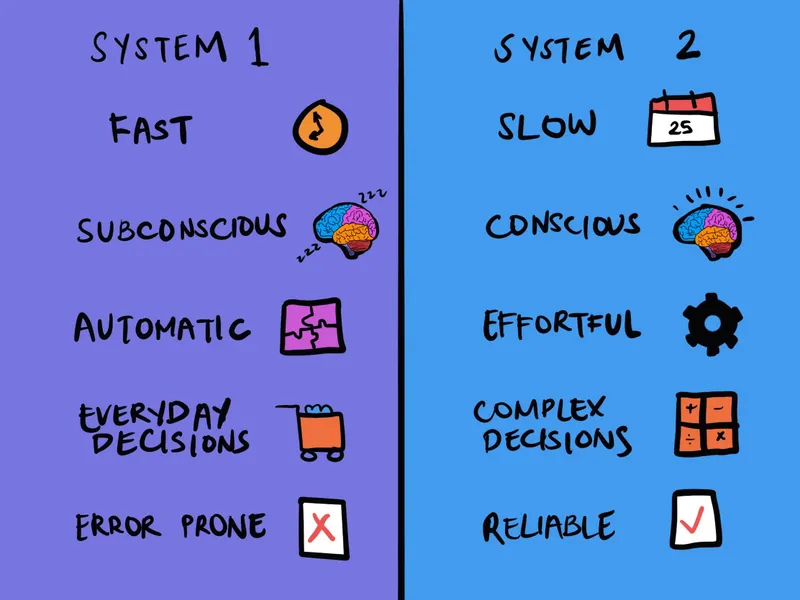
Metacognition and diagnostic calibration US Medical PG Question 2: A 52-year-old man comes to the physician because of a 3-week history of a cough and hoarseness. He reports that the cough is worse when he lies down after lunch. His temperature is 37.5°C (99.5°F); the remainder of his vital signs are within normal limits. Because the physician has recently been seeing several patients with the common cold, the diagnosis of a viral upper respiratory tract infection readily comes to mind. The physician fails to consider the diagnosis of gastroesophageal reflux disease, which the patient is later found to have. Which of the following most accurately describes the cognitive bias that the physician had?
- A. Framing
- B. Anchoring
- C. Visceral
- D. Confirmation
- E. Availability (Correct Answer)
Metacognition and diagnostic calibration Explanation: ***Availability***
- The physician recently seeing several patients with the common cold led to this diagnosis readily coming to mind, demonstrating how easily recalled examples can disproportionately influence diagnosis.
- This bias occurs when easily recalled instances or information (like recent cases of common cold) are used to estimate the likelihood or frequency of an event, even if other more relevant data exist.
*Framing*
- This bias occurs when the way information is presented (e.g., as a gain or a loss) influences a decision, rather than the intrinsic characteristics of the options themselves.
- The scenario does not involve the presentation of information in different ways to sway the physician's judgment.
*Anchoring*
- This bias involves relying too heavily on an initial piece of information (the "anchor") when making subsequent judgments, often leading to insufficient adjustment away from that anchor.
- While the physician initially considered a viral URI, the setup is more about the ease of recall influencing the decision rather than being stuck on an initial data point.
*Visceral*
- This is not a commonly recognized cognitive bias in the context of medical decision-making; "visceral" largely refers to emotional or intuitive feelings rather than a structured cognitive bias.
- Cognitive biases describe systematic patterns of deviation from norm or rationality in judgment, not merely emotional responses.
*Confirmation*
- This bias involves seeking, interpreting, favoring, and recalling information in a way that confirms one's pre-existing beliefs or hypotheses.
- The physician did not actively seek information to confirm the common cold diagnosis; rather, the diagnosis came to mind due to recent encounters, which aligns with availability bias.
Metacognition and diagnostic calibration US Medical PG Question 3: A group of gastroenterologists is concerned about low colonoscopy screening rates. They decide to implement a free patient navigation program to assist local residents and encourage them to obtain colonoscopies in accordance with U.S. Preventive Services Task Force (USPSTF) guidelines. Local residents were recruited at community centers. Participants attended monthly meetings with patient navigators and were regularly reminded that their adherence to screening guidelines was being evaluated. Colonoscopy screening rates were assessed via chart review, which showed that 90% of participants adhered to screening guidelines. Data collected via chart review for local residents recruited at community centers who did not participate in the free patient navigation system found that 34% of that population adhered to USPSTF guidelines. Which of the following has most likely contributed to the observed disparity in colonoscopy screening rates?
- A. Recall bias
- B. Confirmation bias
- C. Reporting bias
- D. Hawthorne effect (Correct Answer)
- E. Sampling bias
Metacognition and diagnostic calibration Explanation: ***Hawthorne effect***
- The **Hawthorne effect** is a type of reactivity in which individuals modify an aspect of their behavior in response to their awareness of being observed.
- In this study, participants were aware that their adherence to screening guidelines was being evaluated, likely leading to increased compliance simply due to this awareness rather than the efficacy of the patient navigation program alone.
*Recall bias*
- **Recall bias** occurs when participants disproportionately remember or inaccurately recall past events, often due to their current health status or beliefs.
- This bias is less likely here as colonoscopy screening rates were assessed via **chart review**, an objective measure, rather than participant self-report.
*Confirmation bias*
- **Confirmation bias** is the tendency to search for, interpret, favor, and recall information in a way that confirms one's preexisting beliefs or hypotheses.
- This bias typically affects the researchers or observers, not the participants' behavior in the observed manner, as the question focuses on the participants' increased screening rates.
*Reporting bias*
- **Reporting bias** refers to selective revealing or suppression of information during the reporting of research findings, and can occur when study participants selectively report symptoms or behaviors.
- While participants might selectively report, the data here was gathered through **chart review**, which is a more objective measure of actual behavior, making reporting bias less likely to explain the disparity in screening rates.
*Sampling bias*
- **Sampling bias** occurs when a sample is not representative of the population from which it is drawn, leading to skewed results.
- While there might be some sampling bias in who chose to participate in the free program, the observed disparity is specifically about behavior change in those *being observed*, pointing more strongly to the Hawthorne effect.
Metacognition and diagnostic calibration US Medical PG Question 4: A student health coordinator plans on leading a campus-wide HIV screening program that will be free for the entire undergraduate student body. The goal is to capture as many correct HIV diagnoses as possible with the fewest false positives. The coordinator consults with the hospital to see which tests are available to use for this program. Test A has a sensitivity of 0.92 and a specificity of 0.99. Test B has a sensitivity of 0.95 and a specificity of 0.96. Test C has a sensitivity of 0.98 and a specificity of 0.93. Which of the following testing schemes should the coordinator pursue?
- A. Test A on the entire student body followed by Test B on those who are positive
- B. Test A on the entire student body followed by Test C on those who are positive
- C. Test C on the entire student body followed by Test B on those who are positive
- D. Test C on the entire student body followed by Test A on those who are positive (Correct Answer)
- E. Test B on the entire student body followed by Test A on those who are positive
Metacognition and diagnostic calibration Explanation: ***Test C on the entire student body followed by Test A on those who are positive***
- To "capture as many correct HIV diagnoses as possible" (maximize true positives), the initial screening test should have the **highest sensitivity**. Test C has the highest sensitivity (0.98).
- To "capture as few false positives as possible" (maximize true negatives and confirm diagnoses), the confirmatory test should have the **highest specificity**. Test A has the highest specificity (0.99).
*Test A on the entire student body followed by Test B on those who are positive*
- Starting with Test A (sensitivity 0.92) would miss more true positive cases than starting with Test C (sensitivity 0.98), failing the goal of **capturing as many cases as possible**.
- Following with Test B (specificity 0.96) would result in more false positives than following with Test A (specificity 0.99).
*Test A on the entire student body followed by Test C on those who are positive*
- This scheme would miss many true positive cases initially due to Test A's lower sensitivity compared to Test C.
- Following with Test C would introduce more false positives than necessary, as it has a lower specificity (0.93) than Test A (0.99).
*Test C on the entire student body followed by Test B on those who are positive*
- While Test C is a good initial screen for its high sensitivity, following it with Test B (specificity 0.96) is less optimal than Test A (specificity 0.99) for minimizing false positives in the confirmation step.
- This combination would therefore yield more false positives in the confirmatory stage than using Test A.
*Test B on the entire student body followed by Test A on those who are positive*
- Test B has a sensitivity of 0.95, which is lower than Test C's sensitivity of 0.98, meaning it would miss more true positive cases at the initial screening stage.
- While Test A provides excellent specificity for confirmation, the initial screening step is suboptimal for the goal of capturing as many diagnoses as possible.
Metacognition and diagnostic calibration US Medical PG Question 5: A 67-year-old man presents to the emergency department with confusion. The patient is generally healthy, but his wife noticed him becoming progressively more confused as the day went on. The patient is not currently taking any medications and has no recent falls or trauma. His temperature is 102°F (38.9°C), blood pressure is 126/64 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a confused man who cannot participate in a neurological exam secondary to his confusion. No symptoms are elicited with flexion of the neck and jolt accentuation of headache is negative. Initial laboratory values are unremarkable and the patient's chest radiograph and urinalysis are within normal limits. An initial CT scan of the head is unremarkable. Which of the following is the best next step in management?
- A. CT angiogram of the head and neck
- B. Vancomycin, ceftriaxone, ampicillin, and dexamethasone
- C. Acyclovir (Correct Answer)
- D. PCR of the cerebrospinal fluid
- E. MRI of the head
Metacognition and diagnostic calibration Explanation: ***Acyclovir***
- This patient presents with **acute confusion and fever** without an obvious infectious source, negative meningeal signs, and normal initial imaging, highly suggestive of **herpes simplex encephalitis (HSE)**.
- HSE is a **medical emergency** with high mortality (70-80%) if untreated, but mortality drops to 20-30% with early acyclovir therapy.
- **Empiric acyclovir must be started immediately** upon clinical suspicion of HSE, **without waiting for diagnostic confirmation**.
- Standard management includes obtaining CSF for PCR **concurrently** with starting acyclovir, but treatment should never be delayed for diagnostic testing.
- The best next step in **management** is initiating acyclovir; CSF PCR is obtained for confirmation but does not delay treatment.
*PCR of the cerebrospinal fluid*
- **CSF PCR for HSV** is the gold standard **diagnostic test** for HSE with high sensitivity (96%) and specificity (99%).
- While lumbar puncture should be performed to obtain CSF for PCR, this is a **diagnostic step** that should be done **concurrently** with starting acyclovir, not instead of it.
- The question asks for best next step in **management**, not diagnosis—acyclovir therapy takes precedence.
- Delaying acyclovir while awaiting diagnostic confirmation significantly increases morbidity and mortality.
*Vancomycin, ceftriaxone, ampicillin, and dexamethasone*
- This broad-spectrum antibiotic regimen is empiric therapy for **bacterial meningitis** and should be considered in patients with fever and altered mental status.
- However, the **absence of meningeal signs** (negative nuchal rigidity, negative jolt accentuation) makes bacterial meningitis less likely.
- In practice, when HSE is suspected but bacterial meningitis cannot be excluded, both antimicrobial regimens may be initiated empirically, but the primary concern here is HSE given the clinical presentation.
*MRI of the head*
- **MRI with FLAIR sequences** is highly sensitive for HSE and typically shows **temporal lobe involvement** (especially medial temporal lobes).
- However, MRI findings may be **normal early in the disease course** (first 48-72 hours).
- MRI is useful for supporting the diagnosis but should **not delay empiric acyclovir therapy**.
- Obtaining MRI before treatment would be inappropriate given the time-sensitive nature of HSE.
*CT angiogram of the head and neck*
- CT angiography evaluates vascular structures and is indicated for suspected **stroke, aneurysm, or vascular dissection**.
- This patient lacks focal neurological deficits, signs of acute stroke, or vascular risk factors that would prioritize vascular imaging.
- The presentation with fever and diffuse encephalopathy points toward an infectious/inflammatory process rather than a vascular etiology.
Metacognition and diagnostic calibration US Medical PG Question 6: A 30-year-old computer scientist receives negative feedback on a recent project from his senior associate. He is told sternly that he must improve his performance on the next project. Later that day, he yells at his intern, a college student, for not showing enough initiative, though he had voiced only satisfaction with his performance up until this point. Which of the following psychological defense mechanisms is he demonstrating?
- A. Acting out
- B. Countertransference
- C. Projection
- D. Displacement (Correct Answer)
- E. Transference
Metacognition and diagnostic calibration Explanation: ***Displacement***
- **Displacement** is a defense mechanism where a person redirects strong emotions, especially negative ones like anger, from the original source to a substitute target that is perceived as less threatening.
- The computer scientist's anger, initially generated by criticism from his senior associate, is redirected to his intern, who is a safer target.
*Acting out*
- **Acting out** involves expressing unconscious emotional conflicts or impulses through behavior, often inappropriate or destructive, rather than through words or feelings.
- While yelling at the intern is a behavior, the primary motive here is redirecting an emotion, not expressing a hidden conflict or impulse without awareness.
*Countertransference*
- **Countertransference** refers to the therapist's emotional reactions to a patient, rooted in their own unresolved conflicts, and is specific to the therapeutic relationship.
- This scenario involves an individual's reaction to workplace stress, not a dynamic within a therapeutic setting.
*Projection*
- **Projection** is attributing one's own unacceptable thoughts, feelings, or impulses to another person.
- In this case, the computer scientist isn't attributing his own poor performance or anger to the intern; rather, he is _redirecting_ his anger.
*Transference*
- **Transference** is the unconscious redirection of feelings and attitudes from a person in the past (e.g., a parent) to a person in the present (e.g., a therapist or boss).
- This scenario involves a direct reaction to a current stressor and redirection of emotion, not the reliving of past relationship dynamics with a new figure.
Metacognition and diagnostic calibration US Medical PG Question 7: A 65-year-old man is admitted to the hospital because of a 1-month history of fatigue, intermittent fever, and weakness. Results from a peripheral blood smear taken during his evaluation are indicative of possible acute myeloid leukemia. Bone marrow aspiration and subsequent cytogenetic studies confirm the diagnosis. The physician sets aside an appointed time-slot and arranges a meeting in a quiet office to inform him about the diagnosis and discuss his options. He has been encouraged to bring someone along to the appointment if he wanted. He comes to your office at the appointed time with his daughter. He appears relaxed, with a full range of affect. Which of the following is the most appropriate opening statement in this situation?
- A. Your lab reports show that you have an acute myeloid leukemia
- B. What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies? (Correct Answer)
- C. You must be curious and maybe even anxious about the results of your tests.
- D. I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.
- E. Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?
Metacognition and diagnostic calibration Explanation: ***"What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies?"***
- This **open-ended question** allows the patient to express their current knowledge and perceptions, which helps the physician tailor the discussion.
- It establishes a **patient-centered approach**, respecting the patient's existing understanding and preparing them for further information.
*"You must be curious and maybe even anxious about the results of your tests."*
- While empathic, this statement makes an **assumption about the patient's feelings** rather than inviting them to share their own.
- It is often better to ask directly or use more open-ended questions that allow the patient to express their true emotions, especially given their **relaxed demeanor**.
*"I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.”"*
- This statement immediately introduces **overwhelming and potentially alarming information** (referral, chemotherapy, radiotherapy) without first establishing the diagnosis or assessing the patient's readiness to receive it.
- It prematurely jumps to treatment and logistics, potentially causing **unnecessary distress** before the patient has processed the core diagnosis.
*"Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?""*
- While it attempts to assess the patient's preference for information, this question is a **closed-ended "either/or" choice** that might limit the patient's ability to express nuanced needs.
- It also prematurely introduces the idea of "options" without first explaining the diagnosis in an understandable context.
*"Your lab reports show that you have an acute myeloid leukemia"*
- This is a **direct and blunt delivery of a serious diagnosis** without any preparatory context or assessment of the patient's existing knowledge or emotional state.
- Delivering such news abruptly can be shocking and overwhelming, potentially **hindering effective communication** and rapport building.
Metacognition and diagnostic calibration US Medical PG Question 8: A 53-year-old man presents with a 2-year-history of dull, nonspecific flank pain that subsides with rest. His past medical history is significant for hypertension, hypercholesterolemia, and type 2 diabetes mellitus. He has no allergies and takes no medications. His father died of kidney disease at the age of 51, and his mother has been treated for ovarian cancer. On presentation, his blood pressure is 168/98 mm Hg, and his heart rate is 102/min. Abdominal examination is significant for palpable bilateral renal masses. His laboratory tests are significant for creatinine of 2.0 mg/dL and a BUN of 22 mg/dL. Which of the following tests is most recommended in this patient?
- A. Chest X-ray
- B. Genetic testing for polycystic kidney disease
- C. CT scan of abdomen and pelvis
- D. 24-hour urine protein collection
- E. Renal ultrasound (Correct Answer)
Metacognition and diagnostic calibration Explanation: ***Renal ultrasound***
- This patient presents with classic features of **autosomal dominant polycystic kidney disease (ADPKD)**: bilateral palpable renal masses, hypertension, elevated creatinine, and a strong family history (father died of kidney disease at 51).
- **Renal ultrasound is the first-line imaging test** for diagnosing ADPKD due to its **non-invasiveness, no radiation exposure, high sensitivity for detecting cysts, and cost-effectiveness**.
- Ultrasound can establish the diagnosis using **established diagnostic criteria** (Pei-Ravine criteria based on age and number of cysts) and is recommended by **KDIGO guidelines** as the initial imaging modality.
- In this patient with clear clinical features and palpable masses, ultrasound will readily confirm the diagnosis by demonstrating multiple bilateral renal cysts.
*24-hour urine protein collection*
- This test quantifies **proteinuria** to assess for glomerular damage.
- While proteinuria can occur in ADPKD, it is not a diagnostic test and would not help identify or characterize the bilateral renal masses in this presentation.
*Chest X-ray*
- A chest X-ray evaluates the **lungs and heart**.
- It provides no diagnostic information regarding renal masses or kidney pathology and is not indicated in this case.
*Genetic testing for polycystic kidney disease*
- **Genetic testing** (for PKD1 or PKD2 mutations) can confirm ADPKD definitively and is useful for family counseling and cases with uncertain imaging findings.
- However, it is **not the first-line test** and is typically performed *after* imaging has established the diagnosis, or in specific situations (e.g., young patients, potential living kidney donors, atypical presentations).
- In this patient with clear clinical and anticipated imaging findings, genetic testing is unnecessary for initial diagnosis.
*CT scan of abdomen and pelvis*
- CT scan provides excellent anatomic detail and is useful in ADPKD for **evaluating complications** such as cyst hemorrhage, infection, suspected malignancy, or for **preoperative planning**.
- However, it is **not the first-line diagnostic test** due to higher cost, radiation exposure, and the fact that ultrasound is equally effective for initial diagnosis.
- CT would be reserved for situations where ultrasound is inconclusive or when complications are suspected.
Metacognition and diagnostic calibration US Medical PG Question 9: A 50-year-old woman presents with severe abdominal pain. Past medical history is significant for a peptic ulcer. Physical examination is limited because the patient will not allow abdominal palpation due to the pain. The attending makes a presumptive diagnosis of peritonitis. Which of the following non-invasive maneuvers would be most helpful in confirming the diagnosis of peritonitis in this patient?
- A. Rectal examination shows guaiac positive stool
- B. Forced cough elicits abdominal pain (Correct Answer)
- C. Hyperactive bowel sounds are heard on auscultation
- D. Bowel sounds are absent on auscultation
- E. Pain is aroused with gentle intensity/pressure at the costovertebral angle
Metacognition and diagnostic calibration Explanation: ***Forced cough elicits abdominal pain***
- A forced cough increases **intra-abdominal pressure**, which in turn stretches the inflamed peritoneum.
- Elicitation of pain with coughing is a highly sensitive and specific sign for **peritoneal irritation** and helps confirm the diagnosis of peritonitis.
*Rectal examination shows guaiac positive stool*
- **Guaiac positive stool** indicates the presence of blood in the stool, which is a sign of gastrointestinal bleeding.
- While a peptic ulcer can cause bleeding, this finding does not directly confirm **peritonitis** or peritoneal inflammation.
*Hyperactive bowel sounds are heard on auscultation*
- **Hyperactive bowel sounds** are often associated with conditions like gastroenteritis or partial bowel obstruction.
- In peritonitis, bowel sounds are typically diminished or absent due to **ileus**, not hyperactive.
*Bowel sounds are absent on auscultation*
- While **absent bowel sounds** can be a sign of peritonitis due to paralytic ileus, this finding is not as specific or immediately helpful as eliciting pain with coughing in confirming the primary diagnosis in a patient already presumed to have peritonitis.
- The absence of bowel sounds can also be seen in other conditions and may take longer to develop consistently.
*Pain is aroused with gentle intensity/pressure at the costovertebral angle*
- Pain at the **costovertebral angle (CVA)** typically indicates inflammation of the kidney or surrounding structures, such as in pyelonephritis.
- This finding is specific to **renal pathology** and not directly related to generalized peritonitis.
Metacognition and diagnostic calibration US Medical PG Question 10: A 63-year-old retired teacher presents to his family physician for an annual visit. He has been healthy for most of his life and currently takes no medications, although he has had elevated blood pressure on several visits in the past few years but declined taking any medication. He has no complaints about his health and has been enjoying time with his grandchildren. He has been a smoker for 40 years–ranging from half to 1 pack a day, and he drinks 1 beer daily. On presentation, his blood pressure is 151/98 mm Hg in both arms, heart rate is 89/min, and respiratory rate is 14/min. Physical examination reveals a well-appearing man with no physical abnormalities. A urinalysis is performed and shows microscopic hematuria. Which of the following is the best next step for this patient?
- A. Perform intravenous pyelography
- B. Reassure the patient and recommend lifestyle modifications for his hypertension
- C. Perform a cystoscopy
- D. Perform a CT scan of the abdomen with contrast (Correct Answer)
- E. Repeat the urinalysis
Metacognition and diagnostic calibration Explanation: ***Perform a CT scan of the abdomen with contrast***
- This patient has **asymptomatic microscopic hematuria** with significant risk factors: age >60 years and **40-year smoking history** (major risk factor for urothelial malignancy).
- According to **AUA guidelines**, patients with risk factors and microscopic hematuria require complete evaluation including **upper tract imaging (CT urography preferred) AND cystoscopy**.
- CT urography is the gold standard for detecting **renal cell carcinoma, urothelial carcinoma, and structural abnormalities** of the upper urinary tract.
- In high-risk patients like this, proceeding directly to imaging is appropriate rather than waiting to confirm persistent hematuria.
*Repeat the urinalysis*
- Repeating urinalysis is appropriate for patients with **transient causes** of hematuria (vigorous exercise, menstruation, urinary tract infection, recent instrumentation).
- This patient has **no evidence of transient causes** and has significant risk factors requiring immediate workup.
- Delaying evaluation in a high-risk patient could miss early malignancy when it is most treatable.
*Perform a cystoscopy*
- **Cystoscopy** is indeed part of the standard hematuria workup and evaluates the bladder and urethra for malignancy.
- However, it should be performed **in conjunction with upper tract imaging**, not alone, as it cannot visualize the kidneys or ureters.
- Both cystoscopy and imaging are needed for complete evaluation; imaging is typically done first to identify upper tract pathology.
*Reassure the patient and recommend lifestyle modifications for his hypertension*
- While addressing **hypertension** is important, ignoring microscopic hematuria in a high-risk patient is inappropriate.
- **Smoking and age** make this patient high-risk for genitourinary malignancies that require prompt investigation.
- This approach could result in dangerous delays in diagnosing serious conditions like **renal cell carcinoma or bladder cancer**.
*Perform intravenous pyelography*
- **Intravenous pyelography (IVP)** is an outdated imaging technique largely replaced by **CT urography**.
- CT urography provides superior sensitivity for detecting **renal masses and urothelial abnormalities** with better anatomical detail.
- IVP has lower diagnostic accuracy and higher radiation exposure compared to modern CT imaging.
More Metacognition and diagnostic calibration US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.