Decision making under uncertainty US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Decision making under uncertainty. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Decision making under uncertainty US Medical PG Question 1: Two dizygotic twins present to the university clinic because they believe they are being poisoned through the school's cafeteria food. They have brought these concerns up in the past, but no other students or cafeteria staff support this belief. Both of them are average students with strong and weak subject areas as demonstrated by their course grade-books. They have no known medical conditions and are not known to abuse illicit substances. Which statement best describes the condition these patients have?
- A. A trial separation is likely to worsen symptoms.
- B. The disorder is its own disease entity in DSM-5.
- C. Antipsychotic medications are rarely beneficial.
- D. Can affect two or more closely related individuals. (Correct Answer)
- E. Cognitive behavioral therapy is a good first-line.
Decision making under uncertainty Explanation: ***Can affect two or more closely related individuals.***
- The shared delusional belief in **folie à deux**, also known as **shared psychotic disorder**, typically occurs in two or more people who are closely associated.
- In this case, the **dizygotic twins** sharing the same delusional belief about being poisoned from cafeteria food fits this pattern.
*A trial separation is likely to worsen symptoms.*
- **Separating the individuals** involved in **folie à deux** is often a crucial step in treatment, as it can help break the cycle of shared delusion and allow for individual therapy.
- Separation typically IMPROVES rather than worsens symptoms by removing the reinforcement of the shared delusion.
*The disorder is its own disease entity in DSM-5.*
- In the **DSM-5**, **folie à deux** is no longer considered a separate diagnostic category.
- Instead, it is classified under **Other Specified Schizophrenia Spectrum and Other Psychotic Disorder** or **Unspecified Schizophrenia Spectrum and Other Psychotic Disorder**, with the specific context of shared delusion noted.
*Antipsychotic medications are rarely beneficial.*
- **Antipsychotics** are actually commonly used in treating folie à deux, particularly for the **primary individual** who initially developed the delusion.
- They can be an important component of treatment, often combined with separation and psychotherapy.
*Cognitive behavioral therapy is a good first-line.*
- **Cognitive Behavioral Therapy (CBT)** can be beneficial, particularly after separation, to help individuals challenge and reframe their delusional beliefs.
- However, the **first-line intervention** for shared psychotic disorder is **separation of the involved individuals**, followed by individual therapy (which may include CBT) and medication as needed.
Decision making under uncertainty US Medical PG Question 2: You are reading through a recent article that reports significant decreases in all-cause mortality for patients with malignant melanoma following treatment with a novel biological infusion. Which of the following choices refers to the probability that a study will find a statistically significant difference when one truly does exist?
- A. Type II error
- B. Type I error
- C. Confidence interval
- D. p-value
- E. Power (Correct Answer)
Decision making under uncertainty Explanation: ***Power***
- **Power** is the probability that a study will correctly reject the null hypothesis when it is, in fact, false (i.e., will find a statistically significant difference when one truly exists).
- A study with high power minimizes the risk of a **Type II error** (failing to detect a real effect).
*Type II error*
- A **Type II error** (or **beta error**) occurs when a study fails to reject a false null hypothesis, meaning it concludes there is no significant difference when one actually exists.
- This is the **opposite** of what the question describes, which asks for the probability of *finding* a difference.
*Type I error*
- A **Type I error** (or **alpha error**) occurs when a study incorrectly rejects a true null hypothesis, concluding there is a significant difference when one does not actually exist.
- This relates to the **p-value** and the level of statistical significance (e.g., p < 0.05).
*Confidence interval*
- A **confidence interval** provides a range of values within which the true population parameter is likely to lie with a certain degree of confidence (e.g., 95%).
- It does not directly represent the probability of finding a statistically significant difference when one truly exists.
*p-value*
- The **p-value** is the probability of observing data as extreme as, or more extreme than, that obtained in the study, assuming the null hypothesis is true.
- It is used to determine statistical significance, but it is not the probability of detecting a true effect.
Decision making under uncertainty US Medical PG Question 3: A 52-year-old man comes to the physician because of a 3-week history of a cough and hoarseness. He reports that the cough is worse when he lies down after lunch. His temperature is 37.5°C (99.5°F); the remainder of his vital signs are within normal limits. Because the physician has recently been seeing several patients with the common cold, the diagnosis of a viral upper respiratory tract infection readily comes to mind. The physician fails to consider the diagnosis of gastroesophageal reflux disease, which the patient is later found to have. Which of the following most accurately describes the cognitive bias that the physician had?
- A. Framing
- B. Anchoring
- C. Visceral
- D. Confirmation
- E. Availability (Correct Answer)
Decision making under uncertainty Explanation: ***Availability***
- The physician recently seeing several patients with the common cold led to this diagnosis readily coming to mind, demonstrating how easily recalled examples can disproportionately influence diagnosis.
- This bias occurs when easily recalled instances or information (like recent cases of common cold) are used to estimate the likelihood or frequency of an event, even if other more relevant data exist.
*Framing*
- This bias occurs when the way information is presented (e.g., as a gain or a loss) influences a decision, rather than the intrinsic characteristics of the options themselves.
- The scenario does not involve the presentation of information in different ways to sway the physician's judgment.
*Anchoring*
- This bias involves relying too heavily on an initial piece of information (the "anchor") when making subsequent judgments, often leading to insufficient adjustment away from that anchor.
- While the physician initially considered a viral URI, the setup is more about the ease of recall influencing the decision rather than being stuck on an initial data point.
*Visceral*
- This is not a commonly recognized cognitive bias in the context of medical decision-making; "visceral" largely refers to emotional or intuitive feelings rather than a structured cognitive bias.
- Cognitive biases describe systematic patterns of deviation from norm or rationality in judgment, not merely emotional responses.
*Confirmation*
- This bias involves seeking, interpreting, favoring, and recalling information in a way that confirms one's pre-existing beliefs or hypotheses.
- The physician did not actively seek information to confirm the common cold diagnosis; rather, the diagnosis came to mind due to recent encounters, which aligns with availability bias.
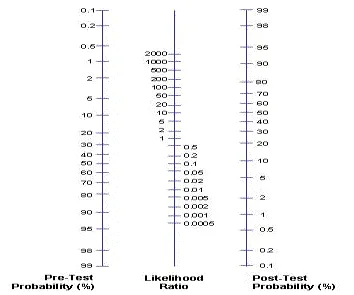
Decision making under uncertainty US Medical PG Question 4: A 14-month-old Caucasian boy is admitted to the pediatric clinic with an 8-month history of diarrhea, abdominal tenderness and concomitant failure to thrive. One of the possibilities that may cause these symptoms is Crohn’s disease, and on the basis of the attending pediatrician’s experience, the pre-test probability of this diagnosis was estimated at 40%. According to Fagan’s diagram (picture), if the likelihood ratio of a negative test result (LR-) is 0.04, what is the chance that this is the right diagnosis?
- A. 2.5% (Correct Answer)
- B. 25%
- C. 97.5%
- D. 40%
- E. 75%
Decision making under uncertainty Explanation: ***2.5%***
- To use **Fagan's nomogram**, draw a line connecting the **pre-test probability** (40%) on the left axis to the **likelihood ratio (LR-)** (0.04) on the middle axis.
- The point where this line intersects the **post-test probability** axis on the right provides the answer, which is approximately **2.5%**.
*25%*
- This value would result from a much higher LR- or a different pre-test probability, not matching the given parameters.
- If the LR- was significantly higher, like around 0.5, with the same pre-test probability, the post-test probability could be closer to 25%.
*97.5%*
- This high post-test probability would only occur with a strong **positive likelihood ratio (LR+)** and a high pre-test probability, indicating a very strong confirmation of the diagnosis.
- A **negative test result (LR-)** should decrease, not increase, the probability of the diagnosis.
*40%*
- This is the **pre-test probability**, not the post-test probability after incorporating the test result.
- The result of a diagnostic test (especially a negative one with a low LR-) should change the probability, so the post-test probability cannot be the same as the pre-test probability unless the LR is 1.
*75%*
- A post-test probability of 75% would indicate a significant increase in the likelihood of the disease, usually associated with a high **LR+** from a positive test result.
- This value is inconsistent with a negative test result and an LR- of 0.04, which should decrease the probability.
Decision making under uncertainty US Medical PG Question 5: A research study is comparing 2 novel tests for the diagnosis of Alzheimer’s disease (AD). The first is a serum blood test, and the second is a novel PET radiotracer that binds to beta-amyloid plaques. The researchers intend to have one group of patients with AD assessed via the novel blood test, and the other group assessed via the novel PET examination. In comparing these 2 trial subsets, the authors of the study may encounter which type of bias?
- A. Selection bias (Correct Answer)
- B. Confounding bias
- C. Recall bias
- D. Measurement bias
- E. Lead-time bias
Decision making under uncertainty Explanation: ***Selection bias***
- This occurs when different patient groups are assigned to different interventions or measurements in a way that creates **systematic differences** between comparison groups.
- In this study, having **separate patient groups** assessed with different diagnostic methods (blood test vs. PET scan) means any differences observed could be due to **differences in the patient populations** rather than differences in test performance.
- To validly compare two diagnostic tests, both tests should ideally be performed on the **same patients** (paired design) or patients should be **randomly assigned** to receive one test or the other, ensuring comparable groups.
- This is a fundamental **study design flaw** that prevents valid comparison of the two diagnostic methods.
*Measurement bias*
- Also called information bias, this occurs when there are systematic errors in how outcomes or exposures are measured.
- While using different measurement tools could introduce measurement variability, the primary issue here is that **different patient populations** are being compared, not just different measurement methods on the same population.
- Measurement bias would be more relevant if the same patients were assessed with both methods but one method was systematically misapplied or measured incorrectly.
*Confounding bias*
- This occurs when an extraneous variable is associated with both the exposure and outcome, distorting the observed relationship.
- While patient characteristics could confound results, the fundamental problem is the **study design itself** (separate groups for separate tests), which is selection bias.
*Recall bias*
- This involves systematic differences in how participants remember or report past events, common in **retrospective case-control studies**.
- Not relevant here, as this involves prospective diagnostic testing, not recollection of past exposures.
*Lead-time bias*
- Occurs in screening studies when earlier detection makes survival appear longer without changing disease outcomes.
- Not applicable to this scenario, which focuses on comparing two diagnostic methods in separate patient groups, not on survival or disease progression timing.
Decision making under uncertainty US Medical PG Question 6: A pharmaceutical corporation is developing a research study to evaluate a novel blood test to screen for breast cancer. They enrolled 800 patients in the study, half of which have breast cancer. The remaining enrolled patients are age-matched controls who do not have the disease. Of those in the diseased arm, 330 are found positive for the test. Of the patients in the control arm, only 30 are found positive. What is this test’s sensitivity?
- A. 330 / (330 + 30)
- B. 330 / (330 + 70) (Correct Answer)
- C. 370 / (30 + 370)
- D. 370 / (70 + 370)
- E. 330 / (400 + 400)
Decision making under uncertainty Explanation: ***330 / (330 + 70)***
- **Sensitivity** measures the proportion of actual **positives** that are correctly identified as such.
- In this study, there are **400 diseased patients** (half of 800). Of these, 330 tested positive (true positives), meaning 70 tested negative (false negatives). So sensitivity is **330 / (330 + 70)**.
*330 / (330 + 30)*
- This calculation represents the **positive predictive value**, which is the probability that subjects with a positive screening test truly have the disease. It uses **true positives / (true positives + false positives)**.
- It does not correctly calculate **sensitivity**, which requires knowing the total number of diseased individuals.
*370 / (30 + 370)*
- This expression is attempting to calculate **specificity**, which is the proportion of actual negatives that are correctly identified. It would be **true negatives / (true negatives + false positives)**.
- However, the numbers used are incorrect for specificity in this context given the data provided.
*370 / (70 + 370)*
- This formula is an incorrect combination of values and does not represent any standard epidemiological measure like **sensitivity** or **specificity**.
- It is attempting to combine false negatives (70) and true negatives (370 from control arm) in a non-standard way.
*330 / (400 + 400)*
- This calculation attempts to divide true positives by the total study population (800 patients).
- This metric represents the **prevalence of true positives within the entire study cohort**, not the test's **sensitivity**.
Decision making under uncertainty US Medical PG Question 7: A 14-month-old boy is brought in by his parents with an 8-month history of diarrhea, abdominal tenderness and concomitant failure to thrive. The pediatric attending physician believes that Crohn’s disease is the best explanation of this patient’s symptoms. Based on the pediatric attending physician’s experience, the pretest probability of this diagnosis is estimated at 40%. According to Fagan nomogram (see image). If the likelihood ratio of a negative test result (LR-) for Crohn’s disease is 0.04, what is the chance that this is the correct diagnosis in this patient with a negative test result?
- A. 40%
- B. 75%
- C. 97.5%
- D. 25%
- E. 2.5% (Correct Answer)
Decision making under uncertainty Explanation: ***2.5%***
- Begin by locating the **pretest probability of 40%** on the left-hand scale of the **Fagan nomogram**
- Draw a line from this point through the **likelihood ratio negative (LR-) of 0.04** on the middle scale, extending it to the right-hand scale to find the **posttest probability of approximately 2.5%**
- This can be verified mathematically: pretest odds = 0.40/0.60 = 0.667; posttest odds = 0.667 × 0.04 = 0.027; posttest probability = 0.027/1.027 ≈ 2.6% (rounds to 2.5%)
*40%*
- This represents the **initial pretest probability** before incorporating the test result
- It does not account for the impact of the **negative test result** with an LR- of 0.04
- The Fagan nomogram is used to **update this probability** based on the test outcome
*75%*
- This value does not align with a **negative test result** and an **LR- of 0.04**
- A posttest probability higher than the pretest probability would require a positive test with an LR+ greater than 1
- With a negative test and LR- = 0.04, the probability must decrease significantly
*97.5%*
- This extremely high posttest probability would require a **positive test** with a very high **likelihood ratio positive (LR+)**
- It is completely inconsistent with a **negative test result** and a low LR- of 0.04
- An LR- of 0.04 indicates strong evidence against the disease, not for it
*25%*
- While this represents a decrease from the pretest probability of 40%, it underestimates the impact of the test result
- An **LR- of 0.04** means the odds of having the disease are reduced by a factor of 25 (multiplied by 0.04)
- This should yield a much lower posttest probability than 25%
Decision making under uncertainty US Medical PG Question 8: A 75-year-old woman presents to her primary care physician with her son because she is convinced that people are stealing from her. Her son claims she has been misplacing her medications and money throughout the house. She recently lost her husband to old age and has become reclusive and no longer wants people to visit. Physical examination is unremarkable and the patient is oriented to person, time, and place. A mini-mental status examination (MMSE) is performed and she has difficulty recalling words after 5 minutes and also has problems with serial subtraction. Which of the following is the most likely diagnosis in this patient?
- A. Histrionic personality disorder
- B. Schizophrenia
- C. Delirium
- D. Schizoid personality disorder
- E. Dementia (Correct Answer)
Decision making under uncertainty Explanation: ***Dementia***
- The patient has **primary cognitive impairment** evidenced by MMSE deficits (poor delayed recall, impaired serial subtraction) and functional decline (misplacing items).
- Her **delusions of theft are secondary to dementia**, a common behavioral and psychological symptom of dementia (BPSD), particularly in Alzheimer's disease.
- The **insidious onset** in a 75-year-old with progressive memory decline points to a neurodegenerative process.
- Orientation remains intact in early-to-moderate dementia, which doesn't rule out the diagnosis.
- The stressor (husband's death) may have unmasked or accelerated symptom recognition but doesn't explain the cognitive deficits.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, which are not evident in this presentation.
- Personality disorders are lifelong patterns, not new-onset conditions in elderly patients with cognitive decline.
- Does not explain the objective cognitive deficits on MMSE.
*Schizophrenia*
- Schizophrenia typically has onset in **late adolescence to early adulthood**, not at age 75.
- While late-onset schizophrenia exists, the **prominent cognitive impairment** (memory, executive function) as the PRIMARY feature points toward dementia rather than a primary psychotic disorder.
- Schizophrenia would show more pervasive psychotic symptoms without the specific pattern of memory and executive dysfunction seen here.
*Delirium*
- Delirium has **acute onset** (hours to days) with **fluctuating consciousness** and altered attention.
- This patient is **oriented to person, time, and place** and has a gradual, progressive course (misplacing items over time).
- No mention of acute medical illness, medication changes, or rapid cognitive fluctuation.
*Schizoid personality disorder*
- A lifelong pattern of **social detachment** and restricted emotional expression, not a new condition in late life.
- Does not explain the cognitive impairment, memory deficits, or delusional beliefs.
- The patient's reclusiveness is reactive to recent loss and concerns about theft, not a longstanding personality trait.
Decision making under uncertainty US Medical PG Question 9: A 65-year-old man is admitted to the hospital because of a 1-month history of fatigue, intermittent fever, and weakness. Results from a peripheral blood smear taken during his evaluation are indicative of possible acute myeloid leukemia. Bone marrow aspiration and subsequent cytogenetic studies confirm the diagnosis. The physician sets aside an appointed time-slot and arranges a meeting in a quiet office to inform him about the diagnosis and discuss his options. He has been encouraged to bring someone along to the appointment if he wanted. He comes to your office at the appointed time with his daughter. He appears relaxed, with a full range of affect. Which of the following is the most appropriate opening statement in this situation?
- A. Your lab reports show that you have an acute myeloid leukemia
- B. What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies? (Correct Answer)
- C. You must be curious and maybe even anxious about the results of your tests.
- D. I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.
- E. Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?
Decision making under uncertainty Explanation: ***"What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies?"***
- This **open-ended question** allows the patient to express their current knowledge and perceptions, which helps the physician tailor the discussion.
- It establishes a **patient-centered approach**, respecting the patient's existing understanding and preparing them for further information.
*"You must be curious and maybe even anxious about the results of your tests."*
- While empathic, this statement makes an **assumption about the patient's feelings** rather than inviting them to share their own.
- It is often better to ask directly or use more open-ended questions that allow the patient to express their true emotions, especially given their **relaxed demeanor**.
*"I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.”"*
- This statement immediately introduces **overwhelming and potentially alarming information** (referral, chemotherapy, radiotherapy) without first establishing the diagnosis or assessing the patient's readiness to receive it.
- It prematurely jumps to treatment and logistics, potentially causing **unnecessary distress** before the patient has processed the core diagnosis.
*"Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?""*
- While it attempts to assess the patient's preference for information, this question is a **closed-ended "either/or" choice** that might limit the patient's ability to express nuanced needs.
- It also prematurely introduces the idea of "options" without first explaining the diagnosis in an understandable context.
*"Your lab reports show that you have an acute myeloid leukemia"*
- This is a **direct and blunt delivery of a serious diagnosis** without any preparatory context or assessment of the patient's existing knowledge or emotional state.
- Delivering such news abruptly can be shocking and overwhelming, potentially **hindering effective communication** and rapport building.
Decision making under uncertainty US Medical PG Question 10: A 53-year-old man presents with a 2-year-history of dull, nonspecific flank pain that subsides with rest. His past medical history is significant for hypertension, hypercholesterolemia, and type 2 diabetes mellitus. He has no allergies and takes no medications. His father died of kidney disease at the age of 51, and his mother has been treated for ovarian cancer. On presentation, his blood pressure is 168/98 mm Hg, and his heart rate is 102/min. Abdominal examination is significant for palpable bilateral renal masses. His laboratory tests are significant for creatinine of 2.0 mg/dL and a BUN of 22 mg/dL. Which of the following tests is most recommended in this patient?
- A. Chest X-ray
- B. Genetic testing for polycystic kidney disease
- C. CT scan of abdomen and pelvis
- D. 24-hour urine protein collection
- E. Renal ultrasound (Correct Answer)
Decision making under uncertainty Explanation: ***Renal ultrasound***
- This patient presents with classic features of **autosomal dominant polycystic kidney disease (ADPKD)**: bilateral palpable renal masses, hypertension, elevated creatinine, and a strong family history (father died of kidney disease at 51).
- **Renal ultrasound is the first-line imaging test** for diagnosing ADPKD due to its **non-invasiveness, no radiation exposure, high sensitivity for detecting cysts, and cost-effectiveness**.
- Ultrasound can establish the diagnosis using **established diagnostic criteria** (Pei-Ravine criteria based on age and number of cysts) and is recommended by **KDIGO guidelines** as the initial imaging modality.
- In this patient with clear clinical features and palpable masses, ultrasound will readily confirm the diagnosis by demonstrating multiple bilateral renal cysts.
*24-hour urine protein collection*
- This test quantifies **proteinuria** to assess for glomerular damage.
- While proteinuria can occur in ADPKD, it is not a diagnostic test and would not help identify or characterize the bilateral renal masses in this presentation.
*Chest X-ray*
- A chest X-ray evaluates the **lungs and heart**.
- It provides no diagnostic information regarding renal masses or kidney pathology and is not indicated in this case.
*Genetic testing for polycystic kidney disease*
- **Genetic testing** (for PKD1 or PKD2 mutations) can confirm ADPKD definitively and is useful for family counseling and cases with uncertain imaging findings.
- However, it is **not the first-line test** and is typically performed *after* imaging has established the diagnosis, or in specific situations (e.g., young patients, potential living kidney donors, atypical presentations).
- In this patient with clear clinical and anticipated imaging findings, genetic testing is unnecessary for initial diagnosis.
*CT scan of abdomen and pelvis*
- CT scan provides excellent anatomic detail and is useful in ADPKD for **evaluating complications** such as cyst hemorrhage, infection, suspected malignancy, or for **preoperative planning**.
- However, it is **not the first-line diagnostic test** due to higher cost, radiation exposure, and the fact that ultrasound is equally effective for initial diagnosis.
- CT would be reserved for situations where ultrasound is inconclusive or when complications are suspected.
More Decision making under uncertainty US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.